Effects of Complex Pain Control Programs on Taekwondo Athletes with Recurrent Low Back Pain: A Case Study
Abstract
1. Introduction
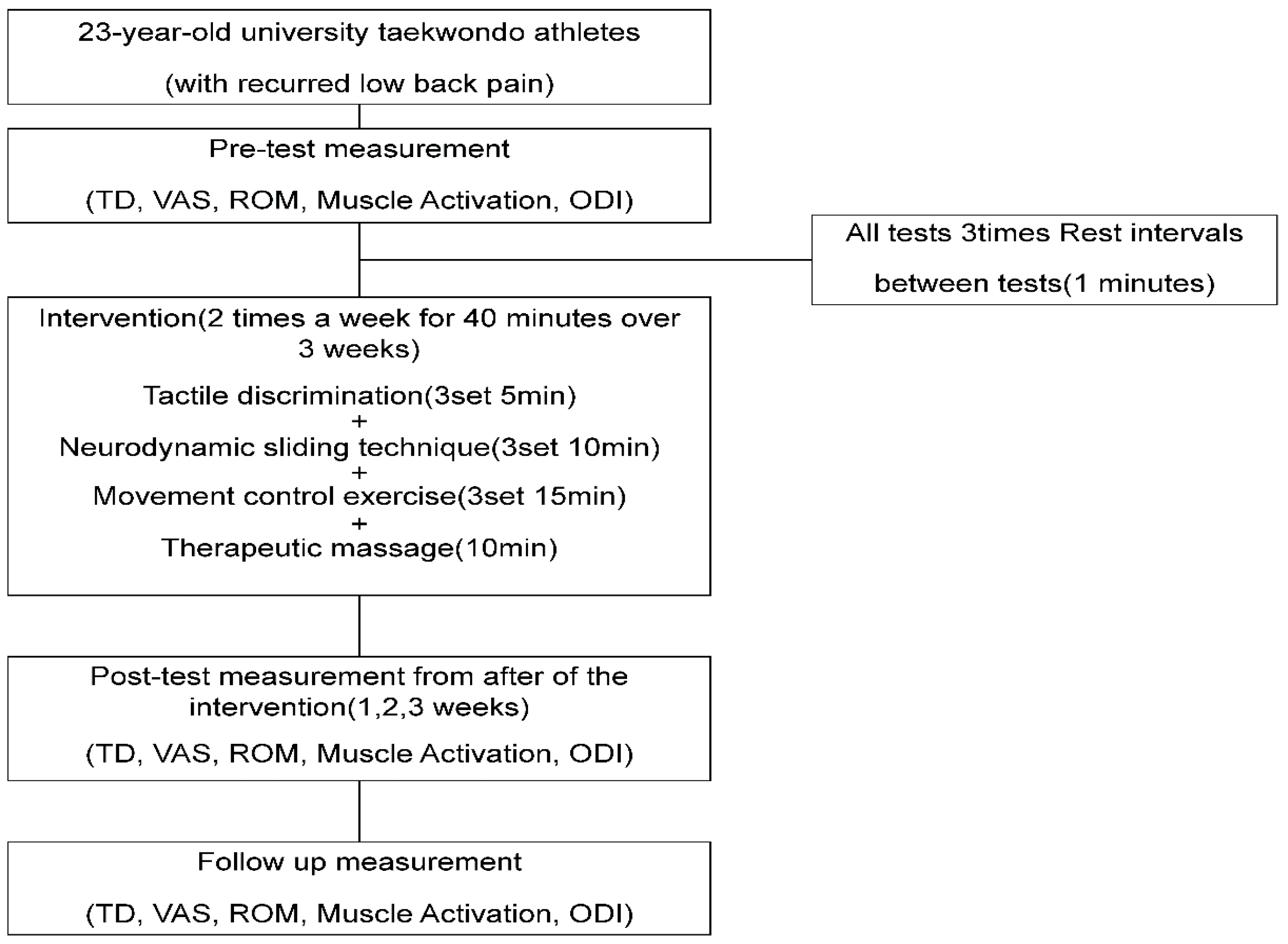
2. Materials and Methods
2.1. Patient Characteristics
2.2. Procedures
2.3. Measurement Methods
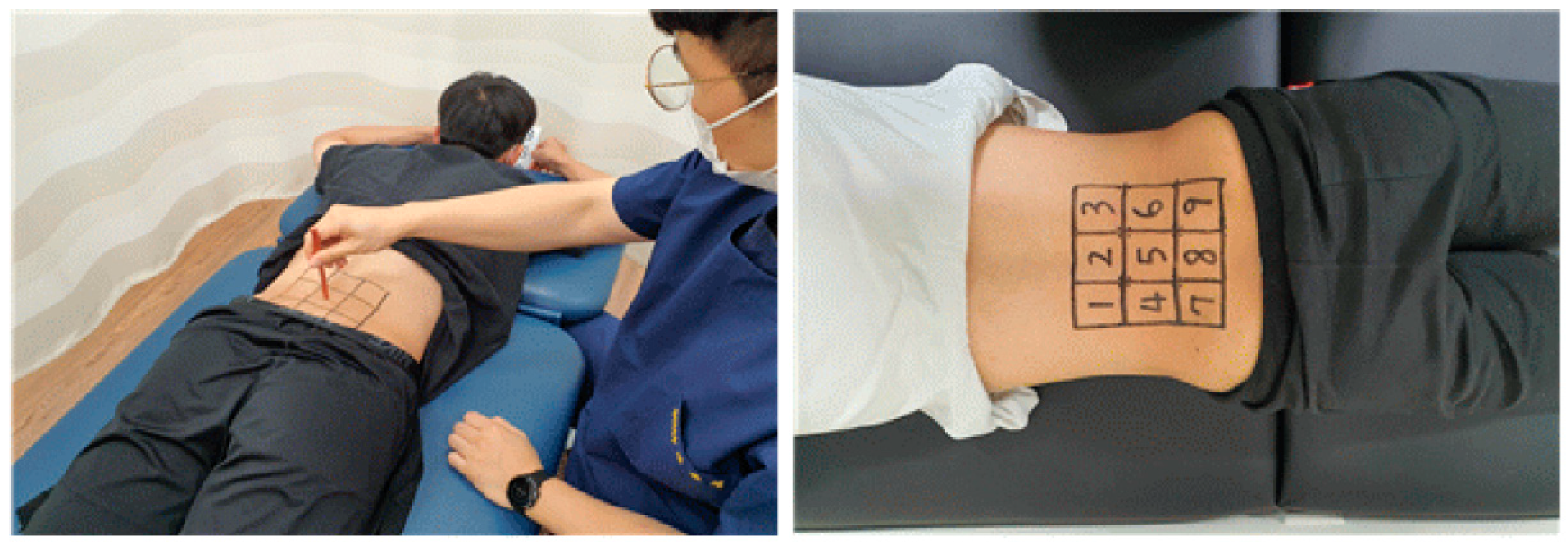
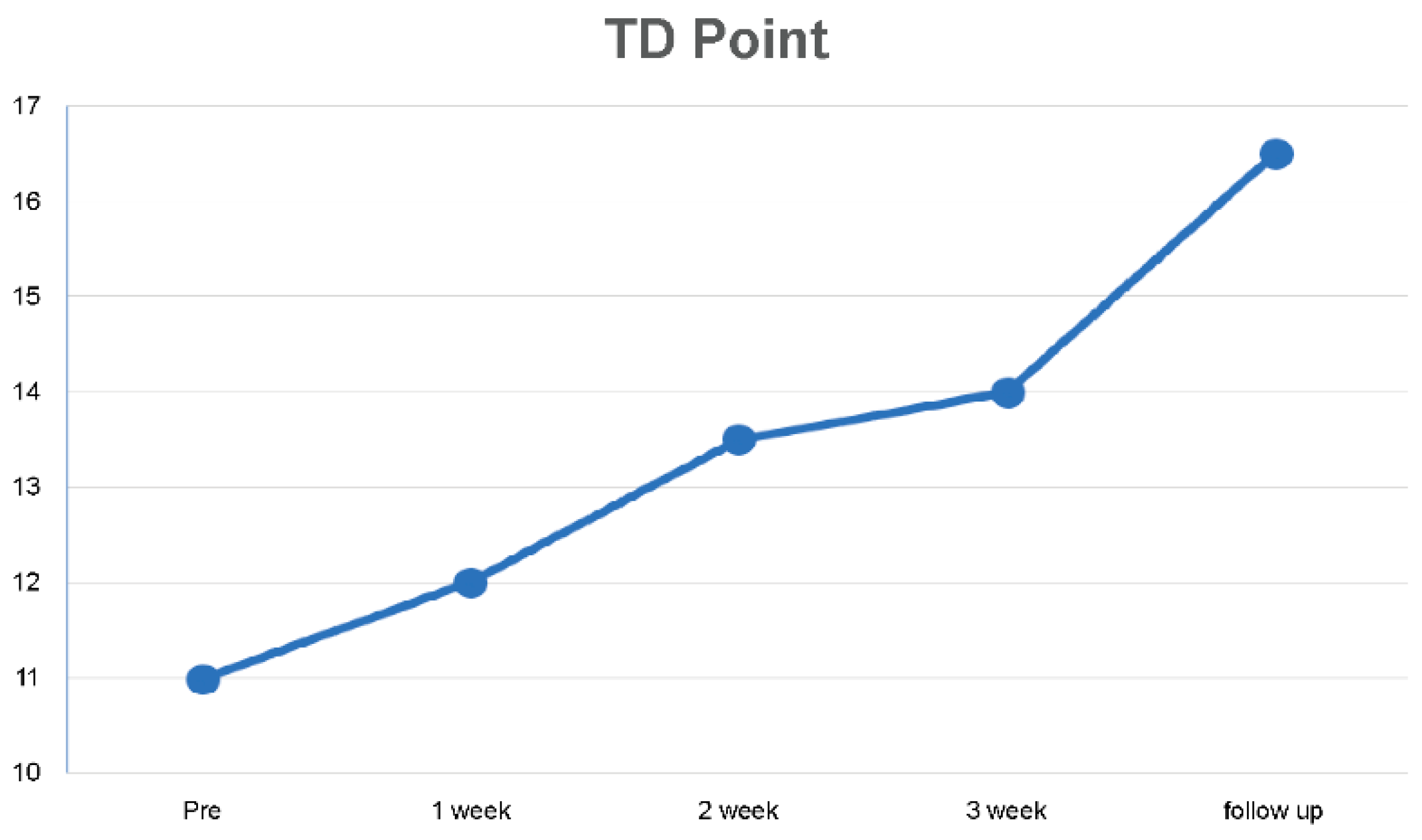
2.3.1. Tactile Discrimination
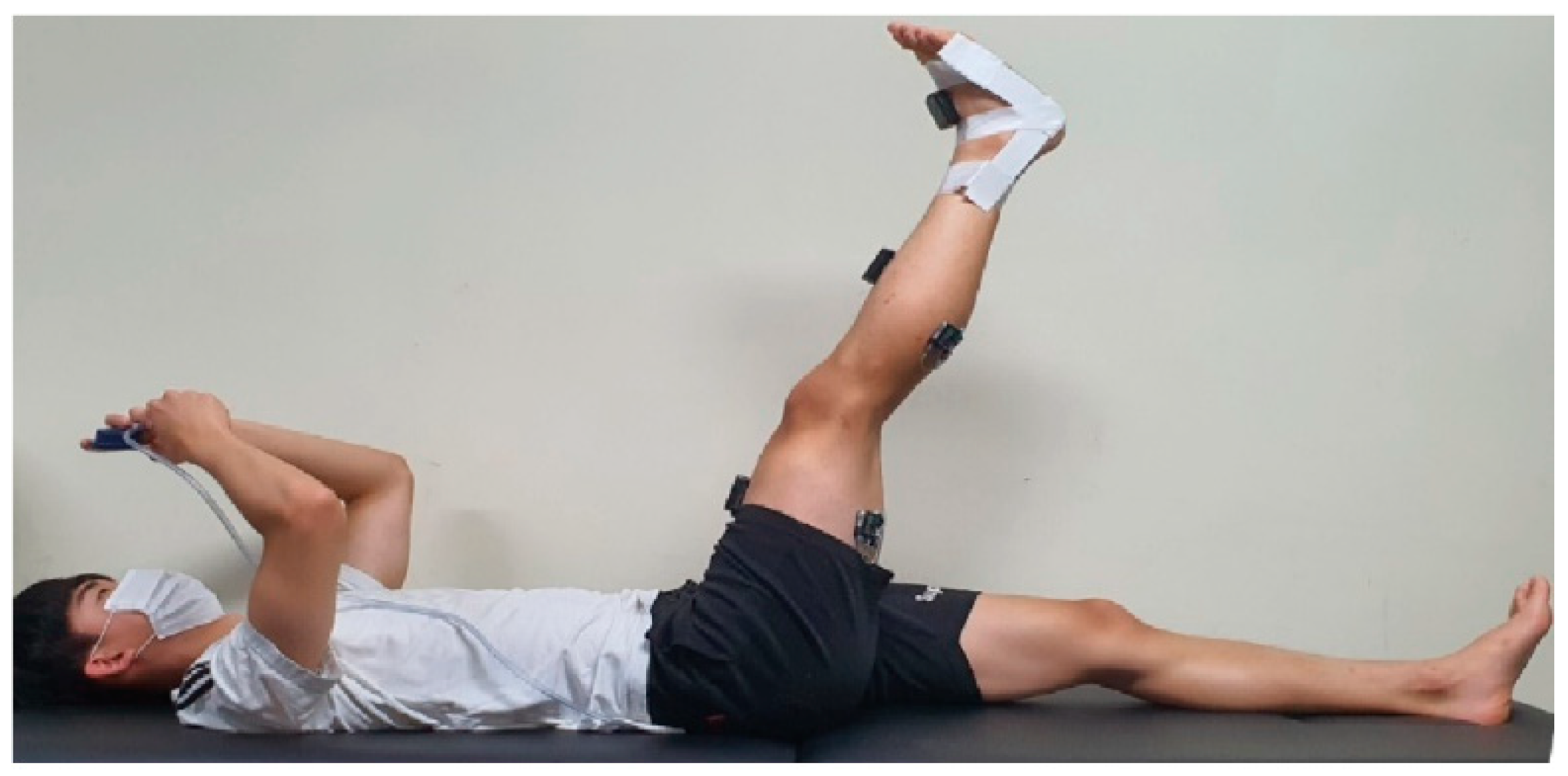
2.3.2. Mechanosensitivity
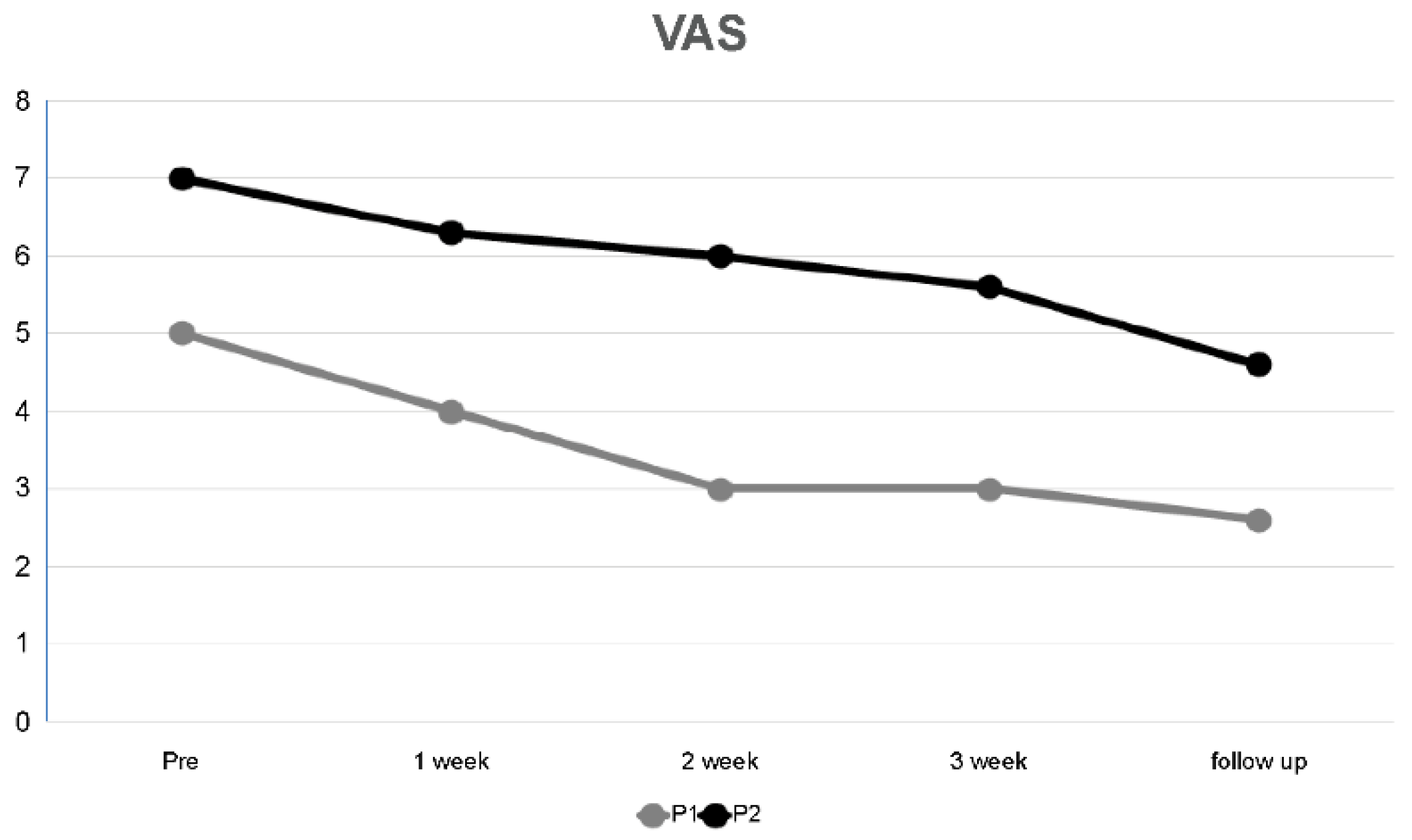
Visual Analogue Scale
Muscle Activation
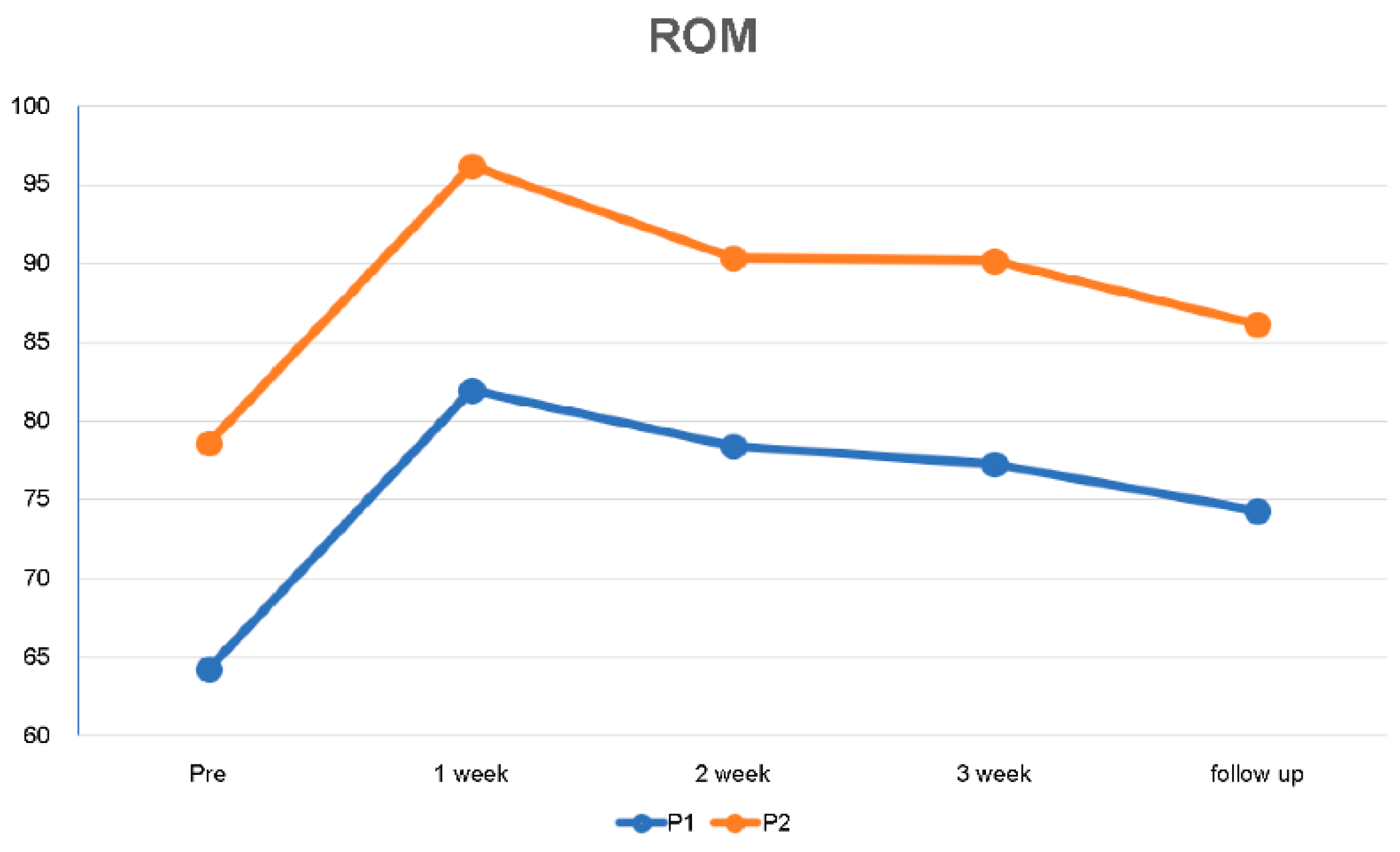
Range of Motion
2.3.3. Oswestry Disability Index
2.4. Intervention
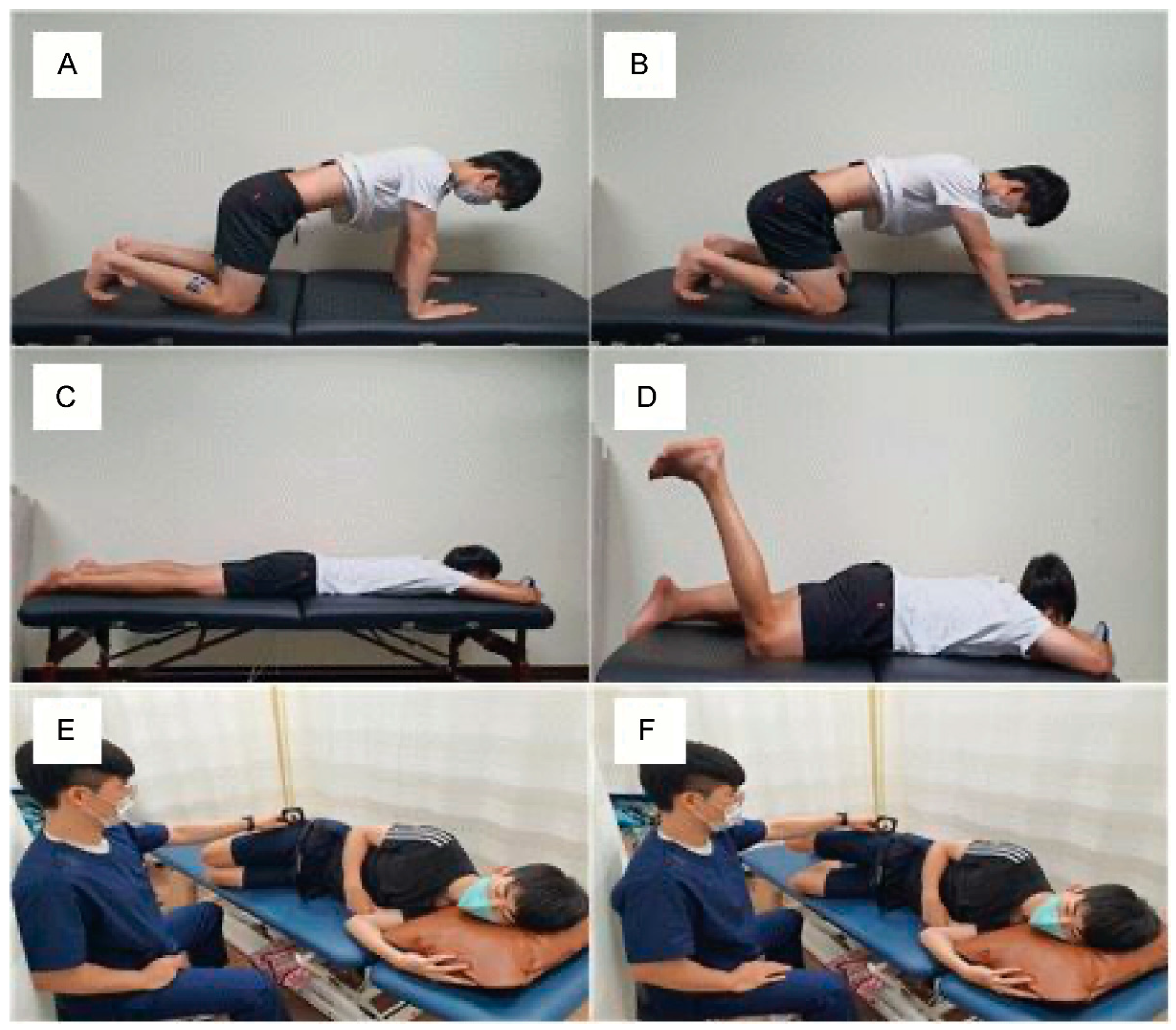
2.4.1. Tactile Discrimination Training
2.4.2. Neurodynamic Exercise
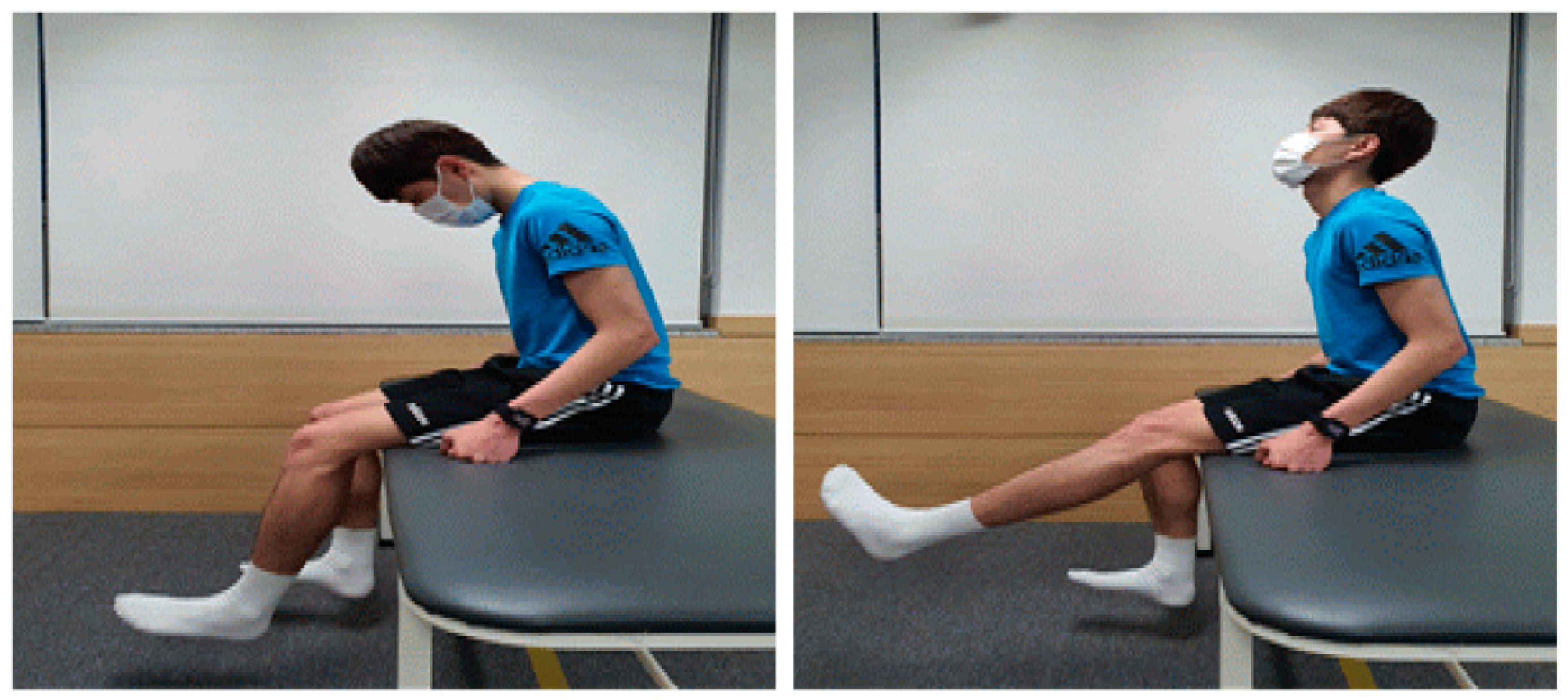
2.4.3. Movement Control Exercise
2.4.4. Therapeutic Massage and Stretching
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Patel, D.R.; Kinsella, E. Evaluation and management of lower back pain in young athletes. Transl. Pediatr. 2017, 6, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Bono, C.M. Low-Back Pain in Athletes. J. Bone Jt. Surg. 2004, 86, 382–396. [Google Scholar] [CrossRef]
- Chimenti, R.L.; Frey-Law, L.A.; Sluka, K.A. A Mechanism-Based Approach to Physical Therapist Management of Pain. Phys. Ther. 2018, 98, 302–314. [Google Scholar] [CrossRef] [PubMed]
- Ahn, J.D.; Hong, S.H.; Kil Park, Y. The Historical and Cultural Identity of Taekwondo as a Traditional Korean Martial Art. Int. J. Hist. Sport 2009, 26, 1716–1734. [Google Scholar] [CrossRef]
