Comparative Study of Long-Term Outcomes of Laparoscopic Liver Resection versus Radiofrequency Ablation for Single Small Hepatocellular Carcinoma Located in Left Lateral Segments of the Liver
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
2.2. RFA Procedure and Surgical Technique
2.3. Statistical Analyses
3. Results
3.1. Patient Characteristics
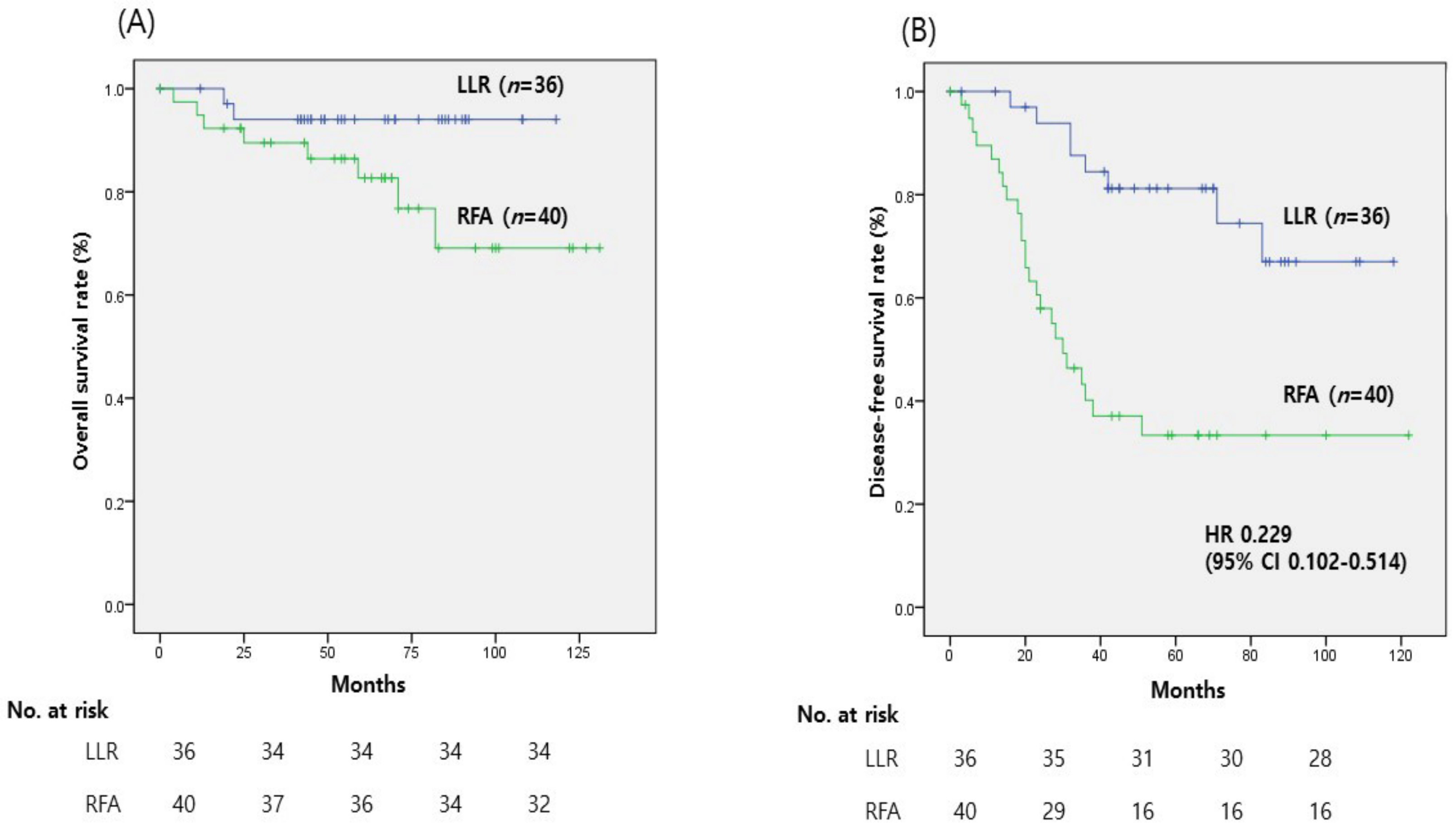
3.2. Outcomes
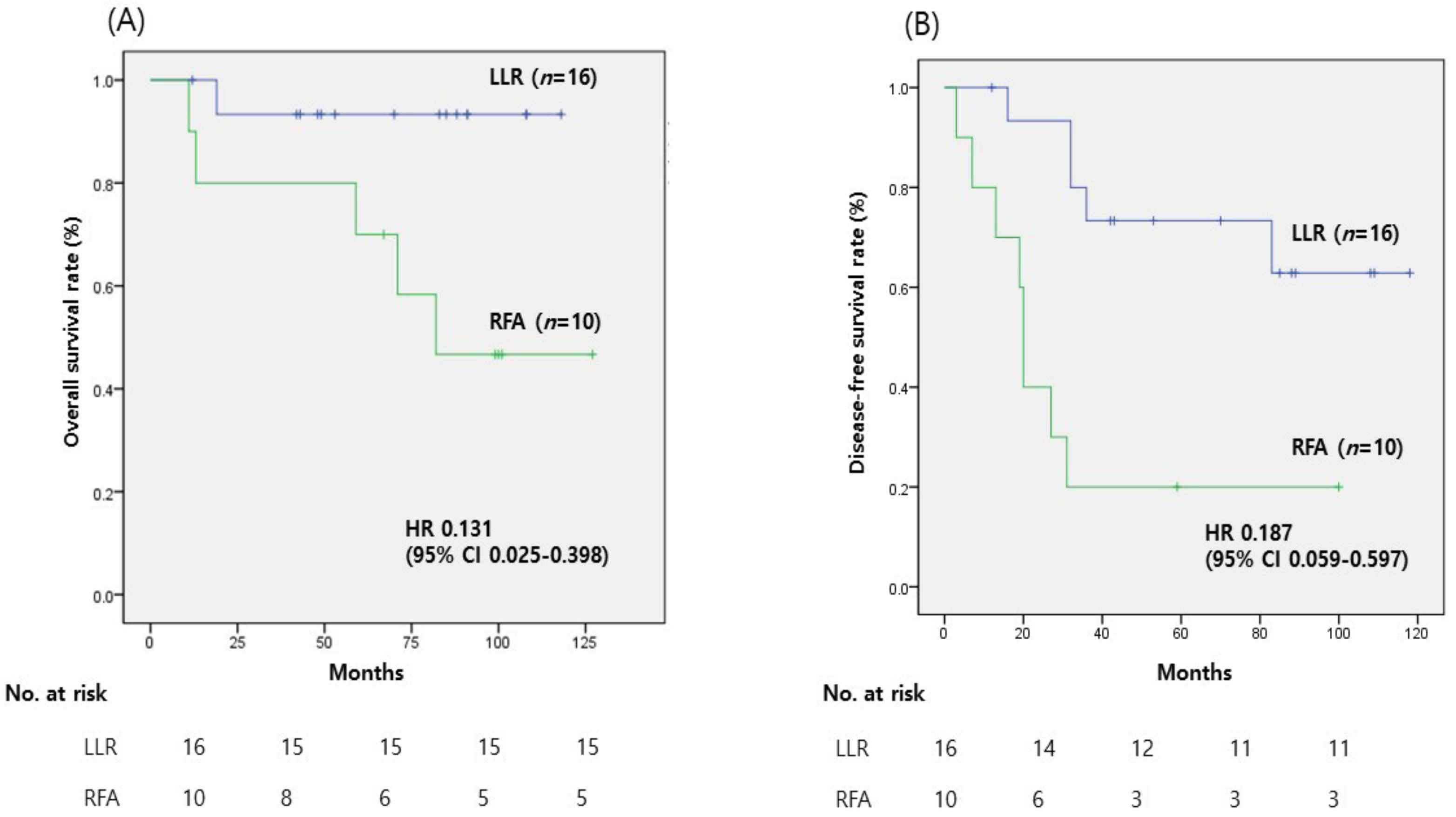
3.3. Subgroup Analyses in Patients with an AFP Level of ≥20 ng/mL
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA-Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Jinjuvadia, R.; Salami, A.; Lenhart, A.; Jinjuvadia, K.; Liangpunsakul, S.; Salgia, R. Hepatocellular Carcinoma: A Decade of Hospitalizations and Financial Burden in the United States. Am. J. Med. Sci. 2017, 354, 362–369. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J. Hepatol. 2018, 69, 182–236. [Google Scholar] [CrossRef] [PubMed]
- Bai, D.S.; Zhang, C.; Chen, P.; Jin, S.J.; Jiang, G.Q. The prognostic correlation of AFP level at diagnosis with pathological grade, progression, and survival of patients with hepatocellular carcinoma. Sci. Rep.-UK 2017, 7, 12870. [Google Scholar] [CrossRef]
- Vivarelli, M.; Bellusci, R.; Cucchetti, A.; Cavrini, G.; De Ruvo, N.; Aden, A.A.; La Barba, G.; Brillanti, S.; Cavallari, A. Low recurrence rate of hepatocellular carcinoma after liver transplantation: Better patient selection or lower immunosuppression? Transplantation 2002, 74, 1746–1751. [Google Scholar] [CrossRef]
- Marrero, J.A.; Kulik, L.M.; Sirlin, C.B.; Zhu, A.X.; Finn, R.S.; Abecassis, M.M.; Roberts, L.R.; Heimbach, J.K. Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2018, 68, 723–750. [Google Scholar] [CrossRef]
- Korean Liver Cancer Association (KLCA) and National Cancer Center (NCC) Korea. 2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma. Clin. Mol. Hepatol. 2022, 28, 583–705. [Google Scholar] [CrossRef]
- Yoon, Y.S.; Han, H.S.; Cho, J.Y.; Ahn, K.S. Total laparoscopic liver resection for hepatocellular carcinoma located in all segments of the liver. Surg. Endosc. 2010, 24, 1630–1637. [Google Scholar] [CrossRef]
