2. Case Report
A 37-year-old man with a height of 1.64 m and weight of 70 kg had experienced intermittent spiking fever and chills for 2 months before this admission. He had no history of previous systemic disease and had lived overseas for 1 year before the first admission. He had no history of animal contact, unexplained wounds, or drug abuse and had no irritative symptoms of the airways, intestine, or brain. Polyarthritis had developed in all proximal interphalangeal joints of both hands and was accompanied by spiking fever and myalgia in both arms, chest wall, and back. Within 2 weeks after the onset of polyarthritis, these symptoms extended to the phalanxes of both feet, ankles, and knee joints. (
Table 1).
His first admission was to the division of infectious diseases. The 2019 novel coronavirus disease (COVID-19) had been excluded after repeated blood sampling and plain X-ray films of the chest. Blood tests showed a white blood cell count of 12,850 cells/mm
3, hemoglobin level of 13.3 g/dL, platelet count of 490,000 cells/mm
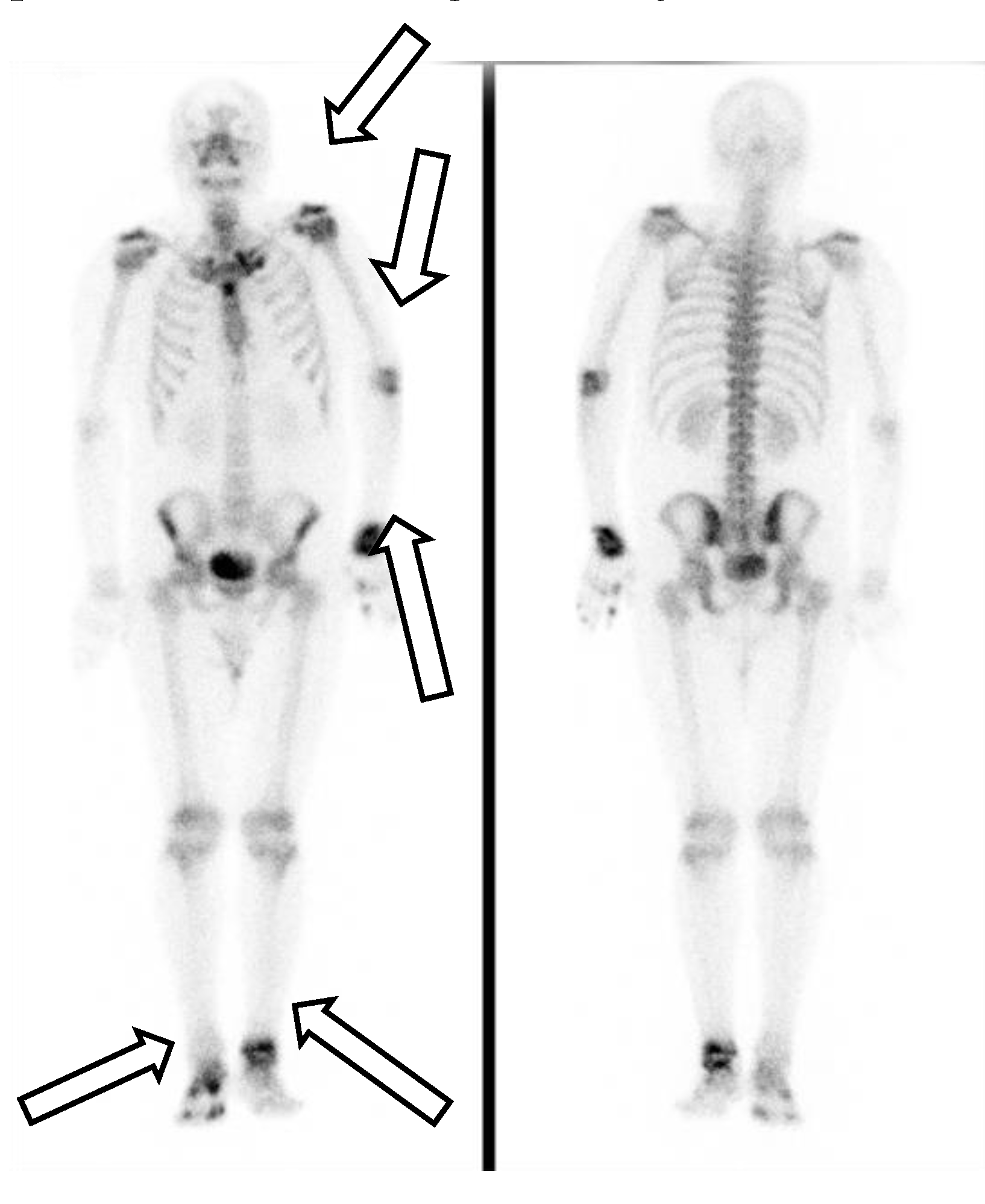
3, plasma creatinine level of 1.0 mg/dL, alanine aminotransferase (ALT) level of 79 U/L, aspartate aminotransferase (AST) level of 38 U/L, and c-reactive protein (CRP) level of 15.00 mg/L. Serum tests did not identify viral hepatitis infection. Microbiology examination of the sputum, blood, urine, and feces did not identify any pathogens. Blood sampling did not detect any autoantibodies. Physical examination did not reveal abnormal murmurs of the heart or abnormal primitive neurologic reflexes. Plain X-ray films of