Effects of Dental Bleaching Agents on the Surface Roughness of Dental Restoration Materials
Abstract
1. Introduction
2. Materials and Methods
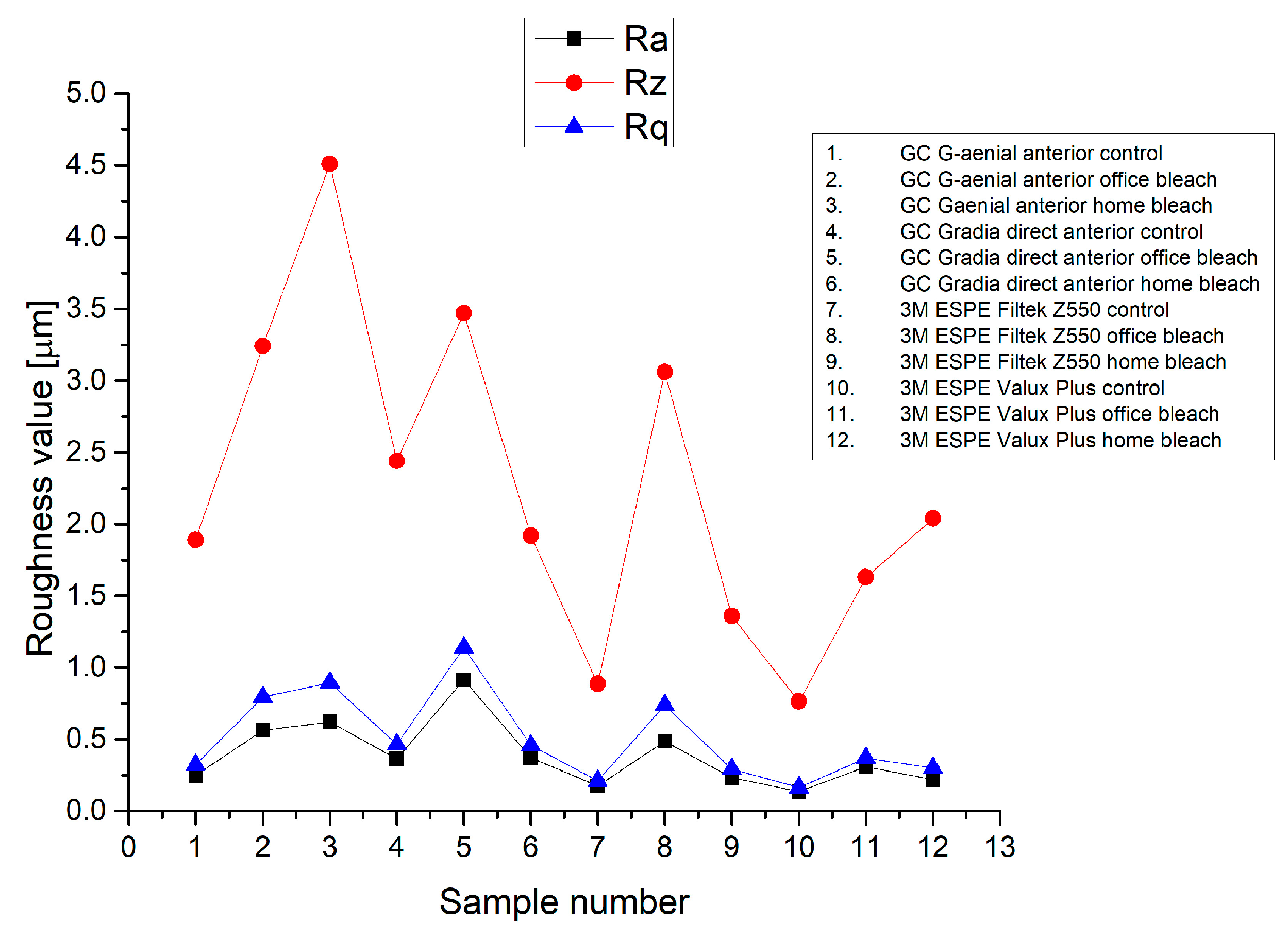
3. Results
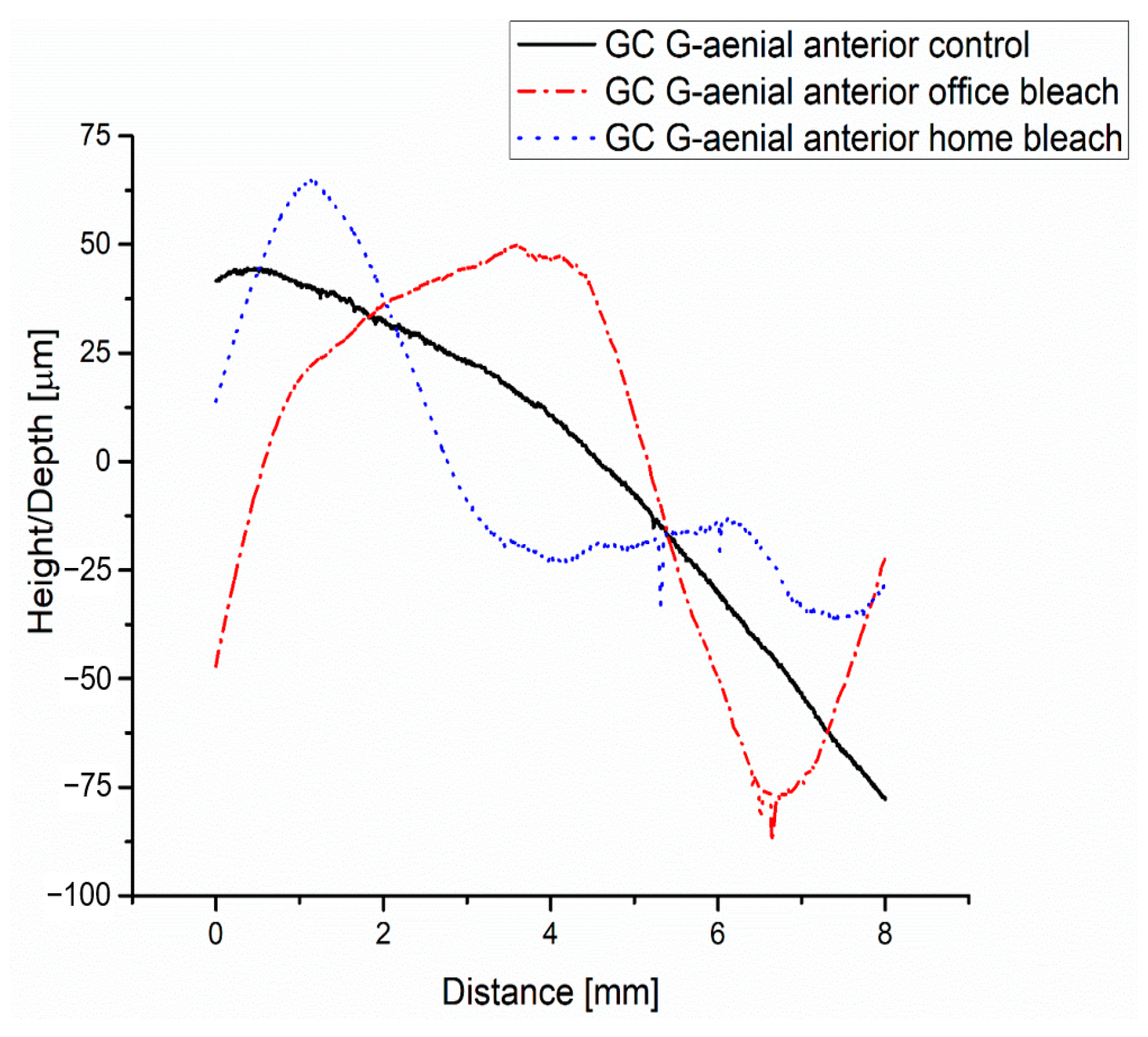
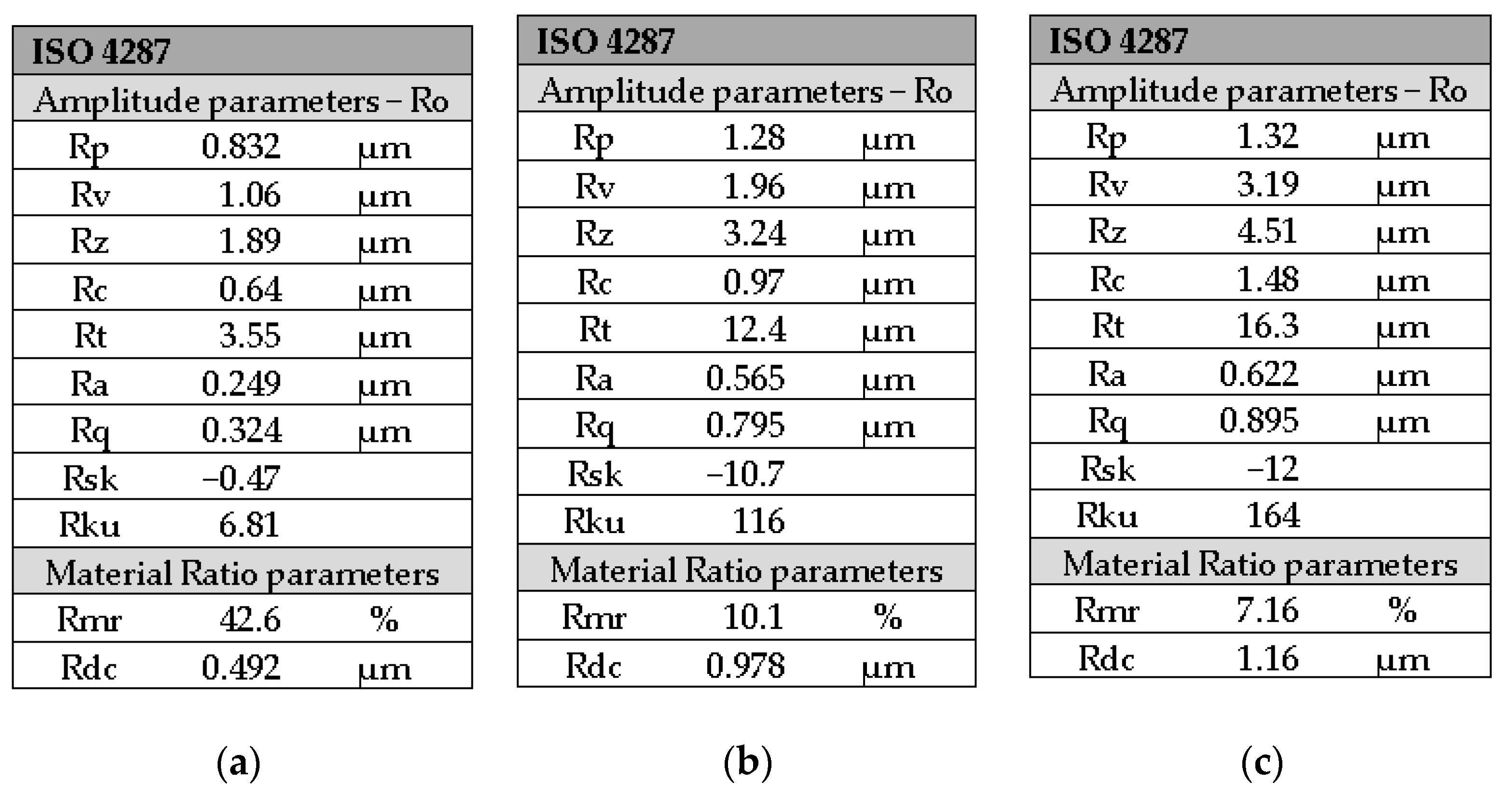
3.1. GC G-Aenial Anterior Composite—Analysis
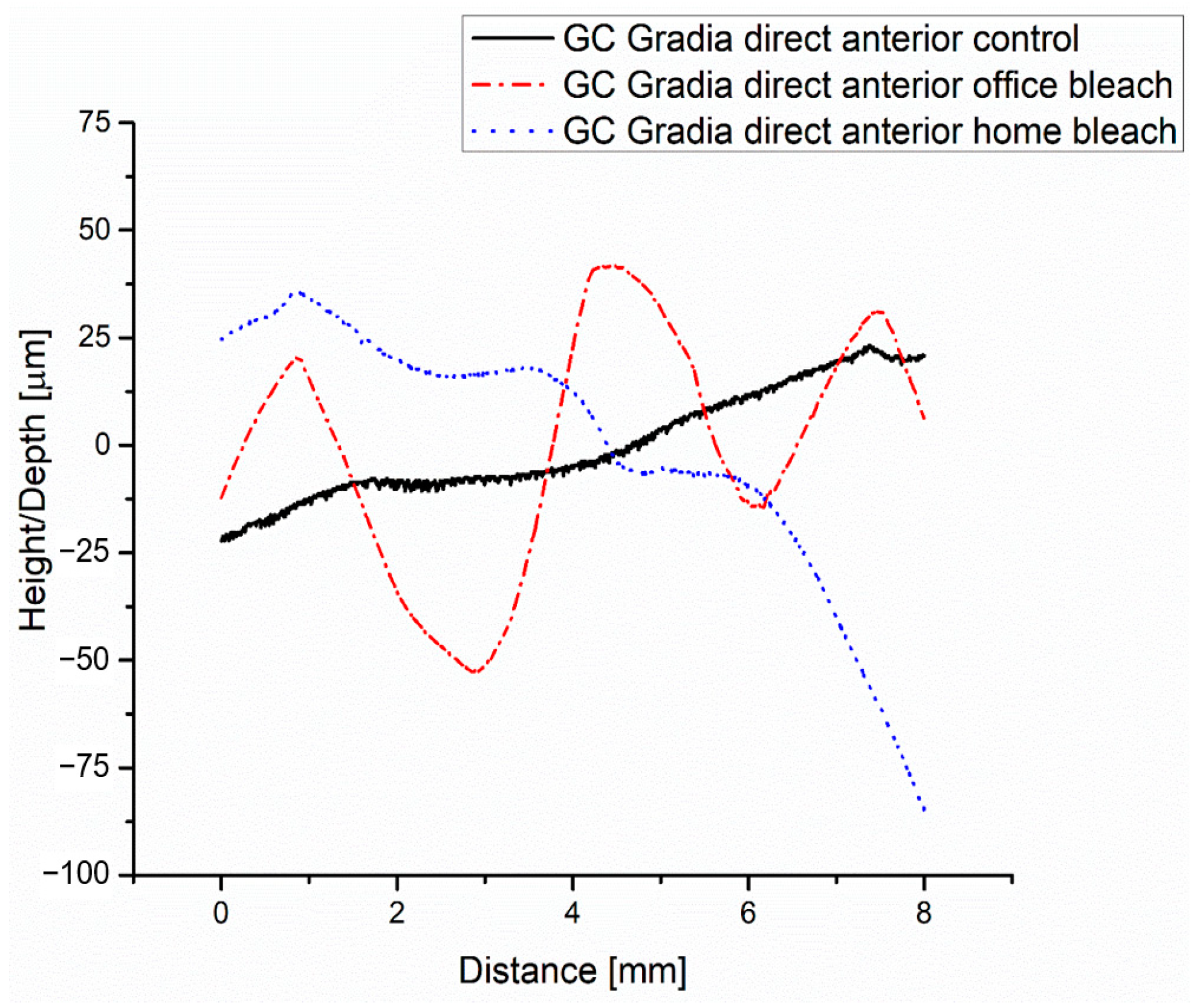
3.2. GC G-Gradia Anterior Composite—Analysis
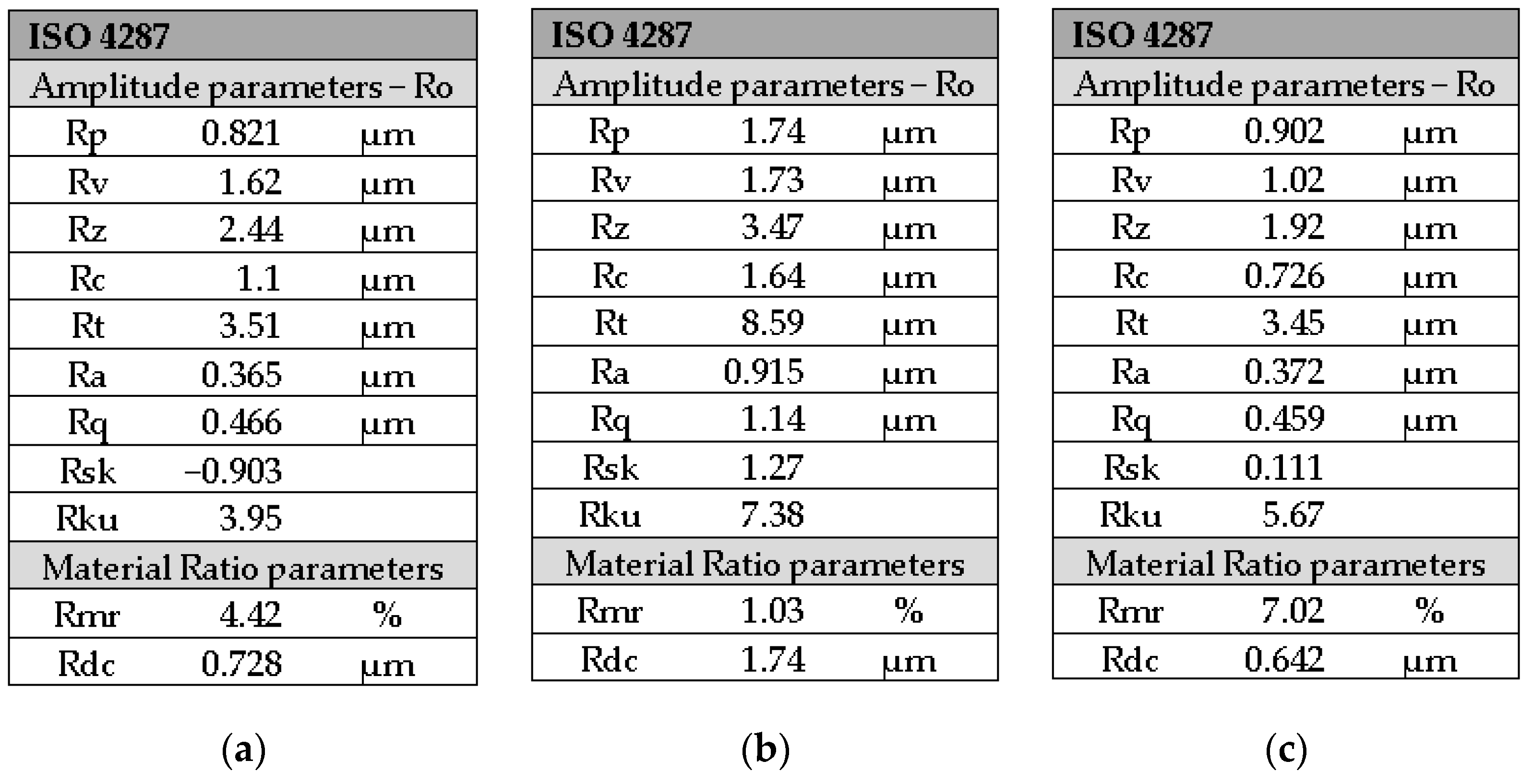
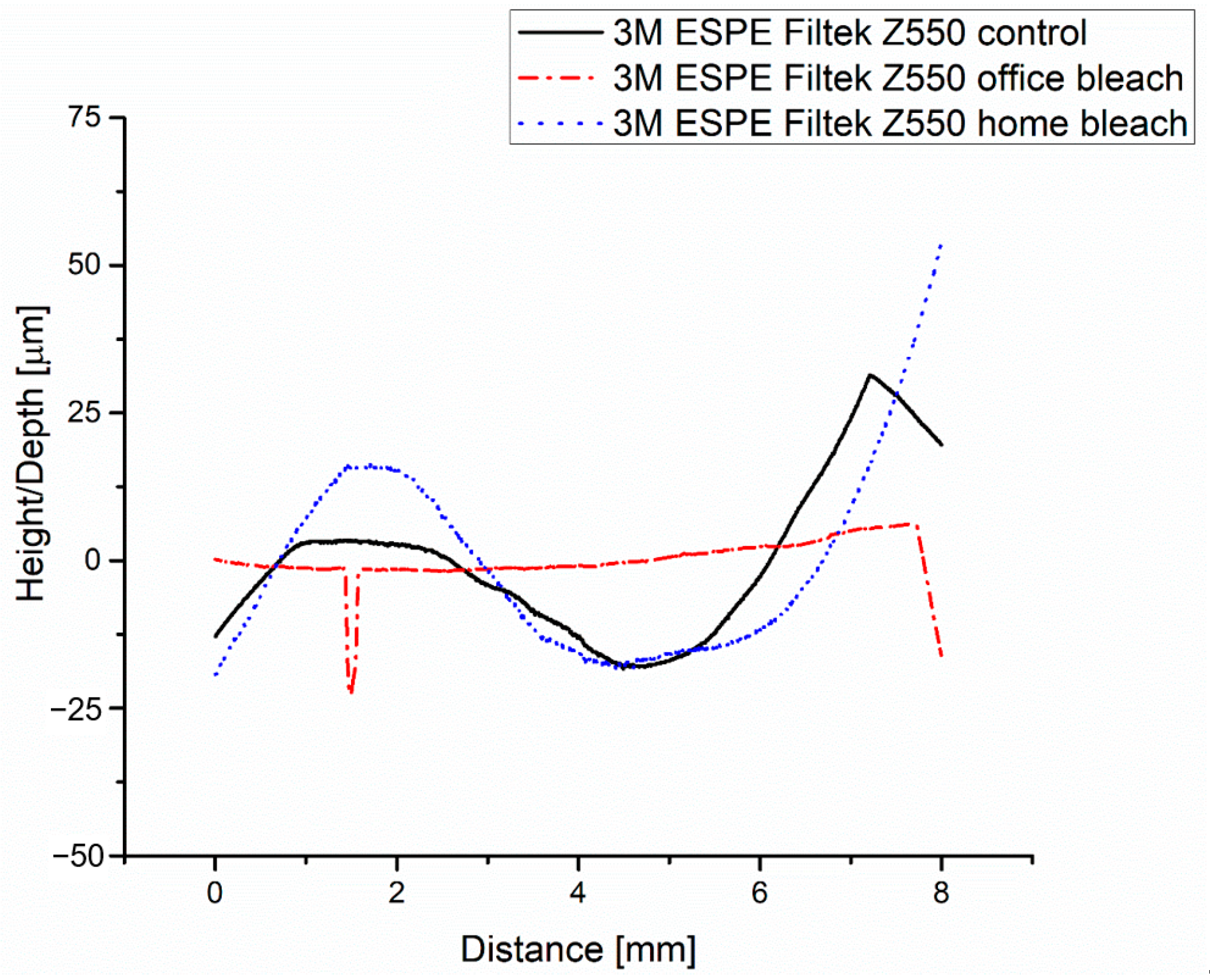
3.3. 3M ESPE Filtek Z550 Composite—Analysis
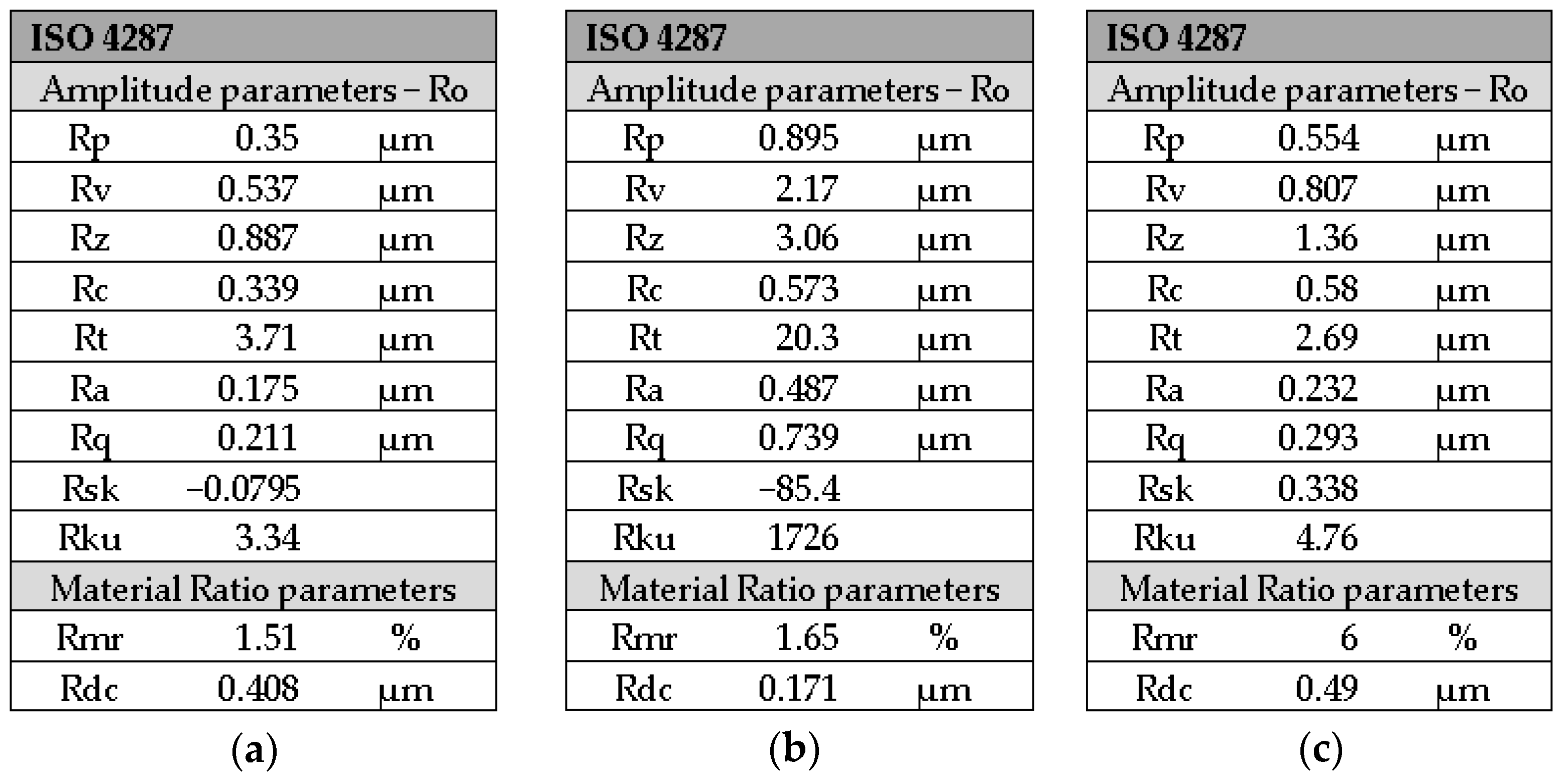
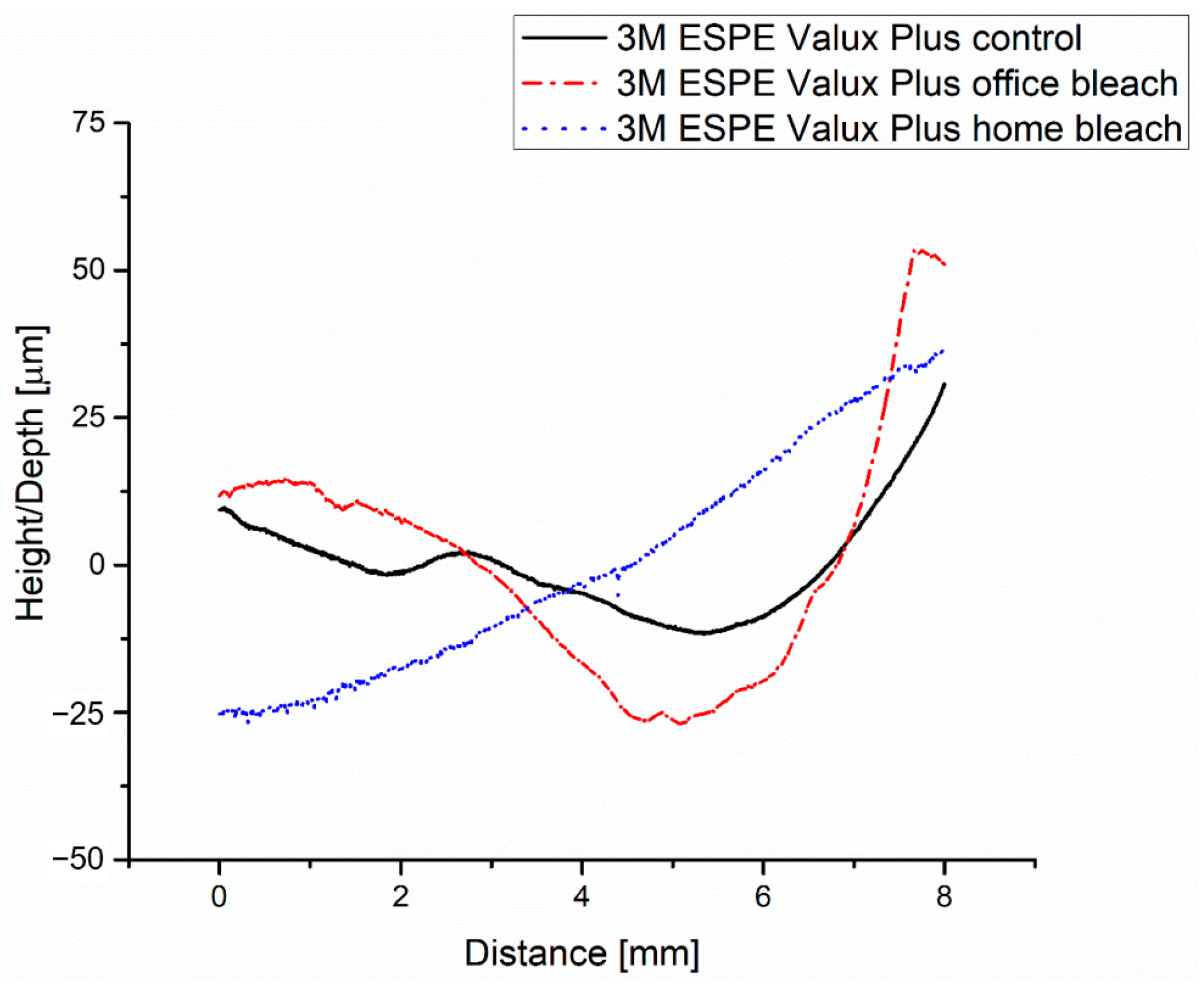
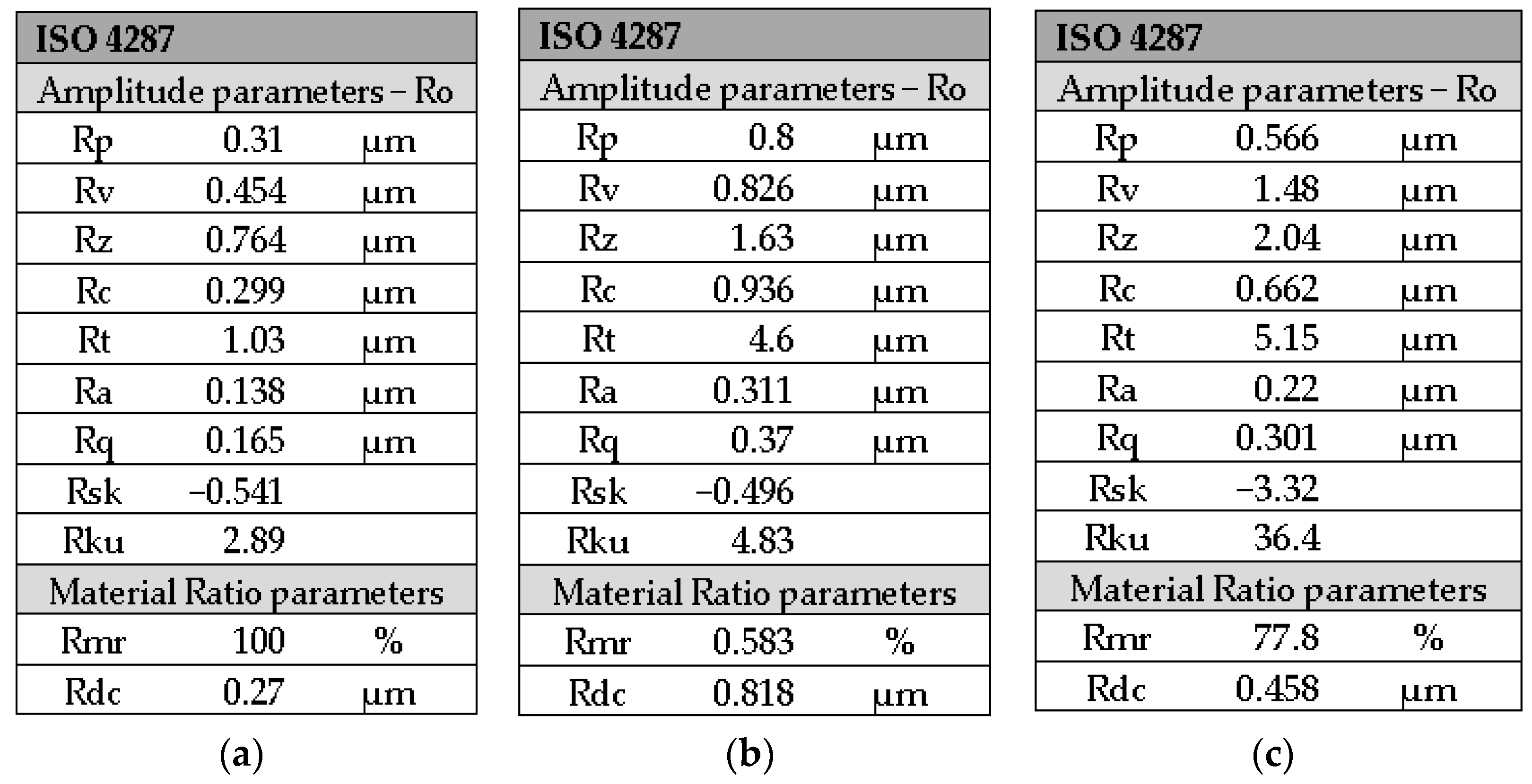
3.4. 3M ESPE Valux plus Composite—Analysis
4. Discussion
4.1. Limitations of the Study
4.2. Recommendations for Further Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fugolin, A.P.P.; Pfeifer, C.S. New Resins for Dental Composites. J. Dent. Res. 2017, 96, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Kumari, R.V.; Nagaraj, H.; Siddaraju, K.; Poluri, R.K. Evaluation of the Effect of Surface Polishing, Oral Beverages and Food Colorants on Color Stability and Surface Roughness of Nanocomposite materials. J. Int. Oral Health 2015, 7, 63–70. [Google Scholar] [PubMed]
- Rawls, H.R.; Esquivel-Upshaw, J.F. Phillips’ Science of Dental Materials, 11th ed.; Elsevier Science: St. Louis, MO, USA, 2003; pp. 399–437. [Google Scholar]
- Ilie, N.; Hickel, R. Resin composite restorative materials. Aust. Dent. J. 2011, 56, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Randolph, L.D.; Palin, W.M.; Leloup, G.; Leprince, J.G. Filler characteristics of modern dental resin composites and their influence on physico-mechanical properties. Dent. Mater. 2016, 32, 1586–1599. [Google Scholar] [CrossRef] [PubMed]
- Ernst, C.P.; Brandenbusch, M.; Meyer, G.; Canbek, K.; Gottschalk, F.; Willershausen, B. Two-year clinical performance of a nanofiller vs a fine-particle hybrid resin composite. Clin. Oral Investig. 2006, 10, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Loguercio, A.D.; Lorini, E.; Weiss, R.V.; Tori, A.P.; Picinatto, C.C.; Ribeiro, N.R.; Reis, A. A 12-month clinical evaluation of composite resins in class III restorations. J. Adhes. Dent. 2007, 9, 57–64. [Google Scholar]
- Aydın, N.; Topçu, F.T.; Karaoğlanoğlu, S.; Oktay, E.A.; Erdemir, U. Effect of finishing and polishing systems on the surface roughness and color change of composite materials. J. Clin. Exp. Dent. 2021, 13, e446–e454. [Google Scholar] [CrossRef]
- Bashetty, K.; Joshi, S. The effect of one-step and multi-step polishing systems on surface texture of two different resin composites. J. Conserv. Dent. 2010, 13, 34–38. [Google Scholar] [CrossRef]
- Yadav, R.D.; Raisingani, D.; Jindal, D.; Mathur, R. A Comparative Analysis of Different Finishing and Polishing Devices on Nanofilled, Microfilled, and Hybrid Composite: A Scanning Electron Microscopy and Profilometric Study. Int. J. Clin. Pediatr. Dent. 2016, 9, 201–208. [Google Scholar] [CrossRef]
