Misfit of Implant-Supported Zirconia (Y-TZP) CAD-CAM Framework Compared to Non-Zirconia Frameworks: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Focused Question
2.2. Eligibility Criteria
2.3. Literature Search
2.4. Data Extraction
2.5. Quality Assessment
3. Results
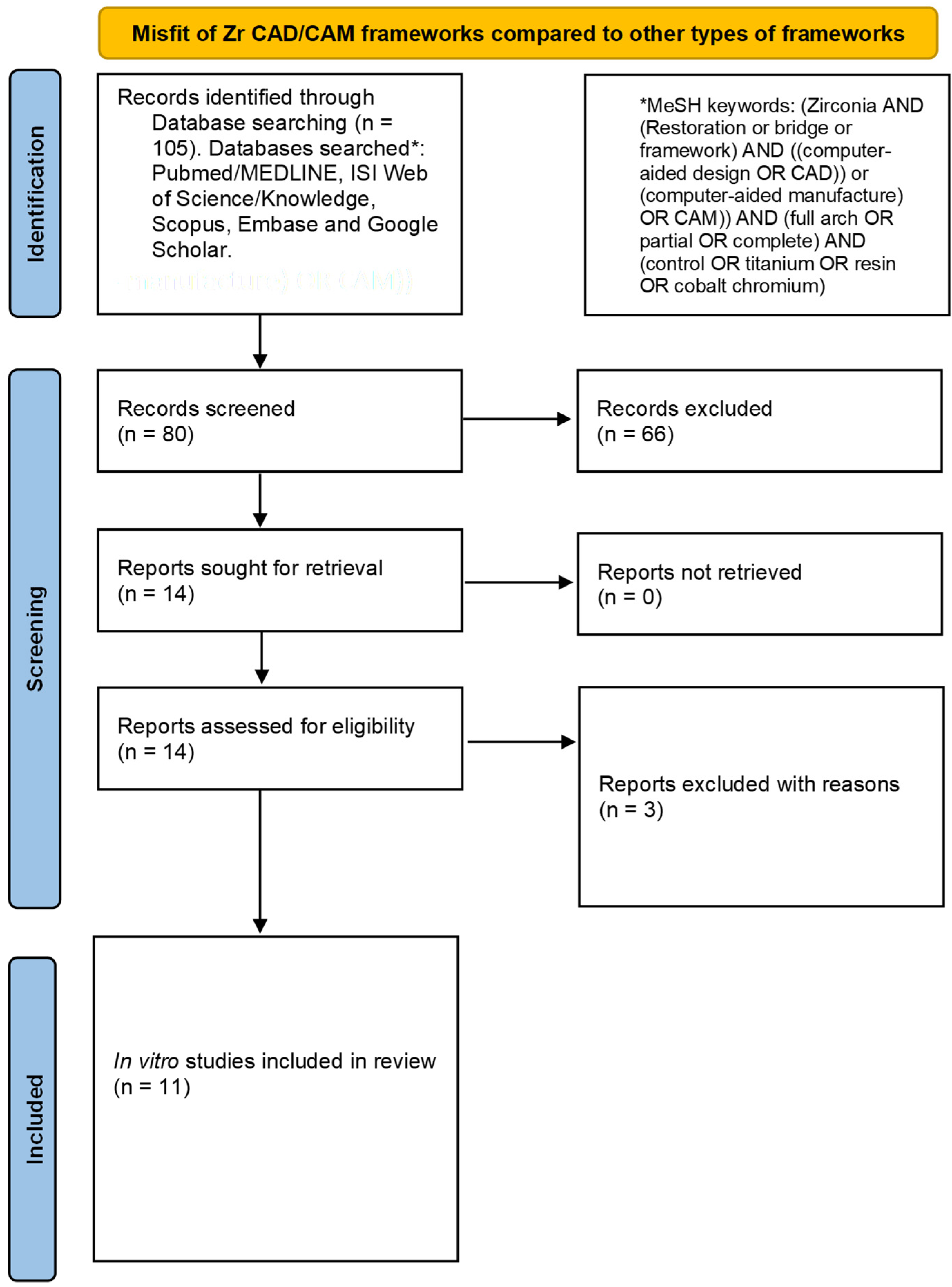
3.1. Results of the Literature Search
3.2. General Characteristics
3.3. Outcomes of Included Studies
3.4. Results of the Quality Assessment
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhang, Y.; Gulati, K.; Li, Z.; Di, P.; Liu, Y. Dental implant nano-engineering: Advances, limitations and future directions. Nanomaterials 2021, 11, 2489. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Rath, B.; Tingart, M.; Eschweiler, J. Role of implants surface modification in osseointegration: A systematic review. J. Biomed. Mat. Res. Part A 2020, 108, 470–484. [Google Scholar] [CrossRef] [PubMed]
- Bagegni, A.; Abou-Ayash, S.; Rücker, G.; Algarny, A.; Att, W. The influence of prosthetic material on implant and prosthetic survival of implant-supported fixed complete dentures: A systematic review and meta-analysis. J. Prosthodont. Res. 2019, 63, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Duong, H.Y.; Roccuzzo, A.; Stähli, A.; Salvi, G.E.; Lang, N.P.; Sculean, A. Oral health-related quality of life of patients rehabilitated with fixed and removable implant-supported dental prostheses. Periodontology 2022, 88, 201–237. [Google Scholar] [CrossRef]
- Varghese, K.G.; Gandhi, N.; Kurian, N.; Daniel, A.Y.; Dhawan, K.; Joseph, M.; Varghese, M.G. Rehabilitation of the severely resorbed maxilla by using quad zygomatic implant-supported prostheses: A systematic review and meta-analysis. J. Prosthet. Dent. 2021; in press. [Google Scholar] [CrossRef]
- Oh, W.-S.; Saglik, B.; Bak, S.-Y. Bone loss in the posterior edentulous mandible with implant-supported overdentures vs complete dentures: A systematic review and meta-analysis. Int. J. Prosthodont. 2020, 33, 184–191. [Google Scholar] [CrossRef]
