Augmented Corticotomy on the Lingual Side in Mandibular Anterior Region Assisting Orthodontics in Protrusive Malocclusion: A Case Report
Abstract
:1. Introduction
2. Case Report
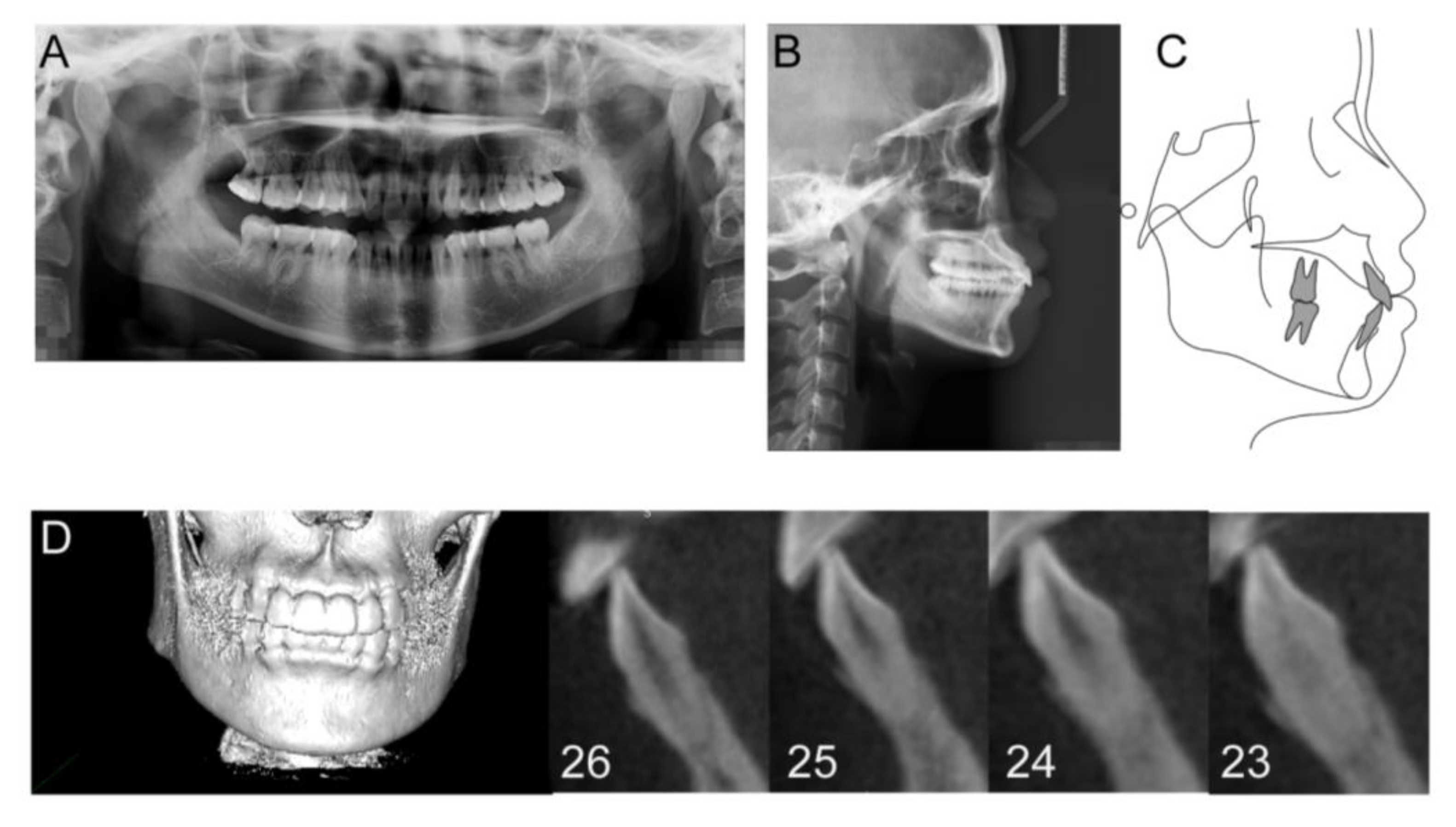
2.1. Diagnosis and Etiology
2.2. Treatment Objectives
2.3. Treatment Alternatives
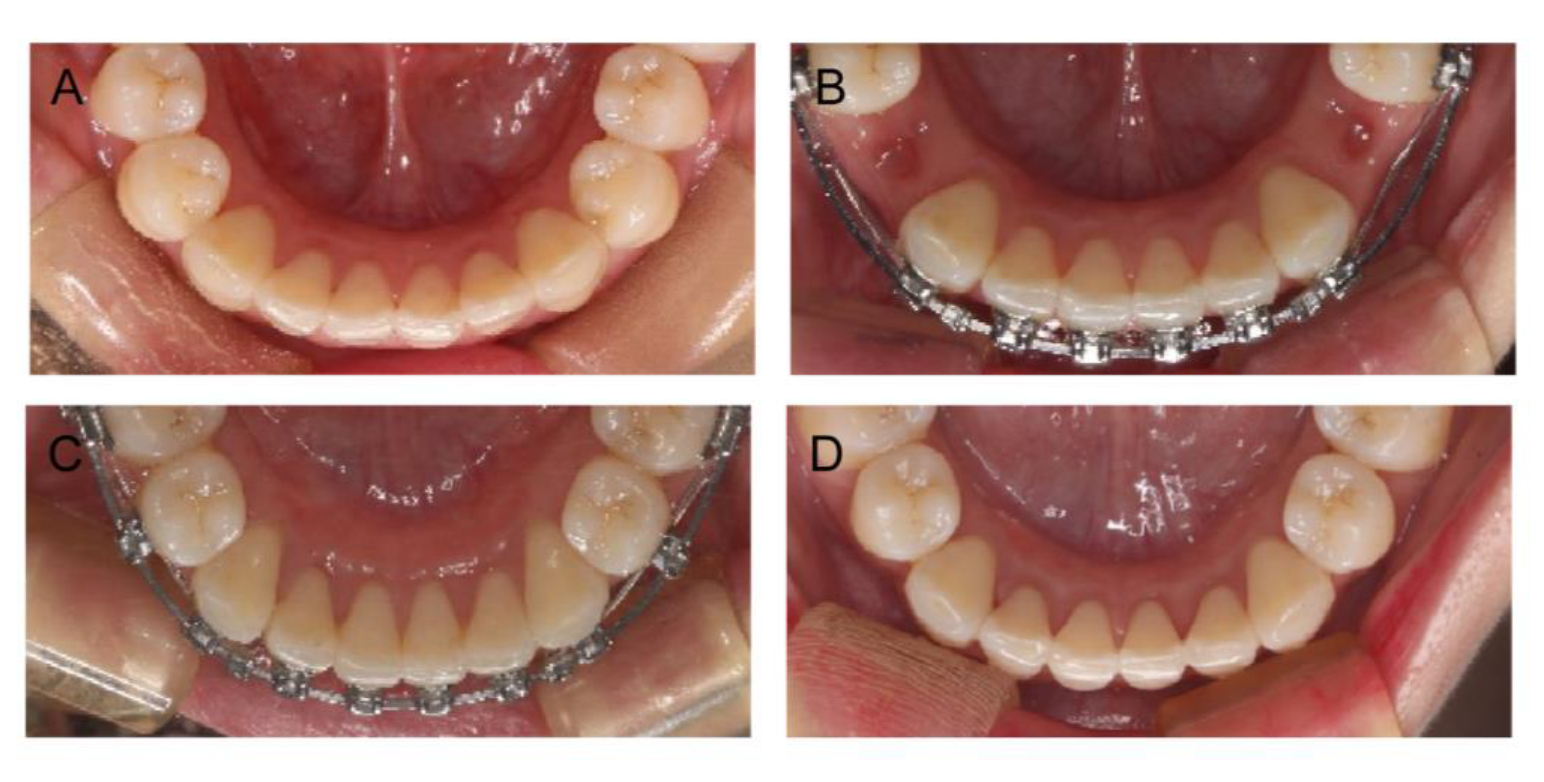
2.4. Treatment Progress
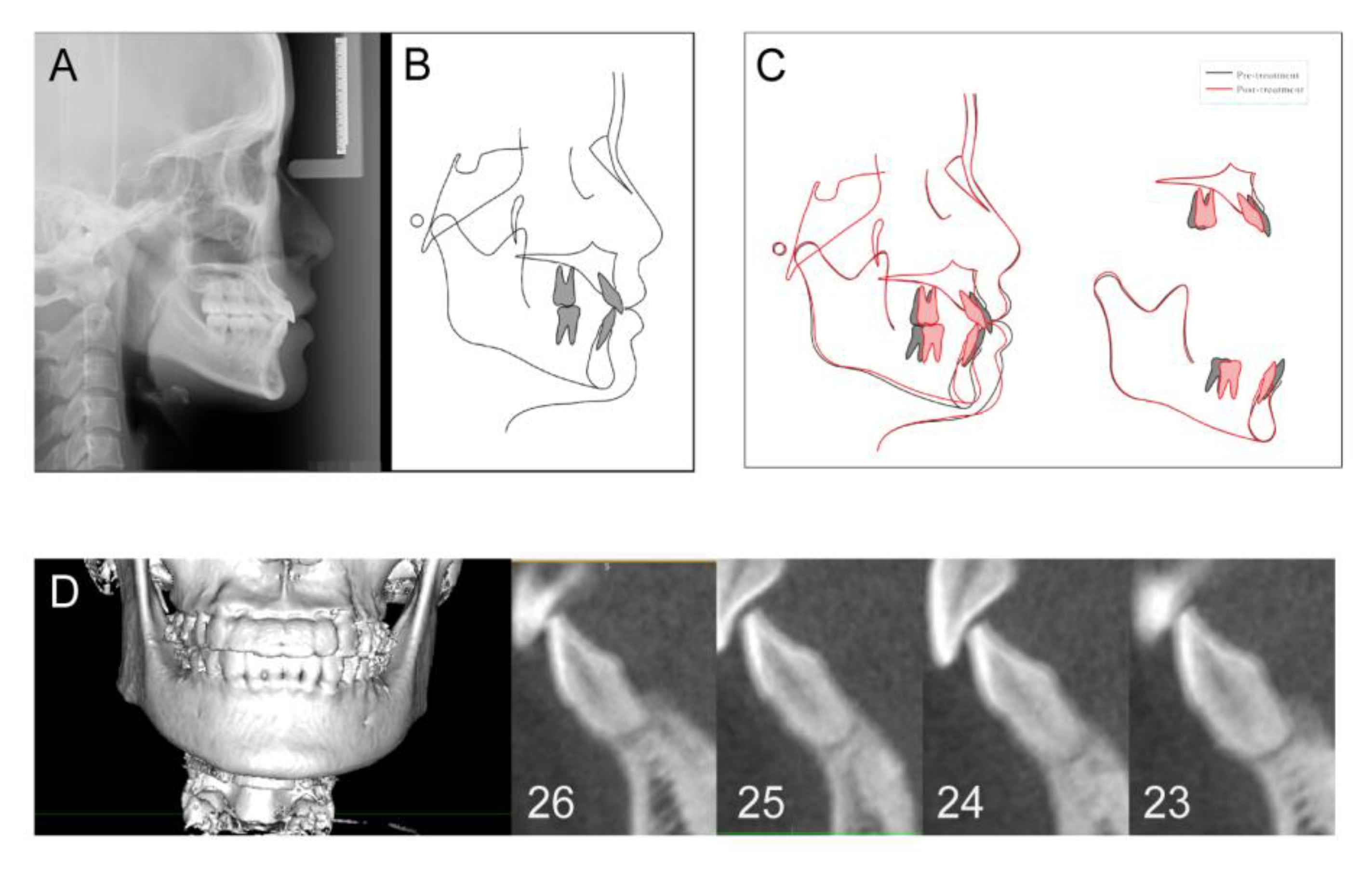
2.5. Treatment Results
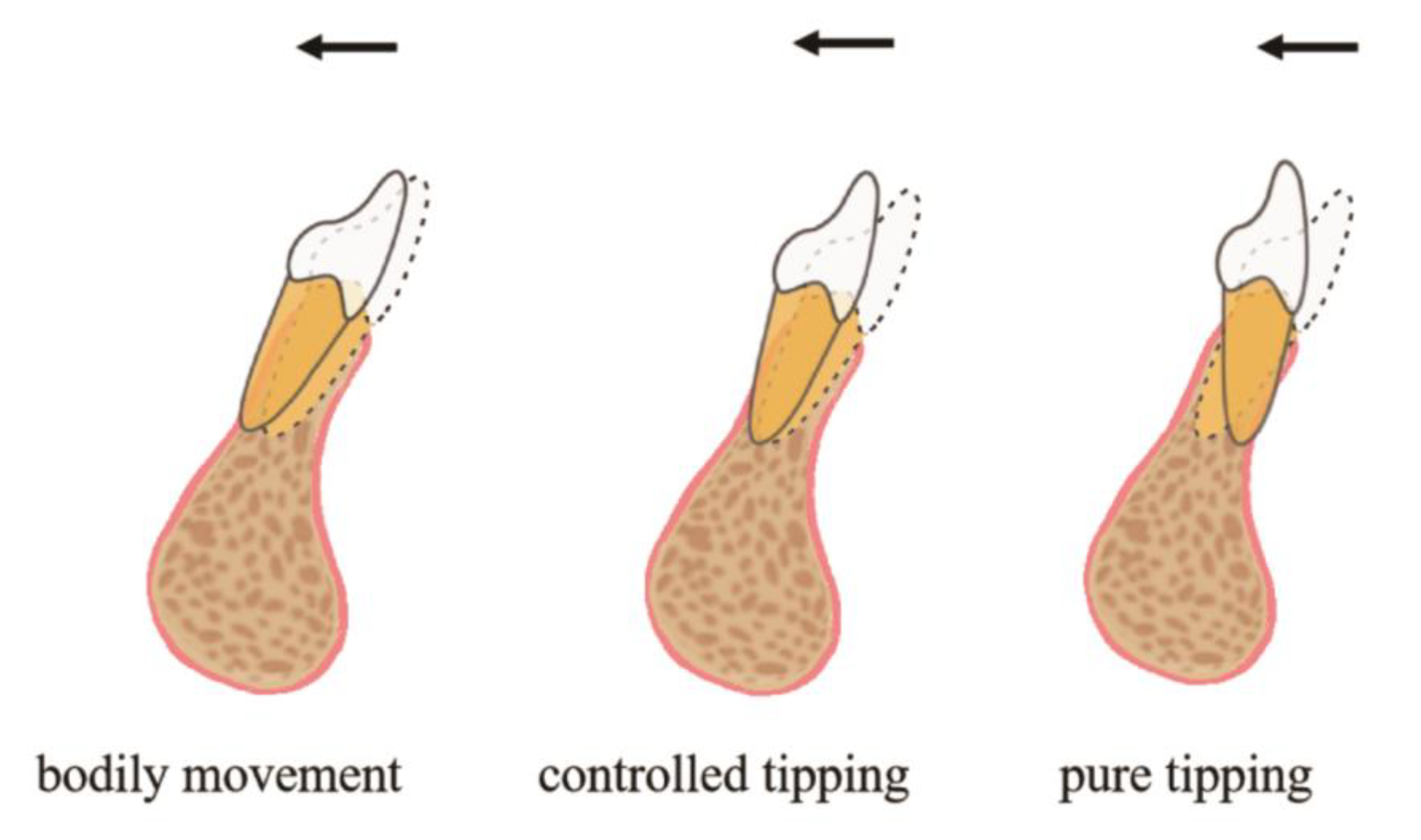
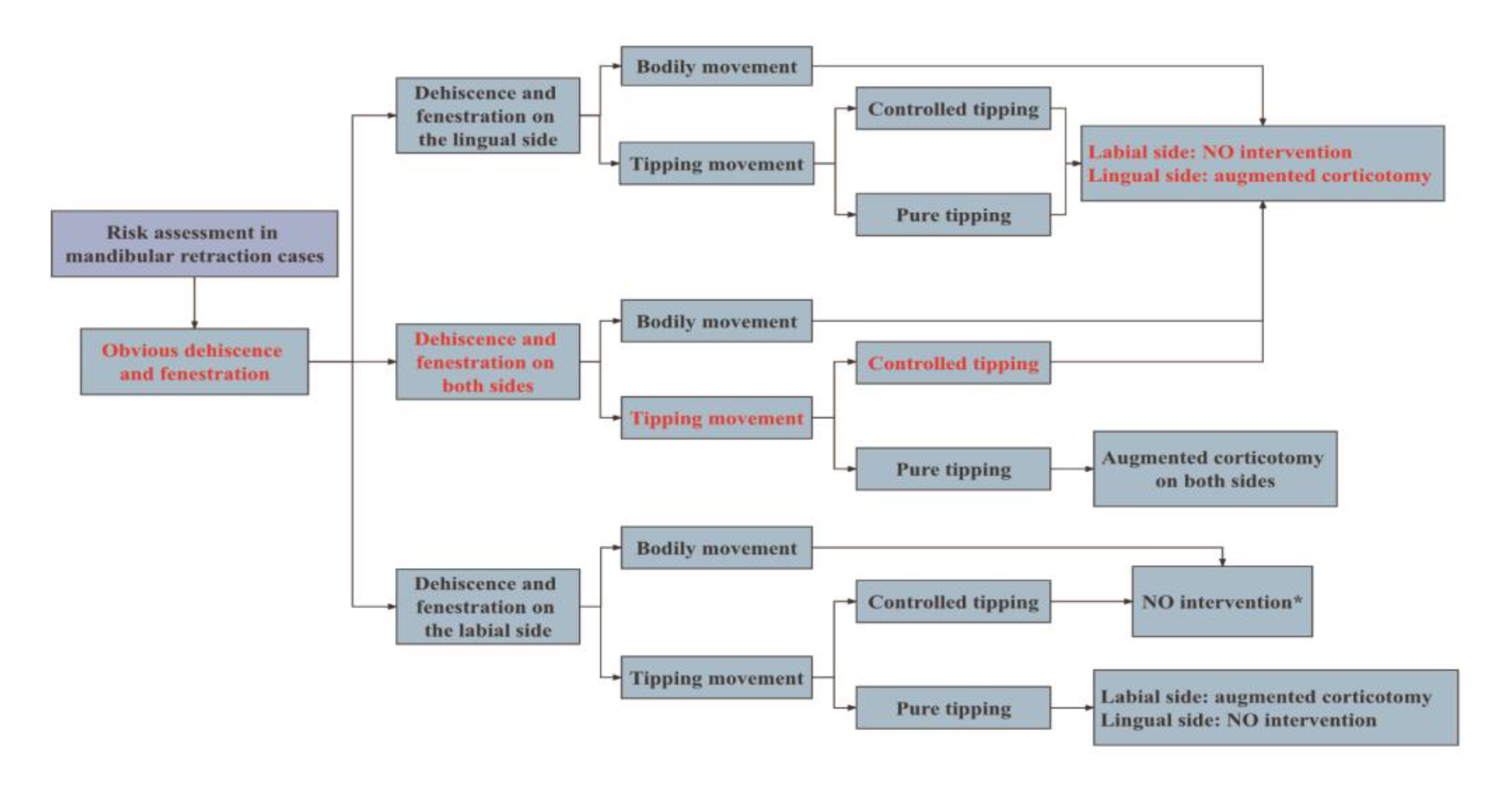
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ruetters, M.; Gehrig, H.; Kronsteiner, D.; Doll, S.; Kim, T.S.; Lux, C.J.; Sen, S. Low-dose CBCT imaging of alveolar buccal bone adjacent to mandibular anterior teeth—A pilot study. Clin. Oral Investig. 2022, 26, 4173–4182. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Cha, K.S.; Lee, J.W.; Lee, S.M. Mandibular skeletal posterior anatomic limit for molar distalization in patients with Class III malocclusion with different vertical facial patterns. Korean J. Orthod. 2021, 51, 250–259. [Google Scholar] [CrossRef]
