Guided-Motion Bicruciate-Stabilized Total Knee Arthroplasty Reproduces Native Medial Collateral Ligament Strain
Abstract
1. Introduction
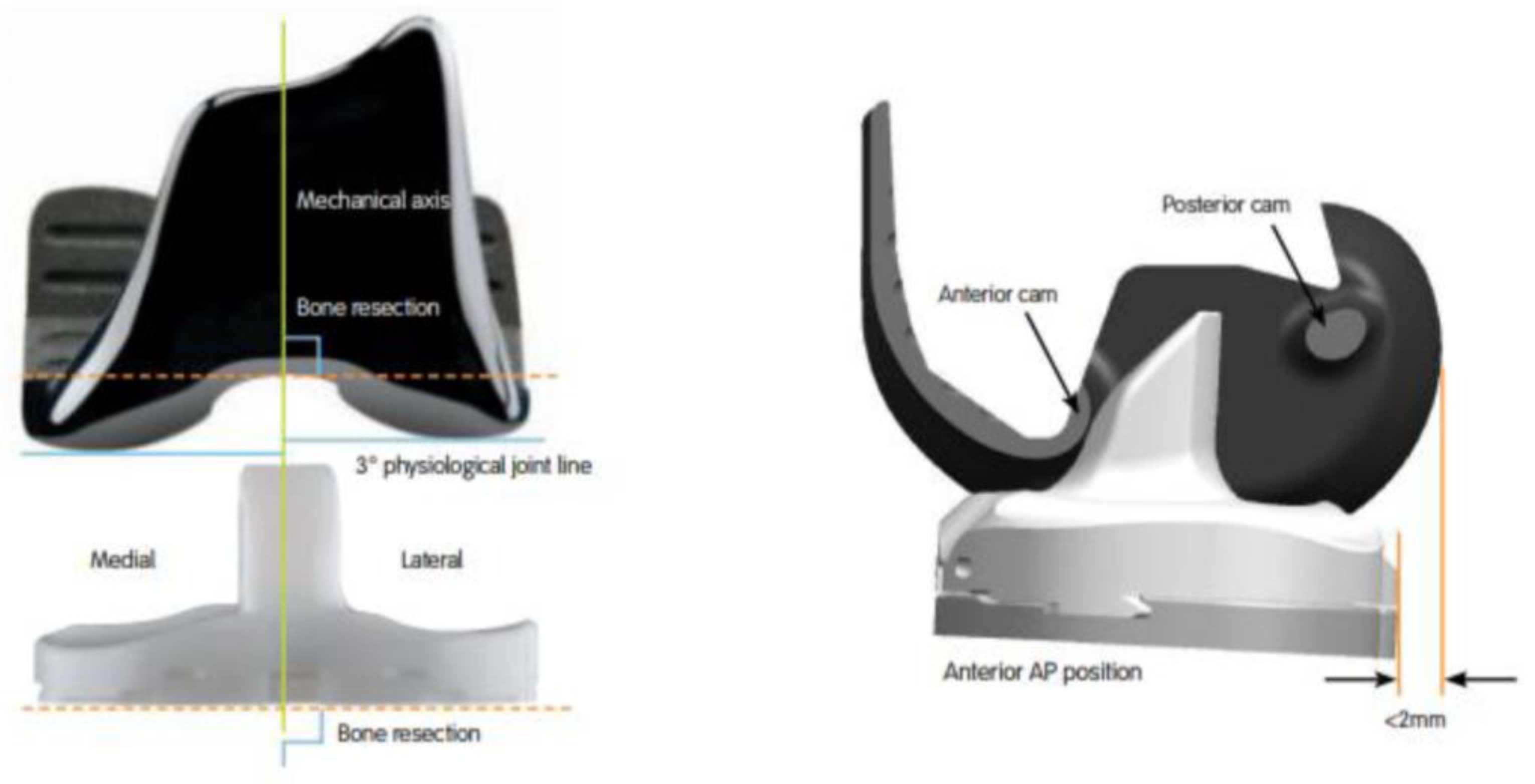
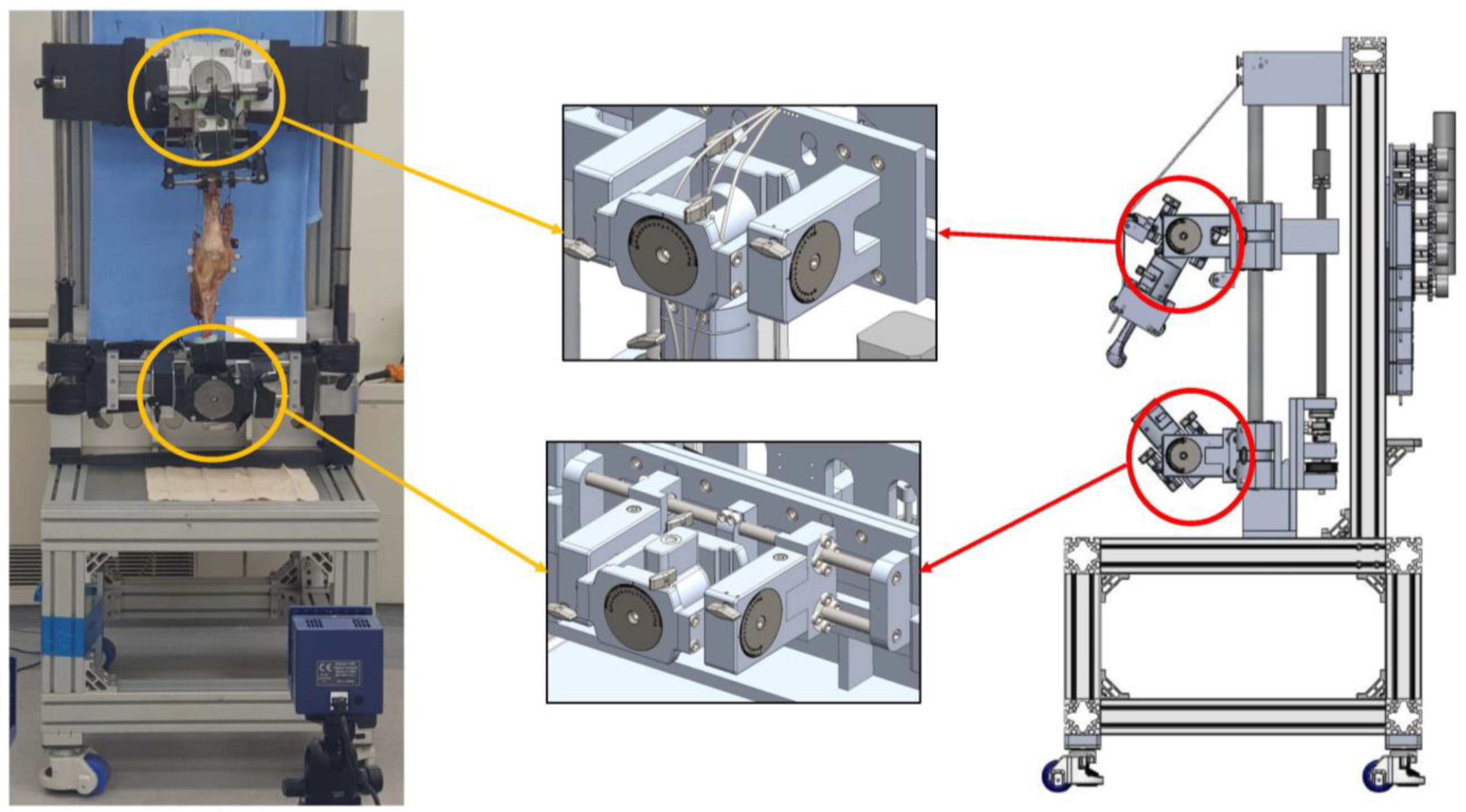
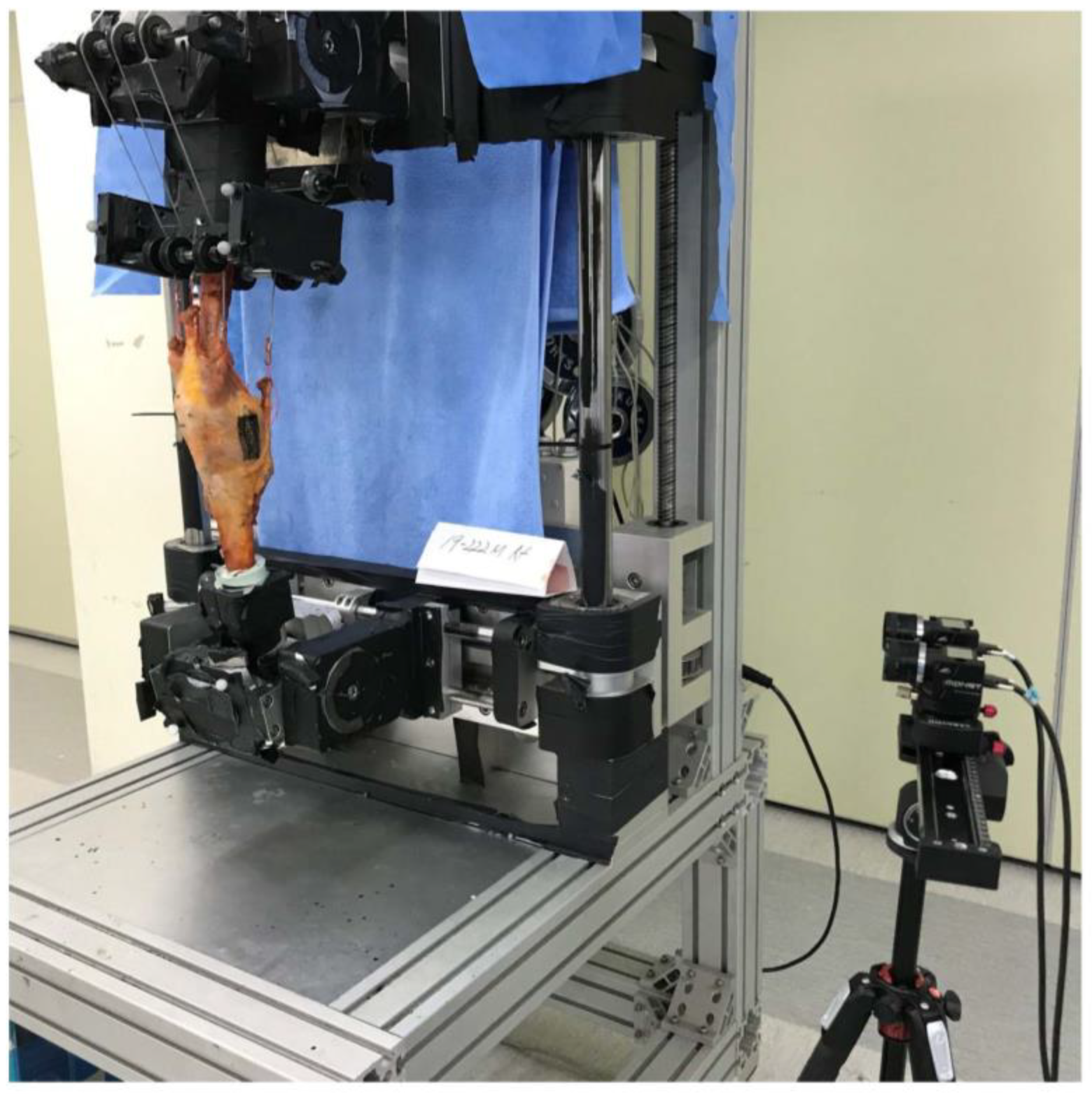
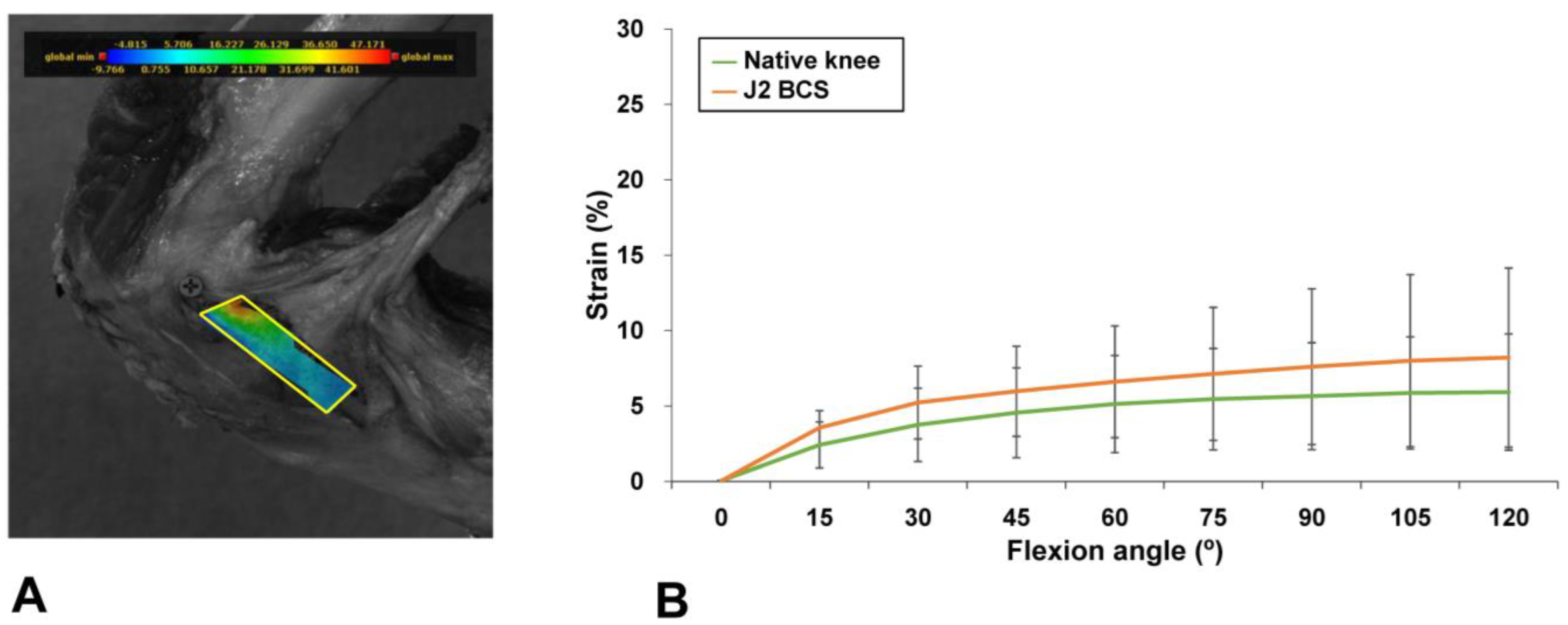
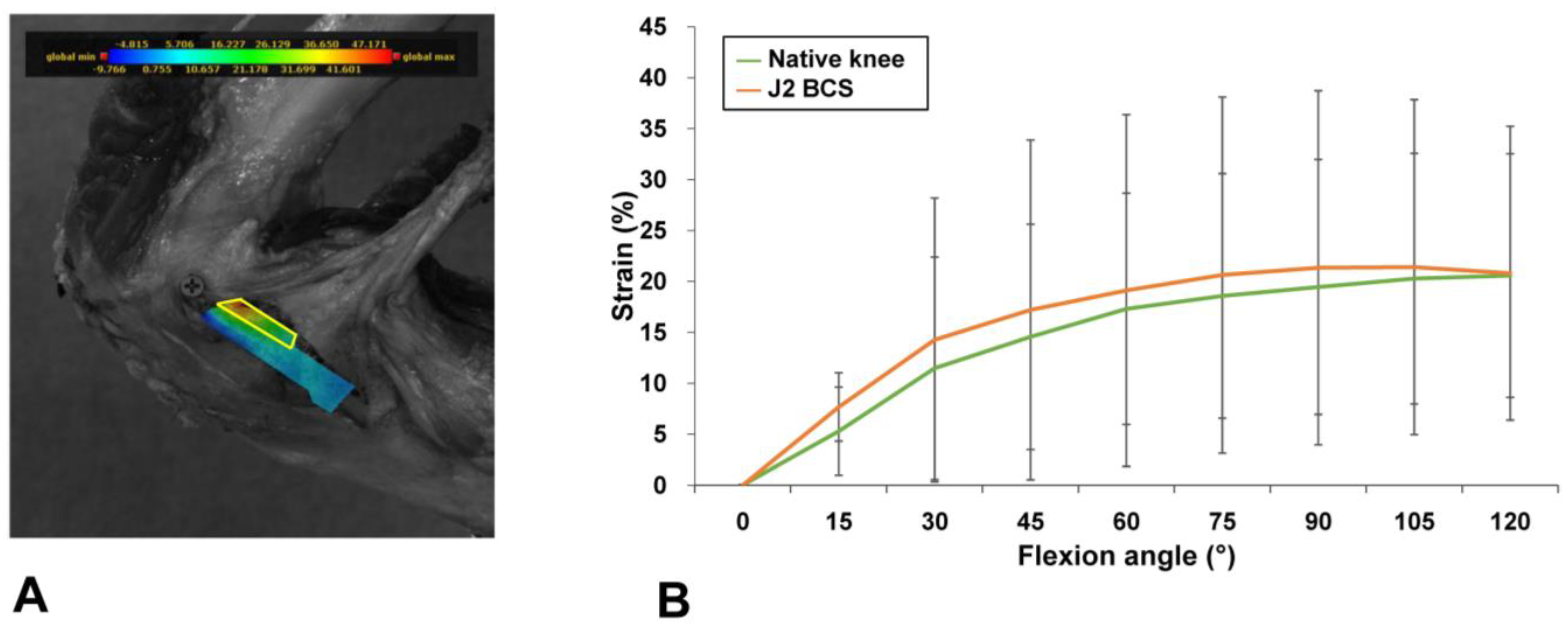
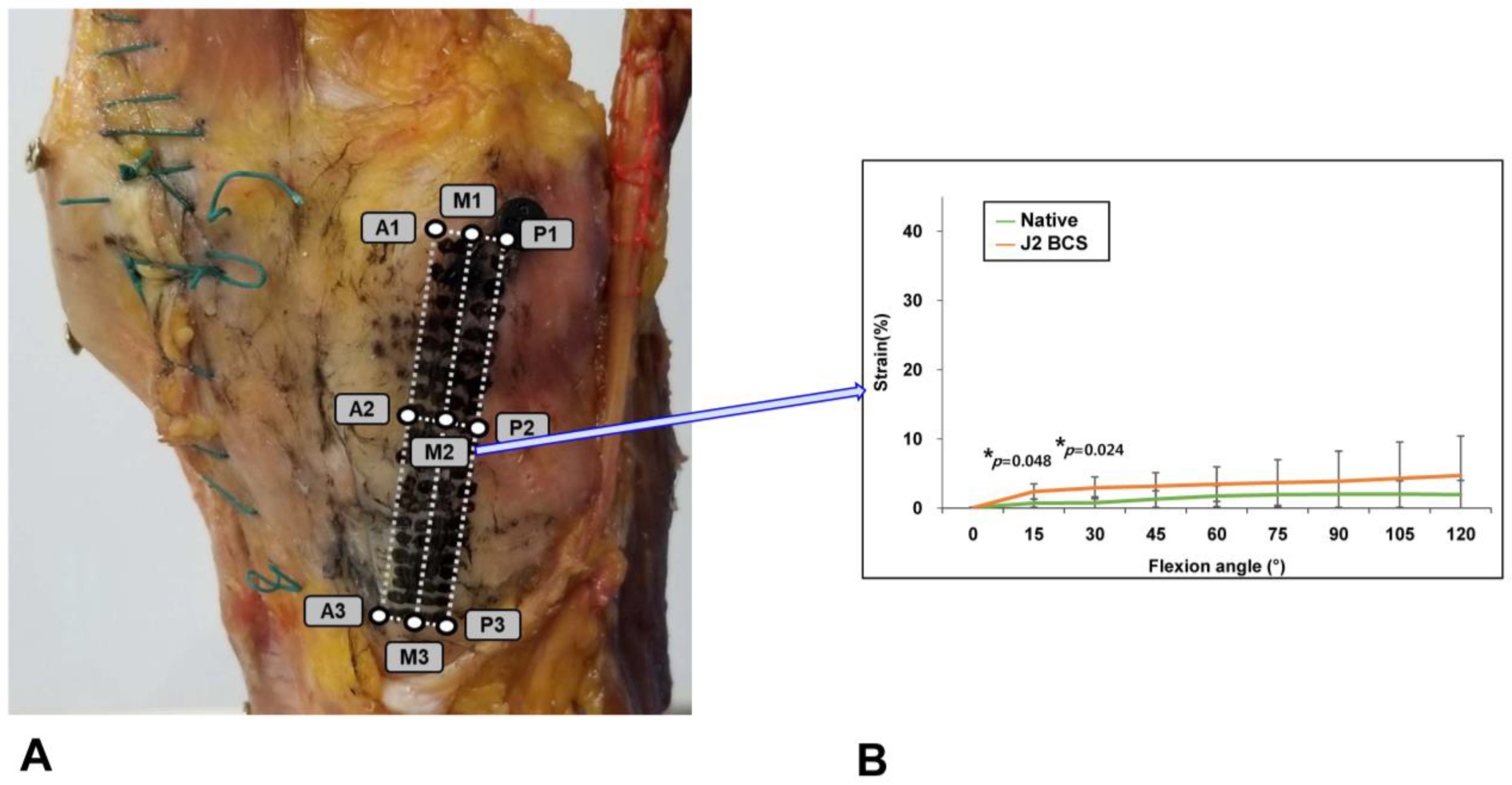
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bourne, R.B.; Chesworth, B.M.; Davis, A.M.; Mahomed, N.N.; Charron, K.D. Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin. Orthop. Relat. Res. 2010, 468, 57–63. [Google Scholar] [CrossRef]
- Nam, D.; Nunley, R.M.; Barrack, R.L. Patient dissatisfaction following total knee replacement: A growing concern? Bone Jt. J. 2014, 96, 96–100. [Google Scholar] [CrossRef]
- Choi, Y.J.; Seo, D.K.; Lee, K.W.; Ra, H.J.; Kang, H.W.; Kim, J.K. Results of total knee arthroplasty for painless, stiff knees. Knee Surg. Relat. Res. 2020, 32, 61. [Google Scholar] [CrossRef]