- Goncalves, M.A.; Teixeira, V.C.; Rodrigues, S.S.; de Oliveira, R.S.; Salvio, L.A. Evaluation of the roughness of composite resins submitted to different surface treatments. Acta Odontol. Latinoam. 2012, 25, 89–95. [Google Scholar]
- Pettini, F.; Corsalini, M.; Savino, M.G.; Stefanachi, G.; Di Venere, D.; Pappalettere, C.; Monno, G.; Boccaccio, A. Roughness Analysis on Composite Materials (Microfilled, Nanofilled and Silorane) after Different Finishing and Polishing Procedures. Open Dent. J. 2015, 9, 357–367. [Google Scholar] [CrossRef]
- Jaramillo-Cartagena, R.; López-Galeano, E.J.; Latorre-Correa, F.; Agudelo-Suárez, A.A. Effect of Polishing Systems on the Surface Roughness of Nano-Hybrid and Nano-Filling Composite Resins: A Systematic Review. Dent. J. 2021, 9, 95. [Google Scholar] [CrossRef] [PubMed]
- Pallarés-Serrano, A.; Pallarés-Serrano, A.; Pallarés-Serrano, S.; Pallarés-Sabater, A. Study of the intra-coronal pressure generated by internal bleaching agents and its influence on temporary restoration. Appl. Sci. 2022, 12, 2799. [Google Scholar] [CrossRef]
- Savić-Stanković, T.; Karadžić, B.; Latković, M.; Miletić, V. Clinical efficiency of a sodium perborate-hydrogen peroxide mixture for intracoronal non-vital teeth bleaching. Srp. Arh. Celok. Lek. 2020, 148, 24–30. [Google Scholar] [CrossRef]
- Sulieman, M.; Addy, M.; Rees, J.S. Development and evaluation of a method in vitro to study the effectiveness of tooth bleaching. J. Dent. 2003, 31, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Emoto, M.; Tomita, K.; Kanemaru, N.; Tokuda, M.; Torii, M. Development of surface coating material for discolored tooth equipped with bleaching effect. Dent. Mater. J. 2012, 31, 797–805. [Google Scholar] [CrossRef]
- Pini, N.I.P.; Piccelli, M.R.; Vieira-Junior, W.F.; Ferraz, L.N.; Aguiar, F.H.B.; Lima, D.A.N.L. In-office tooth bleaching with chitosan-enriched hydrogen peroxide gels: In vitro results. Clin. Oral Investig. 2022, 26, 471–479. [Google Scholar] [CrossRef]
- Acuña, E.D.; Parreiras, S.O.; Favoreto, M.W.; Cruz, G.P.; Gomes, A.; Borges, C.P.F.; Loguercio, A.D.; Reis, A. In-office bleaching with a commercial 40% hydrogen peroxide gel modified to have different pHs: Color change, surface morphology, and penetration of hydrogen peroxide into the pulp chamber. J. Esthet. Restor. Dent. 2022, 34, 322–327. [Google Scholar] [CrossRef]
- Rodríguez-Martínez, J.; Valiente, M.; Sánchez-Martín, M.J. Tooth whitening: From the established treatments to novel approaches to prevent side effects. J. Esthet. Restor. Dent. 2019, 31, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Rashid, H. The effect of surface roughness on ceramics used in dentistry: A review of literature. Eur. J. Dent. 2014, 8, 571–579. [Google Scholar]
