Acceptance and Commitment Therapy to Increase Resilience in Chronic Pain Patients: A Clinical Guideline
Abstract
1. Introduction
2. Acceptance and Commitment Therapy to Increase Resilience in Chronic Pain Patients
2.1. Session ACT 1
2.2. Session ACT 2
2.3. Session ACT 3
2.4. Session ACT 4
2.5. Session ACT 5
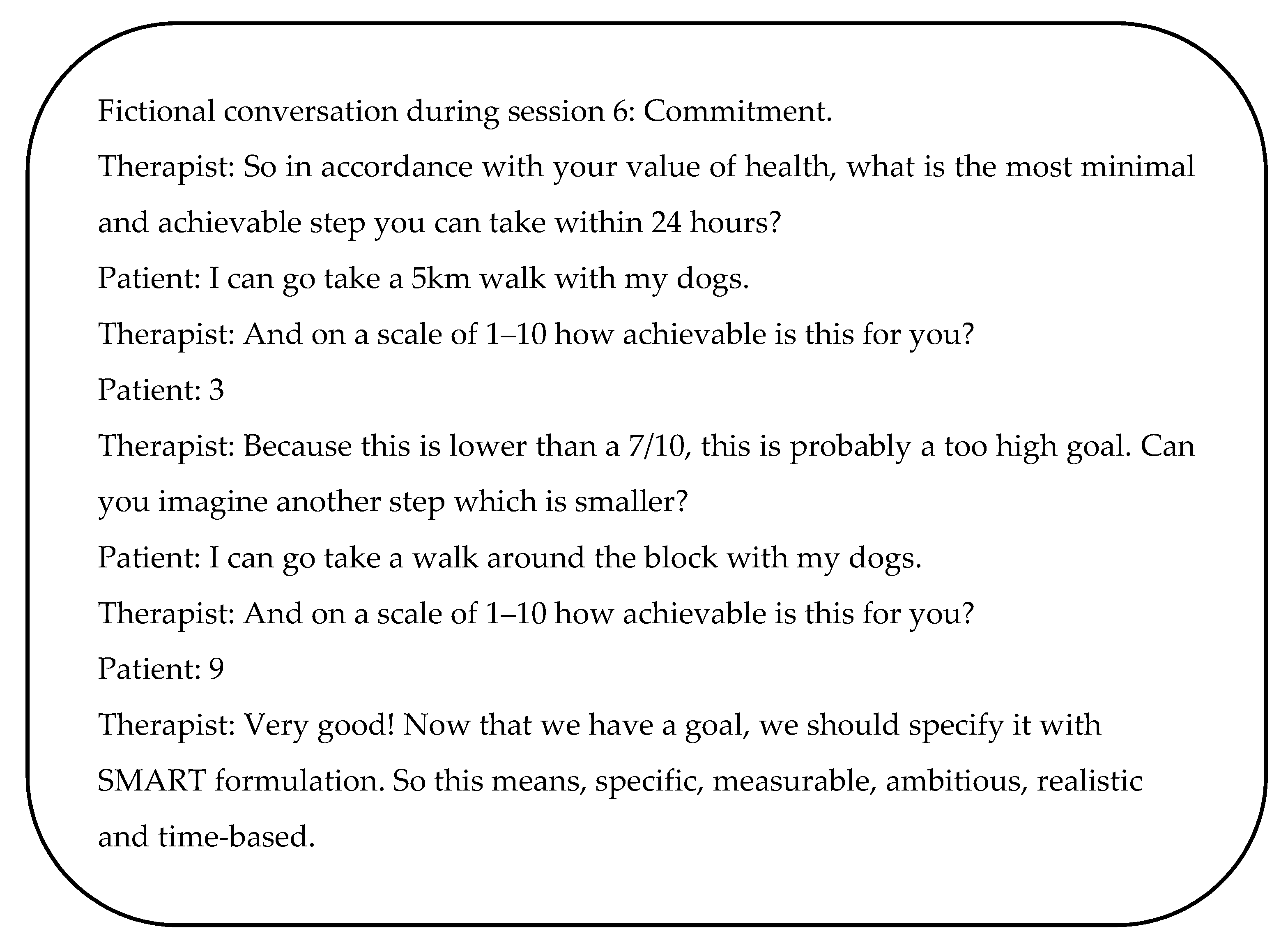
2.6. Session ACT 6
2.7. Session ACT 7
3. Monitor Resilience
4. Practical Considerations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wippert, P.M.; Driesslein, D.; Beck, H.; Schneider, C.; Puschmann, A.K.; Banzer, W.; Schiltenwolf, M. The Feasibility and Effectiveness of a New Practical Multidisciplinary Treatment for Low-Back Pain: A Randomized Controlled Trial. J. Clin. Med. 2019, 9, 115. [Google Scholar] [CrossRef] [PubMed]
- Gatchel, R.J.; Okifuji, A. Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. J. Pain Off. J. Am. Pain Soc. 2006, 7, 779–793. [Google Scholar] [CrossRef] [PubMed]
- Elbers, S.; Wittink, H.; Pool, J.J.M.; Smeets, R. The effectiveness of generic self-management interventions for patients with chronic musculoskeletal pain on physical function, self-efficacy, pain intensity and physical activity: A systematic review and meta-analysis. Eur. J. Pain 2018, 22, 1577–1596. [Google Scholar] [CrossRef] [PubMed]
- Damush, T.M.; Kroenke, K.; Bair, M.J.; Wu, J.; Tu, W.; Krebs, E.E.; Poleshuck, E. Pain self-management training increases self-efficacy, self-management behaviours and pain and depression outcomes. Eur. J. Pain 2016, 20, 1070–1078. [Google Scholar] [CrossRef] [PubMed]
- Billot, M.; Daycard, M.; Rigoard, P. Self-Reiki, Consideration of a Potential Option for Managing Chronic Pain during Pandemic COVID-19 Period. Medicina 2021, 57, 867. [Google Scholar] [CrossRef] [PubMed]
- Du, S.; Hu, L.; Dong, J.; Xu, G.; Chen, X.; Jin, S.; Zhang, H.; Yin, H. Self-management program for chronic low back pain: A systematic review and meta-analysis. Patient Educ. Couns. 2017, 100, 37–49. [Google Scholar] [CrossRef] [PubMed]
- Teater, D. The Psychological and Physical Side Effects of Pain Medication; National Safety Council: Itasca, IL, USA, 2015. [Google Scholar]
- Cheatle, M.D. Prescription Opioid Misuse, Abuse, Morbidity, and Mortality: Balancing Effective Pain Management and Safety. Pain Med. 2015, 16 (Suppl. 1), S3–S8. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Scott, K.; Dukewich, M. Innovative technology using virtual reality in the treatment of pain: Does it reduce pain via distraction, or is there more to it? Pain Med. 2018, 19, 151–159. [Google Scholar] [CrossRef]
- Li, L.; Yu, F.; Shi, D.; Shi, J.; Tian, Z.; Yang, J.; Wang, X.; Jiang, Q. Application of virtual reality technology in clinical medicine. Am. J. Transl. Res. 2017, 9, 3867. [Google Scholar] [PubMed]
