Elucidating the Link: Chronic Obstructive Pulmonary Disease and the Complex Interplay of Gastroesophageal Reflux Disease and Reflux-Related Complications
Abstract
1. Introduction
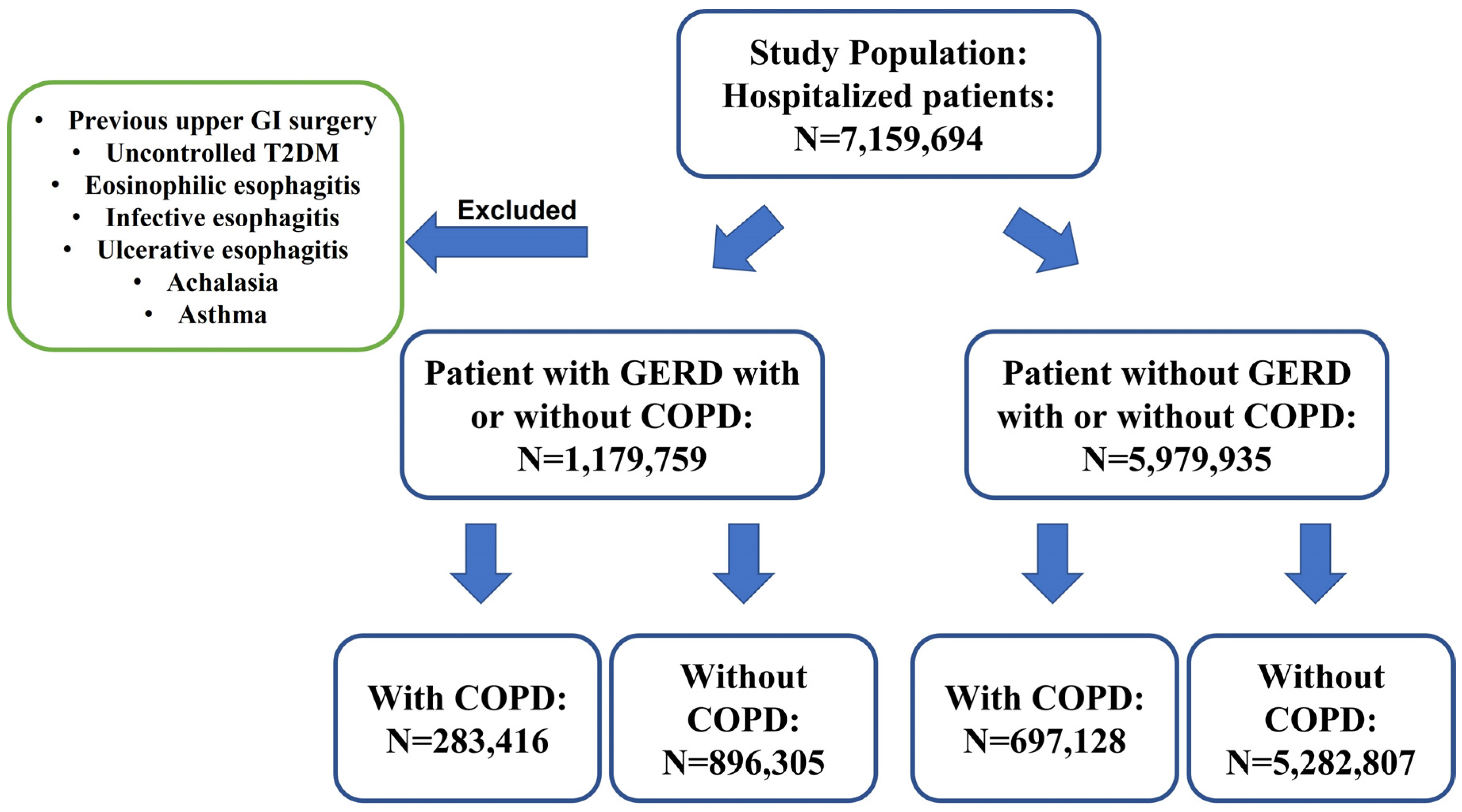
2. Materials and Methods
2.1. Database
2.2. Data Collection and Outcomes
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Katz, P.O.; Dunbar, K.B.; Schnoll-Sussman, F.H.; Greer, K.B.; Yadlapati, R.; Spechler, S.J. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am. J. Gastroenterol. 2022, 117, 27–56. [Google Scholar] [CrossRef]
- El-Serag, H.B.; Sweet, S.; Winchester, C.C.; Dent, J. Update on the epidemiology of gastro-oesophageal reflux disease: A systematic review. Gut 2014, 63, 871–880. [Google Scholar] [CrossRef] [PubMed]
- Fass, R.; Boeckxstaens, G.E.; El-Serag, H.; Rosen, R.; Sifrim, D.; Vaezi, M.F. Gastro-oesophageal reflux disease. Nat. Rev. Dis. Primers 2021, 7, 55. [Google Scholar] [CrossRef] [PubMed]
- Maret-Ouda, J.; Markar, S.R.; Lagergren, J. Gastroesophageal Reflux Disease: A Review. JAMA 2020, 324, 2536–2547. [Google Scholar] [CrossRef] [PubMed]
- Clarrett, D.M.; Hachem, C. Gastroesophageal Reflux Disease (GERD). Mo. Med. 2018, 115, 214–218. [Google Scholar] [PubMed]
- Fass, R.; Pulliam, G.; Johnson, C.; Garewal, H.S.; Sampliner, R.E. Symptom severity and oesophageal chemosensitivity to acid in older and young patients with gastro-oesophageal reflux. Age Ageing 2000, 29, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Halawani, H.; Banoon, S. Prevalence and Determinants of Gastroesophageal Reflux Disease and the Risk Factors Among Adult Patients Attending Al-Iskan Primary Health Care Center in Makkah, 2020. Cureus 2020, 12, e10535. [Google Scholar] [CrossRef] [PubMed]
- Nirwan, J.S.; Hasan, S.S.; Babar, Z.-U.-D.; Conway, B.R.; Ghori, M.U. Global Prevalence and Risk Factors of Gastro-oesophageal Reflux Disease (GORD): Systematic Review with Meta-analysis. Sci. Rep. 2020, 10, 5814. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Yang, W.-L.; Cai, M.-H.; Chen, X.; Zhao, R.; Li, M.-T.; Yan, X.-L.; Xue, L.-W.; Hong, L.; Tang, M.-Y. Burden of gastroesophageal reflux disease in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of disease study 2019. BMC Public Health 2023, 23, 582. [Google Scholar] [CrossRef]