- Silva, F.P.; Vilela, A.L.R.; Almeida, M.M.G.; Oliveira, A.R.F.; Raposo, L.H.A.; Menezes, M.S. Surface Topography, Gloss and Flexural Strength of Pressable Ceramic after Finishing-Polishing Protocols. Braz. Dent. J. 2019, 30, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Mazilu Moldovan, A.; Popescu, V.; Ionescu, C.V.; Cuc, S.; Craciun, A.; Moldovan, M.; Dudea, D.; Mesaros, A.S. Various Aspects Involved in the Study of Tooth Bleaching Procedure: A Questionnaire-Based Study. Int. J. Environ. Res. Public Health 2022, 19, 3977. [Google Scholar] [CrossRef]
- Alrabeah, G.; Shabib, S.; Almomen, R.; Alhedeithi, N.; Alotaibi, S.; Habib, S.R. Effect of Home Bleaching on the Optical Properties and Surface Roughness of Novel Aesthetic Dental Ceramics. Coatings 2023, 13, 330. [Google Scholar] [CrossRef]
- Baciu, E.R.; Forna, N.C. Influence of finishing techniques on the surface roughness of metallic components of prosthetic restorations. Rev. Med. Chir. Soc. Med. Nat. Iasi 2010, 114, 1198–1203. [Google Scholar] [PubMed]
- Bezerra-Júnior, D.M.; Silva, L.M.; Martins, L.D.M.; Cohen-Carneiro, F.; Pontes, D.G. Esthetic rehabilitation with tooth bleaching, enamel microabrasion, and direct adhesive restorations. Gen. Dent. 2016, 64, 60–64. [Google Scholar] [PubMed]
- Gallinari, M.O.; Fagundes, T.C.; da Silva, L.M.; de Almeida Souza, M.B.; Barboza, A.; Briso, A. A New Approach for Dental Bleaching Using Violet Light with or Without the Use of Whitening Gel: Study of Bleaching Effectiveness. Oper. Dent. 2019, 44, 521–529. [Google Scholar] [CrossRef]
- Briso, A.L.F.; Rahal, V.; Azevedo, F.A.; Gallinari, A.; de Gonçalves, O.R.S.; Frascino, S.M.B.; dos Santos, P.H.; Cintra, L.T.A. Neurosensory analysis of tooth sensitivity during at-home dental bleaching: A randomized clinical trial. J. Appl. Oral Sci. 2018, 26, e20170284. [Google Scholar] [CrossRef]
- Esmaeili, B.; Abolghasemzadeh, F.; Gholampor, A.; Daryakenari, G. The effect of home bleaching carbamide peroxide concentration on the microhardness of dental composite materials. Gen. Dent. 2018, 66, 40–44. [Google Scholar]
- Alharbi, A.; Ardu, S.; Bortolotto, T.; Krejci, I. In-office bleaching efficacy on stain removal from CAD/CAM and direct resin composite materials. J. Esthet. Restor. Dent. 2018, 30, 51–58. [Google Scholar] [CrossRef]
- Al-Angari, S.S.; Eckert, G.J.; Sabrah, A.H.A. Color stability, Roughness, and Microhardness of Enamel and Composites Submitted to Staining/Bleaching Cycles. Saudi Dent. J. 2021, 33, 215–221. [Google Scholar] [CrossRef]
- Benetti, F.; Briso, A.L.F.; Ferreira, L.L.; Carminatti, M.; Álamo, L.; Ervolino, E.; Dezan-Júnior, E.; Cintra, L.T.A. In vivo study of the action of a topical anti-inflammatory drug in rat teeth submitted to dental bleaching. Braz. Dent. J. 2018, 29, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L.; Laino, L.; De Stefano, R.; D’Amico, C.; Bocchieri, S.; Amoroso, G.; Isola, G.; Cervino, G. Dental Whitening Gels: Strengths and Weaknesses of an Increasingly Used Method. Gels 2019, 5, 35. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.H. Restorative and Esthetic Dentistry-A Special Issue of the Dentistry Journal. Dent. J. 2018, 6, 5. [Google Scholar] [CrossRef]