- Topçu, A.O.; Yamalik, N.; Güncü, G.N.; Tözüm, T.F.; El, H.; Uysal, S.; Hersek, N. Implant-site related and patient-based factors with the potential to impact patients’ satisfaction, quality of life measures and perceptions toward dental implant treatment. Implant Dent. 2017, 26, 581–591. [Google Scholar] [CrossRef]
- Doundoulakis, J.H.; Eckert, S.E.; Lindquist, C.C.; Jeffcoat, M.K. The implant-supported overdenture as an alternative to the complete mandibular denture. J. Am. Dent. Assoc. 2003, 134, 1455–1458. [Google Scholar] [CrossRef]
- Kreissl, M.E.; Gerds, T.; Muche, R.; Heydecke, G.; Strub, J.R. Technical complications of implant-supported fixed partial dentures in partially edentulous cases after an average observation period of 5 years. Clin. Oral Implants Res. 2007, 18, 720–726. [Google Scholar] [CrossRef]
- McLaughlin, J.B.; Ramos, V., Jr.; Dickinson, D.P. Comparison of Fit of Dentures Fabricated by Traditional Techniques Versus CAD-CAM Technology. J. Prosthodont. 2019, 28, 428–435. [Google Scholar] [CrossRef]
- Yun, M.-J.; Jeon, Y.-C.; Jeong, C.-M.; Huh, J.-B. Comparison of the fit of cast gold crowns fabricated from the digital and the conventional impression techniques. J. Adv. Prosthodont. 2017, 9, 1–13. [Google Scholar] [CrossRef]
- Mitha, T.; Owen, C.P.; Howes, D.G. The three-dimensional casting distortion of five implant-supported frameworks. Int. J. Prosthodont. 2009, 22, 248–250. [Google Scholar] [PubMed]
- de Torres, E.M.; Rodrigues, R.C.S.; de Mattos, M.d.G.C.; Ribeiro, R.F. The effect of commercially pure titanium and alternative dental alloys on the marginal fit of one-piece cast implant frameworks. J. Dent. 2007, 35, 800–805. [Google Scholar] [CrossRef] [PubMed]
- Diwan, R.; Talic, Y.; Omar, N.; Sadiq, W. The effect of storage time of removable partial denture wax pattern on the accuracy of fit of the cast framework. J. Prosthet. Dent. 1997, 77, 375–381. [Google Scholar] [CrossRef]
- Tischler, M.; Patch, C.; Bidra, A.S. Rehabilitation of edentulous jaws with zirconia complete-arch fixed implant-supported prostheses: An up to 4-year retrospective clinical study. J. Prosthet. Dent. 2018, 120, 204–209. [Google Scholar] [CrossRef] [PubMed]
