Upper Hemi-Sternotomy Provides Benefit for Patients with Isolated or Combined Mitral Valve Surgery
Abstract
1. Introduction
2. Material and Methods
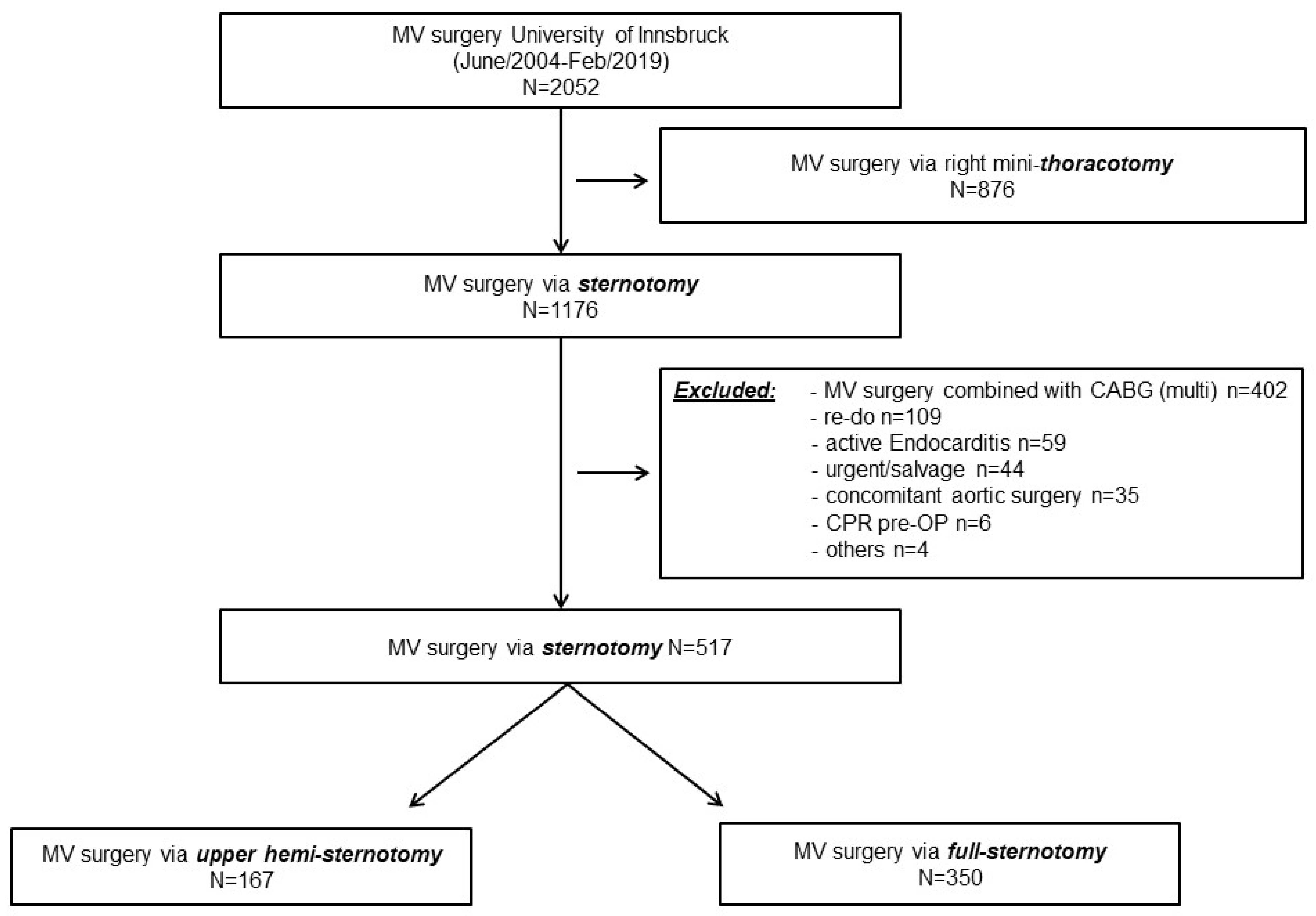
2.1. Patients
2.2. Study Cohort
2.3. Surgical Procedures
2.4. Outcome Parameters
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Outcomes
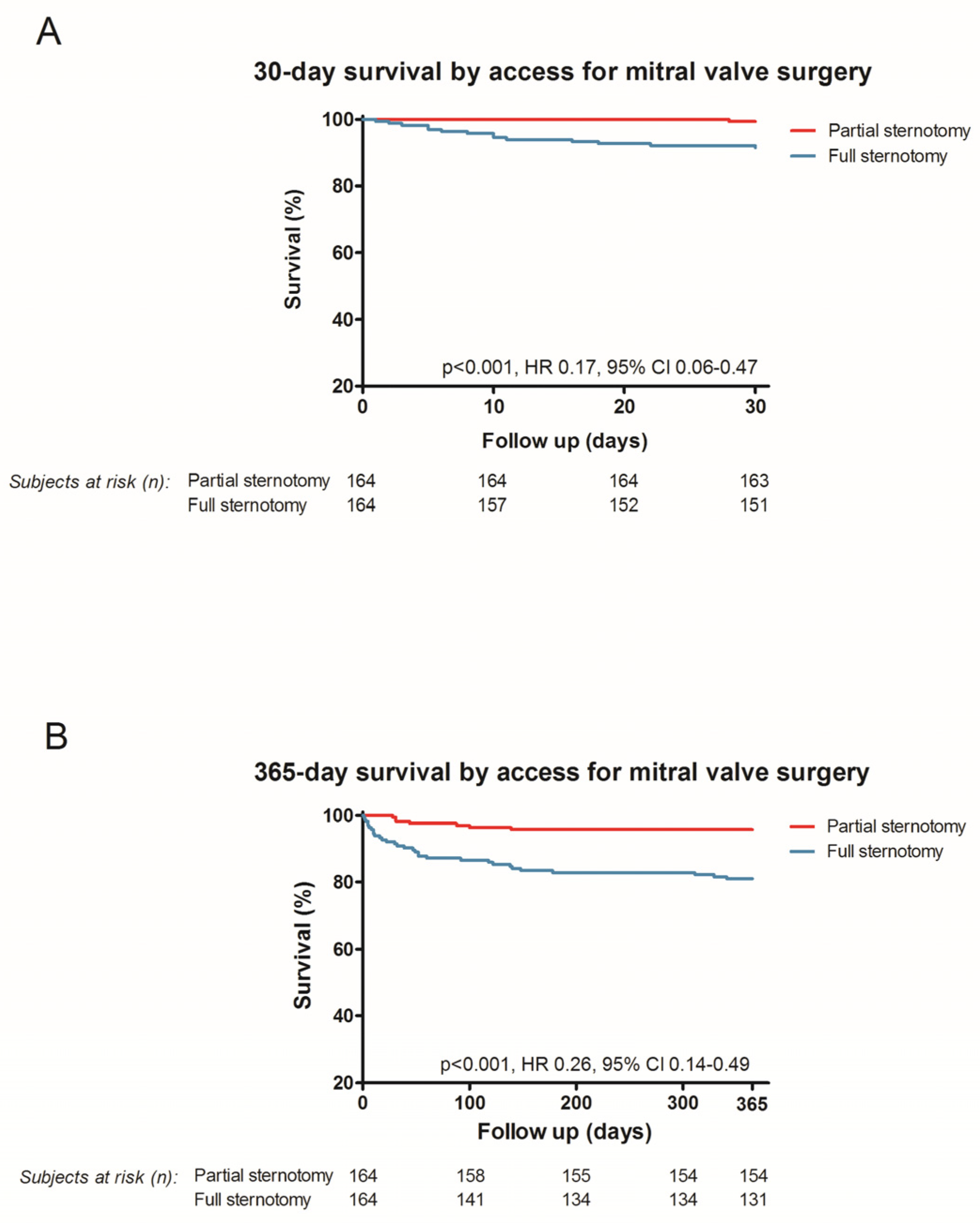
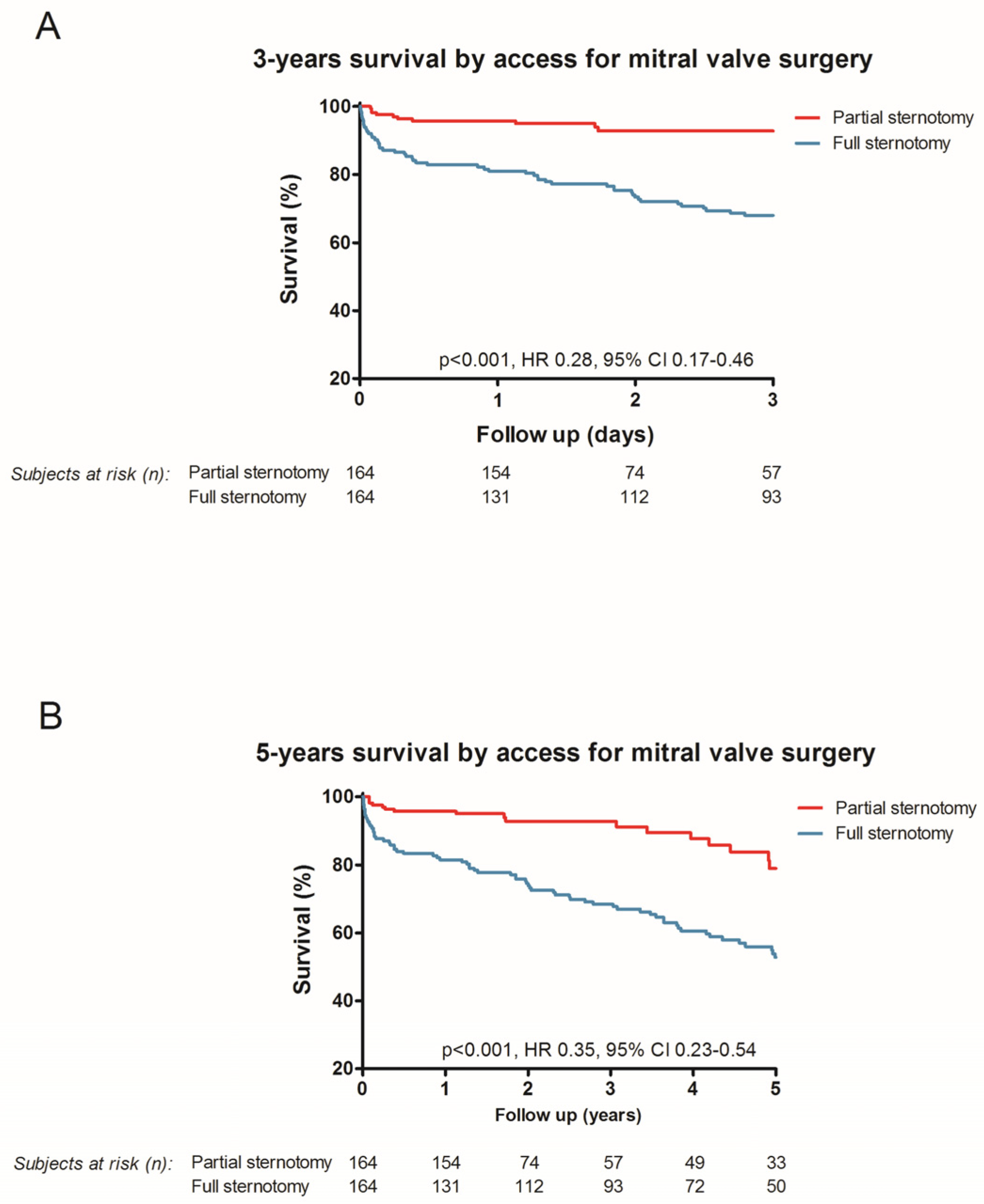
3.2.1. 30-Day Mortality and 1-Year Survival
3.2.2. Additional Outcomes
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beckmann, A.; Meyer, R.; Lewandowski, J.; Markewitz, A.; Harringer, W. German Heart Surgery Report 2018: The Annual Updated Registry of the German Society for Thoracic and Cardiovascular Surgery. Thorac. Cardiovasc. Surg. 2019, 67, 331–344. [Google Scholar] [CrossRef]
- Ward, A.F.; Grossi, E.A.; Galloway, A.C. Minimally invasive mitral surgery through right mini-thoracotomy under direct vision. J. Thorac. Dis. 2013, 5 (Suppl. S6), S673–S679. [Google Scholar] [CrossRef]
- Glauber, M.; Miceli, A.; Canarutto, D.; Lio, A.; Murzi, M.; Gilmanov, D.; Ferrarini, M.; Farneti, P.A.; Quaini, E.L.; Solinas, M. Early and long-term outcomes of minimally invasive mitral valve surgery through right minithoracotomy: A 10-year experience in 1604 patients. J. Cardiothorac. Surg. 2015, 10, 181. [Google Scholar] [CrossRef]
- Grossi, E.A.; Goldman, S.; Wolfe, J.A.; Mehall, J.; Smith, J.M.; Ailawadi, G.; Salemi, A.; Moore, M.; Ward, A.; Gunnarsson, C.; et al. Minithoracotomy for mitral valve repair improves inpatient and postdischarge economic savings. J. Thorac. Cardiovasc. Surg. 2014, 148, 2818–2822.e3. [Google Scholar] [CrossRef] [PubMed]
- Vollroth, M.; Seeburger, J.; Garbade, J.; Borger, M.A.; Misfeld, M.; Mohr, F.W. Conversion rate and contraindications for minimally invasive mitral valve surgery. Ann. Cardiothorac. Surg. 2013, 2, 853–854. [Google Scholar] [CrossRef]
