Serum Uromodulin, a Potential Biomarker of Tubulointerstitial Damage, Correlates Well with Measured GFR and ERPF in Patients with Obstructive Nephropathy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Study Protocol
2.3. Measurement of Uromodulin Concentration
2.4. Assessment of Renal Function
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Renal Function Parameters
3.3. Serum Uromodulin
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhang, Z.H.; He, J.Q.; Qin, W.W.; Zhao, Y.Y.; Tan, N.H. Biomarkers of obstructive nephropathy using a metabolomics approach in rat. Chem. Biol. Interact. 2018, 296, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Mezzano, S.A.; Ruiz-Ortega, M.; Egido, J. Angiotensin II and renal fibrosis. Hypertension 2001, 38, 635–638. [Google Scholar] [CrossRef]
- Rüster, C.; Wolf, G. Renin-angiotensin-aldosterone system and progression of renal disease. J. Am. Soc. Nephrol. 2006, 17, 2985–2991. [Google Scholar] [CrossRef] [PubMed]
- Mao, W.; Liu, S.; Wang, K.; Wang, M.; Shi, H.; Liu, Q.; Bao, M.; Peng, B.; Geng, J. Cystatin C in Evaluating Renal Function in Ureteral Calculi Hydronephrosis in Adults. Kidney Blood Press. Res. 2020, 45, 109–121. [Google Scholar] [CrossRef] [PubMed]
- Washino, S.; Hosohata, K.; Miyagawa, T. Roles Played by Biomarkers of Kidney Injury in Patients with Upper Urinary Tract Obstruction. Int. J. Mol. Sci. 2020, 21, 5490. [Google Scholar] [CrossRef]
- Pennica, D.; Kohr, W.J.; Kuang, W.J.; Glaister, D.; Aggarwal, B.B.; Chen, E.Y.; Goeddel, D.V. Identification of human uromodulin as the Tamm-Horsfall urinary glycoprotein. Science 1987, 236, 83–88. [Google Scholar] [CrossRef]
- El-Achkar, T.M.; Wu, X.R. Uromodulin in kidney injury: An instigator, bystander, or protector? Am. J. Kidney Dis. 2012, 59, 452–461. [Google Scholar] [CrossRef] [PubMed]
- Devuyst, O.; Olinger, E.; Rampoldi, L. Uromodulin: From physiology to rare and complex kidney disorders. Nat. Rev. Nephrol. 2017, 13, 525–544. [Google Scholar] [CrossRef] [PubMed]
- Lhotta, K. Uromodulin and chronic kidney disease. Kidney Blood Press. Res. 2010, 33, 393–398. [Google Scholar] [CrossRef]
- Devuyst, O.; Pattaro, C. The UMOD Locus: Insights into the Pathogenesis and Prognosis of Kidney Disease. J. Am. Soc. Nephrol. 2018, 29, 713–726. [Google Scholar] [CrossRef]
- Thornley, C.; Dawnay, A.; Cattell, W.R. Human Tamm-Horsfall glycoprotein: Urinary and plasma levels in normal subjects and patients with renal disease determined by a fully validated radioimmunoassay. Clin. Sci. 1985, 68, 529–535. [Google Scholar] [CrossRef] [PubMed]