- Henriques, G.E.P.; Consani, S.; de Almeida Rollo, J.M.D.; e Silva, F.A. Soldering and remelting influence on fatigue strength of cobalt-chromium alloys. J. Prosthet. Dent. 1997, 78, 146–152. [Google Scholar] [CrossRef]
- Lauritano, D.; Moreo, G.; Lucchese, A.; Viganoni, C.; Limongelli, L.; Carinci, F. The impact of implant–abutment connection on clinical outcomes and microbial colonization: A narrative review. Materials 2020, 13, 1131. [Google Scholar] [CrossRef] [PubMed]
- Yannikakis, S.; Prombonas, A. Improving the fit of implant prosthetics: An in vitro study. Int. J. Oral Maxillofac. Implants 2013, 28, 126–134. [Google Scholar] [CrossRef][Green Version]
- Pan, Y.; Tsoi, J.K.H.; Lam, W.Y.H.; Pow, E.H.N. Implant framework misfit: A systematic review on assessment methods and clinical complications. Clin. Implant Dent. Relat. Res. 2021, 23, 244–258. [Google Scholar] [CrossRef]
- Baba, N.Z.; AlRumaih, H.S.; Goodacre, B.J.; Goodacre, C.J. Current techniques in CAD-CAM denture fabrication. Gen. Dent. 2016, 64, 23–28. [Google Scholar]
- Baba, N.Z.; Goodacre, B.J.; Goodacre, C.J.; Müller, F.; Wagner, S. CAD-CAM complete denture systems and physical properties: A review of the literature. J. Prosthodont. 2021, 30, 113–124. [Google Scholar] [CrossRef]
- Steinmassl, O.; Dumfahrt, H.; Grunert, I.; Steinmassl, P.A. CAD/CAM produces dentures with improved fit. Clin. Oral Investig. 2018, 22, 2829–2835. [Google Scholar] [CrossRef] [PubMed]
- Pereira, A.L.C.; de Medeiros, A.K.B.; de Sousa Santos, K.; de Almeida, É.O.; Barbosa, G.A.S.; Carreiro, A.D.F.P. Accuracy of CAD-CAM systems for removable partial denture framework fabrication: A systematic review. J. Prosthet. Dent. 2021, 125, 241–248. [Google Scholar] [CrossRef] [PubMed]
- Share & Trends Analysis Report By Product (Titanium Implants, Zirconium Implants), By Region (North America, Europe, Asia Pacific, Latin America, MEA), And Segment Forecasts, 2018–2024. Personalized Medicine Market Analysis By Product And Segment Forecasts To 2018. 2022. Available online: https://www.marketresearch.com/Grang-View-Research-v4060/Dental-implant-size-share-trends-14163164/Chapter5 (accessed on 10 July 2022).