- Moenig, U. Taekwondo: From a Martial Art to a Martial Sport; Routledge: London, UK; New York, NY, USA, 2015. [Google Scholar]
- Zhao, R.T.; Kandil, A.; Nguyen, D.V.; Campos, L.; Amin, N.H.; Chang, E.Y. Pain perception in Taekwondo: Relationship to injury, experience, and time loss. Sport. Med. Int. Open 2020, 4, E53–E58. [Google Scholar]
- Kazemi, M.; Pieter, W. Injuries at a Canadian National Taekwondo Championships: A prospective study. BMC Musculoskelet. Disord. 2004, 5, 22. [Google Scholar] [CrossRef]
- Rabiei, P.; Namin, B.G.; Nasermelli, M.H.; Marjomaki, O.; Mazloum, V. The Effects of Functional Training on Pain, Function, and Performance in Taekwondo Players with Mechanical Low Back Pain. Health 2017, 09, 1176–1189. [Google Scholar] [CrossRef]
- Brukner, P.; Khan, K. Clinical Sports Medicine; McGraw-Hill: Haymarket, Australia, 2009. [Google Scholar]
- Ji, M. Analysis of injuries in taekwondo athletes. J. Phys. Ther. Sci. 2016, 28, 231–234. [Google Scholar] [CrossRef]
- Błach, W.; Klimek, B.; Rydzik, Ł.; Ruzbarsky, P.; Czarny, W.; Raś, I.; Ambroży, T. Nonspecific Low Back Pain among Kyokushin Karate Practitioners. Medicina 2020, 57, 27. [Google Scholar] [CrossRef]
- Kell, R.T.; Risi, A.D.; Barden, J.M. The Response of Persons With Chronic Nonspecific Low Back Pain to Three Different Volumes of Periodized Musculoskeletal Rehabilitation. J. Strength Cond. Res. 2011, 25, 1052–1064. [Google Scholar] [CrossRef]
- O’sullivan, P. Diagnosis and classification of chronic low back pain disorders: Maladaptive movement and motor control impairments as underlying mechanism. Man. Ther. 2005, 10, 242–255. [Google Scholar] [CrossRef] [PubMed]