- Eslami, O.; Shahraki, M.; Bahari, A.; Shahraki, T. Dietary habits and obesity indices in patients with gastro-esophageal reflux disease: A comparative cross-sectional study. BMC Gastroenterol. 2017, 17, 132. [Google Scholar] [CrossRef]
- Ness-Jensen, E.; Lagergren, J. Tobacco smoking, alcohol consumption and gastro-oesophageal reflux disease. Best Pract. Res. Clin. Gastroenterol. 2017, 31, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Hou, Z.K.; Huang, Z.B.; Chen, X.L.; Liu, F.B. Dietary and Lifestyle Factors Related to Gastroesophageal Reflux Disease: A Systematic Review. Ther. Clin. Risk Manag. 2021, 17, 305–323. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.E.; Shahjehan, R.D. Hiatal Hernia. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Rabe, K.F.; Watz, H. Chronic obstructive pulmonary disease. Lancet 2017, 389, 1931–1940. [Google Scholar] [CrossRef] [PubMed]
- Christenson, S.A.; Smith, B.M.; Bafadhel, M.; Putcha, N. Chronic obstructive pulmonary disease. Lancet 2022, 399, 2227–2242. [Google Scholar] [CrossRef]
- Agustí, A.; Celli, B.R.; Criner, G.J.; Halpin, D.; Anzueto, A.; Barnes, P.; Bourbeau, J.; Han, M.K.; Martinez, F.J.; Oca, M.M.D.; et al. Global Initiative for Chronic Obstructive Lung Disease 2023 Report: GOLD Executive Summary. Eur. Respir. J. 2023, 61, 2300239. [Google Scholar] [CrossRef]
- Celli, B.R.; Fabbri, L.M.; Aaron, S.D.; Agusti, A.; Brook, R.; Criner, G.J.; Franssen, F.M.E.; Humbert, M.; Hurst, J.R.; O’Donnell, D.; et al. An Updated Definition and Severity Classification of Chronic Obstructive Pulmonary Disease Exacerbations: The Rome Proposal. Am. J. Respir. Crit. Care Med. 2021, 204, 1251–1258. [Google Scholar] [CrossRef]
- Agustí, A.; Melén, E.; DeMeo, D.L.; Breyer-Kohansal, R.; Faner, R. Pathogenesis of chronic obstructive pulmonary disease: Understanding the contributions of gene-environment interactions across the lifespan. Lancet Respir. Med. 2022, 10, 512–524. [Google Scholar] [CrossRef]
- Wheaton, A.G.; Liu, Y.; Croft, J.B.; VanFrank, B.; Croxton, T.L.; Punturieri, A.; Postow, L.; Greenlund, K.J. Chronic Obstructive Pulmonary Disease and Smoking Status—United States, 2017. MMWR. Morb. Mortal. Wkly. Rep. 2019, 68, 533–538. [Google Scholar] [CrossRef]
- Hikichi, M.; Mizumura, K.; Maruoka, S.; Gon, Y. Pathogenesis of chronic obstructive pulmonary disease (COPD) induced by cigarette smoke. J. Thorac. Dis. 2019, 11, S2129–S2140. [Google Scholar] [CrossRef]