- Shetty, R.; Shoukath, S.; Shetty, N.H.G.; Shetty, S.K.; Dandekeri, S.; Ragher, M. A novel design modification to improve flexural strength of zirconia framework: A comparative experimental in vitro study. J. Pharm. Bioallied Sci. 2020, 12 (Suppl. 1), S495–S503. [Google Scholar] [CrossRef] [PubMed]
- Pott, P.C.; Eisenburger, M.; Stiesch, M. Survival rate of modern all-ceramic FPDs during an observation period from 2011 to 2016. J. Adv. Prosthodont. 2018, 10, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Agustín-Panadero, R.; Serra-Pastor, B.; Fons-Font, A.; Solá-Ruíz, M.F. Prospective clinical study of zirconia full-coverage restorations on teeth prepared with biologically oriented preparation technique on gingival health: Results after two-year follow-up. Oper. Dent. 2018, 43, 482–487. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Lyons, K.; Waddell, N.; Bennani, V.; Swain, M. A comparison of fit of CNC-milled titanium and zirconia frameworks to implants. Clin. Implant Dent. Relat. Res. 2012, 14 (Suppl. 1), e20–e29. [Google Scholar] [CrossRef] [PubMed]
- Zaghloul, H.H.; Younis, J.F. Marginal fit of implant-supported all-ceramic zirconia frameworks. J. Oral Implantol. 2013, 39, 417–424. [Google Scholar] [CrossRef]
- de França, D.G.; Morais, M.H.; das Neves, F.D.; Barbosa, G.A. Influence of CAD-CAM on the fit accuracy of implant-supported zirconia and cobalt-chromium fixed dental prostheses. J. Prosthet. Dent. 2015, 113, 22–28. [Google Scholar] [CrossRef]
- Katsoulis, J.; Mericske-Stern, R.; Rotkina, L.; Zbären, C.; Enkling, N.; Blatz, M.B. Precision of fit of implant-supported screw-retained 10-unit computer-aided-designed and computer-aided-manufactured frameworks made from zirconium dioxide and titanium: An in vitro study. Clin. Oral Implants Res. 2014, 25, 165–174. [Google Scholar] [CrossRef]
- de Araújo, G.M.; de França, D.G.; Silva Neto, J.P.; Barbosa, G.A. Passivity of conventional and CAD-CAM fabricated implant frameworks. Braz. Dent. J. 2015, 26, 277–283. [Google Scholar] [CrossRef]
- Ghodsi, S.; Zeighami, S.; Meisami Azad, M. Comparing retention and internal adaptation of different implant-supported, metal-free frameworks. Int. J. Prosthodont. 2018, 31, 475–477. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, B.; Alshahrani, F.A.; Kale, E.; Johnston, W.M. Effect of feldspathic porcelain layering on the marginal fit of zirconia and titanium complete-arch fixed implant-supported frameworks. J. Prosthet. Dent. 2018, 120, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, B.; Kale, E.; Johnston, W.M. Marginal discrepancy of CAD-CAM complete-arch fixed implant-supported frameworks. J. Prosthet. Dent. 2018, 120, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Al-Meraikhi, H.; Yilmaz, B.; McGlumphy, E.; Brantley, W.; Johnston, W.M. In vitro fit of CAD-CAM complete arch screw-retained titanium and zirconia implant prostheses fabricated on 4 implants. J. Prosthet. Dent. 2018, 119, 409–416. [Google Scholar] [CrossRef] [PubMed]
- da Cunha Fontoura, D.; de Magalhães Barros, V.; de Magalhães, C.S.; Vaz, R.R.; Moreira, A.N. Evaluation of Vertical Misfit of CAD-CAM Implant-Supported Titanium and Zirconia Frameworks. Int. J. Oral Maxillofac. Implants 2018, 33, 1027–1032. [Google Scholar] [CrossRef] [PubMed]