- Dumain, M.; Jaglin, P.; Wood, C.; Rainville, P.; Pageaux, B.; Perrochon, A.; Lavallière, M.; Vendeuvre, T.; Romain, D.; Langlois, P.; et al. Long-Term Efficacy of a Home-Care Hypnosis Program in Elderly Persons Suffering From Chronic Pain: A 12-Month Follow-Up. Pain Manag. Nurs. 2021. [Google Scholar] [CrossRef]
- Billot, M.; Jaglin, P.; Rainville, P.; Rigoard, P.; Langlois, P.; Cardinaud, N.; Tchalla, A.; Wood, C. Hypnosis Program Effectiveness in a 12-week Home Care Intervention To Manage Chronic Pain in Elderly Women: A Pilot Trial. Clin. Ther. 2020, 42, 221–229. [Google Scholar] [CrossRef]
- Jensen, M.P.; Turk, D.C. Contributions of psychology to the understanding and treatment of people with chronic pain: Why it matters to ALL psychologists. Am. Psychol. 2014, 69, 105. [Google Scholar] [CrossRef] [PubMed]
- Fordyce, W.E.; Fowler, R.S.; DeLateur, B. An application of behavior modification technique to a problem of chronic pain. Behav. Res. Ther. 1968, 6, 105–107. [Google Scholar] [CrossRef]
- Fordyce, W.E.; Fowler, R.S.; Lehmann, J.F.; DeLateur, B.J.; Sand, P.L.; Trieschmann, R.B. Operant conditioning in the treatment of chronic pain. Arch. Phys. Med. Rehabil. 1973, 54, 399–408. [Google Scholar]
- Keefe, F.J.; Bradley, L.A. Behavioral and psychological approaches to the assessment and treatment of chronic pain. Gen. Hosp. Psychiatry 1984, 6, 49–54. [Google Scholar] [CrossRef]
- Turk, D.C.; Meichenbaum, D.; Genest, M. Pain and Behavioral Medicine: A Cognitive-Behavioral Perspective; Guilford Press: New York, NY, USA, 1983; Volume 1. [Google Scholar]
- Turner, J.A. Comparison of group progressive-relaxation training and cognitive-behavioral group therapy for chronic low back pain. J. Consult. Clin. Psychol. 1982, 50, 757. [Google Scholar] [CrossRef] [PubMed]
- Melzack, R.; Wall, P.D. Pain mechanisms: A new theory. Science 1965, 150, 971–979. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P. A neuropsychological model of pain: Research and clinical implications. J. Pain 2010, 11, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Melzack, R. From the gate to the neuromatrix. Pain 1999, 82, S121–S126. [Google Scholar] [CrossRef]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy; American Psychological Association: Washington, DC, USA, 2009. [Google Scholar]
- Hayes, S.C.; Strosahl, K.D.; Bunting, K.; Twohig, M.; Wilson, K.G. What is acceptance and commitment therapy. In A Practical Guide to Acceptance and Commitment Therapy; Springer: Berlin, Germany, 2004; pp. 3–29. [Google Scholar]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- McCracken, L. Contextual Cognitive Behavioral Therapy for Chronic Pain; Int Assoc Study Pain (Iasp) Press: Seattle, WA, USA, 2005. [Google Scholar]