- Matteis, S.D.; Jarvis, D.; Darnton, A.; Hutchings, S.; Sadhra, S.; Fishwick, D.; Rushton, L.; Cullinan, P. The occupations at increased risk of COPD: Analysis of lifetime job-histories in the population-based UK Biobank Cohort. Eur. Respir. J. 2019, 54, 1900186. [Google Scholar] [CrossRef]
- Bourbeau, J.; Doiron, D.; Biswas, S.; Smith, B.M.; Benedetti, A.; Brook, J.R.; Aaron, S.D.; Chapman, K.R.; Hernandez, P.; Maltais, F.; et al. Ambient Air Pollution and Dysanapsis: Associations with Lung Function and Chronic Obstructive Pulmonary Disease in the Canadian Cohort Obstructive Lung Disease Study. Am. J. Respir. Crit. Care Med. 2022, 206, 44–55. [Google Scholar] [CrossRef]
- Blanco, I.; Diego, I.; Bueno, P.; Pérez-Holanda, S.; Casas-Maldonado, F.; Miravitlles, M. Prevalence of α1-antitrypsin PiZZ genotypes in patients with COPD in Europe: A systematic review. Eur. Respir. Rev. 2020, 29, 200014. [Google Scholar] [CrossRef]
- Martínez-García, M.Á.; Faner, R.; Oscullo, G.; Rosa-Carrillo, D.l.; Soler-Cataluña, J.J.; Ballester, M.; Muriel, A.; Agusti, A. Chronic Bronchial Infection Is Associated with More Rapid Lung Function Decline in Chronic Obstructive Pulmonary Disease. Ann. Am. Thorac. Soc. 2022, 19, 1842–1847. [Google Scholar] [CrossRef] [PubMed]
- Allinson, J.P.; Hardy, R.; Donaldson, G.C.; Shaheen, S.O.; Kuh, D.; Wedzicha, J.A. Combined Impact of Smoking and Early-Life Exposures on Adult Lung Function Trajectories. Am. J. Respir. Crit. Care Med. 2017, 196, 1021–1030. [Google Scholar] [CrossRef] [PubMed]
- Negewo, N.A.; McDonald, V.M.; Gibson, P.G. Comorbidity in chronic obstructive pulmonary disease. Respir. Investig. 2015, 53, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Rabe, K.F.; Hurst, J.R.; Suissa, S. Cardiovascular disease and COPD: Dangerous liaisons? Eur. Respir. Rev. 2018, 27, 180057. [Google Scholar] [CrossRef]
- Kiani, F.Z.; Ahmadi, A. Prevalence of different comorbidities in chronic obstructive pulmonary disease among Shahrekord PERSIAN cohort study in southwest Iran. Sci. Rep. 2021, 11, 1548. [Google Scholar] [CrossRef]
- Ionescu, A.A.; Schoon, E. Osteoporosis in chronic obstructive pulmonary disease. Eur. Respir. J. 2003, 22, 64s–75s. [Google Scholar] [CrossRef]
