Helical Plating Compared with Straight Plating and Nailing for Treatment of Proximal Third Humeral Shaft Fractures—A Biomechanical Study
Abstract
:1. Introduction
2. Materials and Methods
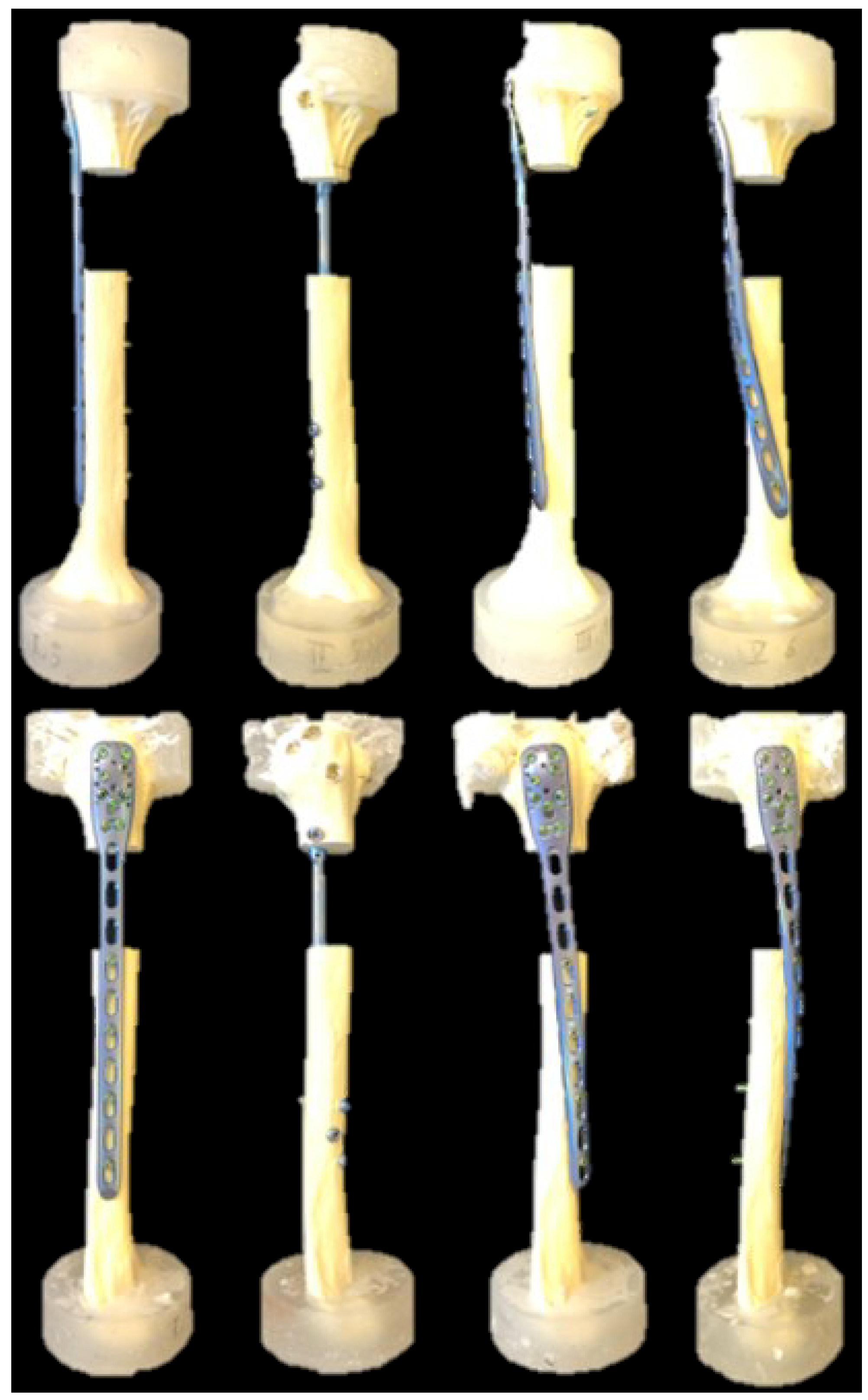
2.1. Specimens and Study Groups
2.2. Specimen Preparation/Surgical Technique
2.3. Test Setup
2.4. Loading Protocol
2.5. Data Acquisition and Analysis
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Balfour, G.W.; Mooney, V.; Ashby, M.E. Diaphyseal fractures of the humerus treated with a ready-made fracture brace. J. Bone Jt. Surg. Am. 1982, 64, 11–13. [Google Scholar] [CrossRef]
- Mann, R.J.; Neal, E.G. Fractures of the Shaft of the Humerus in Adults. South Med. J. 1965, 58, 264–268. [Google Scholar] [CrossRef] [PubMed]
- Ali, E.; Griffiths, D.; Obi, N.; Tytherleigh-Strong, G.; Van Rensburg, L. Nonoperative treatment of humeral shaft fractures revisited. J. Shoulder Elb. Surg. 2015, 24, 210–214. [Google Scholar] [CrossRef]
- Zhao, J.-G.; Wang, J.; Meng, X.-H.; Zeng, X.-T.; Kan, S.-L. Surgical interventions to treat humerus shaft fractures: A network meta-analysis of randomized controlled trials. PLoS ONE 2017, 12, e0173634. [Google Scholar] [CrossRef]
- Wen, H.; Zhu, S.; Li, C.; Chen, Z.; Yang, H.; Xu, Y. Antegrade intramedullary nail versus plate fixation in the treatment of humeral shaft fractures: An update meta-analysis. Medicine 2019, 98, e17952. [Google Scholar] [CrossRef]
- Robinson, C.M.; Khan, L.; Akhtar, A.; Whittaker, R. The extended deltoid-splitting approach to the proximal humerus. J. Orthop. Trauma 2007, 21, 657–662. [Google Scholar] [CrossRef]
- Benninger, E.; Meier, C. Minimally invasive lateral plate placement for metadiaphyseal fractures of the humerus and its implications for the distal deltoid insertion- it is not only about the radial nerve. A cadaveric study. Injury 2017, 48, 615–620. [Google Scholar] [CrossRef]
