Citrus Bergamia and Cynara Cardunculus Reduce Serum Uric Acid in Individuals with Non-Alcoholic Fatty Liver Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population and Randomization
2.3. Outcomes
2.4. Preparation of Nutraceutical
2.5. Anthropometric Measurements and Cardiovascular Risk Factors Assessment
2.6. Blood Measurements
2.7. Statistical Analysis
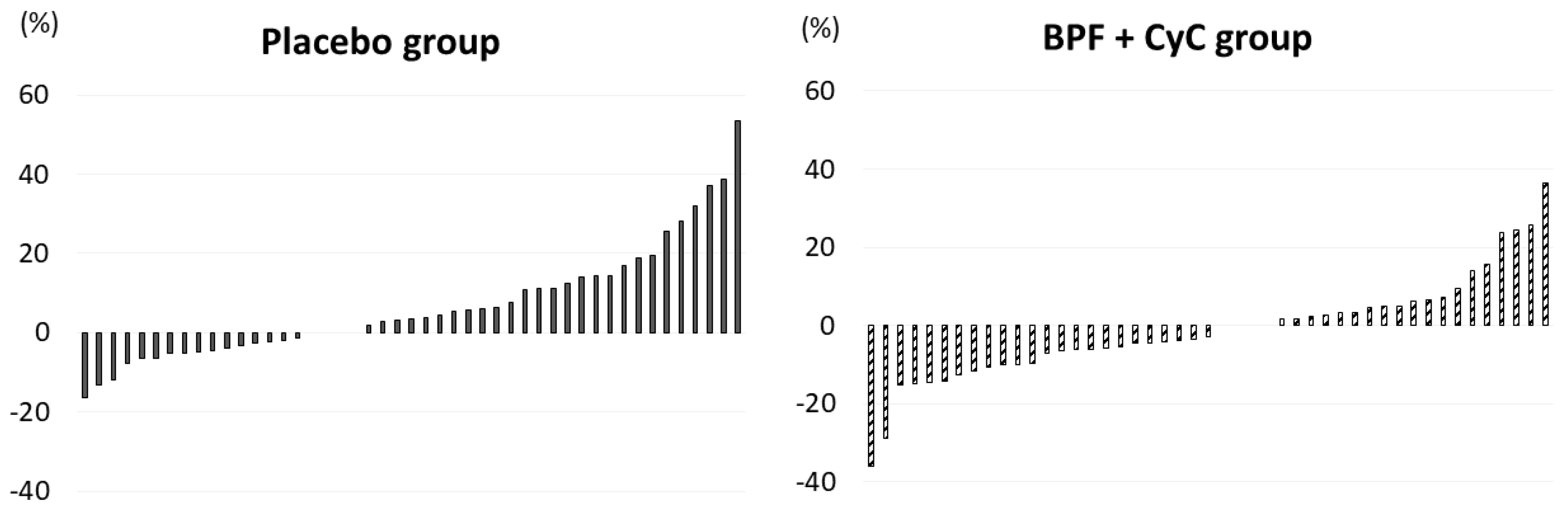
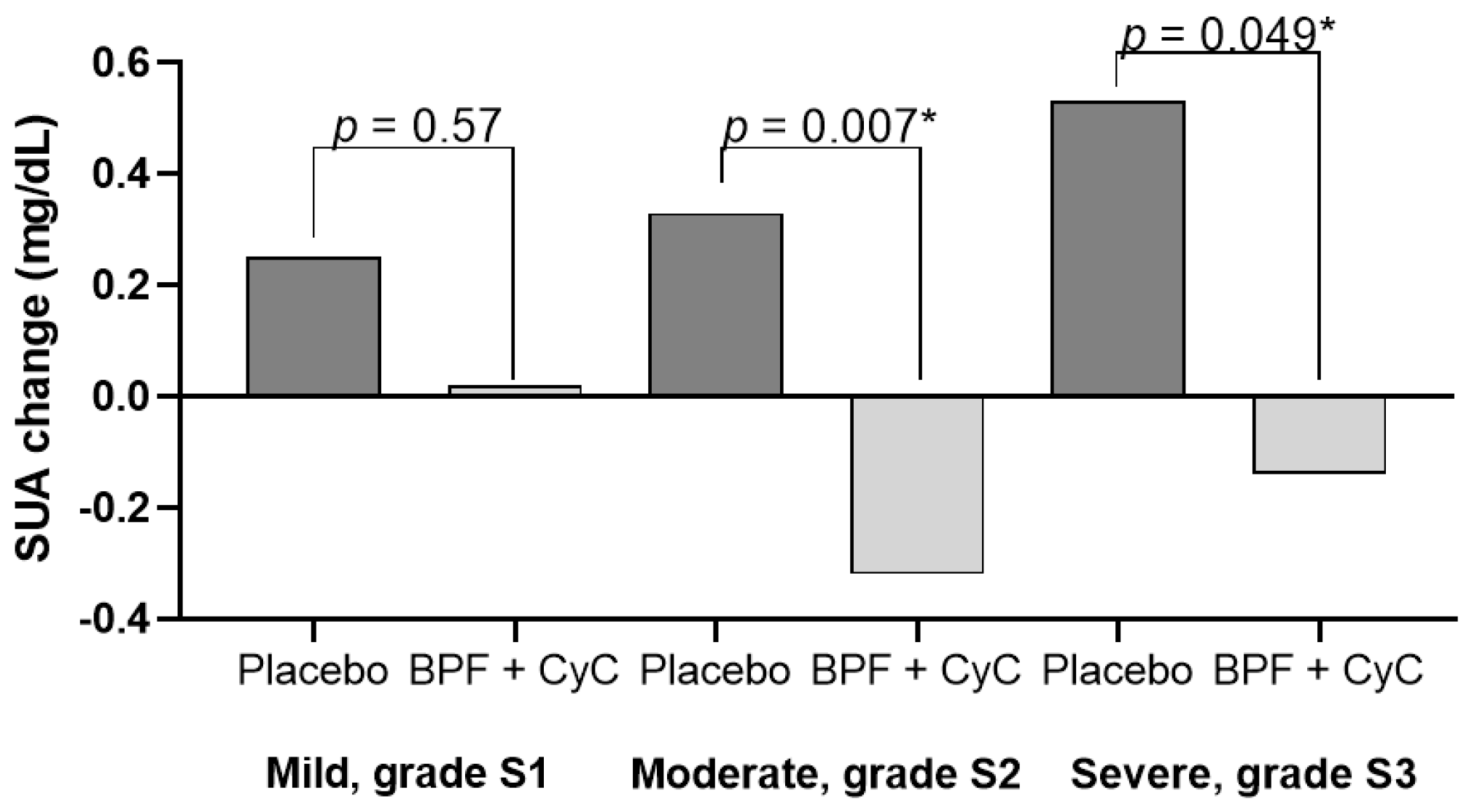
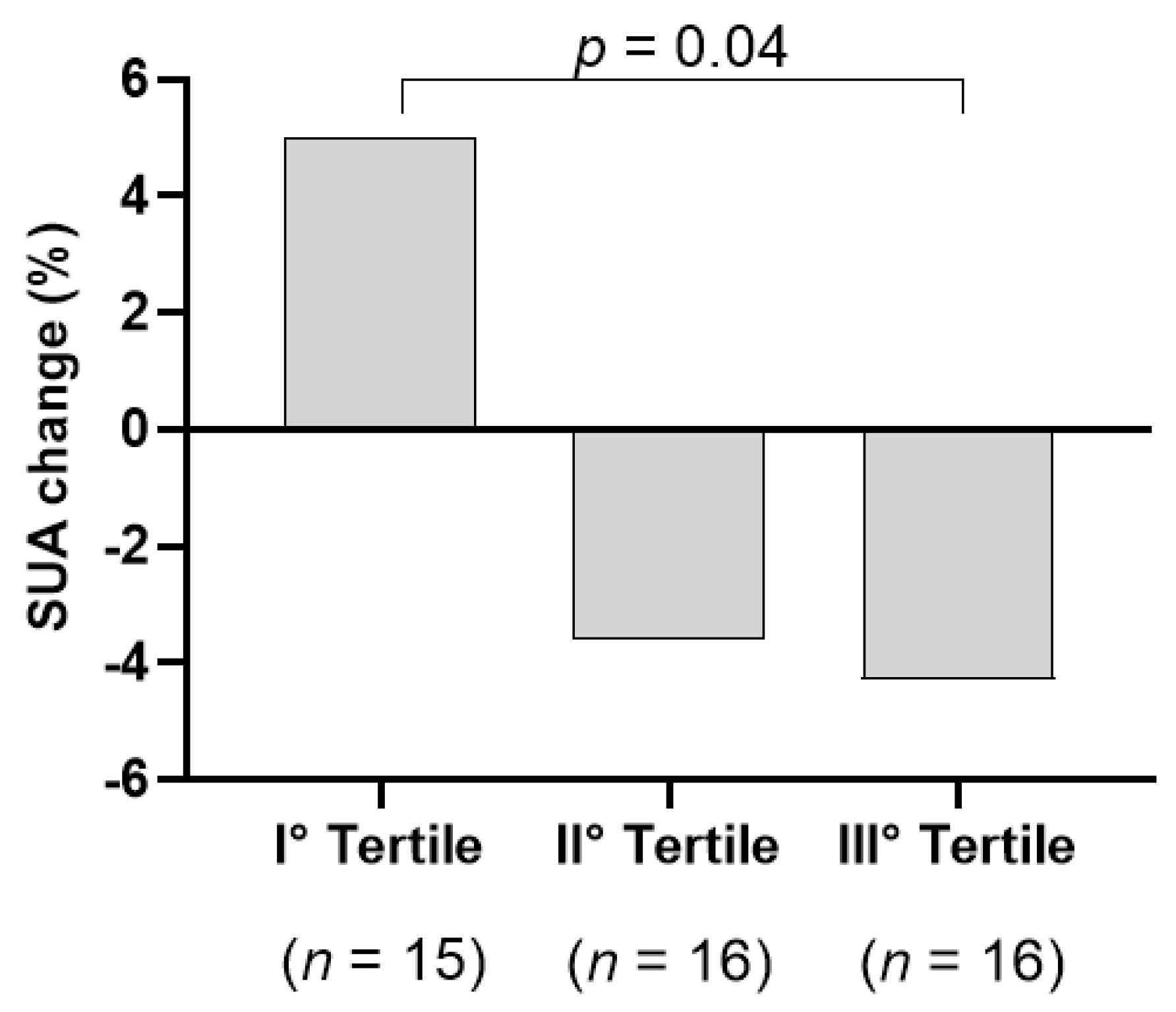
3. Results
4. Discussion
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Oliveira, E.P.; Burini, R.C. High plasma uric acid concentration: Causes and consequences. Diabetol. Metab. Syndr. 2012, 4, 12. [Google Scholar] [CrossRef] [PubMed]
- Maiuolo, J.; Oppedisano, F.; Gratteri, S.; Muscoli, C.; Mollace, V. Regulation of uric acid metabolism and excretion. Int. J. Cardiol. 2016, 213, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Dehlin, M.; Jacobsson, L.; Roddy, E. Global epidemiology of gout: Prevalence, incidence, treatment patterns and risk factors. Nat. Rev. Rheumatol. 2020, 16, 380–390. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A. Racial and gender disparities among patients with gout. Curr. Rheumatol. Rep. 2013, 15, 307. [Google Scholar] [CrossRef]
- Zheng, X.; Wei, Q.; Long, J.; Gong, L.; Chen, H.; Luo, R.; Ren, W.; Wang, Y. Gender-specific association of serum uric acid levels and cardio-ankle vascular index in Chinese adults. Lipids Health Dis. 2018, 17, 80. [Google Scholar] [CrossRef]
- Yu, H.; Zhao, L.; Liu, L.; Li, Y.; Sun, J.; Liu, Y. Relationship between serum uric acid level and nonalcoholic fatty liver disease in type 2 diabetes patients. Medicine 2021, 100, e26946. [Google Scholar] [CrossRef] [PubMed]
- Bao, T.; Ying, Z.; Gong, L.; Du, J.; Ji, G.; Li, Z.; Gao, W.; Jiang, X.; Yang, H.; Huang, Y. Association between serum uric acid and nonalcoholic fatty liver disease in nonobese postmenopausal women: A cross-sectional study. Sci. Rep. 2020, 10, 10072. [Google Scholar] [CrossRef]
- Zheng, X.; Gong, L.; Luo, R.; Chen, H.; Peng, B.; Ren, W.; Wang, Y. Serum uric acid and non-alcoholic fatty liver disease in non-obesity Chinese adults. Lipids Health Dis. 2017, 16, 202. [Google Scholar] [CrossRef]