- Akalιn, T.T.; Bozkurt, F.O.; Tuncer, A.K.; Bağ, H.G.; Özcan, M. Clinical Performance of Nanofilled and Microhybrid Direct Composite Restorations on Endodontically Treated Teeth. Eur. J. Prosthodont. Restor. Dent. 2019, 27, 39–47. [Google Scholar]
- Chesterman, J.; Jowett, A.; Gallacher, A.; Nixon, P. Bulk-fill resin-based composite restorative materials: A review. Br. Dent. J. 2017, 222, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Davies, R.A.; Ardalan, S.; Mu, W.; Tian, K.; Farsaikiya, F.; Darvell, B.W.; Chass, G.A. Geometric, electronic and elastic properties of dental silver amalgam g-(Ag3Sn), g1-(Ag2Hg3), g2-(Sn8Hg) phases, comparison of experiment and theory. Intermetallics 2010, 18, 756–760. [Google Scholar] [CrossRef]
- Sidhu, S.K.; Nicholson, J.W. A Review of Glass-Ionomer Cements for Clinical Dentistry. J. Funct. Biomater. 2016, 7, 16. [Google Scholar] [CrossRef]
- Zhou, X.; Huang, X.; Li, M.; Peng, X.; Wang, S.; Zhou, X.; Cheng, L. Development and status of resin composite as dental restorative materials. J. Appl. Polym. Sci. 2019, 136, 48180. [Google Scholar] [CrossRef]
- Bayne, S.C.; Thompson, J.Y.; Swift, E.J., Jr.; Stamatiades, P.; Wilkerson, M. A characterization of first-generation flowable composites. J. Am. Dent. Assoc. 1998, 129, 567–577. [Google Scholar] [CrossRef]
- Alpöz, A.R.; Ertugrul, F.; Cogulu, D.; Ak, A.T.; Tanoglu, M.; Kaya, E. Effects of light curing method and exposure time on mechanical properties of resin based dental materials. Eur. J. Dent. 2008, 2, 37–42. [Google Scholar] [CrossRef]
- Farzad, A.; Kasraei, S.; Haghi, S.; Masoumbeigi, M.; Torabzadeh, H.; Panahandeh, N. Effects of 3 different light-curing units on the physico-mechanical properties of bleach-shade resin composites. Restor. Dent. Endod. 2022, 47, e9. [Google Scholar] [CrossRef] [PubMed]
- Wilson, F.; Heath, J.R.; Watts, D.C. Finishing composite restorative materials. J. Oral. Rehabil. 1990, 17, 79–87. [Google Scholar] [CrossRef]
- Zuryati, A.G.; Qian, O.Q.; Dasmawati, M. Effects of home bleaching on surface hardness and surface roughness of an experimental nanocomposite. J. Conserv. Dent. 2013, 16, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Carretero Peláez, M.A.; Esparza Gómez, G.C.; Figuero Ruiz, E.; Cerero Lapiedra, R. Alcohol-containing mouthwashes and oral cancer. Critical analysis of literature. Med. Oral 2004, 9, 120. [Google Scholar]
- Abdelaziz, K.M.; Mir, S.; Khateeb, S.U.; Baba, S.M.; Alshahrani, S.S.; Alshahrani, E.A.; Alsafi, Z.A. Influences of Successive Exposure to Bleaching and Fluoride Preparations on the Surface Hardness and Roughness of the Aged Resin Composite Restoratives. Medicina 2020, 56, 476. [Google Scholar] [PubMed]
