Diagnostic Accuracy and Prognostic Value of Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios in Septic Patients outside the Intensive Care Unit
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients Selection and Study Design
2.2. Laboratory and Microbiological Parameters
2.3. Statistical Analysis
3. Results
3.1. Baseline Patients’ Characteristics
3.2. Diagnostic Role of NLR
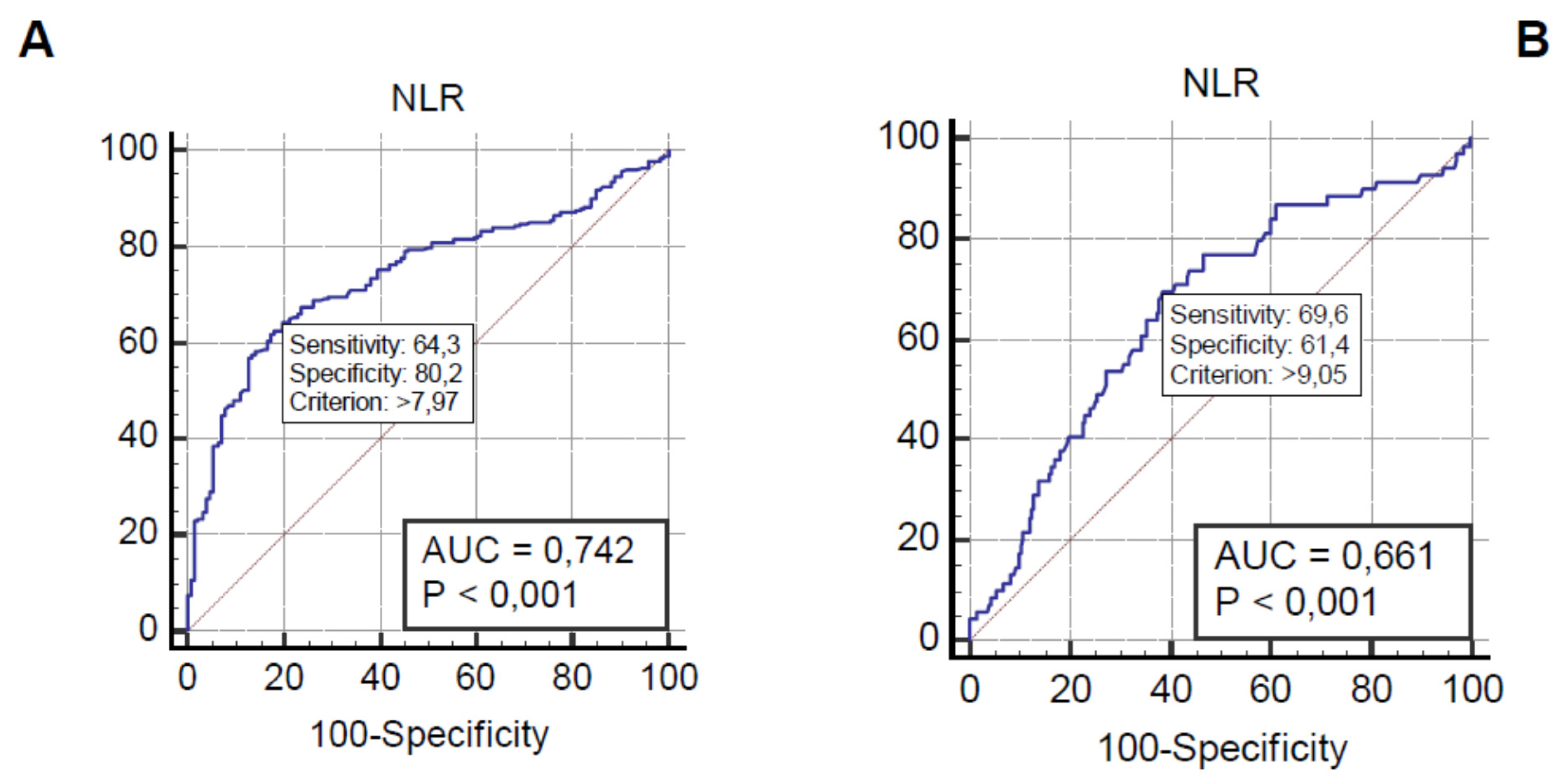
3.3. Role of NLR in Predicting 90-Day Mortality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AUCs | Areas under the curve |
| CBC | Complete blood counts |
| CRP | C-reactive protein |
| ICU | Intensive care unit |
| MR-proADM | Mid-regional pro-adrenomedullin |
| PCR | Polymerase chain reaction |
| PCT | Procalcitonin |
| PPV | Positive predictive value |
| NPV | Negative predictive value |
| ROC | Receiver operating characteristic |
| SIRS | Systemic inflammatory response syndrome |
| SOFA | Sequential sepsis-related organ failure assessment |
| WBC | White blood cell |
References
- Fleischmann, C.; Scherag, A.; Adhikari, N.K.J.; Hartog, C.S.; Tsaganos, T.; Schlattmann, P.; Angus, D.C.; Reinhart, K.; International Forum of Acute Care Trialists. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am. J. Respir. Crit. Care Med. 2016, 193, 259–272. [Google Scholar] [CrossRef]
- Churpek, M.M.; Snyder, A.; Han, X.; Sokol, S.; Pettit, N.; Howell, M.D.; Edelson, D.P. Quick sepsis-related organ failure assessment, systemic inflammatory response syndrome, and early warning scores for detecting clinical deterioration in infected patients outside the intensive care unit. Am. J. Respir. Crit. Care Med. 2017, 195, 906–911. [Google Scholar] [CrossRef] [Green Version]
- Leibovici, L.; Greenshtain, S.; Cohen, O.; Mor, F.; Wysenbeek, A.J. Bacteremia in febrile patients. A clinical model for diagnosis. Arch Intern Med 1991, 151, 1801–1806. [Google Scholar] [CrossRef] [PubMed]
- Bone, R.C.; Balk, R.A.; Cerra, F.B.; Dellinger, R.P.; Fein, A.M.; Knaus, W.A.; Schein, R.M.; Sibbald, W.J. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992, 101, 1644–1655. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spoto, S.; Nobile, E.; Rafano Carnà, E.P.; Fogolari, M.; Caputo, D.; De Florio, L.; Valeriani, E.; Benvenuto, D.; Costantino, S.; Ciccozzi, M.; et al. Best diagnostic accuracy of sepsis combining SIRS criteria or qSOFA score with Procalcitonin and Mid-Regional pro-Adrenomedullin outside ICU. Sci. Rep. 2020, 10, 16605. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.M.; Fink, M.P.; Marshall, J.C.; Abraham, E.; Angus, D.; Cook, D.; Cohen, J.; Opal, S.M.; Vincent, J.-L.; Ramsay, G. SCCM/ESICM/ACCP/ATS/SIS. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit. Care Med. 2003, 31, 1250–1256. [Google Scholar]
