Assessment of Quadriceps Muscle in Advanced Knee Osteoarthritis and Correlation with Lower Limb Alignment
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Radiographic Evaluations
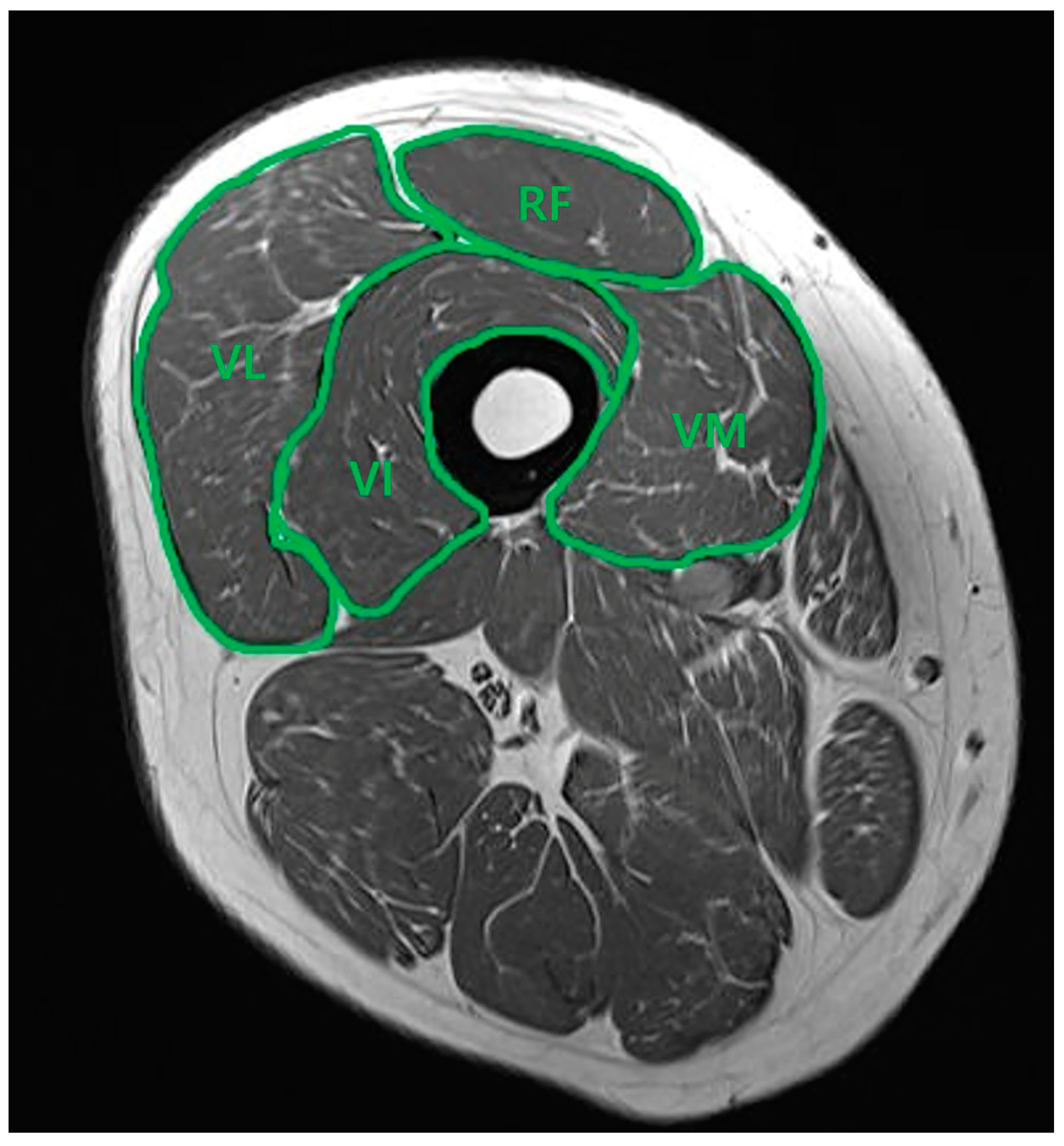
2.3. Thigh Muscle Cross-Sectional Area Measurement
2.4. Statistical Analysis
3. Results
3.1. OA Grade Differences in Thigh Muscle CSA Measurements
3.2. Muscle CSA in Relation to Knee Alignment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Lawrence, K.W.; Link, L.; Lavin, P.; Schwarzkopf, R.; Rozell, J.C. Characterizing patient factors, perioperative interventions, and outcomes associated with inpatients falls after total knee arthroplasty. Knee. Surg. Relat. Res. 2024, 36, 11. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.H.; Park, Y.B.; Baek, S.H. Clinical and Radiological Outcomes of Computer-Assisted Navigation in Primary Total Knee Arthroplasty for Patients with Extra-articular Deformity: Systematic Review and Meta-Analysis. Clin. Orthop. Surg. 2024, 16, 430–440. [Google Scholar] [CrossRef] [PubMed]
- Li, G.; Zhou, C.; Li, S.; Yu, J.; Foster, T.; Bedair, H. Tibiofemoral articulation and axial tibial rotation of the knee after a cruciate retaining total knee arthroplasty. Knee. Surg. Relat. Res. 2024, 36, 20. [Google Scholar] [CrossRef]
- Yang, H.Y.; Yoon, T.W.; Kim, J.Y.; Seon, J.K. Radiologic Assessment of Knee Phenotypes Based on the Coronal Plane Alignment of the Knee Classification in a Korean Population. Clin. Orthop. Surg. 2024, 16, 422–429. [Google Scholar] [CrossRef]
- Øiestad, B.E.; Juhl, C.B.; Eitzen, I.; Thorlund, J.B. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthr. Cartilage. 2015, 23, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Pattyn, E.; Verdonk, P.; Steyaert, A.; Vanden Bossche, L.; Van den Broecke, W.; Thijs, Y.; Witvrouw, E. Vastus medialis obliquus atrophy: Does it exist in patellofemoral pain syndrome? Am. J. Sports Med. 2011, 39, 1450–1455. [Google Scholar] [CrossRef]
- Wang, Y.; Wluka, A.E.; Berry, P.A.; Siew, T.; Teichtahl, A.J.; Urquhart, D.M.; Lloyd, D.G.; Jones, G.; Cicuttini, F.M. Increase in vastus medialis cross-sectional area is associated with reduced pain, cartilage loss, and joint replacement risk in knee osteoarthritis. Arthritis. Rheum. 2012, 64, 3917–3925. [Google Scholar] [CrossRef]
- Raynauld, J.P.; Pelletier, J.P.; Roubille, C.; Dorais, M.; Abram, F.; Li, W.; Wang, Y.; Fairley, J.; Cicuttini, F.M.; Martel-Pelletier, J. Magnetic Resonance Imaging-Assessed Vastus Medialis Muscle Fat Content and Risk for Knee Osteoarthritis Progression: Relevance From a Clinical Trial. Arthritis. Care. Res. 2015, 67, 1406–1415. [Google Scholar] [CrossRef]