- Mohammadi, N.; Kimyai, S.; Abed-Kahnamoii, M.; Ebrahimi-Chaharom, M.E.; Sadr, A.; Daneshi, M. Effect of 15% carbamide peroxide bleaching gel on color stability of giomer and microfilled composite material: An in vitro comparison. Med. Oral Patol. Oral Cir. Bucal 2012, 17, e1082–e1088. [Google Scholar] [CrossRef]
- Canay, S.; Cehreli, M.C. The effect of current bleaching agents on the color of light-polymerized composites in vitro. J. Prosthet. Dent. 2003, 89, 474–478. [Google Scholar] [CrossRef]
- Li, Q.; Yu, H.; Wang, Y. Colour and surface analysis of carbamide peroxide bleaching effects on the dental restorative materials in situ. J. Dent. 2009, 37, 348–356. [Google Scholar] [CrossRef]
- Hubbezoglu, I.; Akaoğlu, B.; Dogan, A.; Keskin, S.; Bolayir, G.; Ozçelik, S.; Dogan, O.M. Effect of bleaching on color change and refractive index of dental composite materials. Dent. Mater. J. 2008, 27, 105–116. [Google Scholar] [CrossRef]
- Kimyai, S.; Lotfipour, F.; Pourabbas, R.; Sadr, A.; Nikazar, S.; Milani, M. Effect of two prophylaxis methods on adherence of Streptococcus mutans to microfilled composite material and giomer surfaces. Med. Oral Patol. Oral Cir. Bucal 2011, 16, e561–e567. [Google Scholar] [CrossRef]
- Attin, T.; Hannig, C.; Wiegand, A.; Attin, R. Effect of bleaching on restorative materials and restorations—A systematic review. Dent. Mater. 2004, 20, 852–861. [Google Scholar] [CrossRef] [PubMed]
- Varanda, E.; Do Prado, M.; Simão, R.A.; Dias, K.R. Effect of in-office bleaching agents on the surface roughness and morphology of different dental composites: An AFM study. Microsc. Res. Tech. 2013, 76, 481–485. [Google Scholar] [PubMed]
- Gurgan, S.; Yalcin, F. The effect of 2 different bleaching regimens on the surface roughness and hardness of tooth-colored restorative materials. Quintessence Int. 2007, 38, e83–e87. [Google Scholar] [PubMed]
- Wang, L.; Francisconi, L.F.; Atta, M.T.; Atta, M.T.; Dos Santos, J.R.; Del Padre, N.C.; Gonini, A., Jr.; Fernandes, K.B. Effect of bleaching gels on surface roughness of nanofilled composite materials. Eur. J. Dent. 2011, 5, 173–179. [Google Scholar] [PubMed]
- Rattacaso, R.M.; da Fonseca Roberti Garcia, L.; Aguilar, F.G.; Consani, S.; de Carvalho Panzeri Pires-de-Souza, F. Bleaching agent action on color stability, surface roughness and microhardness of composites submitted to accelerated artificial aging. Eur. J. Dent. 2011, 5, 143–149. [Google Scholar] [CrossRef]
- Shah, M.B.; Ferracane, J.L.; Kruzic, J.J. R-curve behavior and toughening mechanisms of resin-based dental composites: Effects of hydration and post- cure heat treatment. Dent. Mater. 2009, 25, 760–770. [Google Scholar] [CrossRef]
- Alshali, R.Z.; Salim, N.A.; Satterthwaite, J.D.; Silikas, N. Long-term sorption and solubility of bulk-fill and conventional resin-composites in water and artificial saliva. J. Dent. 2015, 43, 1511–1518. [Google Scholar]
- Vichi, A.; Ferrari, M.; Davidson, C.L. Color and opacity variations in three different resin-based composite products after water aging. Dent. Mater. 2004, 20, 530–534. [Google Scholar] [CrossRef]