- Levey, A.S.; Coresh, J.; Bolton, K.; Culleton, B.; Harvey, K.S.; Ikizler, T.A.; Johnson, C.A.; Kausz, A.; Kimmel, P.L.; Kusek, J.; et al. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am. J. Kidney Dis. 2002, 39, S1–S266. [Google Scholar]
- Fleming, J.S.; Zivanovic, M.A.; Blake, G.M.; Burniston, M.; Cosgriff, P.S. Guidelines for the measurement of glomerular filtration rate using plasma sampling. Nucl. Med. Commun. 2004, 25, 759–769. [Google Scholar] [CrossRef] [PubMed]
- Blaufox, M.D.; Frohmuller, H.G.; Campbell, J.C.; Utz, D.C.; Orvis, A.L.; Owen, C.A., Jr. A simplified method of estimating renal function with iodohippurate I131. J. Surg. Res. 1963, 3, 122–125. [Google Scholar] [CrossRef]
- Wągrowska-Danilewicz, M.; Danilewicz, M. Spectrum of biopsy-proven renal diseases in patients with type 2 diabetes mellitus. A single center study. Pol. J. Pathol. 2015, 66, 361–367. [Google Scholar] [CrossRef]
- Mizdrak, M.; Kumrić, M.; Kurir, T.T.; Božić, J. Emerging Biomarkers for Early Detection of Chronic Kidney Disease. J. Pers. Med. 2022, 12, 548. [Google Scholar] [CrossRef]
- Garimella, P.S.; Biggs, M.L.; Katz, R.; Ix, J.H.; Bennett, M.R.; Devarajan, P.; Kestenbaum, B.R.; Siscovick, D.S.; Jensen, M.K.; Shlipak, M.G.; et al. Urinary uromodulin, kidney function, and cardiovascular disease in elderly adults. Kidney Int. 2015, 88, 1126–1134. [Google Scholar] [CrossRef]
- Scherberich, J.E.; Gruber, R.; Nockher, W.A.; Christensen, E.I.; Schmitt, H.; Herbst, V.; Block, M.; Kaden, J.; Schlumberger, W. Serum uromodulin-a marker of kidney function and renal parenchymal integrity. Nephrol. Dial. Transplant. 2018, 33, 284–295. [Google Scholar] [CrossRef] [PubMed]
- Risch, M.; Sakem, B.; Risch, L.; Nydegger, U.E. The SENIORLAB study in the quest for healthy elderly patients. J. Lab. Med. 2018, 42, 109–120. [Google Scholar] [CrossRef]
- Chevalier, R.L. Chronic partial ureteral obstruction in the neonatal guinea pig. II. Pressure gradients affecting glomerular filtration rate. Pediatr. Res. 1984, 18, 1271–1277. [Google Scholar] [CrossRef]
- Phanish, M.K.; Chapman, A.N.; Yates, S.; Price, R.; Hendry, B.M.; Roderick, P.J.; Dockrell, M.E.C. Evaluation of Urinary Biomarkers of Proximal Tubular Injury, Inflammation, and Fibrosis in Patients With Albuminuric and Nonalbuminuric Diabetic Kidney Disease. Kidney Int. Rep. 2021, 6, 1355–1367. [Google Scholar] [CrossRef]