- Guro, H.; Cho, J.Y.; Han, H.S.; Yoon, Y.S.; Choi, Y.; Periyasamy, M. Current status of laparoscopic liver resection for hepatocellular carcinoma. Clin. Mol. Hepatol. 2016, 22, 212–218. [Google Scholar] [CrossRef]
- Hong, S.K.; Lee, K.W.; Lee, S.; Hong, S.Y.; Suh, S.; Han, E.S.; Choi, Y.; Yi, N.J.; Suh, K.S. Impact of tumor size on hepatectomy outcomes in hepatocellular carcinoma: A nationwide propensity score matching analysis. Ann. Surg. Treat. Res. 2022, 102, 193–204. [Google Scholar] [CrossRef]
- Peng, Z.W.; Lin, X.J.; Zhang, Y.J.; Liang, H.H.; Guo, R.P.; Shi, M.; Chen, M.S. Radiofrequency ablation versus hepatic resection for the treatment of hepatocellular carcinomas 2 cm or smaller: A retrospective comparative study. Radiology 2012, 262, 1022–1033. [Google Scholar] [CrossRef]
- Xu, G.; Qi, F.Z.; Zhang, J.H.; Cheng, G.F.; Cai, Y.; Miao, Y. Meta-analysis of surgical resection and radiofrequency ablation for early hepatocellular carcinoma. World J. Surg. Oncol. 2012, 10, 163. [Google Scholar] [CrossRef]
- Ko, S.E.; Lee, M.W.; Ahn, S.; Rhim, H.; Kang, T.W.; Song, K.D.; Kim, J.M.; Choi, G.S.; Cha, D.I.; Min, J.H.; et al. Laparoscopic Hepatic Resection Versus Laparoscopic Radiofrequency Ablation for Subcapsular Hepatocellular Carcinomas Smaller Than 3 cm: Analysis of Treatment Outcomes Using Propensity Score Matching. Korean J. Radiol. 2022, 23, 615–624. [Google Scholar] [CrossRef]
- Lee, J.; Jin, Y.J.; Shin, S.K.; Kwon, J.H.; Kim, S.G.; Suh, Y.J.; Jeong, Y.; Yu, J.H.; Lee, J.W.; Kwon, O.S.; et al. Surgery versus radiofrequency ablation in patients with Child- Pugh class-A/single small (</=3 cm) hepatocellular carcinoma. Clin. Mol. Hepatol. 2022, 28, 207–218. [Google Scholar] [CrossRef]
- Song, J.; Wang, Y.; Ma, K.; Zheng, S.; Bie, P.; Xia, F.; Li, X.; Li, J.; Wang, X.; Chen, J. Laparoscopic hepatectomy versus radiofrequency ablation for minimally invasive treatment of single, small hepatocellular carcinomas. Surg. Endosc. 2016, 30, 4249–4257. [Google Scholar] [CrossRef]
