Mid-Thoracic Vertebral Compression Fracture after Mini-Trampoline Exercise: A Case Series of Seven Patients
Abstract
:1. Introduction
2. Patients and Methods
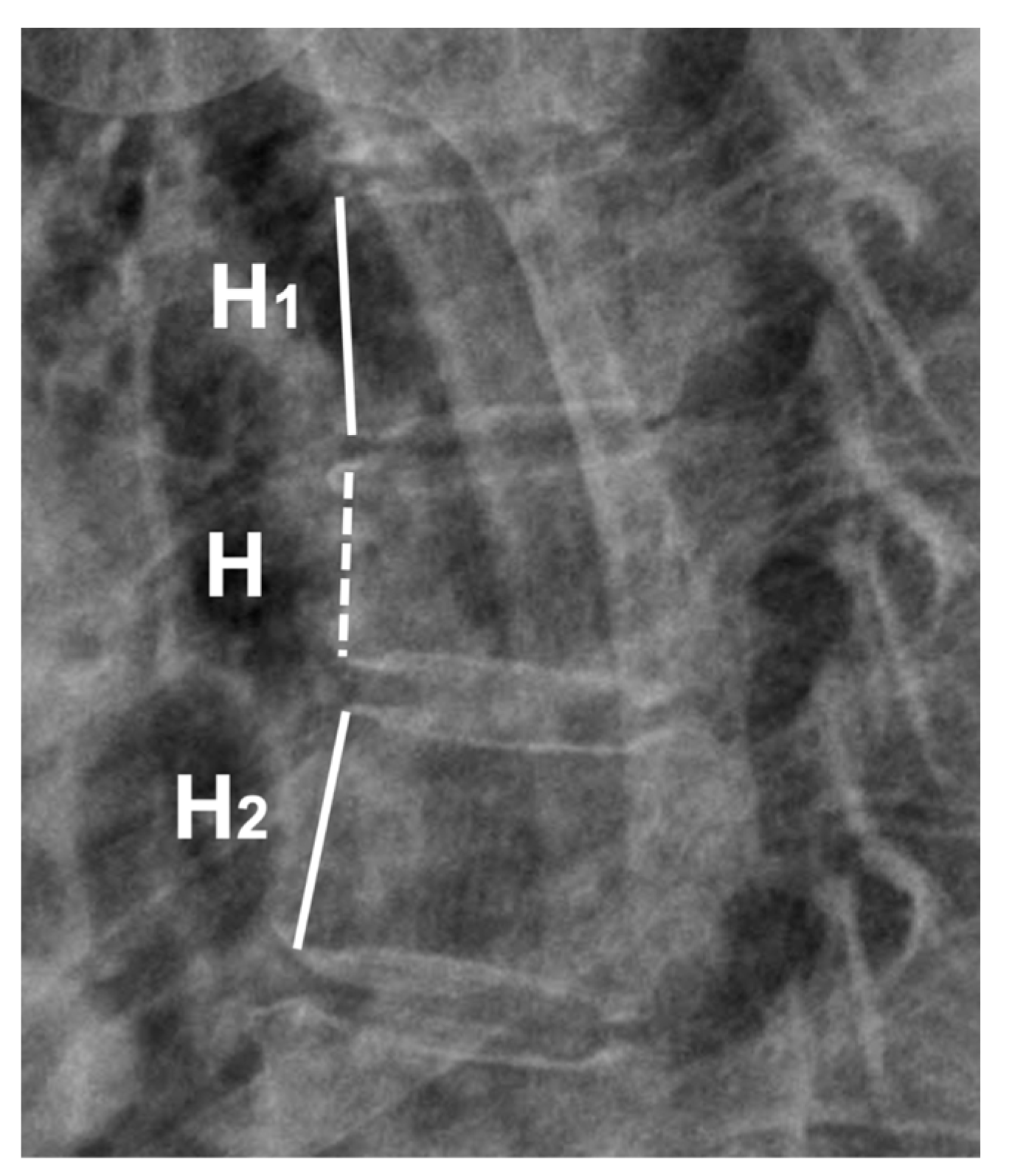
2.1. Data Collection and Radiographic Measurement: Anterior Body Compression Percentage
2.2. Statistical Analysis
3. Results
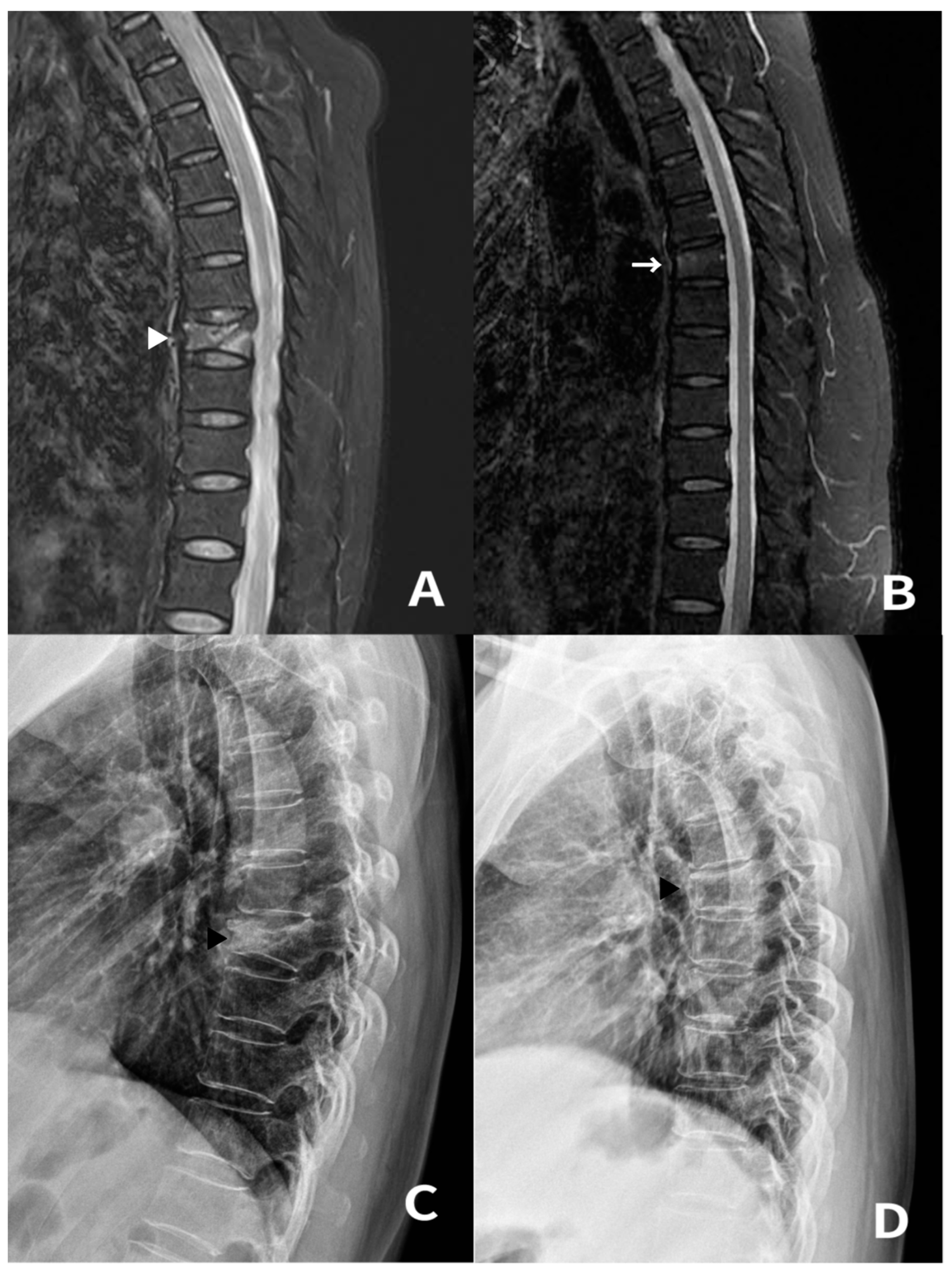
3.1. Case 1 and 2
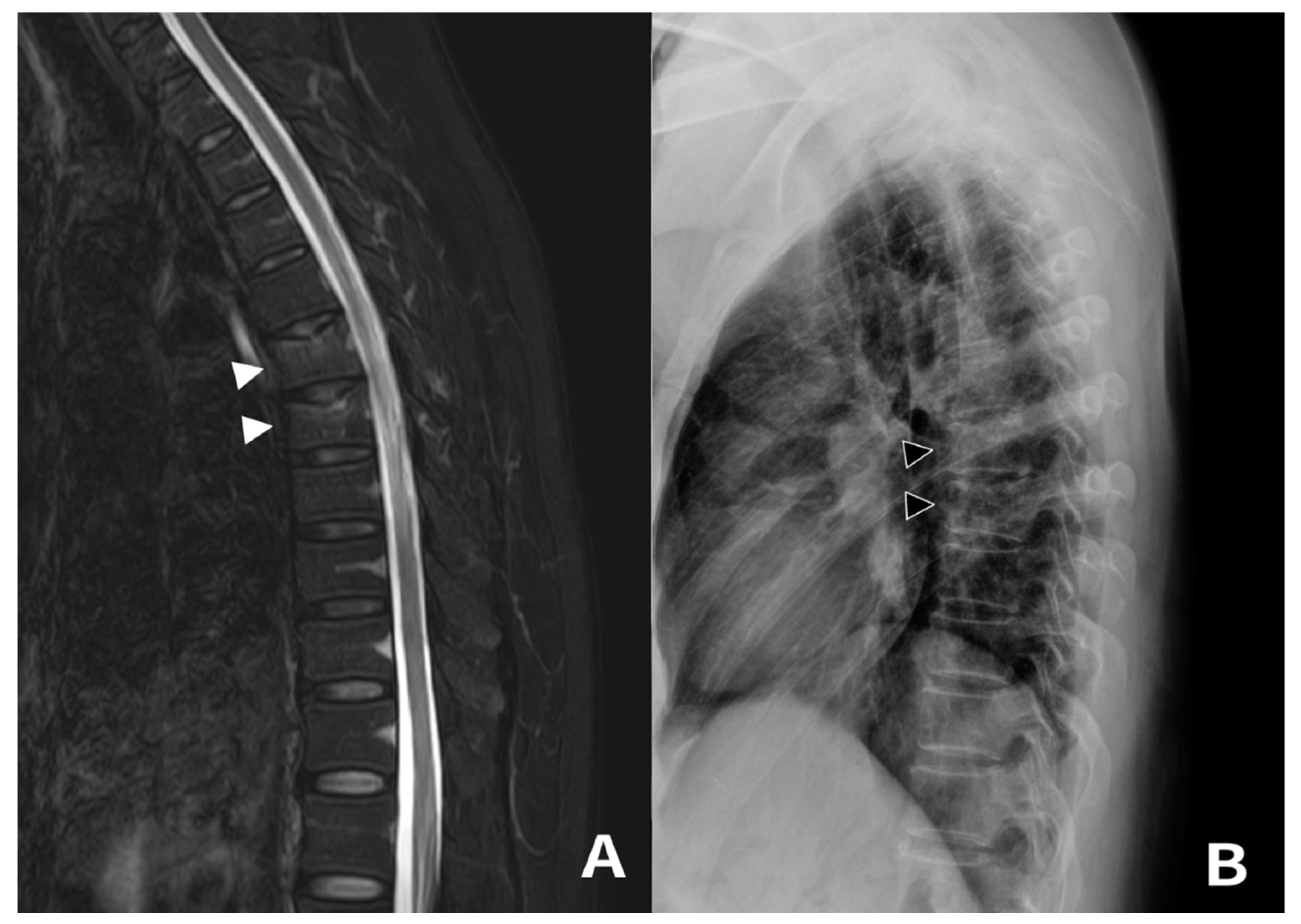
3.2. Case 3
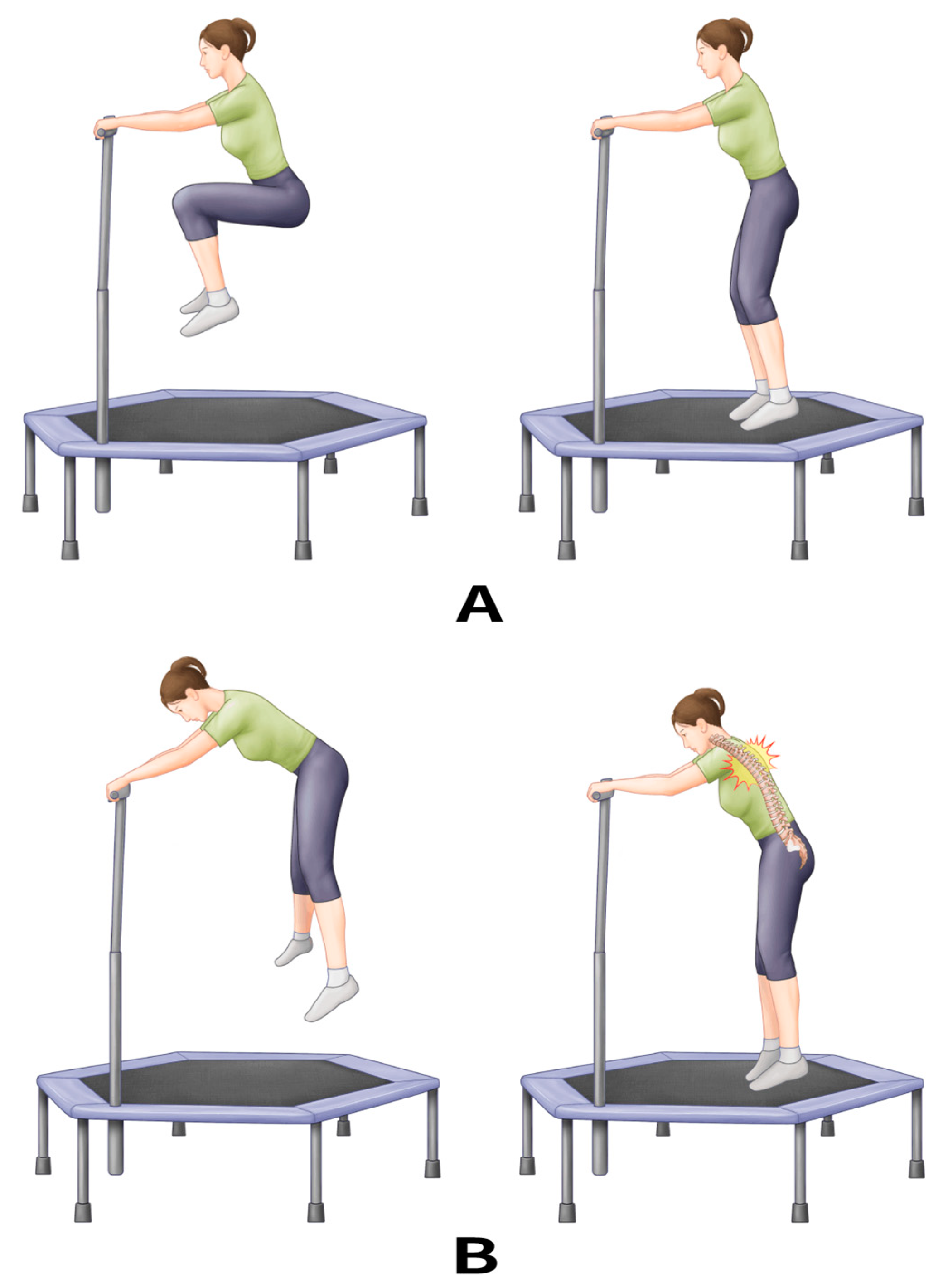
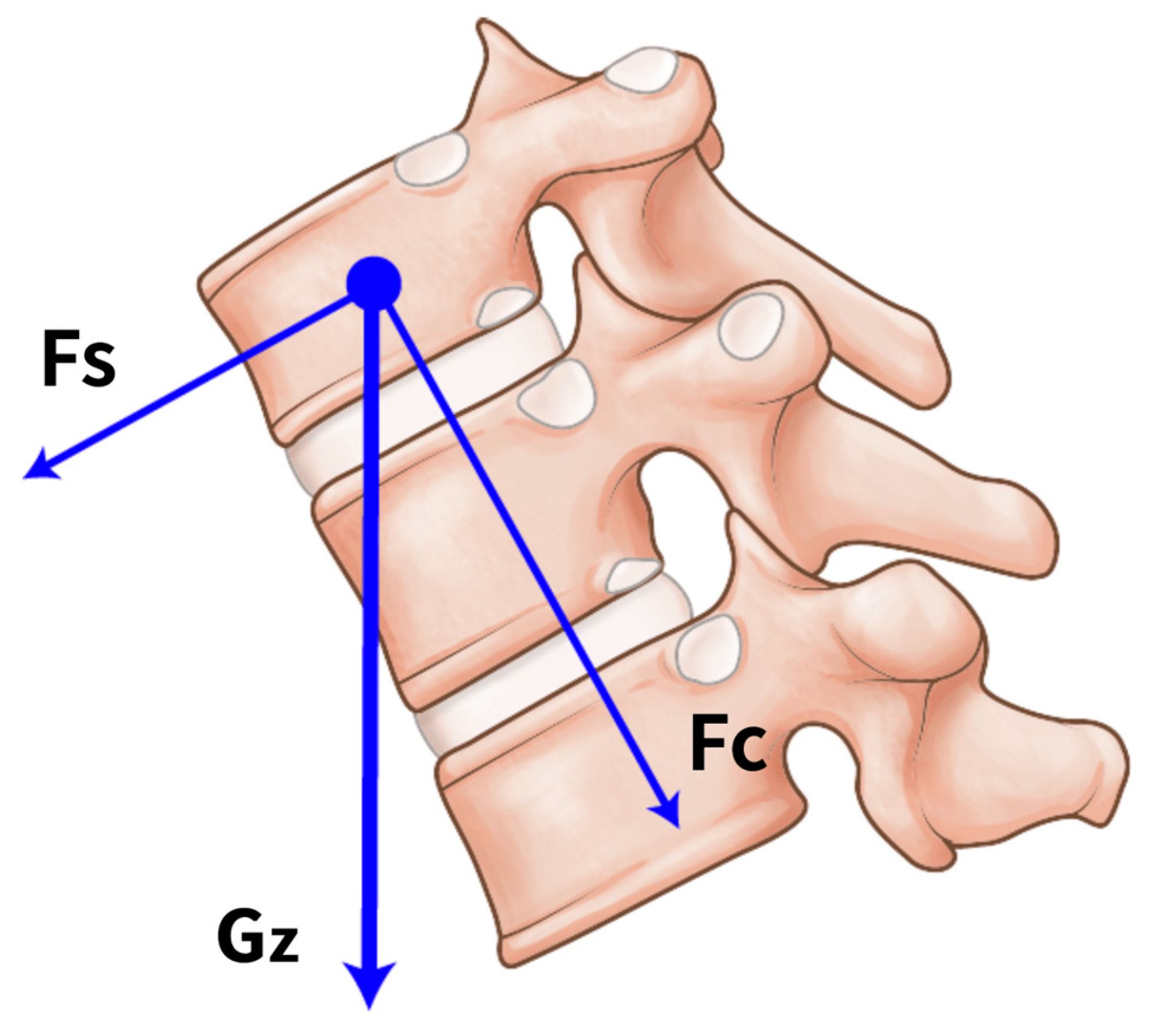
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chekroud, S.R.; Gueorguieva, R.; Zheutlin, A.B.; Paulus, M.; Krumholz, H.M.; Krystal, J.H.; Chekroud, A.M. Association between physical exercise and mental health in 1·2 million individuals in the USA between 2011 and 2015: A cross-sectional study. Lancet Psychiatry 2018, 5, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Christensen, U.; Støvring, N.; Schultz-Larsen, K.; Schroll, M.; Avlund, K. Functional ability at age 75: Is there an impact of physical inactivity from middle age to early old age? Scand. J. Med. Sci. Sports 2006, 16, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.-Y.; Song, K.-S.; Cho, J.H.; Lee, J.H.; Kim, N.H. An updated overview of low back pain management. Asian Spine J. 2022, 16, 968–982. [Google Scholar] [CrossRef] [PubMed]