- Jotwani, V.K.; Lee, A.K.; Estrella, M.M.; Katz, R.; Garimella, P.S.; Malhotra, R.; Rifkin, D.E.; Ambrosius, W.; Freedman, B.I.; Cheung, A.K.; et al. Urinary Biomarkers of Tubular Damage Are Associated with Mortality but Not Cardiovascular Risk among Systolic Blood Pressure Intervention Trial Participants with Chronic Kidney Disease. Am. J. Nephrol. 2019, 49, 346–355. [Google Scholar] [CrossRef] [PubMed]
- Coca, S.G.; Parikh, C.R. Urinary biomarkers for acute kidney injury: Perspectives on translation. Clin. J. Am. Soc. Nephrol. 2008, 3, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Kostic, D.; Beozzo, G.; do Couto, S.B.; Kato, A.H.T.; Lima, L.; Palmeira, P.; Krebs, V.L.J.; Bunduki, V.; Francisco, R.P.V.; Zugaib, M.; et al. The role of renal biomarkers to predict the need of surgery in congenital urinary tract obstruction in infants. J. Pediatr. Urol. 2019, 15, 242.e241–242.e249. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Zhou, L.; Li, Q.; Li, S.; Luo, X.; Zhang, C.; Wu, B.; Brooks, J.D.; Sun, H. Elevated urinary lipocalin-2, interleukin-6 and monocyte chemoattractant protein-1 levels in children with congenital ureteropelvic junction obstruction. J. Pediatr. Urol. 2019, 15, 44.e41–44.e47. [Google Scholar] [CrossRef] [PubMed]
- Madsen, M.G.; Nørregaard, R.; Palmfeldt, J.; Olsen, L.H.; Frøkiær, J.; Jørgensen, T.M. Epidermal growth factor and monocyte chemotactic peptide-1: Potential biomarkers of urinary tract obstruction in children with hydronephrosis. J. Pediatr. Urol. 2013, 9, 838–845. [Google Scholar] [CrossRef] [PubMed]
- Steubl, D.; Block, M.; Herbst, V.; Nockher, W.A.; Schlumberger, W.; Satanovskij, R.; Angermann, S.; Hasenau, A.L.; Stecher, L.; Heemann, U.; et al. Plasma Uromodulin Correlates With Kidney Function and Identifies Early Stages in Chronic Kidney Disease Patients. Medicine 2016, 95, e3011. [Google Scholar] [CrossRef] [PubMed]
- MacIsaac, R.J.; Jerums, G.; Ekinci, E.I. Effects of glycaemic management on diabetic kidney disease. World J. Diabetes 2017, 8, 172–186. [Google Scholar] [CrossRef]
- Risch, L.; Lhotta, K.; Meier, D.; Medina-Escobar, P.; Nydegger, U.E.; Risch, M. The serum uromodulin level is associated with kidney function. Clin. Chem. Lab. Med. 2014, 52, 1755–1761. [Google Scholar] [CrossRef] [PubMed]
- Pruijm, M.; Ponte, B.; Ackermann, D.; Paccaud, F.; Guessous, I.; Ehret, G.; Pechère-Bertschi, A.; Vogt, B.; Mohaupt, M.G.; Martin, P.Y.; et al. Associations of Urinary Uromodulin with Clinical Characteristics and Markers of Tubular Function in the General Population. Clin. J. Am. Soc. Nephrol. 2016, 11, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Lousa, I.; Reis, F.; Beirão, I.; Alves, R.; Belo, L.; Santos-Silva, A. New Potential Biomarkers for Chronic Kidney Disease Management-A Review of the Literature. Int. J. Mol. Sci. 2020, 22, 43. [Google Scholar] [CrossRef] [PubMed]
