Combined Application of Virtual Simulation Technology and 3-Dimensional-Printed Computer-Aided Rapid Prototyping in Autotransplantation of a Mature Third Molar
Abstract
:1. Introduction
2. Case Report
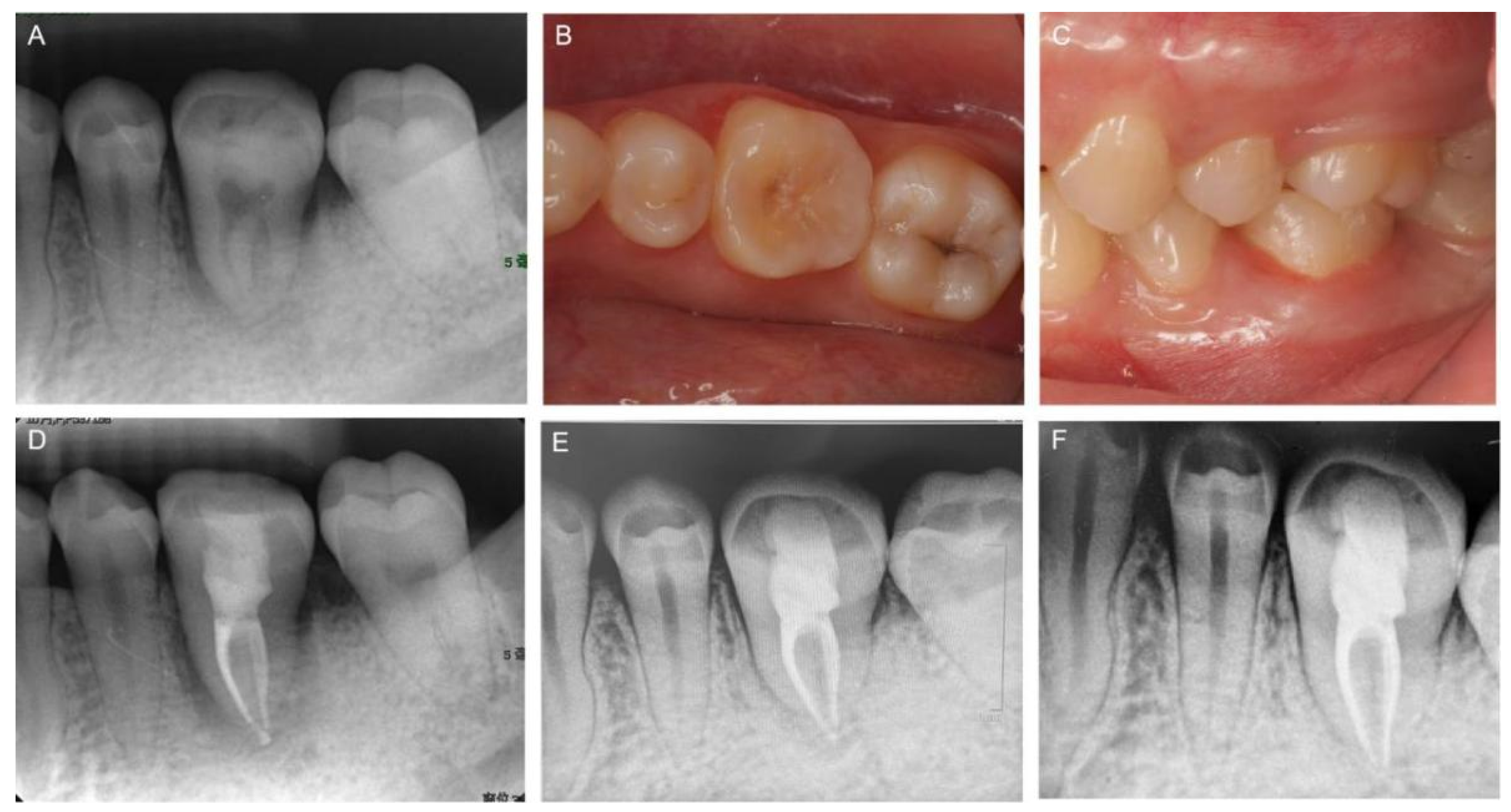
2.1. Clinical Examination and Treatment Planning
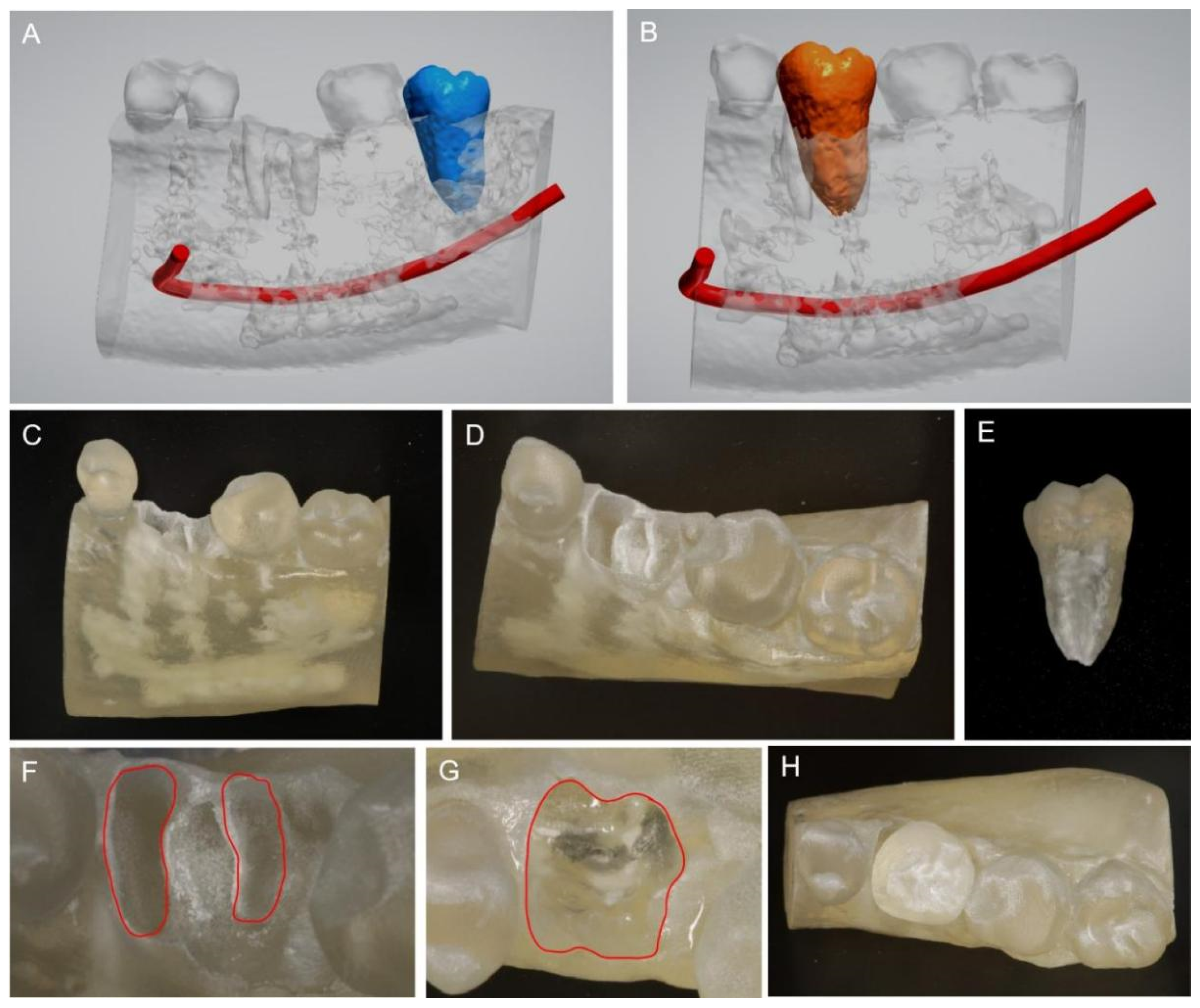
2.2. Preoperative Virtual Simulation and Fabrication of the CARP Models
2.3. Clinical Procedures
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tsukiboshi, M.; Yamauchi, N.; Tsukiboshi, Y. Long-term Outcomes of Autotransplantation of Teeth: A Case Series. J. Endod. 2019, 45, S72–S83. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, K.; Kariya, N.; Namura, D.; Noji, I.; Mitsuhashi, K.; Kimura, H.; Fukuda, A.; Kikukawa, I.; Hayashi, T.; Yamazaki, N.; et al. A retrospective survey of autotransplantation of teeth in dental clinics. J. Oral Rehabil. 2012, 39, 37–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsukiboshi, M. Autotransplantation of teeth: Requirements for predictable success. Dent. Traumatol. 2002, 18, 157–180. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.; Kim, S.; Lo, H.S.; Choi, J.Y.; Kim, H.J.; Ryu, G.J.; Kim, S.Y.; Choi, K.K.; Kim, D.S.; Jang, J.H. Virtual Simulation of Autotransplantation Using 3-dimensional Printing Prototyping Model and Computer-assisted Design Program. J. Endod. 2018, 44, 1883–1888. [Google Scholar] [CrossRef]
- Plotino, G.; Abella Sans, F.; Duggal, M.S.; Grande, N.M.; Krastl, G.; Nagendrababu, V.; Gambarini, G. Present status and future directions: Surgical extrusion, intentional replantation and tooth autotransplantation. Int. Endod. J. 2022, 55, 827–842. [Google Scholar] [CrossRef] [PubMed]