- Thornton, J.S.; Caneiro, J.P.; Hartvigsen, J.; Ardern, C.L.; Vinther, A.; Wilkie, K.; Trease, L.; Ackerman, K.A.; Dane, K.; McDonnell, S.-J.; et al. Treating low back pain in athletes: A systematic review with meta-analysis. Br. J. Sport. Med. 2020, 55, 656–662. [Google Scholar] [CrossRef]
- Trainor, T.J.; Trainor, M.A. Etiology of Low Back Pain in Athletes. Curr. Sport. Med. Rep. 2004, 3, 41–46. [Google Scholar] [CrossRef]
- Gutknecht, M.; Mannig, A.; Waldvogel, A.; Wand, B.M.; Luomajoki, H. The effect of motor control and tactile acuity training on patients with non-specific low back pain and movement control impairment. J. Bodyw. Mov. Ther. 2014, 19, 722–731. [Google Scholar] [CrossRef]
- Nam, T.S.; Choi, Y.; Yeon, D.S.; Leem, J.W.; Paik, K.S. Differential antinociceptive effect of transcutaneous electrical stimulation on pain behavior sensitive or insensitive to phentolamine in neuropathic rats. Neurosci. Lett. 2001, 301, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Herrington, L. Effect of Different Neurodynamic Mobilization Techniques on Knee Extension Range of Motion in the Slump Position. J. Man. Manip. Ther. 2006, 14, 101–107. [Google Scholar] [CrossRef]
- Malfliet, A.; Ickmans, K.; Huysmans, E.; Coppieters, I.; Willaert, W.; Van Bogaert, W.; Rheel, E.; Bilterys, T.; Van Wilgen, P.; Nijs, J. Best Evidence Rehabilitation for Chronic Pain Part 3: Low Back Pain. J. Clin. Med. 2019, 8, 1063. [Google Scholar] [CrossRef]