- Lemos Rinaldi, M.R.; Azeredo, F.; Martinelli de Lima, E.; Deon Rizzatto, S.M.; Sameshima, G.; Macedo de Menezes, L. Cone-beam computed tomography evaluation of bone plate and root length after maxillary expansion using tooth-borne and tooth-tissue-borne banded expanders. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 504–516. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Nguyen, T.; Oberoi, S.; Oh, H.; Kapila, S.; Kao, R.T.; Lin, G.H. The Significance of Utilizing A Corticotomy on Periodontal and Orthodontic Outcomes: A Systematic Review and Meta-Analysis. Biology 2021, 10, 803. [Google Scholar] [CrossRef] [PubMed]
- Frost, H.M. The regional acceleratory phenomenon: A review. Henry Hosp. Med. J. 1983, 31, 3–9. [Google Scholar]
- Wilcko, W.M.; Wilcko, T.; Bouquot, J.E.; Ferguson, D.J. Rapid orthodontics with alveolar reshaping: Two case reports of decrowding. Int. J. Periodontics Restor. Dent. 2001, 21, 9–19. [Google Scholar]
- Wang, C.W.; Yu, S.H.; Mandelaris, G.A.; Wang, H.L. Is periodontal phenotype modification therapy beneficial for patients receiving orthodontic treatment? An American Academy of Periodontology best evidence review. J. Periodontol. 2020, 91, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Kao, R.T.; Curtis, D.A.; Kim, D.M.; Lin, G.H.; Wang, C.W.; Cobb, C.M.; Hsu, Y.T.; Kan, J.; Velasquez, D.; Avila-Ortiz, G.; et al. American Academy of Periodontology best evidence consensus statement on modifying periodontal phenotype in preparation for orthodontic and restorative treatment. J. Periodontol. 2020, 91, 289–298. [Google Scholar] [CrossRef]