- Wei, F.; Li, J.; Chen, C.; Zhang, K.; Cao, L.; Wang, X.; Ma, J.; Feng, S.; Li, W.-D. Higher serum uric acid level predicts non-alcoholic fatty liver disease: A 4-year prospective cohort study. Front. Endocrinol. 2020, 11, 179. [Google Scholar] [CrossRef]
- Ma, Z.; Zhang, J.; Kang, X.; Xu, C.; Sun, C.; Tao, L.; Zheng, D.; Han, Y.; Li, Q.; Guo, X. Hyperuricemia precedes non-alcoholic fatty liver disease with abdominal obesity moderating this unidirectional relationship: Three longitudinal analyses. Atherosclerosis 2020, 311, 44–51. [Google Scholar] [CrossRef]
- Fernández Rodríguez, C.M.; Aller, R.; Gutiérrez García, M.L.; Ampuero, J.; Gómez-Camarero, J.; Martín-Mateos, R.; Burgos-Santamaría, D.; Rosales, J.M.; Aspichueta, P.; Buque, X.; et al. Higher levels of serum uric acid influences hepatic damage in patients with non-alcoholic fatty liver disease (NAFLD). Rev. Esp. Enferm. Dig. Organo Of. Soc. Esp. Patol. Dig. 2019, 111, 264–269. [Google Scholar] [CrossRef]
- Jaruvongvanich, V.; Ahuja, W.; Wirunsawanya, K.; Wijarnpreecha, K.; Ungprasert, P. Hyperuricemia is associated with nonalcoholic fatty liver disease activity score in patients with nonalcoholic fatty liver disease: A systematic review and meta-analysis. Eur. J. Gastroenterol. Hepatol. 2017, 29, 1031–1035. [Google Scholar] [CrossRef] [PubMed]
- Mosca, A.; Nobili, V.; De Vito, R.; Crudele, A.; Scorletti, E.; Villani, A.; Alisi, A.; Byrne, C.D. Serum uric acid concentrations and fructose consumption are independently associated with NASH in children and adolescents. J. Hepatol. 2017, 66, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Saito, Y.; Tanaka, A.; Node, K.; Kobayashi, Y. Uric acid and cardiovascular disease: A clinical review. J. Cardiol. 2021, 78, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Agnoletti, D.; Cicero, A.F.G.; Borghi, C. The Impact of Uric Acid and Hyperuricemia on Cardiovascular and Renal Systems. Cardiol. Clin. 2021, 39, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Seki, H.; Kaneko, H.; Morita, H.; Itoh, H.; Morita, K.; Matsuoka, S.; Kiriyama, H.; Kamon, T.; Fujiu, K.; Michihata, N.; et al. Relation of Serum Uric Acid and Cardiovascular Events in Young Adults Aged 20–49 Years. Am. J. Cardiol. 2021, 152, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Virdis, A.; Masi, S.; Casiglia, E.; Tikhonoff, V.; Cicero, A.F.G.; Ungar, A.; Rivasi, G.; Salvetti, M.; Barbagallo, C.M.; Bombelli, M.; et al. Identification of the Uric Acid Thresholds Predicting an Increased Total and Cardiovascular Mortality Over 20 Years. Hypertension 2020, 75, 302–308. [Google Scholar] [CrossRef]