- Kim, J.; Min, K.D.; Lee, B.I.; Kim, J.B.; Kwon, S.W.; Chun, D.I.; Kim, Y.B.; Seo, G.W.; Lee, J.S.; Park, S.; et al. Comparison of functional outcomes between single-radius and multi-radius femoral components in primary total knee arthroplasty: A meta-analysis of randomized controlled trials. Knee Surg. Relat. Res. 2020, 32, 52. [Google Scholar] [CrossRef]
- Park, C.H.; Song, S.J. Sensor-Assisted Total Knee Arthroplasty: A Narrative Review. Clin. Orthop. Surg. 2021, 13, 1–9. [Google Scholar] [CrossRef]
- Pawar, P.; Naik, L.; Sahu, D.; Bagaria, V. Comparative Study of Pinless Navigation System versus Conventional Instrumentation in Total Knee Arthroplasty. Clin. Orthop. Surg. 2021, 13, 358–365. [Google Scholar] [CrossRef]
- Christen, B.; Kopjar, B. Second-generation bi-cruciate stabilized total knee system has a lower reoperation and revision rate than its predecessor. Arch. Orthop. Trauma Surg. 2018, 138, 1591–1599. [Google Scholar] [CrossRef]
- Grieco, T.F.; Sharma, A.; Dessinger, G.M.; Cates, H.E.; Komistek, R.D. In Vivo Kinematic Comparison of a Bicruciate Stabilized Total Knee Arthroplasty and the Normal Knee Using Fluoroscopy. J. Arthroplast. 2018, 33, 565–571. [Google Scholar] [CrossRef]