- Wolny, T.; Saulicz, E.; Linek, P.; Myśliwiec, A.; Saulicz, M. Effect of manual therapy and neurodynamic techniques vs ultrasound and laser on 2PD in patients with CTS: A randomized controlled trial. J. Hand Ther. 2016, 29, 235–245. [Google Scholar] [CrossRef]
- Dworkin, R.H.; O’Connor, A.B.; Backonja, M.; Farrar, J.T.; Finnerup, N.B.; Jensen, T.S.; Kalso, E.A.; Loeser, J.D.; Miaskowski, C.; Nurmikko, T.J.; et al. Pharmacologic management of neuropathic pain: Evidence-based recommendations. Pain 2007, 132, 237–251. [Google Scholar] [CrossRef]
- Adriaan Louw, P.T.; Kevin Farrell, P.T.; Lauren Wettach PT, D.P.T.; Justine Uhl PT, D.P.T.; Katherine Majkowski PT, D.P.T.; Marcus Welding PT, D.P.T. Immediate effects of sensory discrimination for chronic low back pain: A case series. N. Z. J Physiother. 2015, 43, 58. [Google Scholar]
- Boyd, B.S.; Wanek, L.; Gray, A.T.; Topp, K.S. Mechanosensitivity of the Lower Extremity Nervous System During Straight-Leg Raise Neurodynamic Testing in Healthy Individuals. J. Orthop. Sport. Phys. Ther. 2009, 39, 780–790. [Google Scholar] [CrossRef]
- Criswell, E. Cram’s Introduction to Surface Electromyography; Jones and Bartlett Publishers: Burlington, MA, USA, 2010. [Google Scholar]
- Jung, J.-H.; Moon, D.-C. The effect of neurodynamic technique of tibial nerve on range of motion, pain, and mechanosensitivity of the lower extremity in healthy individuals: A preliminary study. J. Hum. Sport Exerc. 2020, 16, 956–964. [Google Scholar] [CrossRef]
- Takasaki, H.; Okubo, Y. Deep neck flexors impact rectus abdominis muscle activity during active straight leg raising. Int. J. Sport. Phys. Ther. 2020, 15, 1044–1051. [Google Scholar] [CrossRef]