- Tavares, B.G.; França, F.M.; Basting, R.T.; Turssi, C.P.; Amaral, F.L. Effect of bleaching protocols on surface roughness and color change of high- and low-viscosity bulk-fill composite materials. Acta Odontol. Latinoam. 2020, 33, 59–68. [Google Scholar] [CrossRef]
- Bailey, S.J.; Swift, E.J., Jr. Effects of home bleaching products on composite materials. Quintessence Int. 1992, 23, 489–494. [Google Scholar]
- Yap, A.U.; Wattanapayungkul, P. Effects of in-office tooth whiteners on hardness of tooth-colored restoratives. Oper. Dent. 2002, 27, 137–141. [Google Scholar] [PubMed]
- Lainović, T.; Vilotić, M.; Blažić, L.; Kakaš, D.; Marković, D.; Ivanišević, A. Determination of surface roughness and topography of dental resin-based nanocomposites using AFM analysis. Bosn. J. Basic Med. Sci. 2013, 13, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Geethu, F.; Pradeep, K.; Ginjupalli, K.; Saraswathi, V. Effects of Bleaching Agents on the Microhardness and Surface Roughness of Bulk Fill Composites. World J. Dent. 2017, 8, 196–201. [Google Scholar]
- Markovic, L.; Jordan, R.A.; Glasser, M.C.; Arnold, W.H.; Nebel, J.; Tillmann, W.; Ostermann, T.; Zimmer, S. Effects of bleaching agents on surface roughness of filling materials. Dent. Mater. J. 2014, 33, 59–63. [Google Scholar] [CrossRef]
- Gladys, S.; Van Meerbeek, B.; Braem, M.; Lambrechts, P.; Vanherle, G. Comparative physico-mechanical characterization of new hybrid restorative materials with conventional glass-ionomer and resin composite restorative materials. J. Dent. Res. 1997, 76, 883–894. [Google Scholar] [CrossRef]
- Fernandes, R.A.; Strazzi-Sahyon, H.B.; Suzuki, T.Y.U.; Briso, A.L.F. Dos Santos PH. Effect of dental bleaching on the microhardness and surface roughness of sealed composite materials. Restor. Dent. Endod. 2020, 45, e12. [Google Scholar] [CrossRef]
- Dogan, A.; Ozcelik, S.; Dogan, O.M.; Hubbezoglu, I.; Cakmak, M.; Bolayir, G. Effect of bleaching on roughness of dental composite materials. J. Adhes. 2008, 84, 897–914. [Google Scholar] [CrossRef]
- Kaya, M.S.; Bakkal, M.; Durmus, A.; Durmus, Z. Structural and mechanical properties of a giomer-based bulk fill restorative in different curing conditions. J. Appl. Oral Sci. 2018, 26, e20160662. [Google Scholar] [CrossRef]
- Özduman, Z.C.; Kazak, M.; Fildisi, M.A.; Özlen, R.H.; Dalkilic, E.; Donmez, N. Effect of Polymerization Time and Home Bleaching Agent on the Microhardness and Surface Roughness of Bulk-Fill Composites: A Scanning Electron Microscopy Study. Scanning 2019, 2019, 2307305. [Google Scholar] [CrossRef]
- Telang, A.; Narayana, I.H.; Madhu, K.S.; Kalasaiah, D.; Ramesh, P.; Nagaraja, S. Effect of Staining and Bleaching on Color stability and Surface Roughness of Three Resin Composites: An in vitro study. Contemp. Clin. Dent. 2018, 9, 452–456. [Google Scholar]