- Kim, J.M.; Kang, T.W.; Kwon, C.H.; Joh, J.W.; Ko, J.S.; Park, J.B.; Rhim, H.; Lee, J.H.; Kim, S.J.; Paik, S.W. Single hepatocellular carcinoma </= 3 cm in left lateral segment: Liver resection or radiofrequency ablation? World J. Gastroenterol. 2014, 20, 4059–4065. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Yan, L.; Cheng, Z.; Wu, H.; Du, L.; Wang, J.; Xu, Y.; Zeng, Y. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann. Surg. 2010, 252, 903–912. [Google Scholar] [CrossRef] [PubMed]
- Jin, S.; Tan, S.; Peng, W.; Jiang, Y.; Luo, C. Radiofrequency ablation versus laparoscopic hepatectomy for treatment of hepatocellular carcinoma: A systematic review and meta-analysis. World J. Surg. Oncol. 2020, 18, 199. [Google Scholar] [CrossRef] [PubMed]
- Vivarelli, M.; Guglielmi, A.; Ruzzenente, A.; Cucchetti, A.; Bellusci, R.; Cordiano, C.; Cavallari, A. Surgical resection versus percutaneous radiofrequency ablation in the treatment of hepatocellular carcinoma on cirrhotic liver. Ann. Surg. 2004, 240, 102–107. [Google Scholar] [CrossRef]
- Rhim, H. Complications of radiofrequency ablation in hepatocellular carcinoma. Abdom. Imaging 2005, 30, 409–418. [Google Scholar] [CrossRef]
- Giannini, E.G.; Marenco, S.; Borgonovo, G.; Savarino, V.; Farinati, F.; Del Poggio, P.; Rapaccini, G.L.; Di Nolfo, M.A.; Benvegnu, L.; Zoli, M.; et al. Alpha-fetoprotein has no prognostic role in small hepatocellular carcinoma identified during surveillance in compensated cirrhosis. Hepatology 2012, 56, 1371–1379. [Google Scholar] [CrossRef] [PubMed]
- An, S.L.; Xiao, T.; Wang, L.M.; Rong, W.Q.; Wu, F.; Feng, L.; Liu, F.Q.; Tian, F.; Wu, J.X. Prognostic Significance of Preoperative Serum Alpha- fetoprotein in Hepatocellular Carcinoma and Correlation with Clinicopathological Factors: A Single-center Experience from China. Asian Pac. J. Cancer Prev. 2015, 16, 4421–4427. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Yoon, C.J.; Cho, J.Y.; Han, H.S.; Yoon, Y.S.; Lee, H.W.; Lee, J.S.; Kim, M.; Lee, B.; Ahn, S. Comparative long-term outcomes of laparoscopic hepatectomy and radiofrequency ablation for hepatocellular carcinoma located in the anterolateral segments of the liver. J. Hepatobiliary Pancreat Sci. 2022, 29, 349–358. [Google Scholar] [CrossRef] [PubMed]
| LLR (n = 36) | RFA (n = 40) | p-Value | |
|---|---|---|---|
| Sex (F/M) | 11 (30.6%)/25 (69.4%) | 6 (15%)/34 (85%) | 0.112 |