- Nimeri, G.; Kau, C.H.; Abou-Kheir, N.S.; Corona, R. Acceleration of tooth movement during orthodontic treatment—A frontier in orthodontics. Prog. Orthod. 2013, 14, 42. [Google Scholar] [CrossRef]
- Zeitounlouian, T.S.; Zeno, K.G.; Brad, B.A.; Haddad, R.A. Three-dimensional evaluation of the effects of injectable platelet rich fibrin (i-PRF) on alveolar bone and root length during orthodontic treatment: A randomized split mouth trial. BMC Oral Health 2021, 21, 92. [Google Scholar] [CrossRef]
- Jing, W.D.; Xu, L.; Li, X.T.; Xu, X.; Jiao, J.; Hou, J.X.; Wang, X.X. Prevalence of and risk factors for alveolar fenestration and dehiscence in the anterior teeth of Chinese patients with skeletal Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 312–320. [Google Scholar] [CrossRef] [PubMed]
- Peñarrocha-Diago, M.; Balaguer-Martí, J.C.; Peñarrocha-Oltra, D.; Bagán, J.; Peñarrocha-Diago, M.; Flanagan, D. Floor of the mouth hemorrhage subsequent to dental implant placement in the anterior mandible. Clin. Cosmet. Investig. Dent. 2019, 11, 235–242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, D.M.; Neiva, R. Periodontal soft tissue non-root coverage procedures: A systematic review from the AAP Regeneration Workshop. J. Periodontol. 2015, 86, S56–S72. [Google Scholar] [CrossRef] [PubMed]