- Kim, D.-Y.; Lee, S.-H.; Lee, H.-Y.; Lee, H.-J.; Chang, S.-B.; Chung, S.-K.; Kim, H.-J. Validation of the Korean Version of the Oswestry Disability Index. Spine 2005, 30, E123–E127. [Google Scholar] [CrossRef]
- Cleland, J.A.; Childs, J.D.; Palmer, J.A.; Eberhart, S. Slump stretching in the management of non-radicular low back pain: A pilot clinical trial. Man. Ther. 2006, 11, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Comerford, M.; Mottram, S. Kinetic Control-E-book: The Management of Uncontrolled Movement; Elsevier Health Sciences: Amsterdam, The Netherlands, 2011. [Google Scholar]
- França, F.R.; Burke, T.N.; Caffaro, R.R.; Ramos, L.A.; Marques, A.P. Effects of Muscular Stretching and Segmental Stabilization on Functional Disability and Pain in Patients with Chronic Low Back Pain: A Randomized, Controlled Trial. J. Manip. Physiol. Ther. 2012, 35, 279–285. [Google Scholar] [CrossRef]
- Furlan, A.D.; Giraldo, M.; Baskwill, A.; Irvin, E.; Imamura, M. Massage for low-back pain. Cochrane Database Syst. Rev. 2015, 2015, CD001929. [Google Scholar] [CrossRef]
- Bear, M.; Connors, B.; Paradiso, M.A. Neuroscience: Exploring the Brain, Enhanced Edition: Exploring the Brain; Jones and Bartlett Publishers Learning: Burlington, MA, USA, 2020. [Google Scholar]
- Berg, D.; Godau, J.; Walter, U. Transcranial sonography in movement disorders. Lancet Neurol. 2008, 7, 1044–1055. [Google Scholar] [CrossRef]
- Hodges, P.W.; Moseley, G. Pain and motor control of the lumbopelvic region: Effect and possible mechanisms. J. Electromyogr. Kinesiol. 2003, 13, 361–370. [Google Scholar] [CrossRef]