- Marin Cuartas, M.; Javadikasgari, H.; Pfannmueller, B.; Seeburger, J.; Gillinov, A.M.; Suri, R.M.; Borger, M.A. Mitral valve repair: Robotic and other minimally invasive approaches. Prog. Cardiovasc. Dis. 2017, 60, 394–404. [Google Scholar] [CrossRef] [PubMed]
- Saunders, P.C.; Grossi, E.A.; Sharony, R.; Schwartz, C.F.; Ribakove, G.H.; Culliford, A.T.; Delianides, J.; Baumann, F.G.; Galloway, A.C.; Colvin, S.B. Minimally invasive technology for mitral valve surgery via left thoracotomy: Experience with forty cases. J. Thorac. Cardiovasc. Surg. 2004, 127, 1026–1031. [Google Scholar] [CrossRef] [PubMed]
- Semsroth, S.; Matteucci Gothe, R.; Raith, Y.R.; de Brabandere, K.; Hanspeter, E.; Kilo, J.; Kofler, M.; Muller, L.; Ruttman-Ulmer, E.; Grimm, M. Comparison of Two Minimally Invasive Techniques and Median Sternotomy in Aortic Valve Replacement. Ann. Thorac. Surg. 2017, 104, 877–883. [Google Scholar] [CrossRef]
- Gillinov, A.M.; Cosgrove, D.M. Minimally invasive mitral valve surgery: Mini-sternotomy with extended transseptal approach. Semin. Thorac. Cardiovasc. Surg. 1999, 11, 206–211. [Google Scholar] [CrossRef]
- Meyer, B.W.; Verska, J.J.; Lindesmith, G.G.; Jones, J.C. Open Repair of Mitral Valve Lesions: The Superior Approach. Ann. Thorac. Surg. 1965, 1, 453–457. [Google Scholar] [CrossRef]
- Esposito, G.; Cappabianca, G.; Bichi, S.; Patrini, D.; Pellegrino, P. Left atrial roof: An alternative minimal approach for mitral valve surgery. Innovations 2012, 7, 417–420. [Google Scholar] [CrossRef] [PubMed]
- Risteski, P.; Monsefi, N.; Miskovic, A.; Josic, T.; Bala, S.; Salem, R.; Zierer, A.; Moritz, A. Triple valve surgery through a less invasive approach: Early and mid-term results. Interact. Cardiovasc. Thorac. Surg. 2017, 24, 677–682. [Google Scholar] [CrossRef]