- Gliozzi, M.; Malara, N.; Muscoli, S.; Mollace, V. The treatment of hyperuricemia. Int. J. Cardiol. 2016, 213, 23–27. [Google Scholar] [CrossRef]
- Strilchuk, L.; Fogacci, F.; Cicero, A.F. Safety and tolerability of available urate-lowering drugs: A critical review. Expert Opin. Drug Saf. 2019, 18, 261–271. [Google Scholar] [CrossRef]
- Huang, C.H.; Chu, M.P.; Chen, W.W. Examining the use of allopurinol: Perspectives from recent drug injury relief applications. J. Formos. Med. Assoc. Taiwan Yi Zhi 2019, 118, 371–377. [Google Scholar] [CrossRef]
- Ferramosca, A.; Di Giacomo, M.; Zara, V. Antioxidant dietary approach in treatment of fatty liver: New insights and updates. World J Gastroenterol 2017, 23, 4146–4157. [Google Scholar] [CrossRef] [PubMed]
- Roumeliotis, S.; Roumeliotis, A.; Dounousi, E.; Eleftheriadis, T.; Liakopoulos, V. Dietary Antioxidant Supplements and Uric Acid in Chronic Kidney Disease: A Review. Nutrients 2019, 11, 1911. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.L.; Gong, X.; Ji, M.Y.; Wang, C.C.; Wang, J.H.; Li, M.H. Bioactive Compounds from Plant-Based Functional Foods: A Promising Choice for the Prevention and Management of Hyperuricemia. Foods 2020, 9, 973. [Google Scholar] [CrossRef] [PubMed]
- Toyoda, Y.; Takada, T.; Saito, H.; Hirata, H.; Ota-Kontani, A.; Kobayashi, N.; Tsuchiya, Y.; Suzuki, H. Inhibitory effect of Citrus flavonoids on the in vitro transport activity of human urate transporter 1 (URAT1/SLC22A12), a renal re-absorber of urate. NPJ Sci. Food 2020, 4, 3. [Google Scholar] [CrossRef]
- Escudero-López, B.; Ortega, Á.; Cerrillo, I.; Rodríguez-Griñolo, M.R.; Muñoz-Hernández, R.; Macher, H.C.; Martín, F.; Hornero-Méndez, D.; Mena, P.; Del Rio, D.; et al. Consumption of orange fermented beverage improves antioxidant status and reduces peroxidation lipid and inflammatory markers in healthy humans. J. Sci. Food Agric. 2018, 98, 2777–2786. [Google Scholar] [CrossRef]