- Hourigan, S.R.; Nitz, J.C.; Brauer, S.G.; O’Neill, S.; Wong, J.; Richardson, C.A. Positive effects of exercise on falls and fracture risk in osteopenic women. Osteoporos. Int. 2008, 19, 1077–1186. [Google Scholar] [CrossRef]
- Madureira, M.M.; Takayama, L.; Gallinaro, A.; Caparbo, V.F.; Costa, R.A.; Pereira, R.M.R. Balance training program is highly effective in improving functional status and reducing the risk of falls in elderly women with osteoporosis: A randomized controlled trial. Osteoporos. Int. 2007, 18, 419–425. [Google Scholar] [CrossRef]
- Eigenschenk, B.; Thomann, A.; McClure, M.; Davies, L.; Gregory, M.; Dettweiler, U.; Inglés, E. Benefits of outdoor sports for society. A systematic literature review and reflections on evidence. Int. J. Environ. Res. Public Health 2019, 16, 937. [Google Scholar] [CrossRef]
- An, H.-Y.; Chen, W.; Wang, C.-W.; Yang, H.-F.; Huang, W.-T.; Fan, S.-Y. The relationships between physical activity and life satisfaction and happiness among young, middle-aged, and older adults. Int. J. Environ. Res. Public Health 2020, 17, 4817. [Google Scholar] [CrossRef]