- Kopczynska, M.; Sharif, B.; Cleaver, S.; Spencer, N.; Kurani, A.; Lee, C.; Davis, J.; Durie, C.; Gubral, J.J.; Sharma, A.; et al. Red-flag sepsis and SOFA identifies different patient population at risk of sepsis-related deaths on the general ward. Medicine 2018, 97, e13238. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Diekema, D.J.; Hsueh, P.-R.; Mendes, R.E.; Pfaller, M.A.; Rolston, K.V.; Sader, H.S.; Jones, R.N. The microbiology of bloodstream infection: 20-year trends from the SENTRY antimicrobial surveillance program. Antimicrob. Agents Chemother. 2019, 63, e00355-19. [Google Scholar] [CrossRef] [Green Version]
- Sprung, C.L.; Schein, R.M.H.; Balk, R.A. The new sepsis consensus definitions: The good, the bad and the ugly. Intensive Care Med. 2016, 42, 2024–2026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horeczko, T.; Green, J.P.; Panacek, E.A. Epidemiology of the systemic inflammatory response syndrome (SIRS) in the emergency department. West J. Emerg. Med. 2014, 15, 329–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Florio, L.; Riva, E.; Giona, A.; Dedej, E.; Fogolari, M.; Cella, E.; Spoto, S.; Lai, A.; Zehender, G.; Ciccozzi, M.; et al. MALDI-TOF MS Identification and Clustering Applied to Enterobacter Species in Nosocomial Setting. Front. Microbiol. 2018, 14, 9:1885. [Google Scholar] [CrossRef] [PubMed]
- Angeletti, S.; Cella, E.; Prosperi, M.; Spoto, S.; Fogolari, M.; De Florio, L.; Antonelli, F.; Dedej, E.; De Flora, C.; Ferraro, E.; et al. Multi-drug resistant Pseudomonas aeruginosa nosocomial strains: Molecular epidemiology and evolution. Microb. Pathog. 2018, 123, 233–241. [Google Scholar] [CrossRef]
- Cella, E.; Ciccozzi, M.; Lo Presti, A.; Fogolari, M.; Azarian, T.; Prosperi, M.; Salemi, M.; Equestre, M.; Antonelli, F.; Conti, A.; et al. Multi-drug resistant Klebsiella pneumoniae strains circulating in hospital setting: Whole-genome sequencing and Bayesian phylogenetic analysis for outbreak investigations. Sci. Rep. 2017, 7, 3534. [Google Scholar] [CrossRef] [PubMed]
- Cancilleri, F.; Ciccozzi, M.; Fogolari, M.; Cella, E.; De Florio, L.; Berton, A.; Salvatore, G.; Dicuonzo, G.; Spoto, S.; Denaro, V.; et al. A case of methicillin-resistant Staphylococcus aureus wound infection: Phylogenetic analysis to establish if nosocomial or community acquired. Clin. Case Rep. 2018, 6, 871–874. [Google Scholar] [CrossRef]
- Santini, D.; Ratta, R.; Pantano, F.; De Lisi, D.; Maruzzo, M.; Galli, L.; Biasco, E.; Farnesi, A.; Buti, S.; Sternberg, C.N.; et al. Outcome of oligoprogressing metastatic renal cell carcinoma patients treated with locoregional therapy: A multicenter retrospective analysis. Oncotarget 2017, 7, 100708–100716. [Google Scholar] [CrossRef] [Green Version]