- Haidari, F.; Ali Keshavarz, S.; Reza Rashidi, M.; Mohammad Shahi, M. Orange juice and hesperetin supplementation to hyperuricemic rats alter oxidative stress markers and xanthine oxidoreductase activity. J. Clin. Biochem. Nutr. 2009, 45, 285–291. [Google Scholar] [CrossRef]
- Chen, L.; Li, M.; Wu, J.L.; Li, J.X.; Ma, Z.C. Effect of lemon water soluble extract on hyperuricemia in a mouse model. Food Funct. 2019, 10, 6000–6008. [Google Scholar] [CrossRef]
- Alkushi, A.G. Biological Effect of Cynara cardunculus on Kidney Status of Hypercholesterolemic Rats. Pharmacogn. Mag. 2017, 13, S430–S436. [Google Scholar] [CrossRef]
- Ferro, Y.; Pujia, R.; Mazza, E.; Lascala, L.; Lodari, O.; Maurotti, S.; Pujia, A.; Montalcini, T. A new nutraceutical (Livogen Plus®) improves liver steatosis in adults with non-alcoholic fatty liver disease. J. Transl. Med. 2022, 20, 377. [Google Scholar] [CrossRef]
- Mirarchi, A.; Mare, R.; Musolino, V.; Nucera, S.; Mollace, V.; Pujia, A.; Montalcini, T.; Romeo, S.; Maurotti, S. Bergamot Polyphenol Extract Reduces Hepatocyte Neutral Fat by Increasing Beta-Oxidation. Nutrients 2022, 14, 3434. [Google Scholar] [CrossRef]
- Parafati, M.; Lascala, A.; La Russa, D.; Mignogna, C.; Trimboli, F.; Morittu, V.M.; Riillo, C.; Macirella, R.; Mollace, V.; Brunelli, E.; et al. Bergamot Polyphenols Boost Therapeutic Effects of the Diet on Non-Alcoholic Steatohepatitis (NASH) Induced by “Junk Food”: Evidence for Anti-Inflammatory Activity. Nutrients 2018, 10, 1604. [Google Scholar] [CrossRef] [PubMed]
- Kamel, A.M.; Farag, M.A. Therapeutic Potential of Artichoke in the Treatment of Fatty Liver: A Systematic Review and Meta-Analysis. J. Med. Food 2022, 25, 931–942. [Google Scholar] [CrossRef] [PubMed]
- Ferro, Y.; Montalcini, T.; Mazza, E.; Foti, D.; Angotti, E.; Gliozzi, M.; Nucera, S.; Paone, S.; Bombardelli, E.; Aversa, I. Randomized clinical trial: Bergamot citrus and wild cardoon reduce liver steatosis and body weight in non-diabetic individuals aged over 50 years. Front. Endocrinol. 2020, 11, 494. [Google Scholar] [CrossRef] [PubMed]