- Pumar, M.I.; Gray, C.R.; Walsh, J.R.; Yang, I.A.; Rolls, T.A.; Ward, D.L. Anxiety and depression-Important psychological comorbidities of COPD. J. Thorac. Dis. 2014, 6, 1615–1631. [Google Scholar] [CrossRef]
- Wang, J.; Willis, K.; Barson, E.; Smallwood, N. The complexity of mental health care for people with COPD: A qualitative study of clinicians’ perspectives. NPJ Prim. Care Respir. Med. 2021, 31, 40. [Google Scholar] [CrossRef]
- Biener, A.I.; Decker, S.L.; Rohde, F. Prevalence and Treatment of Chronic Obstructive Pulmonary Disease (COPD) in the United States. JAMA 2019, 322, 602. [Google Scholar] [CrossRef] [PubMed]
- Safiri, S.; Carson-Chahhoud, K.; Noori, M.; Nejadghaderi, S.A.; Sullman, M.J.M.; Ahmadian Heris, J.; Ansarin, K.; Mansournia, M.A.; Collins, G.S.; Kolahi, A.-A.; et al. Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990-2019: Results from the Global Burden of Disease Study 2019. BMJ 2022, 378, e069679. [Google Scholar] [CrossRef]
- Sanchez, J.; Schumann, D.M.; Karakioulaki, M.; Papakonstantinou, E.; Rassouli, F.; Frasnelli, M.; Brutsche, M.; Tamm, M.; Stolz, D. Laryngopharyngeal reflux in chronic obstructive pulmonary disease—A multi-centre study. Respir. Res. 2020, 21, 220. [Google Scholar] [CrossRef]
- Lee, A.L.; Goldstein, R.S. Gastroesophageal reflux disease in COPD: Links and risks. Int. J. Chronic Obstr. Pulm. Dis. 2015, 10, 1935–1949. [Google Scholar] [CrossRef]
- Terada, K.; Muro, S.; Sato, S.; Ohara, T.; Haruna, A.; Marumo, S.; Kinose, D.; Ogawa, E.; Hoshino, Y.; Niimi, A.; et al. Impact of gastro-oesophageal reflux disease symptoms on COPD exacerbation. Thorax 2008, 63, 951–955. [Google Scholar] [CrossRef]
- Yu, F.; Huang, Q.; Ye, Y.; Zhang, L. Effectiveness of Proton-Pump Inhibitors in Chronic Obstructive Pulmonary Disease: A Meta-Analysis of Randomized Controlled Trials. Front. Med. 2022, 9, 841155. [Google Scholar] [CrossRef]
- Sakae, T.M.; Pizzichini, M.M.; Teixeira, P.J.; Silva, R.M.; Trevisol, D.J.; Pizzichini, E. Exacerbations of COPD and symptoms of gastroesophageal reflux: A systematic review and meta-analysis. J. Bras. Pneumol. 2013, 39, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Casanova, C.; Baudet, J.S.; del Valle Velasco, M.; Martin, J.M.; Aguirre-Jaime, A.; de Torres, J.P.; Celli, B.R. Increased gastro-oesophageal reflux disease in patients with severe COPD. Eur. Respir. J. 2004, 23, 841–845. [Google Scholar] [CrossRef]