- Talic, N.F. Adverse effects of orthodontic treatment: A clinical perspective. Saudi Dent. J. 2011, 23, 55–59. [Google Scholar] [CrossRef]
- Samruajbenjakun, B.; Kanokpongsak, K.; Leethanakul, C. Comparison of clinical and histological characteristics of orthodontic tooth movement into recent and healed extraction sites combined with corticotomy in rats. Korean J. Orthod. 2018, 48, 405–411. [Google Scholar] [CrossRef]
- Häsler, R.; Schmid, G.; Ingervall, B.; Gebauer, U. A clinical comparison of the rate of maxillary canine retraction into healed and recent extraction sites—A pilot study. Eur. J. Orthod. 1997, 19, 711–719. [Google Scholar] [CrossRef]
- Diedrich, P.; Wehrbein, H. Orthodontic retraction into recent and healed extraction sites. A histologic study. J. Orofac Orthop 1997, 58, 90–99. [Google Scholar] [CrossRef]
- Bertl, K.; Neuner, H.; Meran, A.; Bertl, M.H.; Reich, I.; Nemec, M.; Bruckmann, C.; Stavropoulos, A.; Bantleon, H.P. Does the time-point of orthodontic space closure initiation after tooth extraction affect the incidence of gingival cleft development? A randomized controlled clinical trial. J. Periodontol. 2020, 91, 572–581. [Google Scholar] [CrossRef]