- Del Rio Silva, L.; Velôso, D.V.; Barbin, T.; Borges, G.A.; Presotto, A.G.C.; Mesquita, M.F. Can ceramic veneer spark erosion and mechanical cycling affect the accuracy of milled complete-arch frameworks supported by 6 implants? J. Prosthet. Dent. 2020, 126, 772–778. [Google Scholar] [CrossRef] [PubMed]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control. Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Faggion, C.M., Jr. Guidelines for reporting pre-clinical in vitro studies on dental materials. J. Evid. Based Dent. Pract. 2012, 12, 182–189. [Google Scholar] [CrossRef]
- Abduo, J.; Lyons, K.; Swain, M. Fit of zirconia fixed partial denture: A systematic review. J. Oral Rehabil. 2010, 37, 866–876. [Google Scholar] [CrossRef]
- Bousnaki, M.; Chatziparaskeva, M.; Bakopoulou, A.; Pissiotis, A.; Koidis, P. Variables affecting the fit of zirconia fixed partial dentures: A systematic review. J. Prosthet. Dent. 2020, 123, 686–692. [Google Scholar] [CrossRef]
- Svanborg, P.; Norström Saarva, V.; Stenport, V.; Eliasson, A. Fit of 3Y-TZP complete-arch implant-supported fixed dental prostheses before and after porcelain veneering. J. Prosthet. Dent. 2019, 122, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Liedke, G.S.; Spin-Neto, R.; da Silveira, H.E.D.; Wenzel, A. Radiographic diagnosis of dental restoration misfit: A systematic review. J. Oral Rehabil. 2014, 41, 957–967. [Google Scholar] [CrossRef] [PubMed]
- Farina, A.P.; Spazzin, A.O.; Pantoja, J.M.; Consani, R.L.X.; Mesquita, M.F. An in vitro comparison of joint stability of implant-supported fixed prosthetic suprastructures retained with different prosthetic screws and levels of fit under masticatory simulation conditions. Int. J. Oral Maxillofac. Implants 2012, 27, 833–838. [Google Scholar]
- Farina, A.P.; Spazzin, A.O.; Consani, R.L.; Mesquita, M.F. Screw joint stability after the application of retorque in implant-supported dentures under simulated masticatory conditions. J. Prosthet. Dent. 2014, 111, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Denardi, R.J.; da Silva, R.D.; Thomé, G.; Andrighetto, A.R.; de Freitas, R.M.; Shimizu, R.H.; Shimizu, I.A.; Melo, A.C. Bone response after immediate placement of implants in the anterior maxilla: A systematic review. Oral Maxillofac. Surg. 2019, 23, 13–25. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Gao, J.; Luo, L.; Wang, Y. Does Bruxism Contribute to Dental Implant Failure? A Systematic Review and Meta-Analysis. Clin. Implant Dent. Relat. Res. 2016, 18, 410–420. [Google Scholar] [CrossRef]
- Gherlone, E.; Mandelli, F.; Capparè, P.; Pantaleo, G.; Traini, T.; Ferrini, F. A 3 years retrospective study of survival for zirconia-based single crowns fabricated from intraoral digital impressions. J. Dent. 2014, 42, 1151–1155. [Google Scholar] [CrossRef]
- Cappare, P.; Ferrini, F.; Mariani, G.; Nagni, M.; Cattoni, F. Implant rehabilitation of edentulous jaws with predominantly monolithic zirconia compared to metal-acrylic prostheses: A 2-year retrospective clinical study. J. Biol. Regul. Homeost. Agents 2021, 35 (Suppl. 1), 99–112. [Google Scholar]
- Cattoni, F.; Tetè, G.; D’orto, B.; Bergamaschi, A.; Polizzi, E.; Gastaldi, G. Comparison of hygiene levels in metal-ceramic and stratified zirconia in prosthetic rehabilitation on teeth and implants: A retrospective clinical study of a three-year follow-up. J. Biol. Regul. Homeost. Agents 2021, 35 (Suppl. 1), 41–49. [Google Scholar]
- Gungor-Ozkerim, P.S.; Inci, I.; Zhang, Y.S.; Khademhosseini, A.; Dokmeci, M.R. Bioinks for 3D bioprinting: An overview. Biomater. Sci. 2018, 6, 915–946. [Google Scholar] [CrossRef]