- Oezpeker, C.; Barbieri, F.; Hoefer, D.; Schneider, B.; Bonaros, N.; Grimm, M.; Mueller, L. Mitral Valve Surgery via Partial Upper Sternotomy: Closing the Gap between Conventional Sternotomy and Right Lateral Minithoracotomy. Thorac. Cardiovasc. Surg. 2019, 67, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Downs, E.A.; Johnston, L.E.; LaPar, D.J.; Ghanta, R.K.; Kron, I.L.; Speir, A.M.; Fonner, C.E.; Kern, J.A.; Ailawadi, G. Minimally Invasive Mitral Valve Surgery Provides Excellent Outcomes Without Increased Cost: A Multi-Institutional Analysis. Ann. Thorac. Surg. 2016, 102, 14–21. [Google Scholar] [CrossRef]
- Cao, C.; Gupta, S.; Chandrakumar, D.; Nienaber, T.A.; Indraratna, P.; Ang, S.C.; Phan, K.; Yan, T.D. A meta-analysis of minimally invasive versus conventional mitral valve repair for patients with degenerative mitral disease. Ann. Cardiothorac. Surg. 2013, 2, 693–703. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.; Zhang, G.; Zhang, X. Review: Minimally invasive versus conventional dynamic hip screw fixation in elderly patients with intertrochanteric fractures: A systematic review and meta-analysis. Surg. Innov. 2011, 18, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Goldstone, A.B.; Atluri, P.; Szeto, W.Y.; Trubelja, A.; Howard, J.L.; MacArthur, J.W., Jr.; Newcomb, C.; Donnelly, J.P.; Kobrin, D.M.; Sheridan, M.A.; et al. Minimally invasive approach provides at least equivalent results for surgical correction of mitral regurgitation: A propensity-matched comparison. J. Thorac. Cardiovasc. Surg. 2013, 145, 748–756. [Google Scholar] [CrossRef]
- Nashef, S.A.; Roques, F.; Sharples, L.D.; Nilsson, J.; Smith, C.; Goldstone, A.R.; Lockowandt, U. EuroSCORE II. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2012, 41, 734–744. [Google Scholar] [CrossRef]
- Carpentier, A.; Filsoufi, F. Carpentier’s Reconstructive Valve Surgery, 1st ed.; Saunders: London, UK, 2010; 368p. [Google Scholar]
- Svensson, L.G. Minimally invasive surgery with a partial sternotomy “J” approach. Semin. Thorac. Cardiovasc. Surg. 2007, 19, 299–303. [Google Scholar] [CrossRef]