- Pan, J.; Stehling, C.; Muller-Hocker, C.; Schwaiger, B.J.; Lynch, J.; McCulloch, C.E.; Nevitt, M.C.; Link, T.M. Vastus lateralis/vastus medialis cross-sectional area ratio impacts presence and degree of knee joint abnormalities and cartilage T2 determined with 3T MRI—An analysis from the incidence cohort of the Osteoarthritis Initiative. Osteoarthr. Cartilage. 2011, 19, 65–73. [Google Scholar] [CrossRef]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef]
- Fink, B.; Egl, M.; Singer, J.; Fuerst, M.; Bubenheim, M.; Neuen-Jacob, E. Morphologic changes in the vastus medialis muscle in patients with osteoarthritis of the knee. Arthritis Rheum. 2007, 56, 3626–3633. [Google Scholar] [CrossRef] [PubMed]
- Palmieri-Smith, R.M.; Thomas, A.C.; Karvonen-Gutierrez, C.; Sowers, M.F. Isometric quadriceps strength in women with mild, moderate, and severe knee osteoarthritis. Am. J. Phys. Med. Rehabil. 2010, 89, 541–548. [Google Scholar] [CrossRef]
- Murray, A.M.; Thomas, A.C.; Armstrong, C.W.; Pietrosimone, B.G.; Tevald, M.A. The associations between quadriceps muscle strength, power, and knee joint mechanics in knee osteoarthritis: A cross-sectional study. Clin. Biomech. 2015, 30, 1140–1145. [Google Scholar] [CrossRef]
- Slemenda, C.; Brandt, K.D.; Heilman, D.K.; Mazzuca, S.; Braunstein, E.M.; Katz, B.P.; Wolinsky, F.D. Quadriceps weakness and osteoarthritis of the knee. Ann Intern. Med. 1997, 127, 97–104. [Google Scholar] [CrossRef]
- Liikavainio, T.; Lyytinen, T.; Tyrväinen, E.; Sipilä, S.; Arokoski, J.P. Physical function and properties of quadriceps femoris muscle in men with knee osteoarthritis. Arch. Phys. Med. Rehabil. 2008, 89, 2185–2194. [Google Scholar] [CrossRef]
- Segal, N.A.; Torner, J.C.; Felson, D.; Niu, J.; Sharma, L.; Lewis, C.E.; Nevitt, M. Effect of thigh strength on incident radiographic and symptomatic knee osteoarthritis in a longitudinal cohort. Arthritis Rheum. 2009, 61, 1210–1217. [Google Scholar] [CrossRef]
- Omori, G.; Koga, Y.; Tanaka, M.; Nawata, A.; Watanabe, H.; Narumi, K.; Endoh, K. Quadriceps muscle strength and its relationship to radiographic knee osteoarthritis in Japanese elderly. J. Orthop. Sci. 2013, 18, 536–542. [Google Scholar] [CrossRef]
- Pietrosimone, B.; Thomas, A.C.; Saliba, S.A.; Ingersoll, C.D. Association between quadriceps strength and self-reported physical activity in people with knee osteoarthritis. Int. J. Sports Phys. Ther. 2014, 9, 320–328. [Google Scholar]