the chest did not show mass lesions or abnormalities in the lungs. X-ray of the major joints of all limbs did not show fracture, erosion of bones, or abnormalities of soft tissue. A technetium-99m methylene diphosphonate bone scan revealed increased uptake in the left shoulder, elbow, wrist, and ankle, and right foot and toes, which was compatible with the clinically significant arthritis noted in the physical examination (
Figure 1). The patient’s fever did not respond to antibiotics for 2 weeks from the first admission. Reactive arthritis was suspected initially because no significant pathogens or autoantibodies had been identified, and sterile inflammation was suspected. The fever responded to daily systemic methylprednisolone (40 mg), and the patient was discharged 17 days after the first admission.
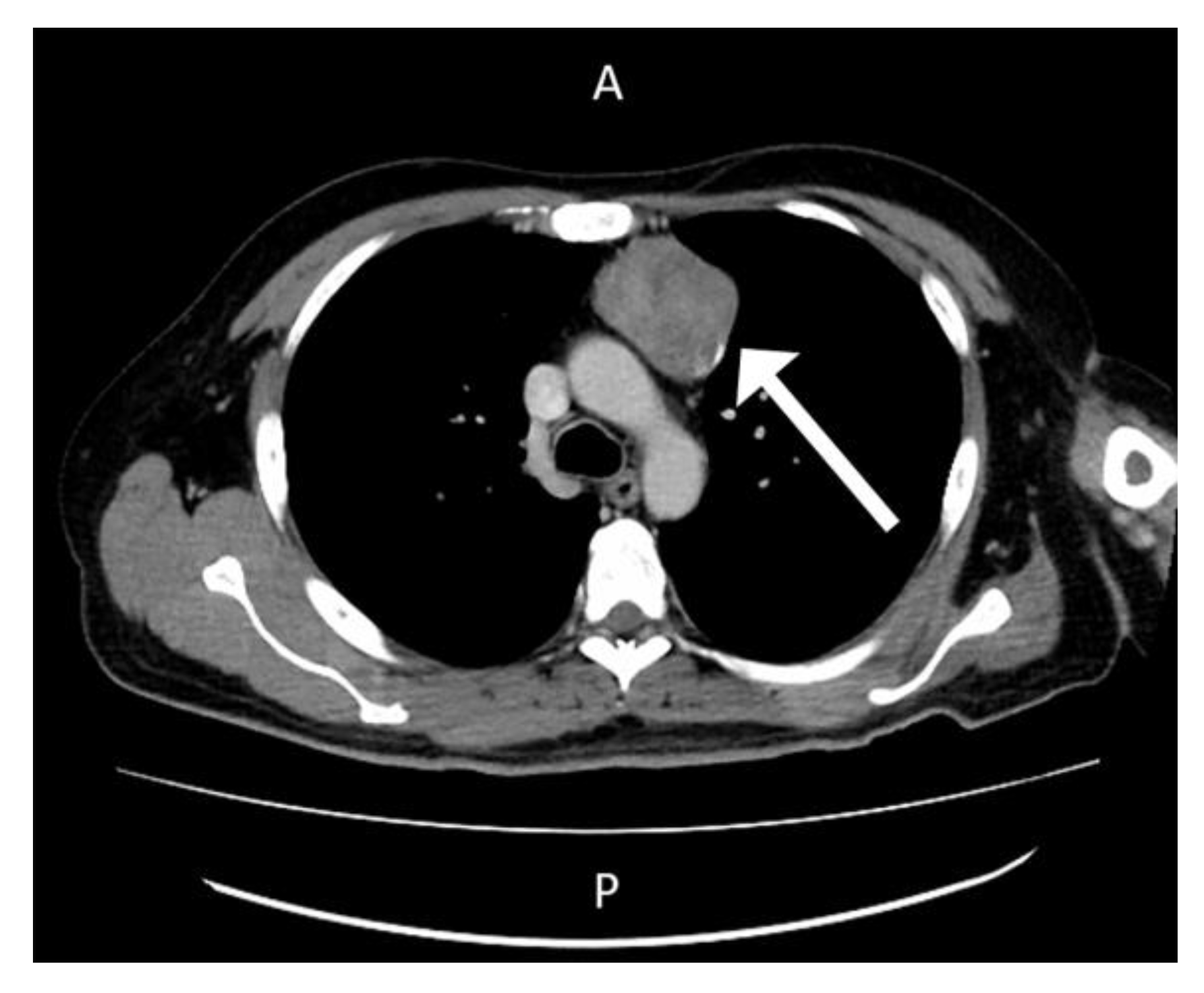
However, polyarthritis in both wrists, metacarpophalangeal joints, knee joints, and ankles developed one week after the patient’s first discharge from the hospital. Physical examinations on the second admission revealed an alert consciousness without abnormal neurologic reflexes. A gallium-67 tumor scan indicated inflammation in the left shoulder, left sternoclavicular junction, left interscapular region, lateral right hip region, left buttock, right knee, and left ankle, but no evidence of malignancy (
Figure 2).
The patient was admitted to the division of rheumatology for suspected partially treated reactive arthritis. Blood tests revealed a white blood cell count of 11,330 cells/mm
3, hemoglobin level of 9.0 g/dL, platelet count of 639,000 cells/mm