- Robinson, P.; Wicksell, R.K.; Olsson, G.L. ACT with chronic pain patients. In A Practical Guide to Acceptance and Commitment Therapy; Springer: Berlin, Germany, 2004; pp. 315–345. [Google Scholar]
- Hayes, S.; Strosahl, K.; Wilson, K. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change; Guilford: New York, NY, USA, 1999; p. 3. [Google Scholar]
- Hayes, S.C.; Duckworth, M.P. Acceptance and commitment therapy and traditional cognitive behavior therapy approaches to pain. Cogn. Behav. Pract. 2006, 13, 185–187. [Google Scholar] [CrossRef]
- Wetherell, J.L.; Afari, N.; Rutledge, T.; Sorrell, J.T.; Stoddard, J.A.; Petkus, A.J.; Solomon, B.C.; Lehman, D.H.; Liu, L.; Lang, A.J. A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain 2011, 152, 2098–2107. [Google Scholar] [CrossRef] [PubMed]
- Feliu-Soler, A.; Montesinos, F.; Gutiérrez-Martínez, O.; Scott, W.; McCracken, L.M.; Luciano, J.V. Current status of acceptance and commitment therapy for chronic pain: A narrative review. J. Pain Res. 2018, 11, 2145. [Google Scholar] [CrossRef] [PubMed]
- Gentili, C.; Rickardsson, J.; Zetterqvist, V.; Simons, L.E.; Lekander, M.; Wicksell, R.K. Psychological flexibility as a resilience factor in individuals with chronic pain. Front. Psychol. 2019, 10, 2016. [Google Scholar] [CrossRef] [PubMed]
- Walker, B. Resilience: What it is and is not. Ecol. Soc. 2020, 25, 11. [Google Scholar] [CrossRef]
- Karoly, P.; Ruehlman, L.S. Psychological “resilience” and its correlates in chronic pain: Findings from a national community sample. Pain 2006, 123, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Yeung, E.W.; Arewasikporn, A.; Zautra, A.J. Resilience and chronic pain. J. Soc. Clin. Psychol. 2012, 31, 593–617. [Google Scholar] [CrossRef]
- Ruehlman, L.S.; Karoly, P.; Newton, C.; Aiken, L.S. The development and preliminary validation of a brief measure of chronic pain impact for use in the general population. Pain 2005, 113, 82–90. [Google Scholar] [CrossRef]
- Gloster, A.T.; Walder, N.; Levin, M.; Twohig, M.; Karekla, M. The empirical status of acceptance and commitment therapy: A review of meta-analyses. J. Contextual Behav. Sci. 2020, 18, 181–192. [Google Scholar] [CrossRef]
- van de Graaf, D.L.; Trompetter, H.R.; Smeets, T.; Mols, F. Online Acceptance and Commitment Therapy (ACT) interventions for chronic pain: A systematic literature review. Internet Interv. 2021, 26, 100465. [Google Scholar] [CrossRef]
- Du, S.; Dong, J.; Jin, S.; Zhang, H.; Zhang, Y. Acceptance and Commitment Therapy for chronic pain on functioning: A systematic review of randomized controlled trials. Neurosci. Biobehav. Rev. 2021, 131, 59–76. [Google Scholar] [CrossRef]