- Park, A.H.; Zhong, S.; Yang, H.; Jeong, J.; Lee, C. Impact of COVID-19 on physical activity: A rapid review. J. Glob. Health 2022, 12, 05003. [Google Scholar] [CrossRef]
- De Boer, D.R.; Hoekstra, F.; Huetink, K.I.; Hoekstra, T.; Krops, L.A.; Hettinga, F.J. Physical activity, sedentary behavior and well-being of adults with physical disabilities and/or chronic diseases during the first wave of the COVID-19 pandemic: A rapid review. Int. J. Environ. Res. Public Health 2021, 18, 6342. [Google Scholar] [CrossRef]
- Ghram, A.; Briki, W.; Mansoor, H.; Al-Mohannadi, A.S.; Lavie, C.J.; Chamari, K. Home-based exercise can be beneficial for counteracting sedentary behavior and physical inactivity during the COVID-19 pandemic in older adults. Postgrad. Med. 2021, 133, 469–480. [Google Scholar] [CrossRef]
- Posch, M.; Schranz, A.; Lener, M.; Tecklenburg, K.; Burtscher, M.; Ruedl, G.; Niedermeier, M.; Wlaschek, W. Effectiveness of a mini-trampoline training program on balance and functional mobility, gait performance, strength, fear of falling and bone mineral density in older women with osteopenia. Clin. Interv. Aging 2019, 14, 2281–2293. [Google Scholar] [CrossRef] [PubMed]