- Jotwani, V.; Garimella, P.S.; Katz, R.; Malhotra, R.; Bates, J.; Cheung, A.K.; Chonchol, M.; Drawz, P.E.; Freedman, B.I.; Haley, W.E.; et al. Tubular Biomarkers and Chronic Kidney Disease Progression in SPRINT Participants. Am. J. Nephrol. 2020, 51, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Melchinger, H.; Calderon-Gutierrez, F.; Obeid, W.; Xu, L.; Shaw, M.M.; Luciano, R.L.; Kuperman, M.; Moeckel, G.W.; Kashgarian, M.; Wilson, F.P.; et al. Urine Uromodulin as a Biomarker of Kidney Tubulointerstitial Fibrosis. Clin. J. Am. Soc. Nephrol. 2022, 17, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
| ON Patients N = 57 | Control Subjects N = 25 | p Value | |
|---|---|---|---|
| Number F/M, N | 32/25 | 18/7 | 0.175 |
| Age (years), mean ± SD | 59.6 ± 13.1 | 53.8 ± 11.7 | 0.064 |
| BMI (kg/m2), mean ± SD | 28.7 ± 5.0 | 26.9 ± 7.6 | 0.288 |
| W/H ratio (cm), mean ± SD | 0.95 ± 0.13 | 0.91 ± 0.01 | 0.720 |
| Fasting glucose level (mmol/L), mean ± SD | 5.4 ± 1.2 | 5.0 ± 0.6 | 0.219 |
| Insulin (mlU/L), median (range) | 14.3 (3.0–50.2) | 10.9 (8.0–30.5) | 0.771 |
| Cholesterol (mmol/L), mean ± SD | 5.2 ± 1.2 | 5.5 ± 0.7 | 0.635 |
| HDL (mmol/L), mean ± SD | 1.3 ± 0.4 | 1.3 ± 0.5 | 0.983 |
| LDL (mmol/L), mean ± SD | 3.1 ± 0.8 | 2.7 ± 1.1 | 0.466 |
| Triglycerides (mmol/L), median (range) | 1.6 (0.7–3.6) | 2.5 (0.7–5.2) | 0.440 |
| C-reactive protein (mg/dL), median (range) | 2.4 (0.4–11.0) | 1.9 (0.9–5.8) | 0.646 |
| mGFR (mL/min/1.73 m2), mean ± SD | 57.8 ± 22.1 | 101.4 ± 9.6 | <0.001 |
| ERPF (mL/min/1.73 m2) | 305.8 ± 113.4 | 449.8 ± 59.0 | <0.001 |
| C Cystatin C (mg/L) | 1.3 ± 0.5 | 0.8 ± 0.1 | <0.001 |
| Uromodulin (ng/mL) | 50.2 ± 26.3 | 78.3 ± 24.5 | <0.001 |
| Group I N = 31 | Group II N = 26 | Control Group N = 25 | p Overall | Group I vs. Group II | Group I vs. Control Group | Group II vs. Control Group | |
|---|---|---|---|---|---|---|---|
| Number (F/M), N | 14/17 | 18/8 | 18/7 | 0.071 | 0.007 | 0.044 | 0.828 |
| mGFR (mL/min/1.73 m2), mean ± SD | 39.7 ± 9.9 | 79.5 ± 9.1 | 101.4 ± 9.6 | <0.001 | <0.001 | <0.001 | <0.001 |
| ERPF (mL/min/1.73 m2), mean ± SD | 251.6 ± 60.2 | 393.8 ± 12.6 | 449.8 ± 59.0 | <0.001 | <0.001 | <0.001 | 0.203 |
| S Creatinine (µmol/L), mean ± SD | 132.8 ± 37.9 | 73.9 ± 14.5 | 71.9 ± 14.8 | <0.001 | <0.001 | <0.001 | 0.959 |
| Urea (mmol/L), mean ± SD | 8.6 ± 3.4 | 4.9 ± 1.6 | 1.5 ± 1.2 | <0.001 | <0.001 | <0.001 | 0.828 |
| Uric Acid (µmol/L), mean ± SD | 396.1 ± 100.8 | 345.4 ± 85.5 | 299.2 ± 82.4 | <0.001 | 0.096 | <0.001 | 0.171 |