- Xia, J.J.; Ge, Z.Y.; Fu, X.H.; Zhang, Y.Z. Autotransplantation of third molars with completely formed roots to replace compromised molars with the computer-aided rapid prototyping. J. Esthet. Restor. Dent. 2020, 32, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-J.; Kim, E. Minimizing the extra-oral time in autogeneous tooth transplantation: Use of computer-aided rapid prototyping (CARP) as a duplicate model tooth. Restor. Dent. Endod. 2012, 37, 136–141. [Google Scholar] [CrossRef] [Green Version]
- Jang, J.H.; Lee, S.J.; Kim, E. Autotransplantation of Immature Third Molars Using a Computer-aided Rapid Prototyping Model: A Report of 4 Cases. J. Endod. 2013, 39, 1461–1466. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Choi, Y.J.; Lee, S.J.; Roh, B.D.; Park, S.H.; Kim, E. Prognostic Factors for Clinical Outcomes in Autotransplantation of Teeth with Complete Root Formation: Survival Analysis for up to 12 Years. J. Endod. 2016, 42, 198–205. [Google Scholar] [CrossRef]
- Reich, P.P. Autogenous Transplantation of Maxillary and Mandibular Molars. J. Oral Maxillofac. Surg. 2008, 66, 2314–2317. [Google Scholar] [CrossRef]
- Plotino, G.; Abella Sans, F.; Duggal, M.S.; Grande, N.M.; Krastl, G.; Nagendrababu, V.; Gambarini, G. European Society of Endodontology position statement: Surgical extrusion, intentional replantation and tooth autotransplantation: European Society of Endodontology developed by. Int. Endod. J. 2021, 54, 655–659. [Google Scholar] [CrossRef]
- Anderson, J.; Wealleans, J.; Ray, J. Endodontic applications of 3D printing. Int. Endod. J. 2018, 51, 1005–1018. [Google Scholar] [CrossRef]
- Reymus, M.; Fotiadou, C.; Kessler, A.; Heck, K.; Hickel, R.; Diegritz, C. 3D printed replicas for endodontic education. Int. Endod. J. 2019, 52, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.K.J.; Foong, K.W.C.; Sim, Y.F.; Chew, M.T. Evaluation of the accuracy of cone beam computed tomography (CBCT) generated tooth replicas with application in autotransplantation. J. Dent. 2022, 117, 103908. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Tian, K.; Xie, X.; Wang, E.; Cui, N. Computer-aided autotransplantation of teeth with 3D printed surgical guides and arch bar: A preliminary experience. PeerJ 2018, 6, e5939. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, S.W.; Choi, I.S.; Lee, B.N.; Ryu, J.; Park, H.J.; Cho, J.H. Periodontal ligament preloading and rapid prototyping of the donor tooth in the autotransplantation of premolars with complete root formation. Am. J. Orthod. Dentofac. Orthop. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Ghassemi, M.; Jamilian, A.; Fritz, U.; Riediger, D.; Ghassemi, A. Orthodontic treatment after autotransplantation. Angle Orthod. 2011, 81, 721–725. [Google Scholar] [CrossRef]
- Kafourou, V.; Tong, H.J.; Day, P.; Houghton, N.; Spencer, R.J.; Duggal, M. Outcomes and prognostic factors that influence the success of tooth autotransplantation in children and adolescents. Dent. Traumatol. 2017, 33, 393–399. [Google Scholar] [CrossRef]
- Monterubbianesi, R.; Tosco, V.; Vitiello, F.; Orilisi, G.; Fraccastoro, F.; Putignano, A.; Orsini, G. Augmented, Virtual and Mixed Reality in Dentistry: A Narrative Review on the Existing Platforms and Future Challenges. Appl. Sci. 2022, 12, 877. [Google Scholar] [CrossRef]
- Kim, J.; Lin, Y.-C.; Danielak, M.; Van, M.; Lee, D.-H.; Kim, H.; Arany, P.R. Virtual Planning and Rapid 3D Prototyping Surgical Guide for Anterior Crown Lengthening Surgery: A Clinical Case Report. J. Prosthodont. 2022, 31, 275–281. [Google Scholar] [CrossRef]
- Gambarini, G.; Galli, M.; Stefanelli, L.V.; Di Nardo, D.; Morese, A.; Seracchiani, M.; De Angelis, F.; Di Carlo, S.; Testarelli, L. Endodontic Microsurgery Using Dynamic Navigation System: A Case Report. J. Endod. 2019, 45, 1397–1402. [Google Scholar] [CrossRef] [PubMed]