- Miklitsch, C.; Krewer, C.; Freivogel, S.; Steube, D. Effects of a predefined mini-trampoline training programme on balance, mobility and activities of daily living after stroke: A randomized controlled pilot study. Clin. Rehabil. 2013, 27, 939–947. [Google Scholar] [CrossRef] [PubMed]
- Doty, J.; Voskuil, R.; Davis, C.; Swafford, R.; Gardner, W.; Kiner, D.; Nowotarski, P. Trampoline-related injuries: A comparison of injuries sustained at commercial jump parks versus domestic home trampolines. J. Am. Acad. Orthop. Surg. 2019, 27, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Muljadi, J.A.; Chaijenkij, K.; Arirachakaran, A.; Kongtharvonskul, J. Comparative surgical risk between type of trampoline (size and place) and type of patients (age and sex) in trampoline related injury: A systematic review and indirect meta-analysis. BMC Sports Sci. Med. Rehabil. 2020, 12, 37. [Google Scholar] [CrossRef]
- Shields, B.J.; Fernandez, S.A.; Smith, G.A. Comparison of minitrampoline-and full-sized trampoline-related injuries in the United States, 1990–2002. Pediatrics 2005, 116, 96–103. [Google Scholar] [CrossRef]
- Brown, P.G.; Lee, M. Trampoline injuries of the cervical spine. Pediatr. Neurosurg. 2000, 32, 170–175. [Google Scholar] [CrossRef]
- Torg, J.S. Trampoline-induced quadriplegia. Clin. Sports Med. 1987, 6, 73–85. [Google Scholar] [CrossRef]
- Keynan, O.; Fisher, C.G.; Vaccaro, A.; Fehlings, M.G.; Oner, F.C.; Dietz, J.; Kwon, B.; Rampersaud, R.; Bono, C.; France, J.; et al. Radiographic measurement parameters in thoracolumbar fractures: A systematic review and consensus statement of the spine trauma study group. Spine 2006, 31, E156–E165. [Google Scholar] [CrossRef]
- Nam, D.C.; Hwang, S.C.; Lee, E.C.; Song, M.-G.; Yoo, J.-I. Femoral neck stress fractures after trampoline exercise: A case report. World J. Clin. Cases 2021, 9, 4783–4788. [Google Scholar] [CrossRef]
- Ashby, K.; Pointer, S.; Eager, D.; Day, L. Australian trampoline injury patterns and trends. Aust. N. Z. J. Public Health 2015, 39, 491–494. [Google Scholar] [CrossRef]