- Radwan, M.; Salewski, C.; Hecker, F.; Miskovic, A.; Risteski, P.; Hlavicka, J.; Moritz, A.; Walther, T.; Holubec, T. Mitral Valve Surgery via Upper Ministernotomy: Single-Centre Experience in More than 400 Patients. Medicina 2021, 57, 1179. [Google Scholar] [CrossRef]
- Svensson, L.G.; Atik, F.A.; Cosgrove, D.M.; Blackstone, E.H.; Rajeswaran, J.; Krishnaswamy, G.; Jin, U.; Gillinov, A.M.; Griffin, B.; Navia, J.L.; et al. Minimally invasive versus conventional mitral valve surgery: A propensity-matched comparison. J. Thorac. Cardiovasc. Surg. 2010, 139, 926–932.e2. [Google Scholar] [CrossRef]
- Oezpeker, U.C.; Barbieri, F.; Hoefer, D.; Bonaros, N.; Grimm, M.; Mueller, L. Partial Upper Sternotomy is a Safe Alternative in Mitral Annulus Decalcification. Semin. Thorac. Cardiovasc. Surg. 2021. [Google Scholar] [CrossRef] [PubMed]
- Lukac, P.; Hjortdal, V.E.; Pedersen, A.K.; Mortensen, P.T.; Jensen, H.K.; Hansen, P.S. Superior transseptal approach to mitral valve is associated with a higher need for pacemaker implantation than the left atrial approach. Ann. Thorac. Surg. 2007, 83, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Vlahakes, G.J. Right ventricular failure after cardiac surgery. Cardiol. Clin. 2012, 30, 283–289. [Google Scholar] [CrossRef]
- Zanobini, M.; Loardi, C.; Poggio, P.; Tamborini, G.; Veglia, F.; Di Minno, A.; Myasoedova, V.; Mammana, L.F.; Biondi, R.; Pepi, M.; et al. The impact of pericardial approach and myocardial protection onto postoperative right ventricle function reduction. J. Cardiothorac. Surg. 2018, 13, 55. [Google Scholar] [CrossRef]
- Rupprecht, L.; Schmid, C. Deep sternal wound complications: An overview of old and new therapeutic options. Open J. Cardiovasc. Surg. 2013, 6, 9–19. [Google Scholar] [CrossRef]
