Surgical and Anatomic Consideration in Endoscopic Dacryocystorhinostomy of a Patient with Damaged Sinonasal Anatomy Post–Caldwell-Luc Surgery: A Case Report
Abstract
:1. Introduction
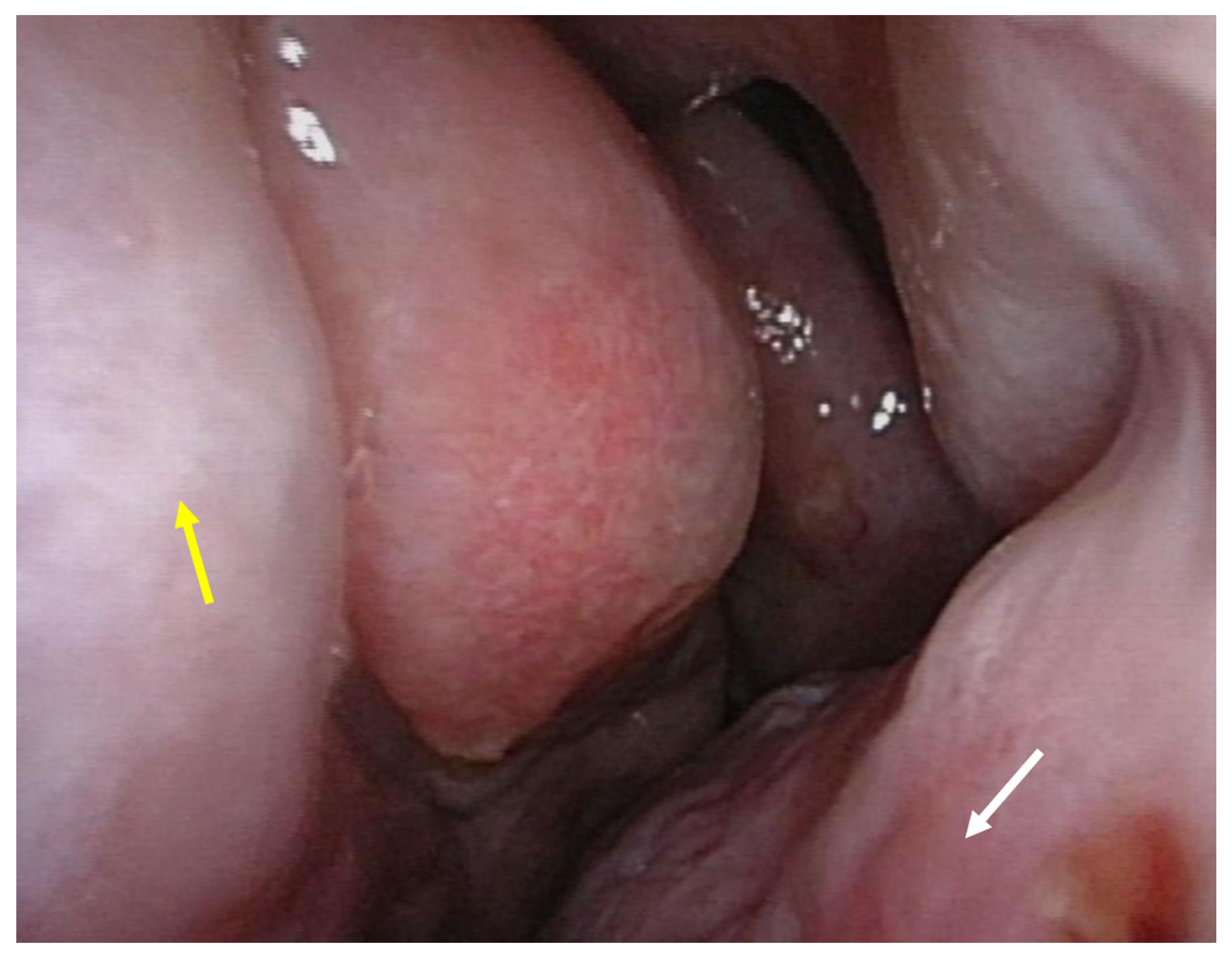
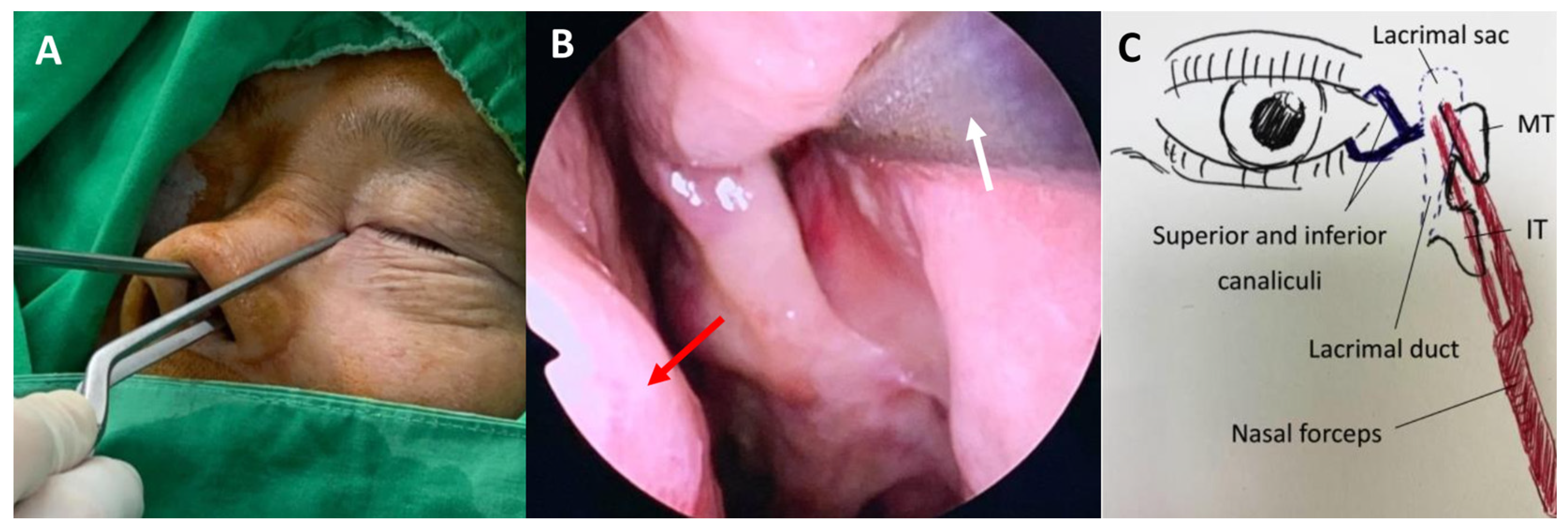
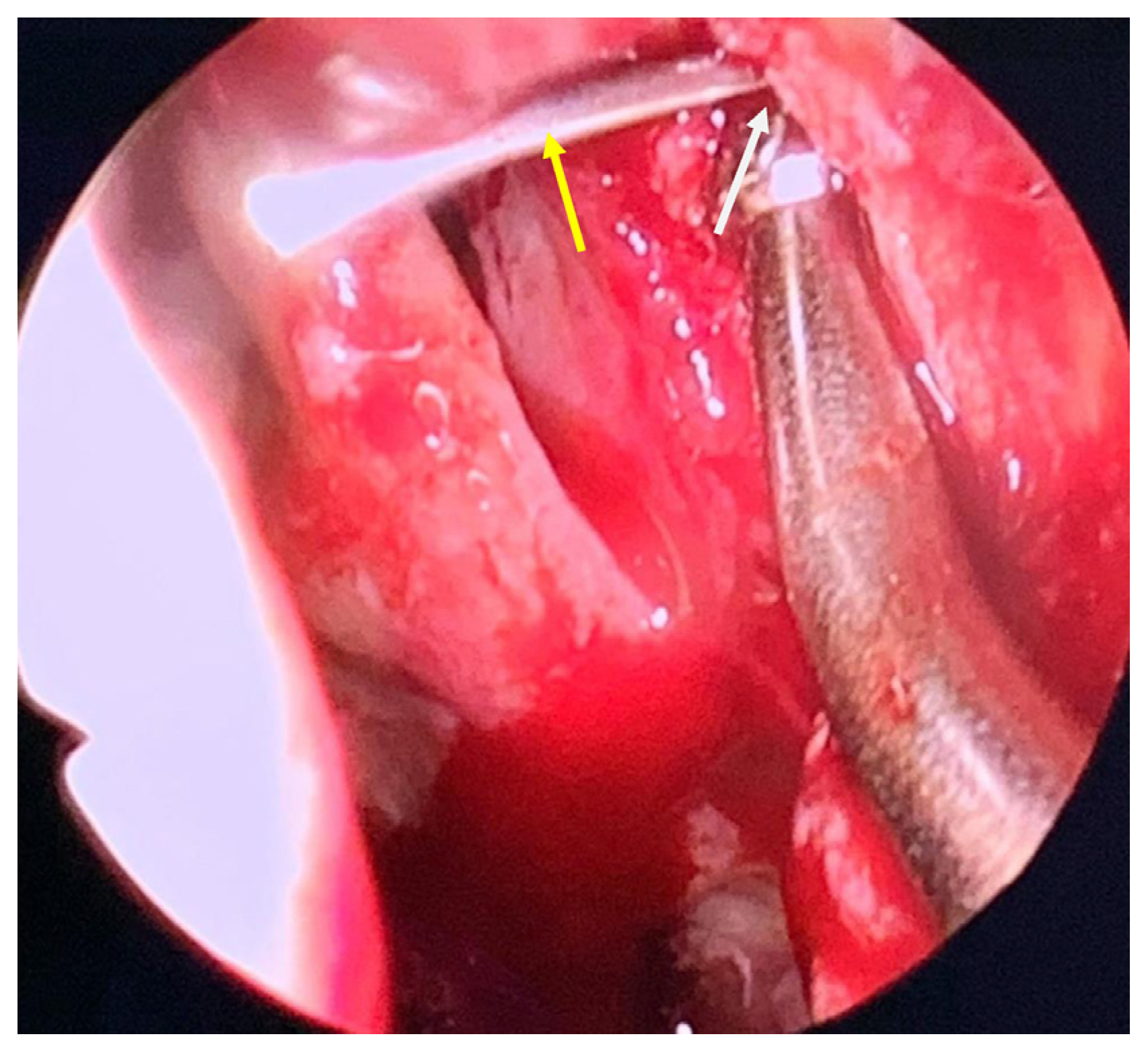
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jawaheer, L.; MacEwen, C.J.; Anijeet, D. Endonasal versus external dacryocystorhinostomy for nasolacrimal duct obstruction. Cochrane Database Syst. Rev. 2017, 2, Cd007097. [Google Scholar] [CrossRef] [Green Version]
- Marcet, M.M.; Kuk, A.K.; Phelps, P.O. Evidence-based review of surgical practices in endoscopic endonasal dacryocystorhinostomy for primary acquired nasolacrimal duct obstruction and other new indications. Curr. Opin. Ophthalmol. 2014, 25, 443–448. [Google Scholar] [CrossRef] [PubMed]
- McDonogh, M.; Meiring, J.H. Endoscopic transnasal dacryocystorhinostomy. J. Laryngol. Otol. 1989, 103, 585–587. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartikainen, J.; Grenman, R.; Puukka, P.; Seppä, H. Prospective randomized comparison of external dacryocystorhinostomy and endonasal laser dacryocystorhinostomy. Ophthalmology 1998, 105, 1106–1113. [Google Scholar] [CrossRef]
- Yakopson, V.S.; Flanagan, J.C.; Ahn, D.; Luo, B.P. Dacryocystorhinostomy: History, evolution and future directions. Saudi J. Ophthalmol. Off. J. Saudi Ophthalmol. Soc. 2011, 25, 37–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajak, S.N.; Psaltis, A.J. Anatomical considerations in endoscopic lacrimal surgery. Ann. Anat. Anat. Anz. 2019, 224, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Macbeth, R. Caldwell, Luc, and their operation. Laryngoscope 1971, 81, 1652–1657. [Google Scholar] [CrossRef]