- Cugusi, L.; Manca, A.; Serpe, R.; Romita, G.; Bergamin, M.; Cadeddu, C.; Solla, P.; Mercuro, G. Effects of a mini-trampoline rebounding exercise program on functional parameters, body composition and quality of life in overweight women. J. Sports Med. Phys. Fit. 2016, 58, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Nuhu, J.M.; Maharaj, S.S. Influence of a mini-trampoline rebound exercise program on insulin resistance, lipid profile and central obesity in individuals with type 2 diabetes. J. Sports Med. Phys. Fit. 2017, 58, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Forwood, M.R.; Larsen, J.A. Exercise recommendations for osteoporosis: A position statement of the Australian and New Zealand Bone and Mineral Society. Aust. Fam. Physician 2000, 29, 761–764. [Google Scholar] [PubMed]
- Kasmire, K.E.; Rogers, S.C.; Sturm, J.J. Trampoline park and home trampoline injuries. Pediatrics 2016, 138, e20161236. [Google Scholar] [CrossRef]
- Gehlbach, S.H.; Bigelow, C.; Heimisdottir, M.; May, S.; Walker, M.; Kirkwood, J.R. Recognition of vertebral fracture in a clinical setting. Osteoporos. Int. 2000, 11, 577–582. [Google Scholar] [CrossRef]
- Lenchik, L.; Rogers, L.F.; Delmas, P.D.; Genant, H.K. Diagnosis of osteoporotic vertebral fractures: Importance of recognition and description by radiologists. Am. J. Roentgenol. 2004, 183, 949–958. [Google Scholar] [CrossRef]