- Rodrigues, C.S.; Nora, B.D.; Mallmann, A.; May, L.G.; Jacques, L.B. Repolishing Resin Composites after Bleaching Treatments: Effects on Color Stability and Smoothness. Oper. Dent. 2019, 44, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Wongpraparatana, I.; Matangkasombut, O.; Thanyasrisung, P.; Panich, M. Effect of Vital Tooth Bleaching on Surface Roughness and Streptococcal Biofilm Formation on Direct Tooth-Colored Restorative. Oper. Dent. 2018, 43, 51–59. [Google Scholar] [CrossRef] [PubMed]

| Name of Composite | Type of Composite | Manufacturer | Composition |
|---|---|---|---|
| Gradia Direct Anterior | Microhybrid composite | GC Tokyo, Japan | Microhybrid composite material matrix: UDMA, dimethacrylates, trimethacrylates. Fillers: silica and prepolymerised resin fillers (73 wt%). |
| G-aenial Anterior | Microhybrid composite | GC Tokyo, Japan | Microhybrid composite matrix: UDMA, dimethacrylate comonomers. Fillers: prepolymerised silica and strontium fluoride-containing fillers (76 wt%). |
| Filtek Z550 | Nanohybrid composite | 3M ESPE, Minnesota USA | Nanohybrid composite matrix: BIS-GMA, TEGDMA, UDMA, BIS-EMA, PEGDMA. Fillers: silica-zirconia fillers, non-agglomerated/non-aggregated silica particles, filler loading (82 wt%). |
| Valux Plus | Microhybrid composite | 3M ESPE, Minnesota USA | Microhybrid composite matrix: BIS-GMA, TEGDMA. Fillers: zirconia/silica loading is 66% by volume with a particle size range of 3.5 to 0.01 micron. |
| Roughness Parameters | Signification |
|---|---|
| Rp | The upper area, between the middle line and the line parallel to it, tangent to the highest peak. |
| Rv | The lower area, located between the middle line and the line parallel to it passing through the deepest gap of the roughness profile. |
| Rz | The maximum height of the irregularity of the profile in ten points. |
| Rc | Average height of profile elements: defined on the assessment length. |
| Rt | Total height of the profile: the height between the deepest valley and the highest peak on the evaluation length. |
| Ra | Average arithmetic deviation of roughness. |
| Rq | The average quadratic deviation of the heights of the profile roughness. |
| Rsk | Asymmetry of the assessed profile: the asymmetry of the height distribution, defined on the sampling length. |
| Rku | Trial of the assessed profile: the clarity/accuracy of the height distribution, defined on the sampling length. |
| Number | Group Name | Rz [µm] | Ra [µm] | Rq [µm] |
|---|---|---|---|---|
| 1 | GC G-aenial anterior control | 1.888 ± 0.0455 | 0.249 ± 0.0038 | 0.324 ± 0.0028 |
| 2 | GC G-aenial anterior office bleach | 3.242 ± 0.0239 | 0.565 ± 0.0038 | 0.795 ± 0.0048 |
| 3 | GC G-aenial anterior home bleach | 4.508 ± 0.0487 | 0.622 ± 0.0048 | 0.895 ± 0.0095 |
| 4 | GC Gradia direct anterior control | 2.438 ± 0.0449 | 0.365 ± 0.0049 | 0.466 ± 0.0062 |
| 5 | GC Gradia direct anterior office bleach | 3.47 ± 0.0485 | 0.915 ± 0.004 | 1.144 ± 0.0493 |
| 6 | GC Gradia direct anterior home bleach | 1.918 ± 0.0421 | 0.372 ± 0.0024 | 0.459 ± 0.006 |