- Luc, H. Une nouvelle Methode operatoire pour la cure radicale et rapide de l’Empyeme chronique du Sinus maxillaire. Arch. Intern. Laryngol. 1897, 10, 273–285. [Google Scholar]
- Joe Jacob, K.; George, S.; Preethi, S.; Arunraj, V.S. A comparative study between endoscopic middle meatal antrostomy and caldwell-luc surgery in the treatment of chronic maxillary sinusitis. Indian J. Otolaryngol. Head Neck Surg. 2011, 63, 214–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Penttilä, M.A.; Rautiainen, M.E.P.; Laranne, J.E.; Pukander, J.S.; Karma, P.H. Endoscopic and Caldwell-Luc Approach in Chronic Maxillary Sinusitis: Intraoperative and Early Postoperative Results. Am. J. Rhinol. 1993, 7, 5–9. [Google Scholar] [CrossRef]
- Nemec, S.F.; Peloschek, P.; Koelblinger, C.; Mehrain, S.; Krestan, C.R.; Czerny, C. Sinonasal imaging after Caldwell-Luc surgery: MDCT findings of an abandoned procedure in times of functional endoscopic sinus surgery. Eur. J. Radiol. 2009, 70, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Im, J.H.; Kim, S.S.; Kim, J.A.; Moon, U.H. CT Findings of Change of the Maxillary Sinus after Caldwell-Luc Operation. J. Korean Radiol. Soc. 2000, 42, 431. [Google Scholar] [CrossRef]
- Murray, J.P. Complications after treatment of chronic maxillary sinus disease with Caldwell-Luc procedure. Laryngoscope 1983, 93, 282–284. [Google Scholar] [CrossRef] [PubMed]