- Moseley, G.L. Graded motor imagery for pathologic pain: A randomized controlled trial. Neurology 2006, 67, 2129–2134. [Google Scholar] [CrossRef]
- Flor, H.; Braun, C.; Elbert, T.; Birbaumer, N. Extensive reorganization of primary somatosensory cortex in chronic back pain patients. Neurosci. Lett. 1997, 224, 5–8. [Google Scholar] [CrossRef] [PubMed]
- Babbage, C.S.; Coppieters, M.W.; McGowan, C.M. Strain and excursion of the sciatic nerve in the dog: Biomechanical considerations in the development of a clinical test for increased neural mechanosensitivity. Veter- J. 2007, 174, 330–336. [Google Scholar] [CrossRef]
- Shacklock, M. Clinical Neurodynamics: A New System of Neuromusculoskeletal Treatment; Elsevier Health Sciences: Amsterdam, The Netherlands, 2005. [Google Scholar]
- Lewin, G.R.; Moshourab, R. Mechanosensation and pain. J. Neurobiol. 2004, 61, 30–44. [Google Scholar] [CrossRef] [PubMed]
- Luomajoki, H.; Kool, J.; de Bruin, E.D.; Airaksinen, O. Improvement in low back movement control, decreased pain and disability, resulting from specific exercise intervention. BMC Sport. Sci. Med. Rehabil. 2010, 2, 11. [Google Scholar] [CrossRef]
- Beneciuk, J.M.; Bishop, M.D.; George, S.Z. Effects of Upper Extremity Neural Mobilization on Thermal Pain Sensitivity: A Sham-Controlled Study in Asymptomatic Participants. J. Orthop. Sport. Phys. Ther. 2009, 39, 428–438. [Google Scholar] [CrossRef]
- Coppieters, M.W.; Do Butler, D.S. ‘Sliders’ slide and “tensioners” tension? An analysis of neurodynamic techniques and considerations regarding their application. Man Ther. 2008, 13, 213–221. [Google Scholar]