| 7 | 3M ESPE Filtek Z550 control | 0.887 ± 0.0034 | 0.175 ± 0.003 | 0.211 ± 0.004 |
| 8 | 3M ESPE Filtek Z550 office bleach | 3.058 ± 0.074 | 0.487 ± 0.0085 | 0.739 ± 0.0055 |
| 9 | 3M ESPE Filtek Z550 home bleach | 1.356 ± 0.027 | 0.232 ± 0.0047 | 0.293 ± 0.0055 |
| 10 | 3M ESPE Valux Plus control | 0.764 ± 0.0054 | 0.138 ± 0.0043 | 0.165 ± 0.0042 |
| 11 | 3M ESPE Valux Plus office bleach | 1.63 ± 0.0354 | 0.311 ± 0.0024 | 0.37 ± 0.0453 |
| 12 | 3M ESPE Valux Plus home bleach | 2.044 ± 0.0627 | 0.22 ± 0.0041 | 0.301 ± 0.0053 |
| Composite | Overall p * | Group Comparisons | |||||
|---|---|---|---|---|---|---|---|
| Control—Home Bleach | Control—Office Bleach | Home—Office Bleach | |||||
| p | Trend | p | Trend | p | Trend | ||
| GC G-aenial anterior | <0.0005 | <0.0005 |  | <0.0005 |  | <0.0005 |  |
| GC Gradia direct anterior | <0.0005 | 0.037 |  | <0.0005 |  | <0.0005 |  |
| 3M ESPE Filtek Z550 | <0.0005 | <0.0005 |  | <0.0005 |  | <0.0005 |  |
| 3M ESPE Valux Plus | <0.0005 | <0.0005 |  | <0.0005 |  | <0.0005 |  |
| Bleaching Type | Composite | Mean ± SD | p * |
|---|---|---|---|
| Home | GC G-aenial anterior | 0.374 ± 0.0048 | <0.0005 |
| GC Gradia direct anterior | 0.007 ± 0.0024 | ||
| 3M ESPE Filtek Z550 | 0.057 ± 0.0047 | ||
| 3M ESPE Valux Plus | 0.082 ± 0.0041 | ||
| Office | GC G-aenial anterior | 0.316 ± 0.0038 | <0.0005 |
| GC Gradia direct anterior | 0.550 ± 0.0039 | ||
| 3M ESPE Filtek Z550 | 0.311 ± 0.0084 | ||
| 3M ESPE Valux Plus | 0.337 ± 0.0024 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popescu, A.D.; Tuculina, M.J.; Diaconu, O.A.; Gheorghiță, L.M.; Nicolicescu, C.; Cumpătă, C.N.; Petcu, C.; Abdul-Razzak, J.; Rîcă, A.M.; Voinea-Georgescu, R. Effects of Dental Bleaching Agents on the Surface Roughness of Dental Restoration Materials. Medicina 2023, 59, 1067. https://doi.org/10.3390/medicina59061067
Popescu AD, Tuculina MJ, Diaconu OA, Gheorghiță LM, Nicolicescu C, Cumpătă CN, Petcu C, Abdul-Razzak J, Rîcă AM, Voinea-Georgescu R. Effects of Dental Bleaching Agents on the Surface Roughness of Dental Restoration Materials. Medicina. 2023; 59(6):1067. https://doi.org/10.3390/medicina59061067
Chicago/Turabian StylePopescu, Alexandru Dan, Mihaela Jana Tuculina, Oana Andreea Diaconu, Lelia Mihaela Gheorghiță, Claudiu Nicolicescu, Cristian Niky Cumpătă, Cristiana Petcu, Jaqueline Abdul-Razzak, Ana Maria Rîcă, and Ruxandra Voinea-Georgescu. 2023. "Effects of Dental Bleaching Agents on the Surface Roughness of Dental Restoration Materials" Medicina 59, no. 6: 1067. https://doi.org/10.3390/medicina59061067
APA StylePopescu, A. D., Tuculina, M. J., Diaconu, O. A., Gheorghiță, L. M., Nicolicescu, C., Cumpătă, C. N., Petcu, C., Abdul-Razzak, J., Rîcă, A. M., & Voinea-Georgescu, R. (2023). Effects of Dental Bleaching Agents on the Surface Roughness of Dental Restoration Materials. Medicina, 59(6), 1067. https://doi.org/10.3390/medicina59061067