- Iwanaga, J.; Wilson, C.; Lachkar, S.; Tomaszewski, K.A.; Walocha, J.A.; Tubbs, R.S. Clinical anatomy of the maxillary sinus: Application to sinus floor augmentation. Anat. Cell Biol. 2019, 52, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Low, W.K. Complications of the Caldwell-Luc operation and how to avoid them. Aust. N. Z. J. Surg. 1995, 65, 582–584. [Google Scholar] [CrossRef] [PubMed]
- Aukštakalnis, R.; Simonavičiūtė, R.; Simuntis, R. Treatment options for odontogenic maxillary sinusitis: A review. Stomatologija 2018, 20, 22–26. [Google Scholar] [PubMed]
- Flowers, R.S.; Anderson, R. Injury to the lacrimal apparatus during rhinoplasty. Plast. Reconstr. Surg. 1968, 42, 577–581. [Google Scholar] [CrossRef] [PubMed]
- Meyers, A.D.; Hawes, M.J. Nasolacrimal obstruction after inferior meatus nasal antrostomy. Arch. Otolaryngol. Head Neck Surg. 1991, 117, 208–211. [Google Scholar] [CrossRef]
- Osguthorpe, J.D.; Calcaterra, T.C. Nasolacrimal obstruction after maxillary sinus and rhinoplastic surgery. Arch. Otolaryngol. 1979, 105, 264–266. [Google Scholar] [CrossRef] [PubMed]
- Cies, W.A.; Baylis, H.I. Epiphora following rhinoplasty and Caldwell-Luc procedures. Ophthalmic Surg. 1976, 7, 77–81. [Google Scholar] [CrossRef]