- Doenst, T.; Diab, M.; Sponholz, C.; Bauer, M.; Farber, G. The Opportunities and Limitations of Minimally Invasive Cardiac Surgery. Dtsch. Arztebl. Int. 2017, 114, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Salenger, R.; Gammie, J.S.; Collins, J.A. Minimally Invasive Aortic Valve Replacement. J. Card. Surg. 2016, 31, 38–50. [Google Scholar] [CrossRef]
- Shehada, S.E.; Ozturk, O.; Wottke, M.; Lange, R. Propensity score analysis of outcomes following minimal access versus conventional aortic valve replacement. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2016, 49, 464–469; discussion 469–470. [Google Scholar] [CrossRef]
- Hashemi, N.; Johnson, J.; Brodin, L.A.; Gomes-Bernardes, A.; Sartipy, U.; Svenarud, P.; Dalen, M.; Back, M.; Alam, M.; Winter, R. Right ventricular mechanics and contractility after aortic valve replacement surgery: A randomised study comparing minimally invasive versus conventional approach. Open Heart 2018, 5, e000842. [Google Scholar] [CrossRef]
- McMurry, T.L.; Hu, Y.; Blackstone, E.H.; Kozower, B.D. Propensity scores: Methods, considerations, and applications in the Journal of Thoracic and Cardiovascular Surgery. J. Thorac. Cardiovasc. Surg. 2015, 150, 14–19. [Google Scholar] [CrossRef] [PubMed]

| Unmatched Data | After Propensity Score-Matching | |||||
|---|---|---|---|---|---|---|
| Full Sternotomy n = 350 | Upper Hemi-Sternotomy n = 167 | p-Value | Full Sternotomy n = 164 | Upper Hemi-Sternotomy n = 164 | p-Value | |
| Age (years) 1 | 69 (60–74) | 71 (63–77) | 0.027 | 72 (64–76) | 71 (63–77) | 0.859 |
| Gender, males (%, n) | 47.7 (167) | 44.3 (74) | 0.468 | 50 (82) | 43.3 (71) | 0.223 |
| Body surface area (m2) | 1.81 (1.66–1.96) | 1.81 (1.65–1.93) | 0.323 | 1.79 (1.65–1.94) | 1.81 (1.65–1.93) | 0.830 |
| Diabetes Mellitus (%, n) | 12 (42) | 18.3 (18) | 0.055 | 12.2 (20) | 18.3 (30) | 0.125 |
| Arterial hypertension (%, n) | 64.2 (224) | 85.9 (85) | <0.001 | 68.3 (112) | 81.1 (133) | 0.008 |
| COPD (%, n) | 35.4 (124) | 30.5 (51) | 0.292 | 35.4 (58) | 30.5 (50) | 0.347 |
| PAOD (%, n) | 2.3 (8) | 4.2 (7) | 0.223 | 2.4 (4) | 4.3 (7) | 0.358 |