- Musolino, V.; Gliozzi, M.; Bombardelli, E.; Nucera, S.; Carresi, C.; Maiuolo, J.; Mollace, R.; Paone, S.; Bosco, F.; Scarano, F. The synergistic effect of Citrus bergamia and Cynara cardunculus extracts on vascular inflammation and oxidative stress in non-alcoholic fatty liver disease. J. Tradit. Complement. Med. 2020, 10, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Ferro, Y.; Carè, I.; Mazza, E.; Provenzano, F.; Colica, C.; Torti, C.; Romeo, S.; Pujia, A.; Montalcini, T. Protein and vitamin B6 intake are associated with liver steatosis assessed by transient elastography, especially in obese individuals. Clin. Mol. Hepatol. 2017, 23, 249. [Google Scholar] [CrossRef]
- Ferro, Y.; Mazza, E.; Angotti, E.; Pujia, R.; Mirarchi, A.; Salvati, M.A.; Terracciano, R.; Savino, R.; Romeo, S.; Scuteri, A. Effect of a novel functional tomato sauce (OsteoCol) from vine-ripened tomatoes on serum lipids in individuals with common hypercholesterolemia: Tomato sauce and hypercholesterolemia. J. Transl. Med. 2021, 19, 19. [Google Scholar] [CrossRef]
- Ben Salem, C.; Slim, R.; Fathallah, N.; Hmouda, H. Drug-induced hyperuricaemia and gout. Rheumatology 2017, 56, 679–688. [Google Scholar] [CrossRef]
- Moriwaki, Y. Effects on uric acid metabolism of the drugs except the antihyperuricemics. J. Bioequivalence Bioavailab. 2014, 6, 10. [Google Scholar] [CrossRef]
- Shi, Y. Caught red-handed: Uric acid is an agent of inflammation. J. Clin. Investig. 2010, 120, 1809–1811. [Google Scholar] [CrossRef]
- Spiga, R.; Marini, M.A.; Mancuso, E.; Di Fatta, C.; Fuoco, A.; Perticone, F.; Andreozzi, F.; Mannino, G.C.; Sesti, G. Uric Acid Is Associated with Inflammatory Biomarkers and Induces Inflammation Via Activating the NF-κB Signaling Pathway in HepG2 Cells. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 1241–1249. [Google Scholar] [CrossRef]
- Biernatkaluza, E.; Schlesinger, N. SAT0318 Lemon Juice Reduces Serum Uric Acid Level Via Alkalization of Urine in Gouty and Hyperuremic Patients—A Pilot Study. Ann. Rheum. Dis. 2015, 74, 774. [Google Scholar] [CrossRef]
- Wang, H.; Cheng, L.; Lin, D.; Ma, Z.; Deng, X. Lemon fruits lower the blood uric acid levels in humans and mice. Sci. Hortic. 2017, 220, 4–10. [Google Scholar] [CrossRef]
- Liu, K.; Wang, W.; Guo, B.H.; Gao, H.; Liu, Y.; Liu, X.H.; Yao, H.L.; Cheng, K. Chemical Evidence for Potent Xanthine Oxidase Inhibitory Activity of Ethyl Acetate Extract of Citrus aurantium L. Dried Immature Fruits. Molecules. 2016, 21, 302. [Google Scholar] [CrossRef]