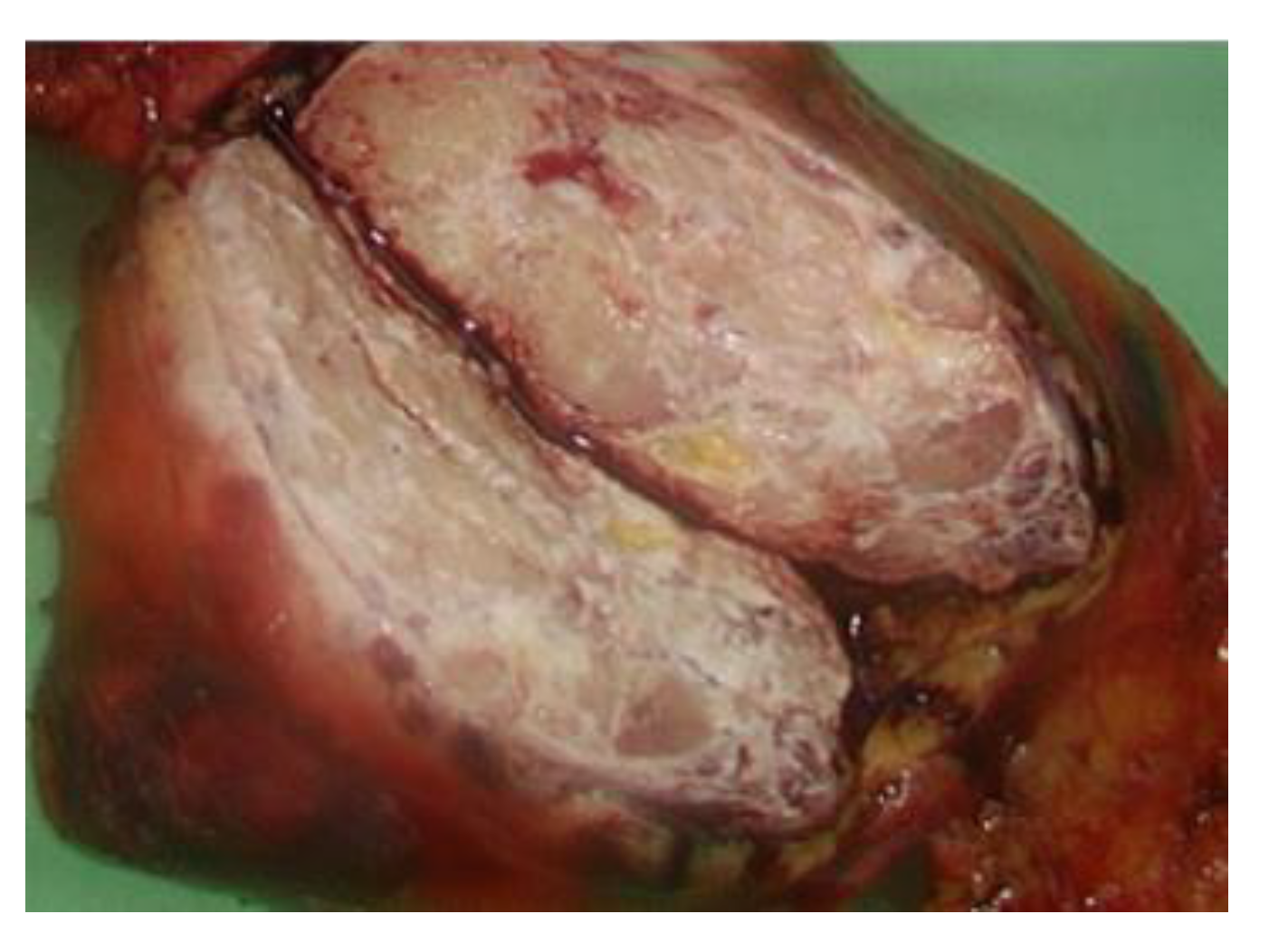
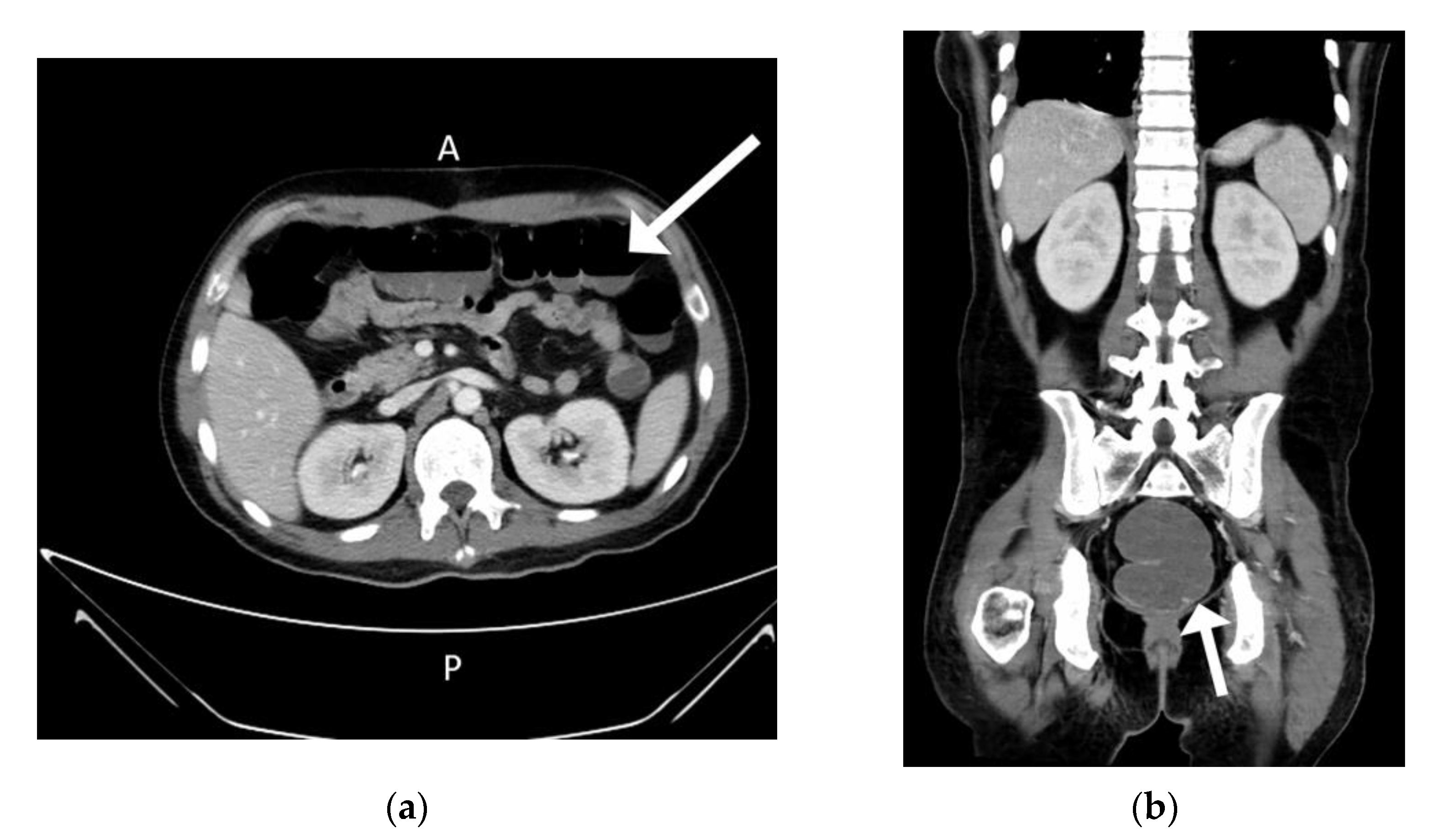
3, creatinine level of 0.6 mg/dL, ALT level of 20 U/L, AST level of 124 U/L, CRP level of 24.27 mg/L, ferritin level of 3408 ng/mL and erythrocyte sedimentation rate of 117/h. Again, microbial examinations of sputum, blood, urine, and feces did not identify any pathogens. Blood sampling did not detect any autoantibodies. Cardiac echo–Doppler revealed no vegetation at the cardiac valves. Sonography of whole abdomen revealed coarsening echo-pattern which was suspected to be fatty liver disease related. Based on the examination protocol for fever with unknown origin [
6], computed tomography scans with contrast of the chest showed a mass lesion in the anterior mediastinum and enlarged lymph nodes (
Figure 3).