- Christen, B.; Neukamp, M.; Aghayev, E. Consecutive series of 226 journey bicruciate substituting total knee replacements: Early complication and revision rates. BMC Musculoskelet. Disord. 2014, 15, 395. [Google Scholar] [CrossRef]
- Hommel, H.; Wilke, K. Good Early Results Obtained with a Guided-Motion Implant for Total Knee Arthroplasty: A Consecutive Case Series. Open Orthop. J. 2017, 11, 51–56. [Google Scholar] [CrossRef][Green Version]
- Iriuchishima, T.; Ryu, K. Bicruciate Substituting Total Knee Arthroplasty Improves Stair Climbing Ability When Compared with Cruciate-Retain or Posterior Stabilizing Total Knee Arthroplasty. Indian J. Orthop. 2019, 53, 641–645. [Google Scholar] [CrossRef]
- Kono, K.; Inui, H.; Tomita, T.; Yamazaki, T.; Taketomi, S.; Sugamoto, K.; Tanaka, S. Bicruciate-stabilised total knee arthroplasty provides good functional stability during high-flexion weight-bearing activities. Knee Surg. Sport. Traumatol. Arthrosc. 2019, 27, 2096–2103. [Google Scholar] [CrossRef]
- Takubo, A.; Ryu, K.; Iriuchishima, T.; Tokuhashi, Y. Comparison of Muscle Recovery Following Bi-cruciate Substituting versus Posterior Stabilized Total Knee Arthroplasty in the Asian Population. J. Knee Surg. 2017, 30, 725–729. [Google Scholar] [CrossRef]
- Delport, H.; Labey, L.; De Corte, R.; Innocenti, B.; Vander Sloten, J.; Bellemans, J. Collateral ligament strains during knee joint laxity evaluation before and after TKA. Clin. Biomech. 2013, 28, 777–782. [Google Scholar] [CrossRef]
- Delport, H.; Labey, L.; Innocenti, B.; De Corte, R.; Vander Sloten, J.; Bellemans, J. Restoration of constitutional alignment in TKA leads to more physiological strains in the collateral ligaments. Knee Surg. Sport. Traumatol. Arthrosc. 2015, 23, 2159–2169. [Google Scholar] [CrossRef]
- Koh, I.J.; Chalmers, C.E.; Lin, C.C.; Park, S.B.; McGarry, M.H.; Lee, T.Q. Posterior stabilized total knee arthroplasty reproduces natural joint laxity compared to normal in kinematically aligned total knee arthroplasty: A matched pair cadaveric study. Arch. Orthop. Trauma Surg. 2021, 141, 119–127. [Google Scholar] [CrossRef]