- van der Heide, B.; Allison, G.; Zusman, M. Pain and muscular responses to a neural tissue provocation test in the upper limb. Man. Ther. 2001, 6, 154–162. [Google Scholar] [CrossRef]
- Roland, M.; Fairbank, J. The Roland–Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine 2000, 25, 3115–3124. [Google Scholar] [CrossRef]
- Matheve, T.; Brumagne, S.; Demoulin, C.; Timmermans, A. Sensor-based postural feedback is more effective than conventional feedback to improve lumbopelvic movement control in patients with chronic low back pain: A randomised controlled trial. J. Neuroeng. Rehabil. 2018, 15, 85. [Google Scholar] [CrossRef]
- Salamat, S.; Talebian, S.; Bagheri, H.; Maroufi, N.; Shaterzadeh, M.J.; Kalbasi, G.; O’Sullivan, K. Effect of movement control and stabilization exercises in people with extension related non -specific low back pain- a pilot study. J. Bodyw. Mov. Ther. 2017, 21, 860–865. [Google Scholar] [CrossRef]
| Variable | Mean ± SD |
|---|---|
| Age (years) | 23 |
| Height (cm) | 178 |
| Weight (kg) | 67 |
| VAS | 5 |
| ODI | 8 |
| Pre-Test | 1 Week | 2 Weeks | 3 Weeks | After 2 Weeks | |
|---|---|---|---|---|---|
| TDP | 11 | 12 | 13.5 | 14 | 16.5 |
| Pre-Test | 1 Week | 2 Weeks | 3 Weeks | After 2 Weeks | ||
|---|---|---|---|---|---|---|
| VAS | P1 | 5 | 4 | 3 | 3 | 2.6 |
| P2 | 7 | 6.3 | 6 | 5.6 | 4.6 |
| ROM | Pre-Test | 1 Week | 2 Weeks | 3 Weeks | After 2 Weeks | |
|---|---|---|---|---|---|---|
| ROM | P1 | 64.30° | 81.93° | 78.37° | 77.27° | 74.27° |
| P2 | 78.57° | 96.17° | 90.33° | 90.20° | 86.20° |