- Tan, J.C.H.; Kagda, F.H.Y.; Murphy, D.; Thambiah, J.S.; Khong, K.S. Minimally invasive helical plating for shaft of humerus fractures: Technique and outcome. Open Orthop. J. 2012, 6, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.H. Helical plate fixation for treatment of comminuted fractures of the proximal and middle one-third of the humerus. Injury 2005, 36, 75–80. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, T.; Rummel, F.; Knop, C.; Merkle, T. Shoulder function after helical long PHILOS plate. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 1463–1469. [Google Scholar] [CrossRef]
- Da Silva, T.; Rummel, F.; Knop, C.; Merkle, T. Comparing iatrogenic radial nerve lesions in humeral shaft fractures treated with helical or straight PHILOS plates: A 10-year retrospective cohort study of 62 cases. Arch. Orthop. Trauma Surg. 2020, 140, 1931–1937. [Google Scholar] [CrossRef] [PubMed]
- Dauwe, J.; Grechenig, P.; Unterfrauner, I.; Schwarz, A.; Weiglein, A.; Hohenberger, G. Axillary nerve elongation in humeral fracture plating: A cadaveric study for comparison between straight and helical Philos plates. J. Orthop. 2020, 19, 233–236. [Google Scholar] [CrossRef]
- Arumilli, B.; Suhm, N.; Marcel, J.; Rikli, D. Long PHILOS plate fixation in a series of humeral fractures. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 1383–1387. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.-G.; Kwon, H.-N.; Biraris, S.; Shon, W.-Y. Minimally invasive plate osteosynthesis using a helical plate for metadiaphyseal complex fractures of the proximal humerus. Orthopedics 2014, 37, e237–e243. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Hu, J.; Guan, J.; Chen, Y.; Wang, L. Proximal third humeral shaft fractures fixed with long helical PHILOS plates in elderly patients: Benefit of pre-contouring plates on a 3D-printed model-a retrospective study. J. Orthop. Surg. Res. 2018, 13, 203. [Google Scholar] [CrossRef]