| Age, median (IQR) | 57.8 (±11.70) | 61.6 (±13.72) | 0.170 |
| Underlying liver disease | |||
| HBV | 30 (83.3%) | 31 (77.5%) | |
| HCV | 0 (0%) | 1 (2.5%) | |
| Alcohol | 14 (38.0%) | 7 (17.5%) | |
| NBNC | 6 (16.7%) | 8 (20%) | |
| BMI (kg/m2) | 23.09 (±4.8) | 22.86 (±3.15) | 0.804 |
| MELD score | 7.36 (±1.7) | 8.55 (±2.05) | 0.080 |
| AFP (ng/mL) | 199.6 (±415.6) | 29.4 (±68.2) | 0.020 |
| Size (cm) | 2 (±0.57) | 1.5 (±0.51) | 0.003 |
| Liver function test | |||
| Total bilirubin (mg/dL) | 0.85 (±0.3) | 0.80 (±0.48) | 0.629 |
| PT INR | 1.06 (±0.7) | 1.13 (±0.10) | 0.003 |
| Albumin (g/dL) | 4.4 (±0.3) | 3.9 (±0.44) | 0.001 |
| AST (IU/L) | 31.8 (±14.3) | 55.7 (±51.6) | 0.007 |
| ALT (IU/L) | 31.3 (±12.9) | 72.4 (±78.9) | 0.002 |
| LLR (n = 36) | RFA (n = 40) | p-Value | |
|---|---|---|---|
| Overall complications | 2 (5.6%) | 6 (15%) | 0.009 |
| Organ injury | 1 (liver) | 3 (liver, stomach, T-colon) | |
| Fluid collection | 1 (2.8%) | 0 (0%) | |
| Pulmonary complication | 1 | ||
| Other | 2 (unknown fever) | ||
| Hospital stay (days) | 4.9 (±2.76) | 2.4 (±2.88) | <0.001 |
| Early recurrence (<6 months) | 0 (0%) | 4 (10%) | 0.044 |
| Recurrence pattern | 0.023 | ||
| None | 27 (75%) | 17 (42.5%) | |
| Intrahepatic | 8 (22.2%) | 21 (52.5%) | |
| Extrahepatic | 0 (0%) | 1 (2.5%) | |
| Both intrahepatic and extrahepatic | 1 (2.8%) | 1 (2.5%) |
| LLR (n = 16) | RFA (n = 10) | p-Value | |
|---|---|---|---|
| Sex (F/M) | 6 (37.5%)/10 (62.5%) | 1 (10%)/9 (90%) | 0.999 |
| Age, median (IQR) | 53.6 (±13.9) | 58.1 (±8.81) | 0.363 |
| Underlying liver disease | |||
| HBV | 9 (90%) | 8 (80%) | |
| HCV | 1 (10%) | 0 (0%) | |
| Alcohol | 7 (43.8%) | 2 (20%) | |
| NBNC | 0 (0%) | 2 (20%) | |
| BMI (kg/m2) | 22.38 (±6.4) | 23.36 (±3.8) | 0.665 |
| MELD score | 7.49 (±1.0) | 8.2 (±2.82) | 0.360 |
| AFP (ng/mL) | 443.44 (±537.5) | 106.32 (±106.5) | 0.026 |
| Size (cm) | 2 (±0.63) | 1.4 (±0.34) | 0.017 |
| Liver function test | |||
| Total bilirubin (mg/dL) | 0.83 (±0.3) | 0.58 (±0.26) | 0.022 |
| PT INR | 1.07 (±0.9) | 1.08 (±0.7) | 0.865 |
| Albumin (g/dL) | 4.3 (±0.4) | 3.7 (±0.5) | 0.006 |
| AST (IU/L) | 35.3 (±19.8) | 86.1 (±68.2) | 0.045 |