- Hughes, L.S.; Clark, J.; Colclough, J.A.; Dale, E.; McMillan, D. Acceptance and Commitment Therapy (ACT) for Chronic Pain: A Systematic Review and Meta-Analyses. Clin. J. Pain 2017, 33, 552–568. [Google Scholar] [CrossRef] [PubMed]
- Galvez-Sánchez, C.M.; Montoro, C.I.; Moreno-Padilla, M.; Reyes Del Paso, G.A.; de la Coba, P. Effectiveness of Acceptance and Commitment Therapy in Central Pain Sensitization Syndromes: A Systematic Review. J. Clin. Med. 2021, 10, 2706. [Google Scholar] [CrossRef]
- Louw, A.; Zimney, K.; Puentedura, E.J.; Diener, I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother Theory Pr. 2016, 32, 332–355. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.A.; Ryan, C.G.; Cooper, L.; Ellington, D.; Whittle, R.; Lavender, M.; Dixon, J.; Atkinson, G.; Cooper, K.; Martin, D.J. Pain Neuroscience Education for Adults With Chronic Musculoskeletal Pain: A Mixed-Methods Systematic Review and Meta-Analysis. J. Pain Off. J. Am. Pain Soc. 2019, 20, 1140.e1–1140.e22. [Google Scholar] [CrossRef] [PubMed]
- Goudman, L.; Huysmans, E.; Ickmans, K.; Nijs, J.; Moens, M.; Putman, K.; Buyl, R.; Louw, A.; Logghe, T.; Coppieters, I. A modern pain neuroscience approach in patients undergoing surgery for lumbar radiculopathy: A clinical perspective. Phys. Ther. 2019, 99, 933–945. [Google Scholar] [CrossRef] [PubMed]
- Willaert, W.; Leysen, L.; Lenoir, D.; Meeus, M.; Cagnie, B.; Nijs, J.; Sterling, M.; Coppieters, I. Combining stress management with pain neuroscience education and exercise therapy in people with whiplash-associated disorders: A clinical perspective. Phys. Ther. 2021, 101, pzab105. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Butler, D.S.; Diener, I.; Puentedura, E.J. Development of a preoperative neuroscience educational program for patients with lumbar radiculopathy. Am. J. Phys. Med. Rehabil. 2013, 92, 446–452. [Google Scholar] [CrossRef]
- Ickmans, K.; Moens, M.; Putman, K.; Buyl, R.; Goudman, L.; Huysmans, E.; Diener, I.; Logghe, T.; Louw, A.; Nijs, J. Back school or brain school for patients undergoing surgery for lumbar radiculopathy? Protocol for a randomised, controlled trial. J. Physiother. 2016, 62, 165. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Levin, M.E.; Plumb-Vilardaga, J.; Villatte, J.L.; Pistorello, J. Acceptance and commitment therapy and contextual behavioral science: Examining the progress of a distinctive model of behavioral and cognitive therapy. Behav. Ther. 2013, 44, 180–198. [Google Scholar] [CrossRef]
- Jansen, G.; Batink, T. Time to ACT: Het Basisboek Voor Professionals; Thema, uitgeverij van Schouten & Nelissen: Zaltbommel, The Netherlands, 2014. [Google Scholar]
- APA. Building Your Resilience. Available online: http://www.apa.org/topics/resilience (accessed on 1 February 2020).