| Cystatin C (mg/L), mean ± SD | 1.7 ± 0.5 | 1.0 ± 0.2 | 0.8 ± 0.1 | <0.001 | <0.001 | <0.001 | 0.254 |
| Uromodulin (ng/mL), mean ± SD | 30.5 ± 11.1 | 73.6 ± 18.6 | 78.3 ± 24.5 | <0.001 | 0.007 | 0.044 | 0.828 |
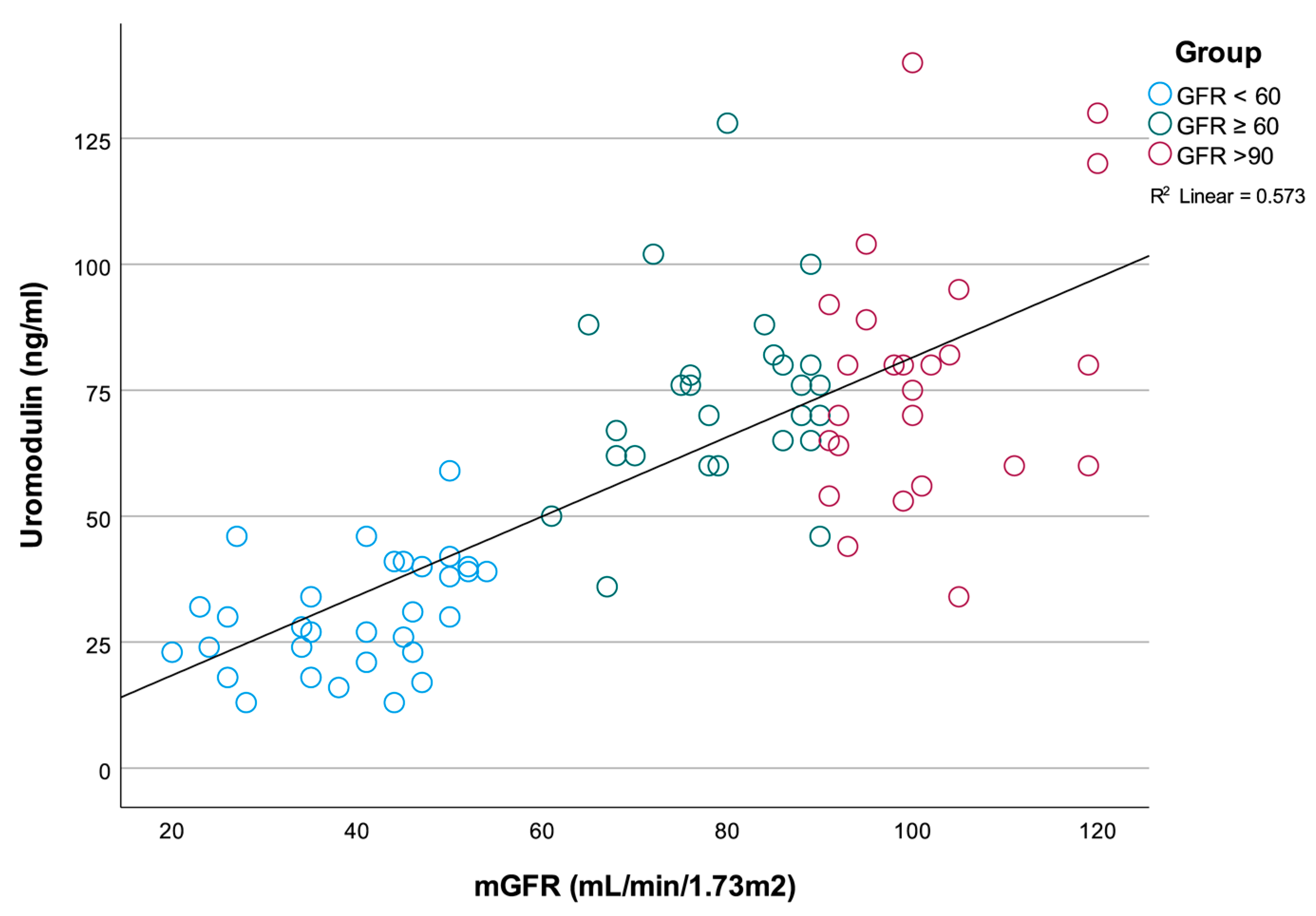
| r | p | |
|---|---|---|
| mGFR (mL/min/1.73 m2) | 0.757 | <0.001 |
| ERPF (mL/min/1.73 m2) | 0.572 | <0.001 |
| Cystatin C (mg/L) | −0.625 | <0.001 |
| Urea (mmol/L) | rho = −0.601 | <0.001 |
| S Creatinine (µmol/L) | rho = −0.644 | <0.001 |
| Uric Acid (µmol/L) | rho = −0.325 | 0.003 |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| B | p | B | p | |
| Age (years) | −0.758 | 0.002 | 0.004 | 0.988 |
| Sex (Female/Male) | 13.705 | 0.036 | 7.907 | 0.148 |
| Cholesterol (total) (mmol/L) | 5.366 | 0.038 | 3.184 | 0.223 |
| HDL (mmol/L) | 4.277 | 0.560 | ||
| LDL (mmol/L) | 2.560 | 0.474 | ||
| Triglycerides (mmol/L) | 9.621 | 0.052 | ||
| ApoA-I (g/L) | 16.983 | 0.062 | ||
| ApoB (g/L) | 30.046 | 0.026 | ||
| CRP (µg/mL) | 3.231 | 0.146 | ||
| Blood glucose level (mmol/L) | −11.671 | 0.001 | −4.909 | 0.027 |
| BMI (kg/m2) | −0.531 | 0.425 | ||
| Waist/Hip ratio | −26.693 | 0.342 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vukmirović Papuga, M.; Bukumirić, Z.; Ilinčić, B.; Mijović, R.; Šašić Ostojić, T.; Žeravica, R. Serum Uromodulin, a Potential Biomarker of Tubulointerstitial Damage, Correlates Well with Measured GFR and ERPF in Patients with Obstructive Nephropathy. Medicina 2022, 58, 1729. https://doi.org/10.3390/medicina58121729
Vukmirović Papuga M, Bukumirić Z, Ilinčić B, Mijović R, Šašić Ostojić T, Žeravica R. Serum Uromodulin, a Potential Biomarker of Tubulointerstitial Damage, Correlates Well with Measured GFR and ERPF in Patients with Obstructive Nephropathy. Medicina. 2022; 58(12):1729. https://doi.org/10.3390/medicina58121729
Chicago/Turabian StyleVukmirović Papuga, Marija, Zoran Bukumirić, Branislava Ilinčić, Romana Mijović, Tanja Šašić Ostojić, and Radmila Žeravica. 2022. "Serum Uromodulin, a Potential Biomarker of Tubulointerstitial Damage, Correlates Well with Measured GFR and ERPF in Patients with Obstructive Nephropathy" Medicina 58, no. 12: 1729. https://doi.org/10.3390/medicina58121729
APA StyleVukmirović Papuga, M., Bukumirić, Z., Ilinčić, B., Mijović, R., Šašić Ostojić, T., & Žeravica, R. (2022). Serum Uromodulin, a Potential Biomarker of Tubulointerstitial Damage, Correlates Well with Measured GFR and ERPF in Patients with Obstructive Nephropathy. Medicina, 58(12), 1729. https://doi.org/10.3390/medicina58121729