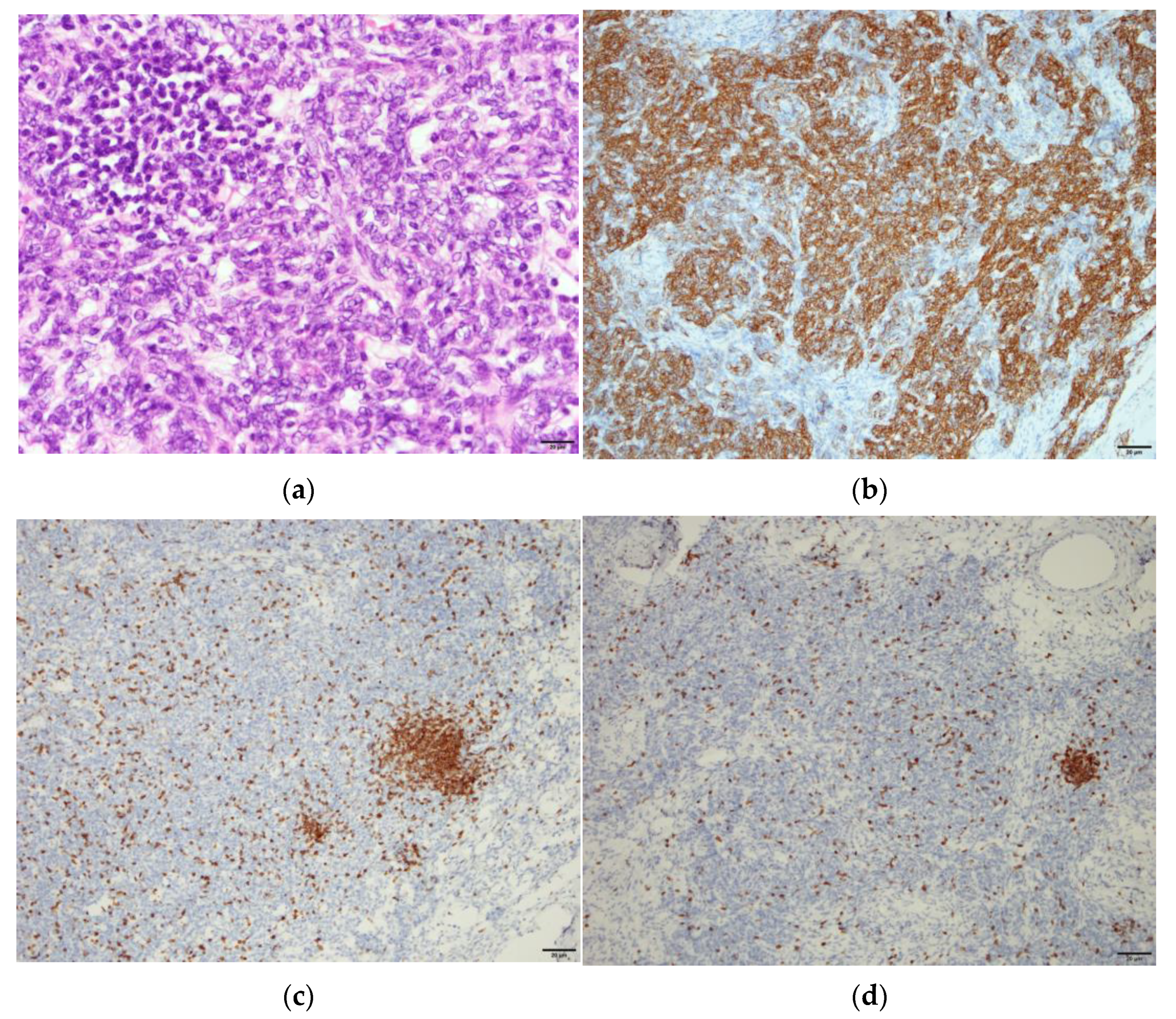
The serum carcinoembryonic antigen concentration was 0.92 ng/mL (normal range: 0.00–5.00 ng/mL), squamous cell carcinoma antigen level was 1.40 ng/mL (normal range: 0.00–2.10 ng/mL), alpha-fetoprotein level was 0.83 ng/mL (normal range for males: 0.00–10.00 ng/mL), carbohydrate antigen 19-9 level was 4.22 U/mL (normal range: 0.00–37.00 U/mL), and beta 2-microglobulin level was 2.72 mg/L (normal range: 1.00–2.40 mg/L). Video-assisted thoracoscopic surgery (VATs) tumor resection identified a mass measuring 7.2 cm × 5.6 cm × 4 cm in the anterior mediastinum (
Figure 4) and two adjacent lymph nodes.
Pathology analysis of the tumor revealed spindle-shaped epithelial cells mixed with small lymphocytes of thymic origin in the absence of malignant cells, and excisional lymph nodes were free of tumor metastasis. Benign thymoma, World Health Organization Type A, was diagnosed (
Figure 5).
The patient’s spiking fever and polyarthritis subsided after the VATs tumor resection. The methylprednisolone dosage was tapered gradually from 40 mg/day to avoid adrenal insufficiency. However, the high fever returned 5 days after the operation and did not respond to antibiotics. Cytomegalovirus (CMV) viremia developed with a serum viral load of 5418 copies/mL, and ganciclovir was prescribed. Ileus and intermittent hematochezia developed gradually 8 days after the VATs (
Figure 6).