- Kang, H.H.; Seo, M.; Lee, J.; Ha, S.Y.; Oh, J.H.; Lee, S.H. Reflux esophagitis in patients with chronic obstructive pulmonary disease. Medicine 2021, 100, e27091. [Google Scholar]
- Kim, J.; Lee, J.H.; Kim, Y.; Kim, K.; Oh, Y.-M.; Yoo, K.H.; Rhee, C.K.; Yoon, H.K.; Kim, Y.S.; Park, Y.B.; et al. Association between chronic obstructive pulmonary disease and gastroesophageal reflux disease: A national cross-sectional cohort study. BMC Pulm. Med. 2013, 13, 51. [Google Scholar] [CrossRef]
- Mokhlesi, B.; Morris, A.L.; Huang, C.F.; Curcio, A.J.; Barrett, T.A.; Kamp, D.W. Increased prevalence of gastroesophageal reflux symptoms in patients with COPD. Chest 2001, 119, 1043–1048. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.L.; Button, B.M.; Denehy, L.; Roberts, S.J.; Bamford, T.L.; Ellis, S.J.; Mu, F.T.; Heine, R.G.; Stirling, R.G.; Wilson, J.W. Proximal and distal gastro-oesophageal reflux in chronic obstructive pulmonary disease and bronchiectasis. Respirology 2014, 19, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Kempainen, R.R.; Savik, K.; Whelan, T.P.; Dunitz, J.M.; Herrington, C.S.; Billings, J.L. High prevalence of proximal and distal gastroesophageal reflux disease in advanced COPD. Chest 2007, 131, 1666–1671. [Google Scholar] [CrossRef]
- Liang, B.M.; Feng, Y.L. Association of gastroesophageal reflux disease symptoms with stable chronic obstructive pulmonary disease. Lung 2012, 190, 277–282. [Google Scholar] [CrossRef] [PubMed]
- O’Kane, L.; Groher, M. Oropharyngeal dysphagia in patients with chronic obstructive pulmonary disease: A systematic review. Rev. CEFAC 2009, 11, 449–506. [Google Scholar]
- Ohta, K.; Murata, K.; Takahashi, T.; Minatani, S.; Sako, S.; Kanada, Y. Evaluation of swallowing function by two screening tests in primary COPD. Eur. Respir. J. 2009, 34, 280–281. [Google Scholar] [CrossRef]
- Menon, S.; Nightingale, P.; Trudgill, N. Chronic Obstructive Pulmonary Disease and the Risk of Esophagitis, Barrett’s Esophagus, and Esophageal Adenocarcinoma: A Primary Care Case-Control Study. J. Clin. Gastroenterol. 2019, 53, e451–e455. [Google Scholar] [CrossRef]
- Brennan, N.J.; Morris, A.J.; Green, M. Thoracoabdominal mechanics during tidal breathing in normal subjects and in emphysema and fibrosing alveolitis. Thorax 1983, 38, 62–66. [Google Scholar] [CrossRef]