- Mo, S.-F.; Zhou, F.; Lv, Y.-Z.; Hu, Q.-H.; Zhang, D.-M.; Kong, L.-D. Hypouricemic action of selected flavonoids in mice: Structure–activity relationships. Biol. Pharm. Bull. 2007, 30, 1551–1556. [Google Scholar] [CrossRef]
- Sarawek, S.; Feistel, B.; Pischel, I.; Butterweck, V. Flavonoids of Cynara scolymus possess potent xanthinoxidase inhibitory activity in vitro but are devoid of hypouricemic effects in rats after oral application. Planta Med. 2008, 74, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Meng, Z.Q.; Tang, Z.H.; Yan, Y.X.; Guo, C.R.; Cao, L.; Ding, G.; Huang, W.Z.; Wang, Z.Z.; Wang, K.D.; Xiao, W.; et al. Study on the anti-gout activity of chlorogenic acid: Improvement on hyperuricemia and gouty inflammation. Am. J. Chin. Med. 2014, 42, 1471–1483. [Google Scholar] [CrossRef]
- Meydani, M.; Hasan, S.T. Dietary polyphenols and obesity. Nutrients 2010, 2, 737–751. [Google Scholar] [CrossRef]
- EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J. Hepatol. 2016, 64, 1388–1402. [CrossRef]
- Sasso, M.; Beaugrand, M.; de Ledinghen, V.; Douvin, C.; Marcellin, P.; Poupon, R.; Sandrin, L.; Miette, V. Controlled attenuation parameter (CAP): A novel VCTE™ guided ultrasonic attenuation measurement for the evaluation of hepatic steatosis: Preliminary study and validation in a cohort of patients with chronic liver disease from various causes. Ultrasound Med. Biol. 2010, 36, 1825–1835. [Google Scholar] [CrossRef]
- Salmi, A.; di Filippo, L.; Ferrari, C.; Frara, S.; Giustina, A. Ultrasound and FibroScan® Controlled Attenuation Parameter in patients with MAFLD: Head to head comparison in assessing liver steatosis. Endocrine 2022, 78, 262–269. [Google Scholar] [CrossRef]
- EASL Clinical Practice Guidelines on non-invasive tests for evaluation of liver disease severity and prognosis—2021 update. J. Hepatol. 2021, 75, 659–689. [CrossRef] [PubMed]
- de Barros, F.; Fonseca, A.B.M. Bariatric surgery during the evolution of fatty liver-A randomized clinical trial comparing gastric bypass and sleeve gastrectomy based on transient elastography. Clin. Obes. 2020, 10, e12393. [Google Scholar] [CrossRef] [PubMed]
- Eilenberg, M.; Munda, P.; Stift, J.; Langer, F.B.; Prager, G.; Trauner, M.; Staufer, K. Accuracy of non-invasive liver stiffness measurement and steatosis quantification in patients with severe and morbid obesity. Hepatobiliary Surg. Nutr. 2021, 10, 610–622. [Google Scholar] [CrossRef] [PubMed]