- Koh, I.J.; Lin, C.C.; Patel, N.A.; Chalmers, C.E.; Maniglio, M.; Han, S.B.; McGarry, M.H.; Lee, T.Q. Kinematically aligned total knee arthroplasty reproduces more native rollback and laxity than mechanically aligned total knee arthroplasty: A matched pair cadaveric study. Orthop. Traumatol. Surg. Res. 2019, 105, 605–611. [Google Scholar] [CrossRef]
- Lim, D.; Kwak, D.S.; Kim, M.; Kim, S.; Cho, H.J.; Choi, J.H.; Koh, I.J. Kinematically aligned total knee arthroplasty restores more native medial collateral ligament strain than mechanically aligned total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2815–2823. [Google Scholar] [CrossRef]
- Pan, B.; Tian, L. Advanced video extensometer for non-contact, real-time, high-accuracy strain measurement. Opt. Express 2016, 24, 19082–19093. [Google Scholar] [CrossRef]
- Villegas, D.F.; Maes, J.A.; Magee, S.D.; Donahue, T.L. Failure properties and strain distribution analysis of meniscal attachments. J. Biomech. 2007, 40, 2655–2662. [Google Scholar] [CrossRef]
- Zavatsky, A.B. A kinematic-freedom analysis of a flexed-knee-stance testing rig. J. Biomech. 1997, 30, 277–280. [Google Scholar] [CrossRef] [PubMed]
- Wickiewicz, T.L.; Roy, R.R.; Powell, P.L.; Edgerton, V.R. Muscle architecture of the human lower limb. Clin Orthop Relat Res 1983, 179, 275–283. [Google Scholar] [CrossRef]
- Hofer, J.K.; Gejo, R.; McGarry, M.H.; Lee, T.Q. Effects of kneeling on tibiofemoral contact pressure and area in posterior cruciate-retaining and posterior cruciate-sacrificing total knee arthroplasty. J. Arthroplast. 2012, 27, 620–624. [Google Scholar] [CrossRef]
- Powers, C.M.; Lilley, J.C.; Lee, T.Q. The effects of axial and multi-plane loading of the extensor mechanism on the patellofemoral joint. Clin. Biomech. 1998, 13, 616–624. [Google Scholar] [CrossRef] [PubMed]
- Koh, I.J.; Kwak, D.S.; Kim, T.K.; Park, I.J.; In, Y. How effective is multiple needle puncturing for medial soft tissue balancing during total knee arthroplasty? A cadaveric study. J. Arthroplast. 2014, 29, 2478–2483. [Google Scholar] [CrossRef] [PubMed]