- Stoffel, K.; Dieter, U.; Stachowiak, G.; Gächter, A.; Kuster, M.S. Biomechanical testing of the LCP--how can stability in locked internal fixators be controlled? Injury 2003, 34 (Suppl. 2), B11–B19. [Google Scholar] [CrossRef]
- Anglin, C.; Wyss, U.P. Review of arm motion analyses. Proc. Inst. Mech. Eng. H 2000, 214, 541–555. [Google Scholar] [CrossRef]
- Pastor, T.; Zderic, I.; Gehweiler, D.; Gardner, M.J.; Stoffel, K.; Richards, G.; Knobe, M.; Gueorguiev, B. Biomechanical analysis of recently released cephalomedullary nails for trochanteric femoral fracture fixation in a human cadaveric model. Arch. Orthop. Trauma Surg. 2021, 142, 3787–3796. [Google Scholar] [CrossRef]
- Pastor, T.; Zderic, I.; van Knegsel, K.P.; Beeres, F.J.P.; Migliorini, F.; Babst, R.; Nebelung, S.; Ganse, B.; Schoeneberg, C.; Gueorguiev, B.; et al. Biomechanical analysis of helical versus straight plating of proximal third humeral shaft fractures. Arch. Orthop. Trauma Surg. 2023, 143, 4983–4991. [Google Scholar] [CrossRef]
- Pastor, T.; Zderic, I.; Schopper, C.; Haefeli, P.C.; Kastner, P.; Souleiman, F.; Gueorguiev, B.; Knobe, M. Impact of Anterior Malposition and Bone Cement Augmentation on the Fixation Strength of Cephalic Intramedullary Nail Head Elements. Medicina 2022, 58, 1636. [Google Scholar] [CrossRef]
- Horn, J.; Gueorguiev, B.; Brianza, S.; Steen, H.; Schwieger, K. Biomechanical evaluation of two-part surgical neck fractures of the humerus fixed by an angular stable locked intramedullary nail. J. Orthop. Trauma 2011, 25, 406–413. [Google Scholar] [CrossRef] [PubMed]
- Pastor, T.; Knobe, M.; van de Wall, B.J.M.; Rompen, I.F.; Zderic, I.; Visscher, L.; Link, B.C.; Babst, R.; Gueorguiev, B.; Beeres, F.J.P. Low-profile dual mini-fragment plating of diaphyseal clavicle fractures. A biomechanical comparative testing. Clin. Biomech. 2022, 94, 105634. [Google Scholar] [CrossRef]
- Pastor, T.; Zderic, I.; Berk, T.; Souleiman, F.; Vögelin, E.; Beeres, F.J.; Gueorguiev, B.; Pastor, T. New Generation of Superior Single Plating vs Low-Profile Dual Mini-Fragment Plating in Diaphyseal Clavicle Fractures. A Biomechanical Comparative Study. J. Shoulder Elb. Surg. 2023, in press. [Google Scholar] [CrossRef]