- Lee, A.S.; Lee, J.S.; He, Z.; Ryu, J.H. Reflux-Aspiration in Chronic Lung Disease. Ann. Am. Thorac. Soc. 2020, 17, 155–164. [Google Scholar] [CrossRef]
- Mittal, R.K.; Shaffer, H.A.; Parollisi, S.; Baggett, L. Influence of breathing pattern on the esophagogastric junction pressure and esophageal transit. Am. J. Physiol. 1995, 269, G577–G583. [Google Scholar] [CrossRef]
- Yoshida, N.; Yoshikawa, T. Defense mechanism of the esophageal mucosa and esophageal inflammation. J. Gastroenterol. 2003, 38 (Suppl. S15), 31–34. [Google Scholar]
- Yamaguchi, T.; Yoshida, N.; Tomatsuri, N.; Takayama, R.; Katada, K.; Takagi, T.; Ichikawa, H.; Naito, Y.; Okanoue, T.; Yoshikawa, T. Cytokine-induced neutrophil accumulation in the pathogenesis of acute reflux esophagitis in rats. Int. J. Mol. Med. 2005, 16, 71–77. [Google Scholar] [PubMed]
- Barnes, P.J.; Burney, P.G.; Silverman, E.K.; Celli, B.R.; Vestbo, J.; Wedzicha, J.A.; Wouters, E.F. Chronic obstructive pulmonary disease. Nat. Rev. Dis. Primers 2015, 1, 15076. [Google Scholar] [CrossRef]
- Du, Y.; Zhang, H.; Xu, Y.; Ding, Y.; Chen, X.; Mei, Z.; Ding, H.; Jie, Z. Association among genetic polymorphisms of GSTP1, HO-1, and SOD-3 and chronic obstructive pulmonary disease susceptibility. Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 2081–2088. [Google Scholar] [CrossRef]
- Agustí, A.; Hogg, J.C. Update on the Pathogenesis of Chronic Obstructive Pulmonary Disease. N. Engl. J. Med. 2019, 381, 1248–1256. [Google Scholar] [CrossRef] [PubMed]
- Schaberg, T.; Klein, U.; Rau, M.; Eller, J.; Lode, H. Subpopulations of alveolar macrophages in smokers and nonsmokers: Relation to the expression of CD11/CD18 molecules and superoxide anion production. Am. J. Respir. Crit. Care Med. 1995, 151, 1551–1558. [Google Scholar] [CrossRef] [PubMed]
| GERD w/ COPD | GERD w/o COPD | p Value | |
|---|---|---|---|
| Age | 69.4 ± 0.1 | 62.6 ± 0.1 | <0.05 |
| Sex | |||
| Female | 163,422 (57.7%) | 526,068 (58.7%) | <0.01 |
| Male | 119,994 (42.3%) | 370,237 (41.3%) | <0.01 |
| Race | |||
| White | 223,968 (79.0%) | 641,169 (71.5%) | <0.01 |
| Black | 31,758 (11.2%) | 112,906 (12.6%) | <0.01 |
| Hispanic | 11,897 (4.2%) | 69,712 (7.8%) | <0.01 |
| Asian | 2402 (0.8%) | 15,969 (1.8%) | <0.01 |
| Risk factors | |||