| ROM | Pre-Test | 1 Week | 2 Weeks | 3 Weeks | After 2 Weeks | |
|---|---|---|---|---|---|---|
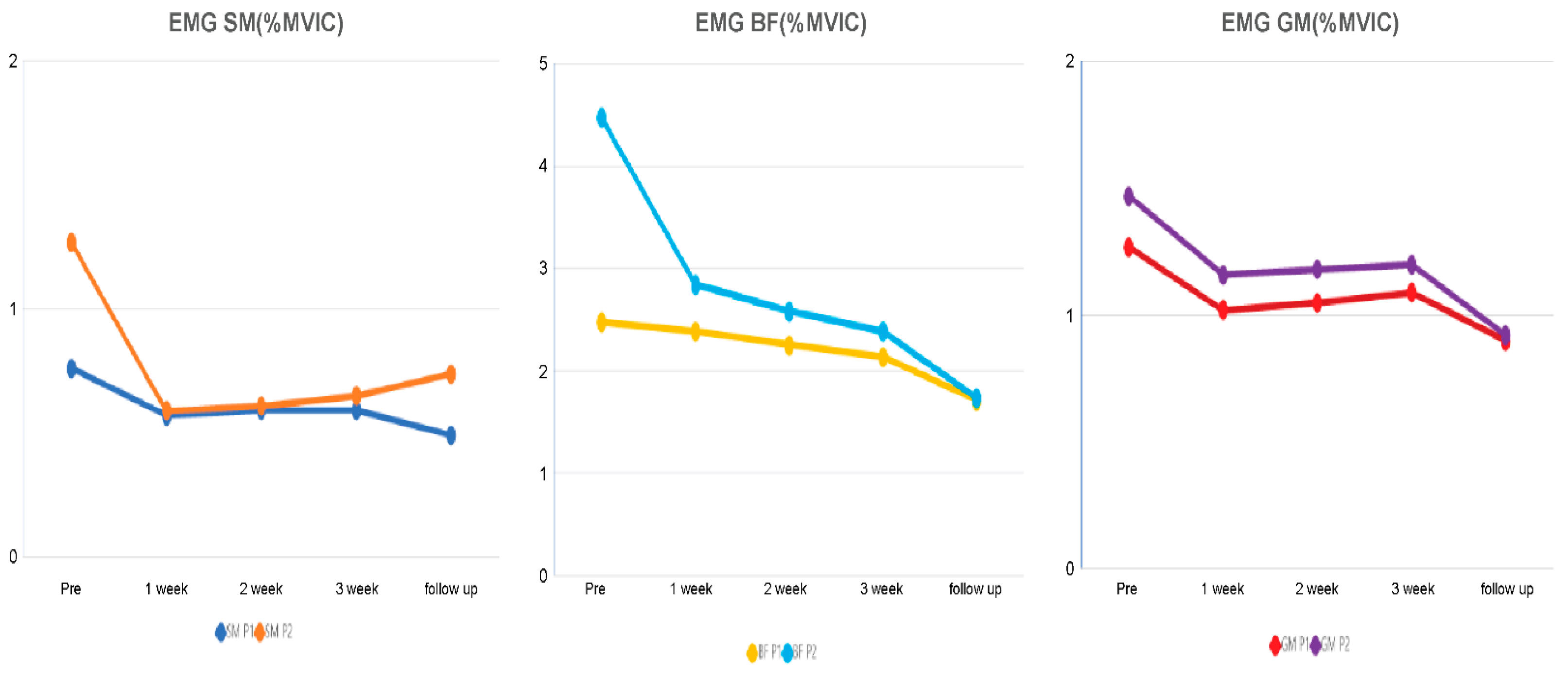
| SM (%MVIC) | P1 (64°) | 0.76 | 0.57 | 0.59 | 0.59 | 0.49 |
| P2 (78°) | 1.27 | 0.59 | 0.61 | 0.65 | 0.74 | |
| BF (%MVIC) | P1 (64°) | 2.47 | 2.38 | 2.25 | 2.13 | 1.71 |
| P2 (78°) | 4.47 | 2.28 | 2.58 | 2.38 | 1.73 | |
| GM (%MVIC) | P1 (64°) | 1.27 | 1.02 | 1.05 | 1.09 | 0.90 |
| P2 (78°) | 1.47 | 1.16 | 1.18 | 1.20 | 0.92 |
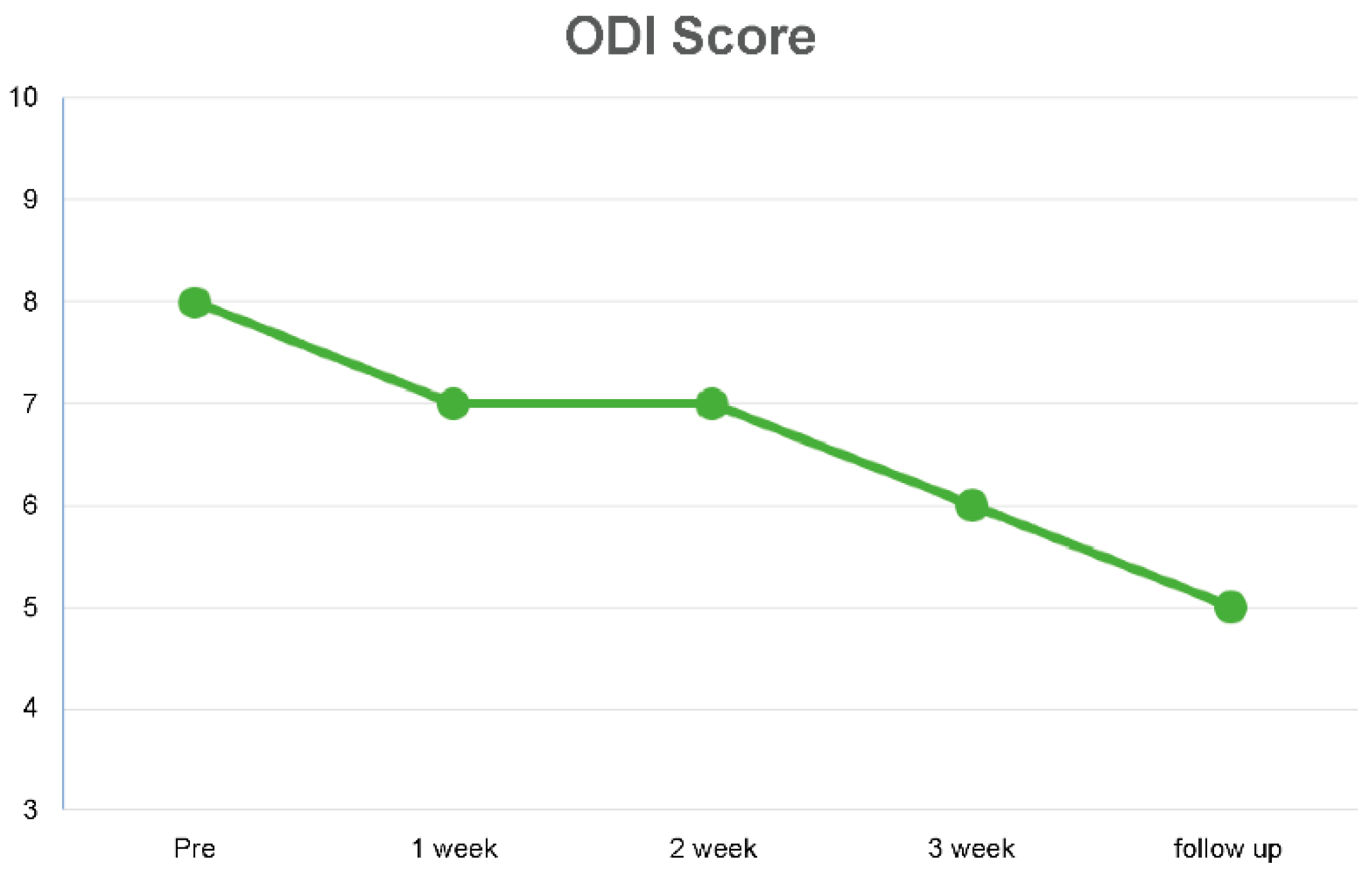
| Pre-Test | 1 Week | 2 Weeks | 3 Weeks | After 2 Weeks | |
|---|---|---|---|---|---|
| ODI score | 8 | 7 | 7 | 6 | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.-G.; Jung, J.-H.; Moon, D.-C. Effects of Complex Pain Control Programs on Taekwondo Athletes with Recurrent Low Back Pain: A Case Study. Medicina 2023, 59, 1271. https://doi.org/10.3390/medicina59071271
Kim H-G, Jung J-H, Moon D-C. Effects of Complex Pain Control Programs on Taekwondo Athletes with Recurrent Low Back Pain: A Case Study. Medicina. 2023; 59(7):1271. https://doi.org/10.3390/medicina59071271
Chicago/Turabian StyleKim, Hong-Gil, Ju-Hyeon Jung, and Dong-Chul Moon. 2023. "Effects of Complex Pain Control Programs on Taekwondo Athletes with Recurrent Low Back Pain: A Case Study" Medicina 59, no. 7: 1271. https://doi.org/10.3390/medicina59071271
APA StyleKim, H.-G., Jung, J.-H., & Moon, D.-C. (2023). Effects of Complex Pain Control Programs on Taekwondo Athletes with Recurrent Low Back Pain: A Case Study. Medicina, 59(7), 1271. https://doi.org/10.3390/medicina59071271