- Sun, L.; Yuan, L.; Wang, B.; Zhang, L.; Shen, G.; Fang, B. Changes of alveolar bone dehiscence and fenestration after augmented corticotomy-assisted orthodontic treatment: A CBCT evaluation. Prog. Orthod. 2019, 20, 7. [Google Scholar] [CrossRef]
- Brugnami, F.; Caiazzo, A.; Signorelli, L.; Capri, D. Regenerative Orthodontics: GBR and Corticotomy to Stretch the Limits of Orthodontic Treatment. Int. J. Periodontics Restor. Dent. 2021, 41, 105–111. [Google Scholar] [CrossRef]
- Mandelaris, G.A.; Vence, B.S.; Rosenfeld, A.L.; Forbes, D.P. A classification system for crestal and radicular dentoalveolar bone phenotypes. Int. J. Periodontics Restor. Dent. 2013, 33, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Makki, L.; Ferguson, D.J.; Wilcko, M.T.; Wilcko, W.M.; Bjerklin, K.; Stapelberg, R.; Al-Mulla, A. Mandibular irregularity index stability following alveolar corticotomy and grafting: A 10-year preliminary study. Angle Orthod. 2015, 85, 743–749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fu, T.; Liu, S.; Zhao, H.; Cao, M.; Zhang, R. Effectiveness and Safety of Minimally Invasive Orthodontic Tooth Movement Acceleration: A Systematic Review and Meta-analysis. J. Dent. Res. 2019, 98, 1469–1479. [Google Scholar] [CrossRef] [PubMed]