- Hayes, S.C. Rule-Governed Behavior: Cognition, Contingencies and Instructional Control; Plenum Press: New York, NY, USA, 1989. [Google Scholar]
- Twohig, M.P. Acceptance and Commitment Therapy: Introduction; Elsevier: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, M.A.; Edwards, R.R.; Becker, W.C.; Kaptchuk, T.J.; Kerns, R.D. Psychological Interventions for the Treatment of Chronic Pain in Adults. Psychol. Sci. Public Interest 2021, 22, 52–95. [Google Scholar] [CrossRef] [PubMed]
- Ussher, M.; Spatz, A.; Copland, C.; Nicolaou, A.; Cargill, A.; Amini-Tabrizi, N.; McCracken, L.M. Immediate effects of a brief mindfulness-based body scan on patients with chronic pain. J. Behav. Med. 2014, 37, 127–134. [Google Scholar] [CrossRef]
- Firth, A.M.; Cavallini, I.; Sütterlin, S.; Lugo, R.G. Mindfulness and self-efficacy in pain perception, stress and academic performance. The influence of mindfulness on cognitive processes. Psychol. Res. Behav. Manag. 2019, 12, 565. [Google Scholar] [CrossRef] [PubMed]
- Joyce, S.; Shand, F.; Tighe, J.; Laurent, S.J.; Bryant, R.A.; Harvey, S.B. Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018, 8, e017858. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The Brief Resilience Scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Connor, K.M.; Davidson, J.R. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Ponce-Garcia, E.; Madewell, A.N.; Kennison, S.M. The Development of the Scale of Protective Factors: Resilience in a Violent Trauma Sample. Violence Vict. 2015, 30, 735–755. [Google Scholar] [CrossRef]
- Du, S.; Dong, J.; Jin, S.; Zhang, H.; Zhang, Y. Acceptance and commitment therapy for chronic pain conditions on functioning: A systematic review protocol. J. Adv. Nurs. 2021, 77, 417–426. [Google Scholar] [CrossRef]
- ACT. Video Materiaal. Available online: https://www.actinactie.nl/video-materiaal/ (accessed on 28 March 2022).
- Luoma, J.B.; Hayes, S.C.; Walser, R.D. Learning ACT: An Acceptance & Commitment Therapy Skills-Training Manual for Therapists; New Harbinger Publications: Oakland, CA, USA, 2007. [Google Scholar]
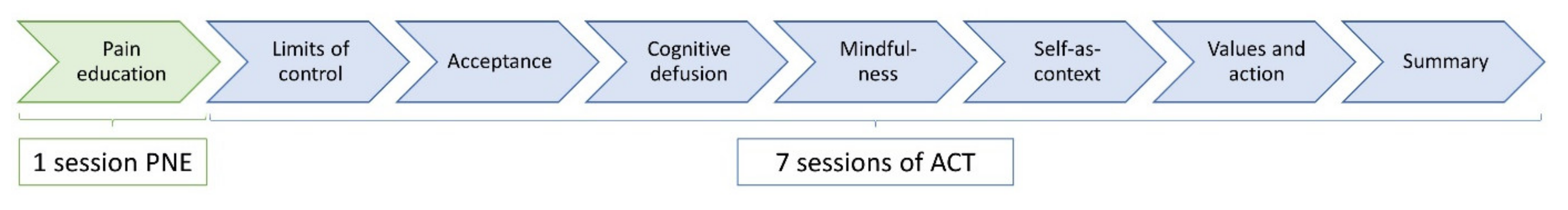
| ACT Sessions | Content of Session | Home Assignment |
|---|---|---|
| Session 1 | Limits of control |
|
| Session 2 | Acceptance |
|
| Session 3 | Cognitive defusion |
|
| Session 4 | Mindfulness |
|
| Session 5 | Self-as-context |
|
| Session 6 | Values and committed action |
|
| Session 7 | Summarisation |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moens, M.; Jansen, J.; De Smedt, A.; Roulaud, M.; Billot, M.; Laton, J.; Rigoard, P.; Goudman, L. Acceptance and Commitment Therapy to Increase Resilience in Chronic Pain Patients: A Clinical Guideline. Medicina 2022, 58, 499. https://doi.org/10.3390/medicina58040499
Moens M, Jansen J, De Smedt A, Roulaud M, Billot M, Laton J, Rigoard P, Goudman L. Acceptance and Commitment Therapy to Increase Resilience in Chronic Pain Patients: A Clinical Guideline. Medicina. 2022; 58(4):499. https://doi.org/10.3390/medicina58040499
Chicago/Turabian StyleMoens, Maarten, Julie Jansen, Ann De Smedt, Manuel Roulaud, Maxime Billot, Jorne Laton, Philippe Rigoard, and Lisa Goudman. 2022. "Acceptance and Commitment Therapy to Increase Resilience in Chronic Pain Patients: A Clinical Guideline" Medicina 58, no. 4: 499. https://doi.org/10.3390/medicina58040499
APA StyleMoens, M., Jansen, J., De Smedt, A., Roulaud, M., Billot, M., Laton, J., Rigoard, P., & Goudman, L. (2022). Acceptance and Commitment Therapy to Increase Resilience in Chronic Pain Patients: A Clinical Guideline. Medicina, 58(4), 499. https://doi.org/10.3390/medicina58040499