- Fernández Dell’Oca, A.A. The principle of helical implants. Unusual ideas worth considering. Injury 2002, 33 (Suppl. 1), SA1–SA27. [Google Scholar] [CrossRef] [PubMed]
- Déjardin, L.M.; Guiot, L.P.; von Pfeil, D.J.F. Interlocking nails and minimally invasive osteosynthesis. Vet. Clin. N. Am. Small Anim. Pract. 2012, 42, 935–962. [Google Scholar] [CrossRef]
- Garlock, A.N.; Donovan, J.; LeCronier, D.J.; Houghtaling, J.; Burton, S.; Atkinson, P.J. A modified intramedullary nail interlocking design yields improved stability for fatigue cycling in a canine femur fracture model. Proc. Inst. Mech. Eng. H 2012, 226, 469–476. [Google Scholar] [CrossRef]
- Nourisa, J.; Rouhi, G. Biomechanical evaluation of intramedullary nail and bone plate for the fixation of distal metaphyseal fractures. J. Mech. Behav. Biomed. Mater. 2016, 56, 34–44. [Google Scholar] [CrossRef]
- Flanagan, B.P.; LeCronier, D.; Kubacki, M.R.; Telehowski, P.; Atkinson, P. A Method to Modify Angle-Stable Intramedullary Nail Construct Compliance. Iowa Orthop. J. 2014, 34, 68–73. [Google Scholar] [PubMed]
- Gautier, E.; Sommer, C. Guidelines for the clinical application of the LCP. Injury 2003, 34 (Suppl. 2), B63–B76. [Google Scholar] [CrossRef]
- Zhang, L.; Chen, L.-W.; Zhang, W.-J.; Zhao, C.-M.; Huang, B.; Yu, Q.; Ni, B. Treatment of proximal and middle one-third humeral fractures with lateral distal tibial helical plate. Eur. J. Orthop. Surg. Traumatol. 2012, 22, 673–679. [Google Scholar] [CrossRef]
- Gardner, M.J.; Griffith, M.H.; Lorich, D.G. Helical plating of the proximal humerus. Injury 2005, 36, 1197–1200. [Google Scholar] [CrossRef]
- Ekdahl, M.; Dominguez, C.; Pinedo, M.; López, S.; Gutiérrez, V. New precontoured long locking plate for proximal metadiaphyseal fractures of the humerus: A cadaveric study for its use with the minimally invasive technique. JSES Int. 2021, 5, 540–545. [Google Scholar] [CrossRef]