- Segal, N.A.; Glass, N.A. Is quadriceps muscle weakness a risk factor for incident or progressive knee osteoarthritis? Phys. Sportsmed. 2011, 39, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Alnahdi, A.H.; Zeni, J.A.; Snyder-Mackler, L. Muscle impairments in patients with knee osteoarthritis. Sports Health 2012, 4, 284–292. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi, M.; Fukumoto, Y.; Kobayashi, M.; Kawasaki, T.; Maegawa, S.; Ibuki, S.; Ichihashi, N. Quantity and Quality of the Lower Extremity Muscles in Women with Knee Osteoarthritis. Ultrasound Med. Biol. 2015, 41, 2567–2574. [Google Scholar] [CrossRef]
- Berger, M.J.; Chess, D.G.; Doherty, T.J. Vastus medialis motor unit properties in knee osteoarthritis. BMC Musculoskelet Disord. 2011, 12, 199. [Google Scholar] [CrossRef]
- Segal, N.A.; Findlay, C.; Wang, K.; Torner, J.C.; Nevitt, M.C. The longitudinal relationship between thigh muscle mass and the development of knee osteoarthritis. Osteoarthr. Cartilage. 2012, 20, 1534–1540. [Google Scholar] [CrossRef]
- van den Noort, J.C.; van der Leeden, M.; Stapper, G.; Wirth, W.; Maas, M.; Roorda, L.D.; Lems, W.F.; Dekker, J.; van der Esch, M. Muscle weakness is associated with non-contractile muscle tissue of the vastus medialis muscle in knee osteoarthritis. BMC Musculoskelet Disord. 2022, 23, 91. [Google Scholar] [CrossRef]
| OA Group (n = 50) | Control Group (n = 25) | p-Value | |
|---|---|---|---|
| Age (years) | 0.000 * | ||
| Mean ± SD | 69.3 ± 6.7 | 44.8 ± 15.1 | |
| Gender | 0.008 * | ||
| Male, n (%) | 9 (18.0%) | 13 (52.0%) | |
| Female, n (%) | 41 (82.0%) | 12 (48.0%) | |
| Height (cm) | 0.000 * | ||
| Mean ± SD | 154.9 ± 9.6 | 165.9 ± 8.4 | |
| Weight (kg) | 0.000 * | ||
| Mean ± SD | 63.3 ± 9.0 | 76.3 ± 16.1 | |
| BMI (kg/m2) | 0.247 | ||
| Mean ± SD | 26.4 ± 3.2 | 27.6 ± 4.7 | |
| Side | 0.624 | ||
| Right, n (%) | 23 (46.0%) | 13 (52.0%) | |
| Left, n (%) | 27 (54.0%) | 12 (48.0%) | |
| Alignment classification | 0.000 * | ||
| Normal, n (%) | 13 (26.0%) | 23 (92.0%) | |
| Mild varus, n (%) | 15 (30.0%) | 2 (8.0%) | |
| Severe varus, n (%) | 22 (44.0%) | 0 (0%) | |
| OA grade (KL) | 0.000 * | ||
| KL 0, n (%) | 0 (0%) | 4 (16.0%) | |
| KL 1, n (%) | 0 (0%) | 11 (44.0%) | |
| KL 2, n (%) | 0 (0%) | 10 (40.0%) | |
| KL 3, n (%) | 5 (10.0%) | 0 (0%) | |
| KL 4, n (%) | 45 (90.0%) | 0 (0%) |
| OA Group (n = 50) | Control Group (n = 25) | p-Value | |
|---|---|---|---|
| RF | 10.52 ± 2.15 | 10.94 ± 1.92 | 0.408 |
| VI | 33.14 ± 3.48 | 32.26 ± 4.27 | 0.338 |
| VM | 22.39 ± 2.77 | 21.67 ± 3.39 | 0.327 |
| VL | 33.94 ± 2.65 | 35.13 ± 4.17 | 0.203 |