- Herzallah, I.R.; Marglani, O.A.; Muathen, S.H.; Obaid, A.A. Endoscopic and Radiologic Findings in Failed Dacryocystorhinostomy: Teaching Pearls for Success. Am. J. Rhinol. Allergy. 2019, 33, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Sung, J.Y.; Lee, Y.H.; Kim, K.N.; Kang, T.S.; Lee, S.B. Surgical outcomes of endoscopic dacryocystorhinostomy: Analysis of age effect. Sci. Rep. 2019, 9, 19861. [Google Scholar] [CrossRef] [PubMed]
- Strong, E.B. Endoscopic dacryocystorhinostomy. Craniomaxillofac. Trauma Reconstr. 2013, 6, 67–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, C.-C.; Lee, L.-C.; Kuo, B.-I.; Lee, C.-J.; Liu, F.-Y. Surgical and Anatomic Consideration in Endoscopic Dacryocystorhinostomy of a Patient with Damaged Sinonasal Anatomy Post–Caldwell-Luc Surgery: A Case Report. Medicina 2022, 58, 78. https://doi.org/10.3390/medicina58010078
Hsu C-C, Lee L-C, Kuo B-I, Lee C-J, Liu F-Y. Surgical and Anatomic Consideration in Endoscopic Dacryocystorhinostomy of a Patient with Damaged Sinonasal Anatomy Post–Caldwell-Luc Surgery: A Case Report. Medicina. 2022; 58(1):78. https://doi.org/10.3390/medicina58010078
Chicago/Turabian StyleHsu, Chia-Chen, Lung-Chi Lee, Bo-I Kuo, Che-Jui Lee, and Fang-Yu Liu. 2022. "Surgical and Anatomic Consideration in Endoscopic Dacryocystorhinostomy of a Patient with Damaged Sinonasal Anatomy Post–Caldwell-Luc Surgery: A Case Report" Medicina 58, no. 1: 78. https://doi.org/10.3390/medicina58010078
APA StyleHsu, C.-C., Lee, L.-C., Kuo, B.-I., Lee, C.-J., & Liu, F.-Y. (2022). Surgical and Anatomic Consideration in Endoscopic Dacryocystorhinostomy of a Patient with Damaged Sinonasal Anatomy Post–Caldwell-Luc Surgery: A Case Report. Medicina, 58(1), 78. https://doi.org/10.3390/medicina58010078