| Home oxygen | 49,713 (17.5%) | 13,145 (1.5%) | <0.01 |
| Obesity | 56,610 (20.0%) | 181,703 (20.3%) | >0.05 |
| Smoking | 71,730 (25.3%) | 98,072 (10.9%) | <0.01 |
| Hiatal hernia | 14,340 (5.1%) | 50,383 (5.6%) | >0.05 |
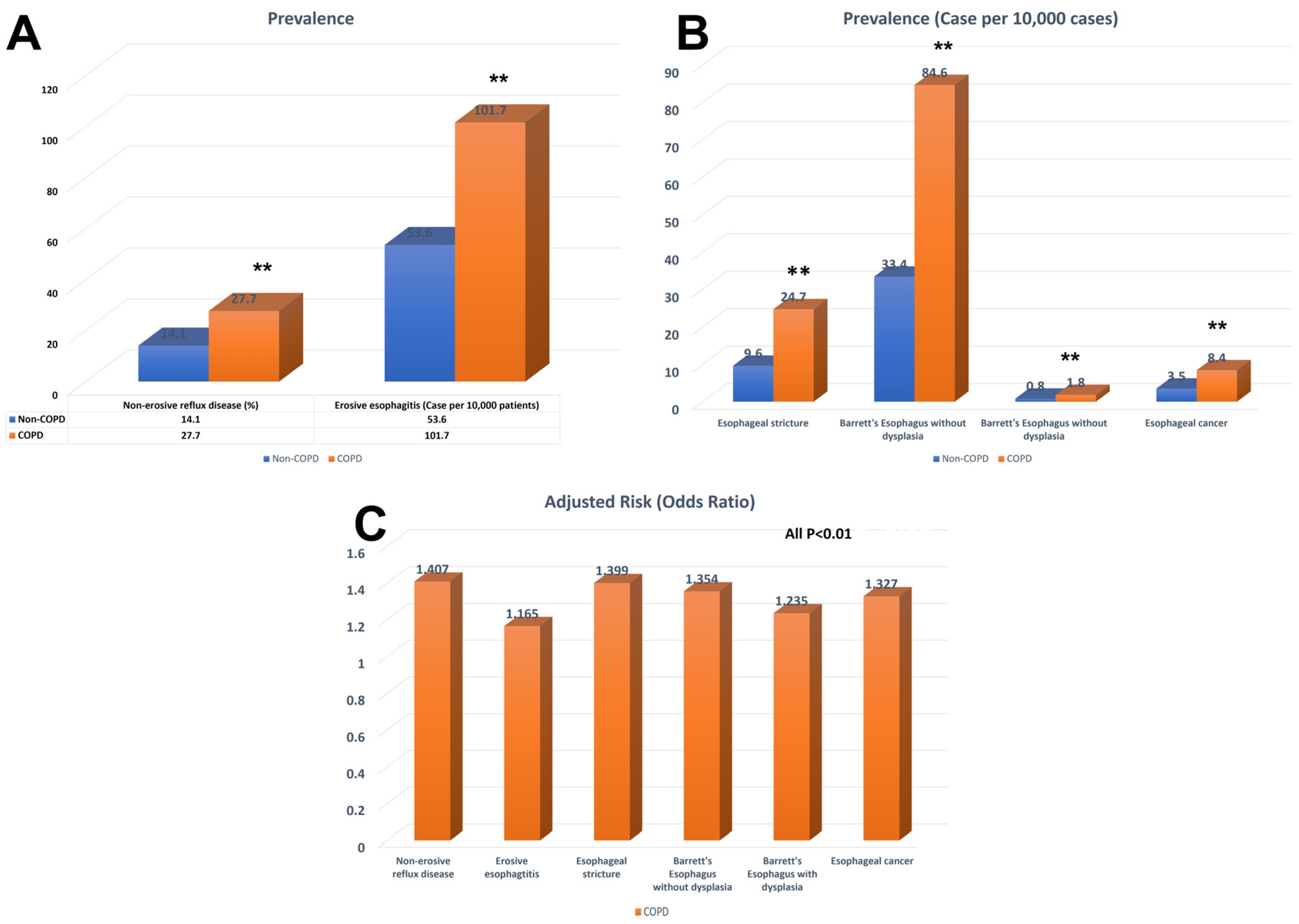
| Case | Prevalence (%) or Case per 10,000 Patients | Adjusted OR | 95% CI | p Value | |
|---|---|---|---|---|---|
| Nonerosive reflux disease | |||||
| COPD | 276,281 | 27.70% | 1.407 | 1.399–1.414 | <0.01 |
| Non-COPD | 868,762 | 14.10% | |||
| Erosive esophagitis | |||||
| COPD | 7348 | 101.7 | 1.165 | 1.133–1.199 | <0.01 |
| Non-COPD | 28,361 | 53.6 | |||
| Esophageal stricture | |||||
| COPD | 1782 | 24.7 | 1.399 | 1.321–1.481 | <0.01 |
| Non-COPD | 5100 | 9.6 | |||
| Barrett’s esophagus w/o dysplasia | |||||
| COPD | 5081 | 84.6 | 1.354 | 1.312–1.397 | <0.01 |
| Non-COPD | 17,625 | 33.4 | |||
| Barrett’s esophagus w/ dysplasia | |||||
| COPD | 128 | 1.8 | 1.235 | 1.002–1.521 | <0.05 |
| Non-COPD | 404 | 0.8 | |||
| Esophageal cancer | |||||
| COPD | 605 | 8.4 | 1.327 | 1.204–1.462 | <0.01 |
| Non-COPD | 1852 | 3.5 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, X.; Wright, Z.; Wang, J.; Roy, S.; Fass, R.; Song, G. Elucidating the Link: Chronic Obstructive Pulmonary Disease and the Complex Interplay of Gastroesophageal Reflux Disease and Reflux-Related Complications. Medicina 2023, 59, 1270. https://doi.org/10.3390/medicina59071270
Wang X, Wright Z, Wang J, Roy S, Fass R, Song G. Elucidating the Link: Chronic Obstructive Pulmonary Disease and the Complex Interplay of Gastroesophageal Reflux Disease and Reflux-Related Complications. Medicina. 2023; 59(7):1270. https://doi.org/10.3390/medicina59071270
Chicago/Turabian StyleWang, Xiaoliang, Zachary Wright, Jiayan Wang, Stephen Roy, Ronnie Fass, and Gengqing Song. 2023. "Elucidating the Link: Chronic Obstructive Pulmonary Disease and the Complex Interplay of Gastroesophageal Reflux Disease and Reflux-Related Complications" Medicina 59, no. 7: 1270. https://doi.org/10.3390/medicina59071270
APA StyleWang, X., Wright, Z., Wang, J., Roy, S., Fass, R., & Song, G. (2023). Elucidating the Link: Chronic Obstructive Pulmonary Disease and the Complex Interplay of Gastroesophageal Reflux Disease and Reflux-Related Complications. Medicina, 59(7), 1270. https://doi.org/10.3390/medicina59071270