| No. | Study | Groups (n = Number of Frameworks Constructed) | Method of Fabrication | Misfit Assessment | Other Assessed Variables | Overall Outcomes | |
|---|---|---|---|---|---|---|---|
| Test | Control | ||||||
| 1 | Abduo et al. 2012 [28] | Y-TZP CAD-CAM (n = 5) | Ti CAD-CAM (n = 5) | Copy milling (subtractive) | Optical microscopy; Vertical passive fit | Strain | Vertical misfits for Y-TZP and Ti CAD-CAM groups were comparable. Passive misfit for Y-TZP CAD-CAM was significantly lower than that of Ti CAD-CAM. No significant difference in strain among both groups. |
| 2 | Zaghloul & Younis et al. 2013 [29] | Y-TZP CAD-CAM (n = 10) Y-TZP Copy Milling (n = 10) | Ni-Cr Cast (n = 10) | CAD-CAM Copy milling (subtractive) | Digital microscopy; Vertical marginal fit | Cyclic fatigue | Y-TZP CAD-CAM had the highest marginal misfit. No significant difference between Y-TZP copy milling and N-Cr cast frameworks. |
| 3 | de França et al. 2014 [30] | Y-TZP CAD-CAM (n = 4) | Co-Cr Cast (n = 8) Co-Cr CAD-CAM (n = 4) | CAD-CAM (milled/subtractive) | SEM; Vertical fit | None | All CAD-CAM frameworks had comparable misfits. CAD-CAM frameworks had significantly lower misfits than cast frameworks. |
| 4 | Katsoulis et al. 2014 [31] | Y-TZP CAD-CAM (n = 5) | Co-Cr Cast (n = 5) Y-TZP-M CAD-CAM (n = 5) Ti CAD/AM (n = 6) | CAD-CAM (subtractive/milling) Co-Cr cast | One-screw test, SEM; Vertical passive fit | None | No significant difference was observed for vertical misfit between Y-TZP and Ti CAD-CAM, but both were significantly better than Co-Cr. |
| 5 | de Araújo et al. 2015 [32] | Group 1: Y-TZP CAD-CAM (n = 4) | Co-Cr cast (n = 4) Group 2: Co-Cr CAD-CAM (n = 4) | CAD-CAM, Cast (milled/subtractive) | SEM; Vertical passive fit | None | Co-Cr CAD-CAM had a significantly lower misfit than the Y-TZP CAD-CAM and Co-Cr Cast specimens. Y-TZP CAD-CAM had a better fit than the cast frameworks. |
| 6 | Ghodsi et al. 2018 [33] | Y-TZP CAD-CAM | PEEK CAD-CAM RC CAD-CAM | CAD-CAM (milled/subtractive) | Replica technique; Internal adaptation | Retention force | Y-TZP CAD-CAM had a significantly lower misfit than PEEK and RC. No difference between PEEK and RC misfits. |
| 7 | Yilmaz et al. 2018 [34] | Y-TZP CAD-CAM Before and after veneering | Ti CAD-CAM Before and after veneering | CAD-CAM (milled/subtractive) | 3D fit (virtual assessment) | None | Y-TZP and Ti CAD-CAM frameworks before and after veneering were comparable. Significant effect of porcelain veneering on Y-TZP frameworks. |
| 8 | Yilmaz et al. 2018 [35] | Y-TZP CAD-CAM | HDP CAD-CAM Ti CAD-CAM | CAD-CAM (milled/subtractive) | Marginal misfit; One-screw test | None | HDP had a significantly lower misfit than the Y-TZP and Ti CAD-CAM specimens. No difference between Y-TZP and Ti misfits. |
| 9 | Al-Meraikhi et al. 2018 [36] | Y-TZP CAD-CAM (n = 5) | Ti CAD-CAM (n = 5) | CAD-CAM (milled/subtractive) | Marginal misfit; One-screw test; CT scanning; Color mapping | None | No significant difference between the fits of the Y-TZP and Ti frameworks was observed. |
| 10 | da Cunha Fontoura et al. 2018 [37] | Y-TZP CAD-CAM (n = 5) | Ti CAD-CAM (n = 5) | CAD-CAM (milled/subtractrive) | Vertical misfit; SEM | Torque | No significant difference between the misfits of the Y-TZP and Ti frameworks. |
| 11 | Del Rio Silva et al. 2020 [38] | Y-TZP Copy-Milling (n = 5) | Ti CAD-CAM (n = 5) Co-Cr Cast (n = 5) | Co-Cr cast (milled/subtractive) | Marginal fit; One screw test | Stress, loosening torque | Ti had a lower misfit than Y-TZP. Ti and Y-TZP both had lower misfits than Co-Cr. Veneering improved the fit in all groups. |