- Tang, O.; Miller, E.R., 3rd; Gelber, A.C.; Choi, H.K.; Appel, L.J.; Juraschek, S.P. DASH diet and change in serum uric acid over time. Clin. Rheumatol. 2017, 36, 1413–1417. [Google Scholar] [CrossRef] [PubMed]
- Cutolo, M.; Cimmino, M.A.; Perez-Ruiz, F. Potency on lowering serum uric acid in gout patients: A pooled analysis of registrative studies comparing febuxostat vs. allopurinol. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 4186–4195. [Google Scholar]
- Bai, L.; Zhou, J.B.; Zhou, T.; Newson, R.B.; Cardoso, M.A. Incident gout and weight change patterns: A retrospective cohort study of US adults. Arthritis Res. Ther. 2021, 23, 69. [Google Scholar] [CrossRef]
| Variables | Placebo (n = 47) | BPF + CyC (n = 47) | p-Value |
|---|---|---|---|
| Age (years) | 50 ± 11 | 52 ± 9 | 0.37 |
| Weight (Kg) | 80.0 ± 10 | 79.9 ± 13 | 0.95 |
| BMI (Kg/m2) | 28.9 ± 4 | 29.1 ± 3 | 0.79 |
| WHR | 0.91 ± 0.1 | 1.12 ± 1.2 | 0.26 |
| SBP (mmHg) | 112 ± 17 | 112 ± 15 | 0.99 |
| DBP (mmHg) | 71 ± 14 | 73 ± 11 | 0.55 |
| CAP score (dB/m) | 286 ± 40 | 294 ± 39 | 0.30 |
| IQR | 11 ± 5 | 11 ± 4 | 0.96 |
| Glucose (mg/dL) | 92 ± 8 | 92 ± 7 | 0.75 |
| HOMA-IR | 2.28 ± 1.0 | 2.32 ± 1.3 | 0.88 |
| TC (mg/dL) | 193 ± 38 | 188 ± 34 | 0.49 |
| TG (mg/dL) | 115 ± 50 | 102 ± 46 | 0.16 |
| HDL-C (mg/dL) | 50 ± 12 | 53 ± 12 | 0.30 |
| LDL-C (mg/dL) | 120 ± 33 | 115 ± 31 | 0.46 |
| AST (IU/L) | 24 ± 15 | 21 ± 6 | 0.21 |
| ALT (IU/L) | 33 ± 28 | 24 ± 13 | 0.05 |
| γGT (UI/L) | 27 ± 20 | 25 ± 18 | 0.73 |
| SUA (mg/dL) | 5.2 ± 1.1 | 5.1 ± 1.1 | 0.82 |
| Creatinine (mg/dL) | 0.82 ± 0.1 | 0.81 ± 0.1 | 0.72 |
| Total bilirubin (mg/dL) | 0.62 ± 0.3 | 0.63 ± 0.3 | 0.95 |
| Prevalence | |||
| Gender (Male, %) | 60 | 55 | 0.83 |
| Physical activity (%) | 47 | 49 | 1 |
| Smokers (%) | 9 | 28 | 0.030 |
| Obesity (%) | 40 | 32 | 0.87 |
| Hypertension (%) | 32 | 34 | 1 |
| Hyperlipidemia (%) | 52 | 46 | 0.67 |
| Antihypertensive drugs (%) | 26 | 30 | 0.81 |
| Beta-blockers (%) | 9 | 6 | 1 |
| Diuretics (%) | 6 | 11 | 0.71 |
| Lipid-lowering agents (%) | 9 | 17 | 0.35 |
| Antiplatelet agents (%) | 4 | 11 | 0.43 |
| Urate-lowering drugs (%) | 4 | 0 | 0.49 |
| Variables | Placebo (n = 47) | BPF + CyC (n = 47) | p-Value |