| Group I (n = 36) Normal Alignment | Group II (n = 17) Mild Varus Alignment | Group III (n = 22) Severe Varus Alignment | p-Value | ||
|---|---|---|---|---|---|
| Age (years) | 0.000 * | I < II, III | |||
| Mean ± SD | 51.2 ± 17.4 | 66.4 ± 10.5 | 69.3 ± 7.7 | ||
| Gender | 0.247 | ||||
| Male, n (%) | 14 (38.9%) | 3 (17.6%) | 5 (22.7%) | ||
| Female, n (%) | 22 (61.1%) | 14 (82.4%) | 17 (77.3%) | ||
| Height (cm) | 0.008 * | I < III | |||
| Mean ± SD | 163.5 ± 9.8 | 155.4 ± 8.9 | 154.6 ± 10.6 | ||
| Weight (kg) | 0.028 * | I < III | |||
| Mean ± SD | 73.2 ± 14.6 | 65.5 ± 12.8 | 62.1 ± 10.6 | ||
| BMI (kg/m2) | 0.564 | ||||
| Mean ± SD | 27.3 ± 4.1 | 27.1 ± 4.0 | 26.0 ± 3.7 | ||
| Side | 0.594 | ||||
| Right, n (%) | 20 (55.6%) | 5 (29.4%) | 11 (50.0%) | ||
| Left, n (%) | 16 (44.4%) | 12 (70.6%) | 11 (50.0%) | ||
| OA grade (KL) | 0.000 * | ||||
| KL 0, n (%) | 4 (11.1%) | 0 (0%) | 0 (0%) | ||
| KL 1, n (%) | 10 (27.8%) | 1 (5.9%) | 0 (0%) | ||
| KL 2, n (%) | 9 (25.0%) | 1 (5.9%) | 0 (0%) | ||
| KL 3, n (%) | 2 (5.6%) | 1 (5.9%) | 2 (9.1%) | ||
| KL 4, n (%) | 11 (30.6%) | 14 (82.4%) | 20 (90.9%) |
| Group I (n = 36) Normal Alignment | Group II (n = 17) Mild Varus Alignment | Group III (n = 22) Severe Varus Alignment | p-Value | ||
|---|---|---|---|---|---|
| RF | 10.86 ± 2.12 | 9.92 ± 2.17 | 10.90 ± 1.86 | 0.251 | |
| VI | 31.88 ± 3.71 | 33.05 ± 2.62 | 34.27 ± 4.21 | 0.058 | |
| VM | 22.31 ± 3.22 | 21.96 ± 3.00 | 22.04 ± 2.70 | 0.907 | |
| VL | 34.94 ± 3.67 | 35.06 ± 3.00 | 32.78 ± 2.14 | 0.027 * | I, II > III |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bae, K.-C.; Son, E.-S.; Yon, C.-J.; Park, J.; Kim, D.-H. Assessment of Quadriceps Muscle in Advanced Knee Osteoarthritis and Correlation with Lower Limb Alignment. Medicina 2024, 60, 1983. https://doi.org/10.3390/medicina60121983
Bae K-C, Son E-S, Yon C-J, Park J, Kim D-H. Assessment of Quadriceps Muscle in Advanced Knee Osteoarthritis and Correlation with Lower Limb Alignment. Medicina. 2024; 60(12):1983. https://doi.org/10.3390/medicina60121983
Chicago/Turabian StyleBae, Ki-Cheor, Eun-Seok Son, Chang-Jin Yon, Jubin Park, and Du-Han Kim. 2024. "Assessment of Quadriceps Muscle in Advanced Knee Osteoarthritis and Correlation with Lower Limb Alignment" Medicina 60, no. 12: 1983. https://doi.org/10.3390/medicina60121983
APA StyleBae, K.-C., Son, E.-S., Yon, C.-J., Park, J., & Kim, D.-H. (2024). Assessment of Quadriceps Muscle in Advanced Knee Osteoarthritis and Correlation with Lower Limb Alignment. Medicina, 60(12), 1983. https://doi.org/10.3390/medicina60121983