- Argyropoulos, M.; Kent, M. Early Results of the A.L.P.S. Proximal Humerus Locking Plate. Open Orthop. J. 2018, 12, 53–58. [Google Scholar] [CrossRef]
- Zamboni, C.; Carmo, B.L.; Moraes, L.V.M.; Hungria, J.O.S.; Mercadante, M.T.; Fucs, P.M.M.B. A practical guide for the use of contour locking plates for the repair of humeral diaphyseal fractures with proximal extension. Injury 2019, 50, 2247–2251. [Google Scholar] [CrossRef] [PubMed]
- Pastor, T.; Kastner, P.; Souleiman, F.; Gehweiler, D.; Migliorini, F.; Link, B.-C.; Beeres, F.J.P.; Babst, R.; Nebelung, S.; Ganse, B.; et al. Anatomical analysis of different helical plate designs for proximal humeral shaft fracture fixation. Eur. J. Trauma Emerg. Surg. 2022, 49, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Pastor, T.; Beeres, F.J.P.; Kastner, P.; Gehweiler, D.; Migliorini, F.; Nebelung, S.; Scaglioni, M.F.; Souleiman, F.; Link, B.C.; Babst, R.; et al. Anatomical analysis of different helical plate designs for distal femoral fracture fixation. Injury 2022, 53, 2636–2641. [Google Scholar] [CrossRef] [PubMed]

| Parameter of Interest | Group 1 (Straight) | Group 2 (Nail) | Group 3 (45°-Helical) | Group 4 (90°-Helical) |
|---|---|---|---|---|
| Stiffness | ||||
| Axial (Nm/mm) | 66.4 ± 22.9 | 363.8 ± 133.2 | 74.8 ± 27.4 | 55.9 ± 19.2 |
| Flexion (Nm/°) | 0.84 ± 0.10 | 0.66 ± 0.07 | 0.72 ± 0.05 | 0.59 ± 0.14 |
| Extension (Nm/°) | 0.85 ± 0.14 | 0.69 ± 0.12 | 0.69 ± 0.09 | 0.56 ± 0.09 |
| Varus (Nm/°) | 0.66 ± 0.05 | 0.84 ± 0.12 | 0.65 ± 0.10 | 0.79 ± 0.07 |
| Valgus (Nm/°) | 0.65 ± 0.04 | 0.77 ± 0.19 | 0.64 ± 0.08 | 0.75 ± 0.07 |
| Torsional–internal rotation (Nm/°) | 0.32 ± 0.02 | 0.33 ± 0.05 | 0.31 ± 0.03 | 0.31 ± 0.04 |
| Torsional–external rotation (Nm/°) | 0.33 ± 0.02 | 0.34 ± 0.07 | 0.30 ± 0.02 | 0.31 ± 0.04 |
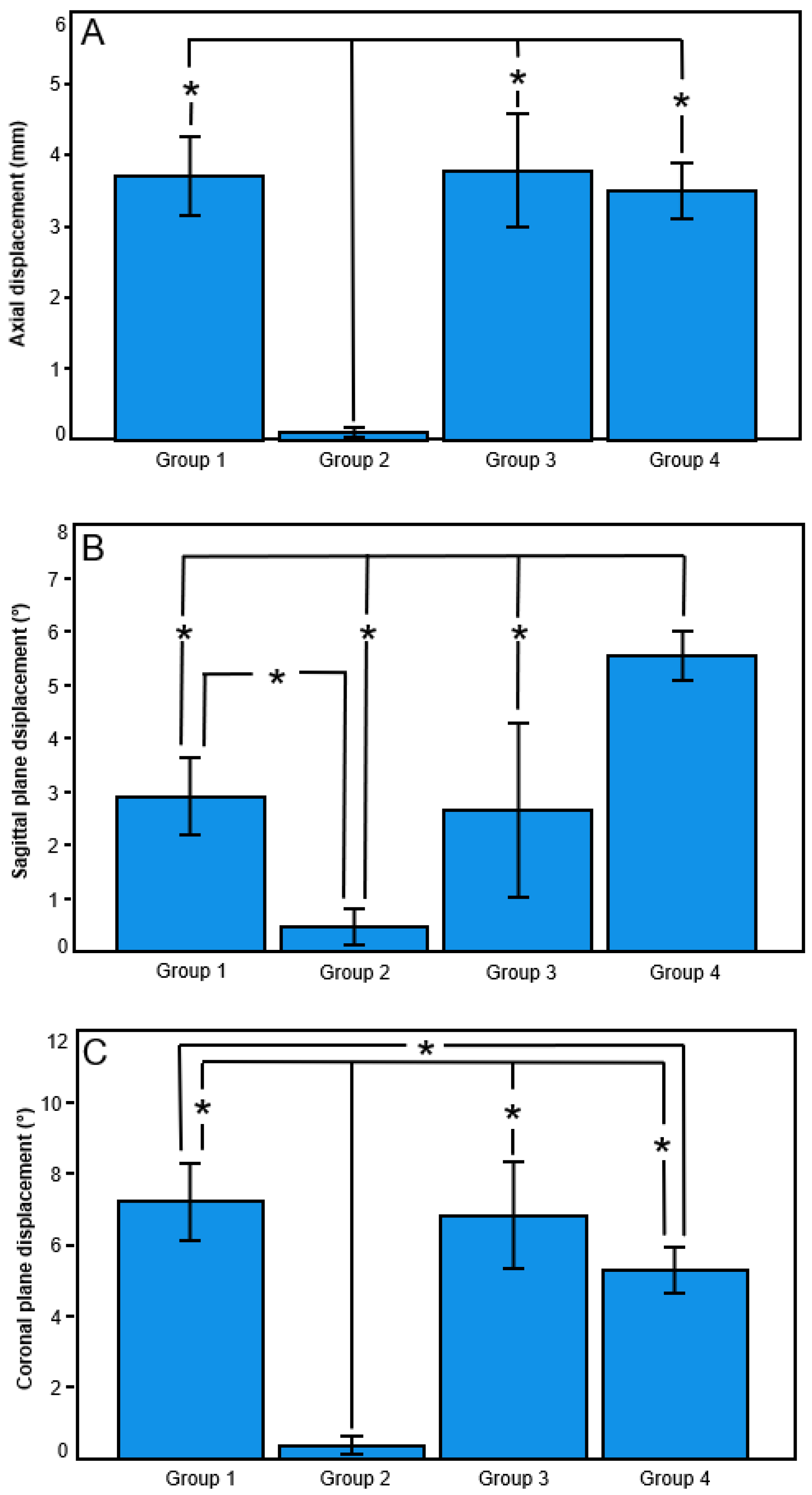
| Displacement under axial compression | ||||