- Rekhi, U.; Catunda, R.Q.; Gibson, M.P. Surgically accelerated orthodontic techniques and periodontal response: A systematic review. Eur. J. Orthod. 2020, 42, 635–642. [Google Scholar] [CrossRef] [PubMed]




| Measurement | Normal (Standard Deviation) | Pretreatment | Posttreatment | Difference |
|---|---|---|---|---|
| SNA (°) | 83.1 (2.7) | 82.0 | 81.9 | −0.1 |
| SNB (°) | 80.3 (2.6) | 79.2 | 80.0 | 0.8 |
| ANB (°) | 2.7 (1.8) | 2.8 | 1.9 | −0.9 |
| UI—SN (°) | 103.4 (5.5) | 105.8 | 108.4 | 2.6 |
| LI—MP (°) | 96.3 (5.4) | 105.2 | 90.7 | −14.5 |
| UI-LI (°) | 129.1 (7.1) | 118.1 | 131.1 | 13 |
| MP—SN (°) | 32.6 (6.9) | 30.9 | 29.8 | −1.1 |
| MP—FH (°) | 25.5 (4.8) | 26.1 | 25.1 | −1.0 |
| Wits (mm) | −1 (1) | −0.8 | −1 | 0.2 |
| PP-OP (°) | 10 (4) | 7.3 | 5.1 | −2.2 |
| P-A Face Height (%) | 65 (4) | 67.5 | 68.4 | 0.9 |
| Y-Axis (°) | 67 (5.5) | 68.2° | 66.7 | −1.5 |
| UL-E (mm) | −1.6 (1.5) | −0.1 | −1.8 | −1.7 |
| LL-E (mm) | −0.2 (1.9) | 4.1 | −0.6 | −4.7 |
| Tooth | 26 | 25 | 24 | 23 | Mean ± SD |
|---|---|---|---|---|---|
| Lingual (mm2) | 1.49 | 1.74 | 1.82 | 1.09 | 1.54 ± 0.33 |
| Labial (mm2) | 0.68 | 1.86 | 0.68 | 0.94 | 1.04 ± 0.56 |
| Tooth | 26 | 25 | 24 | 23 | Mean ± SD |