- LaPrade, R.F.; Engebretsen, A.H.; Ly, T.V.; Johansen, S.; Wentorf, F.A.; Engebretsen, L. The anatomy of the medial part of the knee. J. Bone Jt. Surg. Am. Vol. 2007, 89, 2000–2010. [Google Scholar] [CrossRef]
- Provenzano, P.P.; Heisey, D.; Hayashi, K.; Lakes, R.; Vanderby, R., Jr. Subfailure damage in ligament: A structural and cellular evaluation. J. Appl. Physiol. 2002, 92, 362–371. [Google Scholar] [CrossRef]
- Sullivan, D.; Levy, I.M.; Sheskier, S.; Torzilli, P.A.; Warren, R.F. Medial restraints to anterior-posterior motion of the knee. J. Bone Jt. Surg. Am. Vol. 1984, 66, 930–936. [Google Scholar] [CrossRef]
- Cabuk, H.; Kusku Cabuk, F. Mechanoreceptors of the ligaments and tendons around the knee. Clin. Anat. 2016, 29, 789–795. [Google Scholar] [CrossRef]
- West, J.A.; Scudday, T.; Anderson, S.; Amin, N.H. Clinical outcomes and patient satisfaction after total knee arthroplasty: A follow-up of the first 50 cases by a single surgeon. J. Int. Med. Res. 2019, 47, 1667–1676. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwak, D.-S.; Kim, Y.D.; Cho, N.; Cho, H.