| No. | Author | Implant/Abutment System | Implant Dimensions/Location | Implant-Supported Restoration | Fabrication System | Misfit (µm) |
|---|---|---|---|---|---|---|
| 1 | Abduo et al. 2012 [28] | Mk III TiUnite; Nobel Biocare AB; External hex. | Length: 11.5 mm; diameter: 4.0 mm. First Premolar and second molar on each side | All-on-four full arch fixed denture | Forte, Nobel Biocare, AB (CAD); Fabrication by CAD manufacturer. | Vertical misfit: Y-TZP CAD-CAM: 3.7 µm Ti CAD-CAM: 3.6 µm Passive misfit: Y-TZP CAD-CAM: 5.5 µm Ti: 13.6 µm |
| 2 | Zaghloul & Younis et al. 2013 [29] | Friatiz, Dentsply | Length: 11 mm,; diameter: 4–5 mm Second premolar and second molar | Three-unit FPD | Cerec 3 CAD-CAM (Y-TZP); Y-TZP Copy Milling; Ni-Cr Conventional casting | Y-TZP CAD-CAM: 84.58 ± 3.767 µm Y-TZP copy milling: 50.33 ± 3.415 µm Ni-Cr cast: 42.27 ± 3.766 µm |
| 3 | de França et al. 2014 [30] | Tapered RP; Nobel Biocare; Internal hex | Titamax Cortical Ti; Neodent Diameter: 4.1 mm; length: 9 mm. Second premolar and second molar | Three-unit FPD | Not specified | Y-TZP CAD-CAM: 5.9 ± 3.6 µm Co-Cr CAD-CAM: 1.2 ± 2.2 µm Co-Cr Cast: Castable abutment: 12.9 ± 11.0 µm Machined abutment: 11.8 ± 9.8 µm |
| 4 | Katsoulis et al. 2014 [31] | Replace SelectTM Tapered RP; Nobel Biocare | Diameter: 4.3 mm. RMSPM, RMC, RMCI, LMCI, LMC, LMSPM | Ten-unit fixed denture on six implants | CAD: Nobel Biocare (Nobel ProceraTM); Nobel Biocare CAM: Nobel Procera Production Facility; Nobel Biocare | Y-TZP-L: Median 14 µm 95% CI: 10–26 µm Y-TZP-M: Median 18 µm 95% CI: 12–27 µm Ti-L: Median 15 µm 95% CI: 6–18 µm Co-Cr Cast: Median 236 µm 95% CI: 181–301 µm |
| 5 | de Araújo et al. 2015 [32] | Titamax Cortical Ti; Neodent | Diameter: 3.75 mm; length: 9 mm. Three individual implants (second premolar, first molar, second molar) | Three-unit FPD | Not specified | Y-TZP CAD-CAM: 103.81 ± 43.15 µm Co-Cr CAD-CAM: 48.76 ± 13:45 µm Co-Cr Cast: 187.55 ± 103.63 µm |
| 6 | Ghodsi et al. 2018 [33] | Not specified | Not described | 12 implants (denture details not stated) | CAD: 3Shape; CAM: 3Shape D810 CAD | Y-TZP CAD-CAM: 74.80 µm PEEK CAD-CAM: 181.39 µm RC: 174.89 µm |
| 7 | Yilmaz et al. 2018 [34] | Nobel Biocare Active RP | Length: 13 mm; diameter: 4.3 mm. Two straight in the anterior and two distally tilted internal-hexagon dental implants; canine and molar regions | All-on-four fixed denture | CAD: S600 ARTI; Zirkonzahn CAM: M1 Wet Heavy Metal Milling Unit | Before veneering: Y-TZP CAD-CAM: 89 µm T CAD-CAM µm: 88 After veneering: Y-TZP: 175 Ti: 175 |
| 8 | Yilmaz et al. 2018 [35] | Nobel Biocare Active RP | Length: 13 mm; diameter: 4.3 mm Perpendicular in RMC and LMC; 30-degree distally inclined in RMFM | All-on-four fixed denture | CAD: Zirkonzahn Software; Zirkonzahn CAM: M1 Wet Heavy Metal Milling Unit | RMC HDP: 60 µm Y-TZP CAD-CAM: 83 µm Ti CAD-CAM: 74 µm LMC Not detectable RMFM HDP: 55 µm Y-TZP CAD-CAM: 74 µm Ti CAD-CAM: 102 µm |
| 9 | Al-Meraikhi et al. 2018 [36] | Nobel Bioactive | Implants: 4.3 mm × 13 mm Internal Hex | All-on-four fixed denture. Two implants at canine and two implants at first molar positions | CAD: S600 ARTI Zirkonzahn CAM Milling Unit M1 Heavy; Zirkonzahn | LMC-Ti: 8.2 ± 2.6 µm RMC-Ti: 74 ± 15 µm RMC-Y-TZP: 84.4 ± 12.1 µm RMFM-Ti: 102 ±26.7 µm RMFM-Y-TZP: 93.8 ± 30 µm |