|---|---|---|---|---|---|
| Coronal (mm) | 0.40 | 0.63 | 0.30 | 2.11 | 0.86 ± 0.84 |
| Middle (mm) | 1.14 | 0.88 | 0.76 | 2.22 | 1.25 ± 0.67 |
| Apical (mm) | 0.26 | 1.14 | 0.31 | 1.87 | 0.72 ± 0.77 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lu, Y.; Liu, H.; Liu, J.; Chen, M. Augmented Corticotomy on the Lingual Side in Mandibular Anterior Region Assisting Orthodontics in Protrusive Malocclusion: A Case Report. Medicina 2022, 58, 1181. https://doi.org/10.3390/medicina58091181
Lu Y, Liu H, Liu J, Chen M. Augmented Corticotomy on the Lingual Side in Mandibular Anterior Region Assisting Orthodontics in Protrusive Malocclusion: A Case Report. Medicina. 2022; 58(9):1181. https://doi.org/10.3390/medicina58091181
Chicago/Turabian StyleLu, Yun, Haohao Liu, Jialiang Liu, and Meihua Chen. 2022. "Augmented Corticotomy on the Lingual Side in Mandibular Anterior Region Assisting Orthodontics in Protrusive Malocclusion: A Case Report" Medicina 58, no. 9: 1181. https://doi.org/10.3390/medicina58091181
APA StyleLu, Y., Liu, H., Liu, J., & Chen, M. (2022). Augmented Corticotomy on the Lingual Side in Mandibular Anterior Region Assisting Orthodontics in Protrusive Malocclusion: A Case Report. Medicina, 58(9), 1181. https://doi.org/10.3390/medicina58091181