-J.; Ko, J.; Kim, M.; Choi, J.H.; Lim, D.; Koh, I.J. Guided-Motion Bicruciate-Stabilized Total Knee Arthroplasty Reproduces Native Medial Collateral Ligament Strain. Medicina 2022, 58, 1751. https://doi.org/10.3390/medicina58121751
Kwak D-S, Kim YD, Cho N, Cho H-J, Ko J, Kim M, Choi JH, Lim D, Koh IJ. Guided-Motion Bicruciate-Stabilized Total Knee Arthroplasty Reproduces Native Medial Collateral Ligament Strain. Medicina. 2022; 58(12):1751. https://doi.org/10.3390/medicina58121751
Chicago/Turabian StyleKwak, Dai-Soon, Yong Deok Kim, Nicole Cho, Ho-Jung Cho, Jaeryong Ko, Minji Kim, Jae Hyuk Choi, Dohyung Lim, and In Jun Koh. 2022. "Guided-Motion Bicruciate-Stabilized Total Knee Arthroplasty Reproduces Native Medial Collateral Ligament Strain" Medicina 58, no. 12: 1751. https://doi.org/10.3390/medicina58121751
APA StyleKwak, D.-S., Kim, Y. D., Cho, N., Cho, H.-J., Ko, J., Kim, M., Choi, J. H., Lim, D., & Koh, I. J. (2022). Guided-Motion Bicruciate-Stabilized Total Knee Arthroplasty Reproduces Native Medial Collateral Ligament Strain. Medicina, 58(12), 1751. https://doi.org/10.3390/medicina58121751