CMV colitis was diagnosed based on a positive polymerase chain reaction test for CMV in the feces. A rapid test to detect Clostridium difficile revealed the presence of glutamate dehydrogenase antigen, and vancomycin and metronidazole were prescribed for the C. difficile infection. The patient developed fluctuating disturbed consciousness followed by intermittent seizure, and hematochezia developed 17 days after the tumor resection. Hyperammonemia (968 mg/dL) was noted, followed by status epilepsy. Blood tests showed a creatinine level of 0.5 mg/dL, ALT level of 36 U/L, AST level of 17 U/L, total bilirubin level of 0.9 mg/dL, direct bilirubin level of 0.3 mg/dL, and the absence of viral hepatitis infection. The patient received mechanical ventilation and emergency hemodialysis for metabolic encephalopathy. However, he developed a coma as a result of severe brain edema and died of subsequent brain death.
3. Discussion
Infectious arthritis, reactive arthritis after certain infections, and rheumatic diseases should receive a differential diagnosis when patients present with fever and polyarthritis. Reactive arthritis was suspected during this patient’s first admission. However, this patient did not have typical symptoms of infection of the urethra, conjunctiva, or intestine. Microbial examinations did not identify common pathogens of reactive arthritis such as Chlamydia trachomatis, Salmonella, Shigella, Campylobacter, or Yersinia species. The diagnosis of reactive arthritis also needs to exclude malignancy [
7,
8].
Patients with PNS-related polyarthritis are more likely to be male (male-to-female ratio of 7:1) and have a median age of 54 years. Several solid tumors and hematologic malignancies are associated with PNS-related polyarthritis. Lung cancer is the most frequent type of solid malignancy. In contrast to most patients with inflammatory arthritis, patients with PNS-related polyarthritis respond poorly to corticosteroids and disease-modifying antirheumatic drugs [
5].
Thymoma is the most common lymphatic malignancy associated with PNS [
3]. In the group of patients with PNS of thymoma, 63.1% of patients present with myasthenia gravis and 7.7% of patients present with pure red cell aplasia. Lichen planus (6.3%), good syndrome (5.9%) and lupus (4.1%) are also often presented of this kind of patient [
1]. Cases involving thymoma with fever could be diagnosed as Good syndrome, for which invasive bacterial infection is a typical sign [
9]. However, polyarthritis rarely occurs in patents with Good syndrome. Seventy-six percent of patients diagnosed with both PNS and thymoma before surgery experience remission of PNS after tumor resection, although thirty-three percent of these patients have recurrence of symptoms or onset of new PNS 1 month after tumor resection [
1]. In our patient, fever and polyarthritis recurred 5 days after the VATs operation. In the literature, fever and polyarthritis mimicking reactive arthritis had never been reported in the context of PNS with thymoma. The patient had not responded to the treatment for reactive arthritis, including corticosteroid and sulfasalazine until VATs tumor resection [
7].
CMV viremia and fever developed 5 days after VATs. CMV colitis, C. difficile-related pseudomembranous colitis and severe ileus were noticed 14 days after VATs. Hyperammonemia and status epilepsy developed 20 days after VATs tumor resection. No abnormalities were detected for the possible secondary causes of hyperammonemia include liver disease, renal disease, infection, and medication record. Congenital causes, such as inborn errors of metabolism [
10], had been excluded because the patient had no congenital abnormalities or growth defects. CMV viremia and colitis, and pseudomembranous colitis were suspected as the major cause of this patient’s hyperammonemia. Long-term antibiotic and steroid use are risk factors for CMV and C. difficile colitis. Antibiotics had been prescribed for 2 months after the first admission because of the patient’s fever and suspected infections, especially because this patient was treated during the COVID-19 pandemic. We hypothesize that the risk of antibiotic-related CMV and C. difficile colitis may have been lower if the patient’s thymoma and associated PNS, which appeared as polyarthritis, had been identified earlier.