- Farley, C.T.; Houdijk, H.H.; Van Strien, C.; Louie, M. Mechanism of leg stiffness adjustment for hopping on surfaces of different stiffnesses. J. Appl. Physiol. 1998, 85, 1044–1055. [Google Scholar] [CrossRef]
- Beerse, M.; Wu, J. Coordination dynamics of hopping on a mini-trampoline in adults and children. Gait Posture 2021, 84, 175–181. [Google Scholar] [CrossRef]
| Patient | Age | Sex | Height (cm) | Weight (kg) | BMI (kg/m2) | T-Score | Pain Onset (Weeks) | MTE Duration (min) | Fracture Location | AVCP (%) | VAS | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Initial | Last | |||||||||||
| 1 | 65 | F | 161 | 61.3 | 23.65 | −2.1 | 4 | 45 | T8 | 26.06 | 7 | 1 |
| 2 | 63 | F | 159 | 79.7 | 31.53 | −1.3 | 4 | 45 | T6 | 15.11 | 7 | 1 |
| 3 | 60 | M | 166 | 67.8 | 24.60 | −2.6 | 2 | 60 | T8 | 9.04 | 8 | 1 |
| 4 | 64 | F | 158 | 60.3 | 24.15 | −2.2 | 1 | 45 | T8 | 10.00 | 7 | 2 |
| 5 | 70 | F | 158 | 57.4 | 22.99 | −3.1 | 2 | 30 | T7 | 13.07 | 7 | 2 |
| 6 | 53 | F | 164 | 55.2 | 20.52 | −2.6 | 3 | 30 | T6 | 16.39 | 6 | 2 |
| T7 | 19.94 | |||||||||||