| ALT (IU/L) | 31.9 (13.1) | 96.9 (±64.9) | 0.011 |
| LLR (n = 16) | RFA (n = 10) | p-Value | |
|---|---|---|---|
| Overall complications | 2 (12.5%) | 1 (10%) | 0.854 |
| Organ injury | 1 (6.25%, liver) | 1 (10%, stomach) | |
| Fluid collection | 0 (0%) | 0 (0%) | |
| Pulmonary complication | 1 (6.25%) | 0 (0%) | |
| Others | 0 (0%) | 0 (0%) | |
| Hospital stay (days) | 5.0 (±2.83) | 1.8 (±0.48) | <0.001 |
| Early recurrence (<6 months) | 0 (0%) | 1 (10%) | 0.343 |
| Recurrence pattern | 0.009 | ||
| None | 11 (68.8%) | 2 (20%) | |
| Intrahepatic | 5 (31.3%) | 7 (70%) | |
| Extrahepatic | 0 (0%) | 1 (10%) | |
| Both intrahepatic and extrahepatic | 0 (0%) | 0 (0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, M.; Cho, J.Y.; Han, H.-S.; Yoon, Y.-S.; Lee, H.W.; Lee, B.; Park, Y.; Kim, J.; Yoon, C.J. Comparative Study of Long-Term Outcomes of Laparoscopic Liver Resection versus Radiofrequency Ablation for Single Small Hepatocellular Carcinoma Located in Left Lateral Segments of the Liver. Medicina 2023, 59, 1063. https://doi.org/10.3390/medicina59061063
Kang M, Cho JY, Han H-S, Yoon Y-S, Lee HW, Lee B, Park Y, Kim J, Yoon CJ. Comparative Study of Long-Term Outcomes of Laparoscopic Liver Resection versus Radiofrequency Ablation for Single Small Hepatocellular Carcinoma Located in Left Lateral Segments of the Liver. Medicina. 2023; 59(6):1063. https://doi.org/10.3390/medicina59061063
Chicago/Turabian StyleKang, MeeYoung, Jai Young Cho, Ho-Seong Han, Yoo-Seok Yoon, Hae Won Lee, Boram Lee, Yeshong Park, Jinju Kim, and Chang Jin Yoon. 2023. "Comparative Study of Long-Term Outcomes of Laparoscopic Liver Resection versus Radiofrequency Ablation for Single Small Hepatocellular Carcinoma Located in Left Lateral Segments of the Liver" Medicina 59, no. 6: 1063. https://doi.org/10.3390/medicina59061063
APA StyleKang, M., Cho, J. Y., Han, H.-S., Yoon, Y.-S., Lee, H. W., Lee, B., Park, Y., Kim, J., & Yoon, C. J. (2023). Comparative Study of Long-Term Outcomes of Laparoscopic Liver Resection versus Radiofrequency Ablation for Single Small Hepatocellular Carcinoma Located in Left Lateral Segments of the Liver. Medicina, 59(6), 1063. https://doi.org/10.3390/medicina59061063