|---|---|---|---|
| Weight (Kg) | −2.1 ± 1.8 | −3.1 ± 2.3 | 0.031 |
| BMI (Kg/m2) | −0.8 ± 0.6 | −1.1 ± 0.8 | 0.026 |
| WHR | −0.001 ± 0.04 | −0.19 ± 1.2 | 0.29 |
| Glucose (mg/dL) | −0.4 ± 6.7 | −0.6 ± 6.7 | 0.87 |
| HOMA-IR | −0.3 ± 0.8 | −0.5 ± 1 | 0.50 |
| TG (mg/dL) | −14.7 ± 39 | 0.6 ± 54 | 0.12 |
| HDL-C (mg/dL) | −0.4 ± 6 | −3 ± 5 | 0.34 |
| LDL-C (mg/dL) | −2.6 ± 28 | −9.1 ± 14 | 0.35 |
| AST (IU/L) | −2.4 ± 6 | −1.1 ± 6 | 0.34 |
| ALT (IU/L) | −6.1 ± 13 | −2.7 ± 6 | 0.10 |
| γGT (UI/L) | −3.7 ± 9 | −6.0 ± 9 | 0.22 |
| SUA (mg/dL) | 0.3 ± 0.7 | −0.1 ± 0.7 | 0.004 |
| aSUA (mg/dL) * | 0.3 ± 0.1 | −0.1 ± 0.1 | 0.005 |
| SUA (%) | 6.7 ± 14 | −1.1 ± 13 | 0.008 |
| aSUA (%) * | 6.6 ± 2 | −1.0 ± 2 | 0.012 |
| Creatinine (mg/dL) | −0.004 ± 0.08 | −0.006 ± 0.07 | 0.91 |
| C.I. 95% | ||||||
|---|---|---|---|---|---|---|
| Dependent Variable SUA Change | B | SE | β | p-Value | LL | UL |
| Treatment | −0.43 | 0.14 | −0.29 | 0.004 | −0.71 | −0.14 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferro, Y.; Maurotti, S.; Mazza, E.; Pujia, R.; Sciacqua, A.; Musolino, V.; Mollace, V.; Pujia, A.; Montalcini, T. Citrus Bergamia and Cynara Cardunculus Reduce Serum Uric Acid in Individuals with Non-Alcoholic Fatty Liver Disease. Medicina 2022, 58, 1728. https://doi.org/10.3390/medicina58121728
Ferro Y, Maurotti S, Mazza E, Pujia R, Sciacqua A, Musolino V, Mollace V, Pujia A, Montalcini T. Citrus Bergamia and Cynara Cardunculus Reduce Serum Uric Acid in Individuals with Non-Alcoholic Fatty Liver Disease. Medicina. 2022; 58(12):1728. https://doi.org/10.3390/medicina58121728
Chicago/Turabian StyleFerro, Yvelise, Samantha Maurotti, Elisa Mazza, Roberta Pujia, Angela Sciacqua, Vincenzo Musolino, Vincenzo Mollace, Arturo Pujia, and Tiziana Montalcini. 2022. "Citrus Bergamia and Cynara Cardunculus Reduce Serum Uric Acid in Individuals with Non-Alcoholic Fatty Liver Disease" Medicina 58, no. 12: 1728. https://doi.org/10.3390/medicina58121728
APA StyleFerro, Y., Maurotti, S., Mazza, E., Pujia, R., Sciacqua, A., Musolino, V., Mollace, V., Pujia, A., & Montalcini, T. (2022). Citrus Bergamia and Cynara Cardunculus Reduce Serum Uric Acid in Individuals with Non-Alcoholic Fatty Liver Disease. Medicina, 58(12), 1728. https://doi.org/10.3390/medicina58121728