| 10 | da Cunha Fontoura et al. 2018 [37] | ITI Straumann | Diameter 4.1; length: Not available. Location: mandibular-2 at central incisors and 2 at canines | All-on-four. First premolar to first premolar | CAD: Zirkozahn Modellier; Zirkozahn CAM: Milling Unit M5 Heavy; Zirkonzahn | Ti CAD-CAM: 6.011 ± 0.750 µm Y-TZP CAD-CAM: 9.055 ± 3.692 µm |
| 11 | Del Rio Silva et al. 2020 [38] | Easy Grip Porous EH | Implants: 4.1 mm × 11.5 mm (premolar region), 4.1 mm × 11.5 mm (incisor region), 5 mm × 7 mm (molar region) | Fixed complete denture supported by six implants | Ceramill Map 400+; Amann Girrbach/Ceramill Motion 2; Amann Girrbach (Y-TZP) and CNC D15W; Yenadent (Co-Cr & Ti) | Mean values not provided. Ti CAD-CAM had the highest fit before veneering. No difference in fit after veneering. |
| Assessment Item | Abduo et al. 2012 [28] | Zaghloul & Younis et al. 2013 [29] | de França et al. 2014 [30] | Katsoulis et al. 2014 [32] | de Araújo et al. 2015 [32] | Ghodsi et al. 2018 [33] | Yilmaz et al. 2018 [34] | Yilmaz et al. 2018b [35] | Al-Meraikhi et al. 2018 [36] | Diego et al. 2018 [37] | Silva et al. 2020 [38] |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Adequate abstract | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (2a) Introduction (Background) | Yes | Yes | Yes | Yes | Yes | Not clear | Yes | Yes | Yes | Yes | Yes |
| (2b) Introduction (Objectives) | Yes | Yes | Yes | Yes | Yes | Not clear | Yes | Yes | Yes | Yes | Yes |
| Methods | |||||||||||
| 3. Replicable methods | Yes | Yes | Yes | Yes | Yes | Not clear | Yes | Yes | Yes | Yes | Yes |
| 4. Adequate outcomes | Yes | Yes | Yes | Yes | Yes | Not clear | Yes | Yes | Yes | Yes | Yes |
| 5. Pre-determined sample size | No | No | No | Yes | Yes | No | No | No | No | Yes | Yes |
| 6. Allocation of samples | |||||||||||
| (a) Randomization | No | No | No | No | No | Yes | No | No | No | No | No |
| (b) Allocation concealment | No | No | No | No | No | No | No | No | No | No | No |
| (c) Implementation | No | No | No | No | No | No | No | No | No | No | No |
| 7. Blinding | No | No | No | Yes | No | No | No | No | No | No | No |
| 8. Statistics | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 9. Adequate outcomes & estimation | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 10. Discussion: Limitations | Yes | Not clear | Yes | Not clear | Yes | No | Yes | Yes | Yes | No | Yes |
| 11. Funding | Yes | No | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| 12. Accessible protocol | No | No | No | No | No | No | No | No | No | No | No |
| Overall quality | Medium | Medium | Medium | High | Medium | Low | Medium | Medium | Medium | Medium | High |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsayed, H.D. Misfit of Implant-Supported Zirconia (Y-TZP) CAD-CAM Framework Compared to Non-Zirconia Frameworks: A Systematic Review. Medicina 2022, 58, 1347. https://doi.org/10.3390/medicina58101347
Alsayed HD. Misfit of Implant-Supported Zirconia (Y-TZP) CAD-CAM Framework Compared to Non-Zirconia Frameworks: A Systematic Review. Medicina. 2022; 58(10):1347. https://doi.org/10.3390/medicina58101347
Chicago/Turabian StyleAlsayed, Hussain D. 2022. "Misfit of Implant-Supported Zirconia (Y-TZP) CAD-CAM Framework Compared to Non-Zirconia Frameworks: A Systematic Review" Medicina 58, no. 10: 1347. https://doi.org/10.3390/medicina58101347
APA StyleAlsayed, H. D. (2022). Misfit of Implant-Supported Zirconia (Y-TZP) CAD-CAM Framework Compared to Non-Zirconia Frameworks: A Systematic Review. Medicina, 58(10), 1347. https://doi.org/10.3390/medicina58101347