| Dialysis (%, n) | 0.9 (3) | 3 (5) | 0.064 | 0.6 (1) | 3.0 (5) | 0.099 |
| Prev.CVE (%, n) | 4.3 (15) | 4.8 (8) | 0.762 | 6.7 (11) | 4.9 (8) | 0.478 |
| Acute HF < 3 months (%, n) | 4 (14) | 12.6 (21) | <0.001 | 5.5 (9) | 12.8 (21) | 0.022 |
| EuroSCORE II (%) 1 | 3.04 (1.69–4.84) | 3.0 (1.67–4.74) | 0.874 | 3.14 (1.88–4.95) | 3.0 (1.67–4.74) | 0.267 |
| LV-ejection fraction (%) 1 | 55 (47–61) | 59 (50–65) | 0.005 | 57 (49–63) | 59 (50–65) | 0.659 |
| NYHA III (%, n) | 54.0 (189) | 59.3 (99) | 0.228 | 56.1 (92) | 59.8 (98) | 0.502 |
| NYHA IV (%, n) | 5.7 (20) | 5.4 (9) | 0.893 | 5.5 (9) | 5.5 (9) | n.a |
| Interm.-atrial fibrillation (%, n) | 46.9 (164) | 37.1 (62) | 0.054 | 43.9 (72) | 37.8 (62) | 0.261 |
| Perm.-atrial fibrillation (%, n) | 23.2 (81) | 17.4 (29) | 0.159 | 22.0 (36) | 17.7 (29) | 0.332 |
| sPAP (mmHg) 1 | 50 (36–60) | 45 (36–57) | 0.135 | 50 (40–60) | 45 (36–57) | 0.024 |
| NT-proBNP (ng/L) 1 | 1189 (619–2498) | 1080 (414–2535) | 0.323 | 1248 (618–2476) | 1080 (430–2451) | 0.238 |
| Propensity Score Matched | |||
|---|---|---|---|
| Full Sternotomy n = 164 | Upper Hemi-Sternotomy n = 164 | p-Value | |
| MV-etiology | |||
| Primary (%, n) | 87.7 (144) | 86.0 (141) | 0.624 |
| Secondary (%, n) | 12.2 (20) | 14.0 (23) | 0.624 |
| Moderate to severe AC (%, n) | 35.4 (58) | 36.0 (59) | 0.908 |
| Surgical interventions | |||
| MVS isolated (%, n) | 47.6 (78) | 50.6 (83) | 0.581 |
| MV repair (%, n) | 59.8 (98) | 65.2 (107) | 0.305 |
| MV + TV-surgery (%, n) | 30.5 (50) | 31.1 (51) | 0.905 |
| MV + AV-surgery (%, n) | 18.3 (30) | 15.9 (26) | 0.557 |
| MV + AV + TV-surgery (%, n) | 3.7 (6) | 2.4 (4) | 0.521 |
| Atrial fibrillation surgery (%, n) | 15.2 (25) | 7.9 (13) | 0.038 |
| Full Sternotomy n = 164 | Upper Hemi-Sternotomy n = 164 | p-Value | |
|---|---|---|---|
| CPB time (min) 1 | 161 (130–196) | 164 (140–196) | 0.262 |
| Aortic X-clamp time (min) 1 | 107 (81–133) | 106 (88–132) | 0.829 |