- Han, S.; Wang, H.; Chen, J.; Zhao, J.; Zhong, H. Application effect of computer-aided design combined with three-dimensional printing technology in autologous tooth transplantation: A retrospective cohort study. BMC Oral Health 2022, 22, 5. [Google Scholar] [CrossRef] [PubMed]
- Al-Khanati, N.M.; Kara Beit, Z. Reconsidering some standards in immediate autotransplantation of teeth: Case report with 2-year follow-up. Ann. Med. Surg. 2022, 75, 103470. [Google Scholar] [CrossRef] [PubMed]
- Hwang, L.A.; Chang, C.Y.; Su, W.C.; Chang, C.W.; Huang, C.Y. Rapid prototyping-assisted tooth autotransplantation is associated with a reduced root canal treatment rate: A retrospective cohort study. BMC Oral Health 2022, 22, 25. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, H.; Cai, M.; Liu, Z.; Liu, H.; Shen, Y.; Huang, X. Combined Application of Virtual Simulation Technology and 3-Dimensional-Printed Computer-Aided Rapid Prototyping in Autotransplantation of a Mature Third Molar. Medicina 2022, 58, 953. https://doi.org/10.3390/medicina58070953
Zhang H, Cai M, Liu Z, Liu H, Shen Y, Huang X. Combined Application of Virtual Simulation Technology and 3-Dimensional-Printed Computer-Aided Rapid Prototyping in Autotransplantation of a Mature Third Molar. Medicina. 2022; 58(7):953. https://doi.org/10.3390/medicina58070953
Chicago/Turabian StyleZhang, Hui, Min Cai, Zhiguo Liu, He Liu, Ya Shen, and Xiangya Huang. 2022. "Combined Application of Virtual Simulation Technology and 3-Dimensional-Printed Computer-Aided Rapid Prototyping in Autotransplantation of a Mature Third Molar" Medicina 58, no. 7: 953. https://doi.org/10.3390/medicina58070953
APA StyleZhang, H., Cai, M., Liu, Z., Liu, H., Shen, Y., & Huang, X. (2022). Combined Application of Virtual Simulation Technology and 3-Dimensional-Printed Computer-Aided Rapid Prototyping in Autotransplantation of a Mature Third Molar. Medicina, 58(7), 953. https://doi.org/10.3390/medicina58070953