| 7 | 65 | F | 161 | 61.2 | 23.61 | −2.5 | 2 | 30 | T5 | 14.83 | 6 | 1 |
| T6 | 11.95 | |||||||||||
| T8 | 11.28 | |||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.C.; Kim, H.-B.; Chung, H.-J.; Yang, J.H.; Kang, M.-S. Mid-Thoracic Vertebral Compression Fracture after Mini-Trampoline Exercise: A Case Series of Seven Patients. Medicina 2023, 59, 1529. https://doi.org/10.3390/medicina59091529
Park SC, Kim H-B, Chung H-J, Yang JH, Kang M-S. Mid-Thoracic Vertebral Compression Fracture after Mini-Trampoline Exercise: A Case Series of Seven Patients. Medicina. 2023; 59(9):1529. https://doi.org/10.3390/medicina59091529
Chicago/Turabian StylePark, Sung Cheol, Hyoung-Bok Kim, Hoon-Jae Chung, Jae Hyuk Yang, and Min-Seok Kang. 2023. "Mid-Thoracic Vertebral Compression Fracture after Mini-Trampoline Exercise: A Case Series of Seven Patients" Medicina 59, no. 9: 1529. https://doi.org/10.3390/medicina59091529
APA StylePark, S. C., Kim, H.-B., Chung, H.-J., Yang, J. H., & Kang, M.-S. (2023). Mid-Thoracic Vertebral Compression Fracture after Mini-Trampoline Exercise: A Case Series of Seven Patients. Medicina, 59(9), 1529. https://doi.org/10.3390/medicina59091529