| Second pump run/X-clamp (%, n) | 9.8 (16) | 6.1 (10) | 0.220 |
| ECMO (%, n) | 2.4 (4) | 1.2 (2) | 0.545 |
| LOS (%, n) | 31.1 (51) | 18.9 (31) | 0.011 |
| Tamponade or excessive bleeding (%, n) | 4.3 (7) | 3.0 (5) | 0.556 |
| Hemofiltration/-dialysis new (%, n) | 17.1 (28) | 12.8 (21) | 0.278 |
| Ventilation length (h) 1 | 13 (7–30) | 8 (5–17) | <0.001 |
| Red blood units (first 24 h) 1 | 1 (0–3) | 1 (0–3) | n.a. |
| ICU length (days) 1 | 2 (1–14) | 1 (1–3) | <0.001 |
| Hospital stay (days) 1 | 9 (8–13) | 8 (7–10) | <0.001 |
| MOF (%, n) | 6.7 (11) | 4.3 (7) | 0.332 |
| Sepsis (%, n) | 5.5 (9) | 2.4 (4) | 0.157 |
| Pneumonia (%, n) | 4.9 (8) | 3.0 (5) | 0.396 |
| Deep wound infection (%, n) | 3.7 (6) | 3.0 (5) | 0.759 |
| Stroke (%, n) | 3.0 (5) | 1.2 (2) | 0.252 |
| PM-implantation (%, n) | 5.5 (9) | 3.7 (6) | 0.428 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oezpeker, C.U.; Barbieri, F.; Hoefer, D.; Bonaros, N.; Grimm, M.; Mueller, L. Upper Hemi-Sternotomy Provides Benefit for Patients with Isolated or Combined Mitral Valve Surgery. Medicina 2022, 58, 142. https://doi.org/10.3390/medicina58020142
Oezpeker CU, Barbieri F, Hoefer D, Bonaros N, Grimm M, Mueller L. Upper Hemi-Sternotomy Provides Benefit for Patients with Isolated or Combined Mitral Valve Surgery. Medicina. 2022; 58(2):142. https://doi.org/10.3390/medicina58020142
Chicago/Turabian StyleOezpeker, Cenk Ulvi, Fabian Barbieri, Daniel Hoefer, Nikolaos Bonaros, Michael Grimm, and Ludwig Mueller. 2022. "Upper Hemi-Sternotomy Provides Benefit for Patients with Isolated or Combined Mitral Valve Surgery" Medicina 58, no. 2: 142. https://doi.org/10.3390/medicina58020142
APA StyleOezpeker, C. U., Barbieri, F., Hoefer, D., Bonaros, N., Grimm, M., & Mueller, L. (2022). Upper Hemi-Sternotomy Provides Benefit for Patients with Isolated or Combined Mitral Valve Surgery. Medicina, 58(2), 142. https://doi.org/10.3390/medicina58020142