| Axial (mm) | 3.71 ± 0.55 | 0.11 ± 0.06 | 3.79 ± 0.79 | 3.49 ± 0.39 |
| Sagittal plane (°) | 2.91 ± 0.72 | 0.48 ± 0.34 | 2.65 ± 1.62 | 5.53 ± 0.46 |
| Coronal plane (°) | 7.22 ± 1.08 | 0.37 ± 0.25 | 6.82 ± 1.49 | 5.28 ± 0.63 |
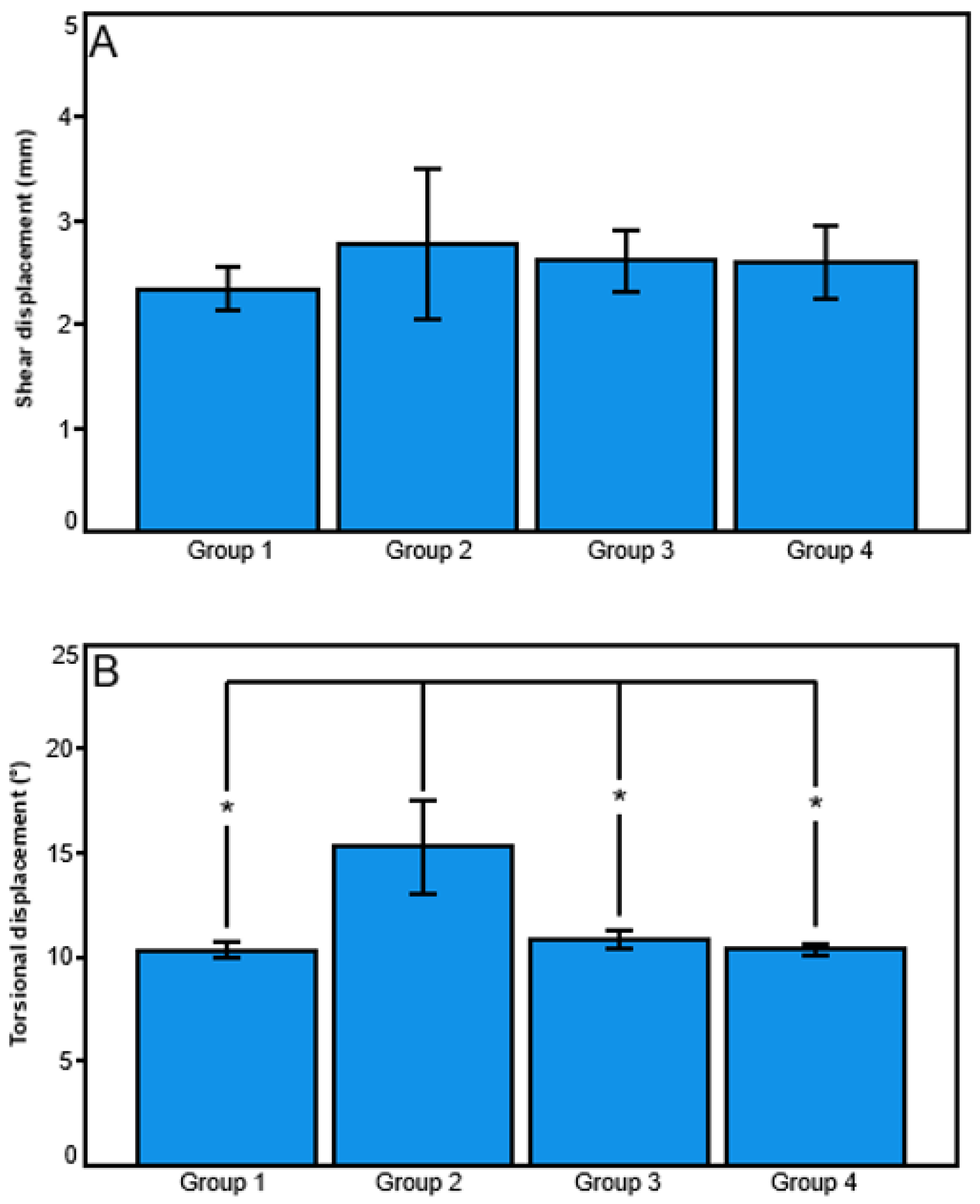
| Displacement under torsion in internal and external rotation | ||||
| Shear (mm) | 2.34 ± 0.20 | 2.77 ± 0.73 | 2.62 ± 0.30 | 2.60 ± 0.36 |
| Torsional (°) | 10.30 ± 0.38 | 15.31 ± 2.27 | 10.85 ± 0.42 | 10.35 ± 0.30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pastor, T.; Zderic, I.; Pastor, T.; Drenchev, L.; Skulev, H.K.; van Knegsel, K.P.; Lenz, M.; Link, B.-C.; Gueorguiev, B.; Beeres, F.J.P. Helical Plating Compared with Straight Plating and Nailing for Treatment of Proximal Third Humeral Shaft Fractures—A Biomechanical Study. Medicina 2023, 59, 2043. https://doi.org/10.3390/medicina59112043
Pastor T, Zderic I, Pastor T, Drenchev L, Skulev HK, van Knegsel KP, Lenz M, Link B-C, Gueorguiev B, Beeres FJP. Helical Plating Compared with Straight Plating and Nailing for Treatment of Proximal Third Humeral Shaft Fractures—A Biomechanical Study. Medicina. 2023; 59(11):2043. https://doi.org/10.3390/medicina59112043
Chicago/Turabian StylePastor, Torsten, Ivan Zderic, Tatjana Pastor, Ludmil Drenchev, Hristo Kostov Skulev, Kenneth P. van Knegsel, Mark Lenz, Björn-Christian Link, Boyko Gueorguiev, and Frank J. P. Beeres. 2023. "Helical Plating Compared with Straight Plating and Nailing for Treatment of Proximal Third Humeral Shaft Fractures—A Biomechanical Study" Medicina 59, no. 11: 2043. https://doi.org/10.3390/medicina59112043
APA StylePastor, T., Zderic, I., Pastor, T., Drenchev, L., Skulev, H. K., van Knegsel, K. P., Lenz, M., Link, B.-C., Gueorguiev, B., & Beeres, F. J. P. (2023). Helical Plating Compared with Straight Plating and Nailing for Treatment of Proximal Third Humeral Shaft Fractures—A Biomechanical Study. Medicina, 59(11), 2043. https://doi.org/10.3390/medicina59112043