- Rizzo, S.; Galvano, A.; Pantano, F.; Iuliani, M.; Vincenzi, B.; Passiglia, F.; Spoto, S.; Tonini, G.; Bazan, V.; Russo, A.; et al. The effects of enzalutamide and abiraterone on skeletal related events and bone radiological progression free survival in castration resistant prostate cancer patients: An indirect comparison of randomized controlled trials. Crit. Rev. Oncol. Hematol. 2017, 120, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Sakr, Y.; Sprung, C.L.; Ranieri, V.M.; Reinhart, K.; Gerlach, H.; Moreno, R.; Carlet, J.; Le Gall, J.R.; Payen, D. Sepsis Occurrence in Acutely Ill Patients Investigators. Sepsis in European intensive care units: Results of the SOAP study. Crit. Care Med. 2006, 34, 344–353. [Google Scholar] [CrossRef]
- Bates, D.W.; Sands, K.; Miller, E.; Lanken, P.N.; Hibberd, P.L.; Graman, P.S.; Schwartz, J.S.; Kahn, K.; Snydman, D.R.; Parsonnet, J.; et al. Predicting bacteremia in patients with sepsis syndrome. J. Infect. Dis. 1997, 176, 1538–1551. [Google Scholar] [CrossRef] [Green Version]
- Sridharan, P.; Chamberlain, R.S. The efficacy of procalcitonin as a biomarker in the management of sepsis: Slaying dragons or tilting at windmills? Surg. Infect. 2013, 14, 489–511. [Google Scholar] [CrossRef]
- Spoto, S.; Fogolari, M.; De Florio, L.; Minieri, M.; Vicino, G.; Legramante, J.; Lia, M.S.; Terrinoni, A.; Caputo, D.; Costantino, S.; et al. Procalcitonin and MR-proAdrenomedullin combination in the etiological diagnosis and prognosis of sepsis and septic shock. Microb. Pathog. 2019, 137, 103763. [Google Scholar] [CrossRef] [PubMed]
- Briel, M.; Schuetz, P.; Mueller, B.; Young, J.; Schild, U.; Nusbaumer, C.; Périat, P.; Bucher, H.C.; Christ-Crain, M. Procalcitonin-guided antibiotic use vs a standard approach for acute respiratory tract infections in primary care. Arch. Intern. Med. 2008, 168, 2000–2007. [Google Scholar] [CrossRef]
- Stolz, D.; Christ-Crain, M.; Bingisser, R.; Leuppi, J.; Miedinger, D.; Müller, C.; Huber, P.; Müller, B.; Tamm, M. Antibiotic treatment of exacerbations of COPD: A randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest 2007, 131, 9–19. [Google Scholar] [CrossRef] [Green Version]
- Larsen, F.F.; Petersen, J.A. Novel biomarkers for sepsis: A narrative review. Eur. J. Intern. Med. 2017, 45, 46–50. [Google Scholar] [CrossRef]
- Spoto, S.; Valeriani, E.; Caputo, D.; Cella, E.; Fogolari, M.; Pesce, E.; Mulè, M.T.; Cartillone, M.; Costantino, S.; Dicuonzo, G.; et al. The role of procalcitonin in the diagnosis of bacterial infection after major abdominal surgery: Advantage from daily measurement. Medicine 2018, 97, e9496. [Google Scholar] [CrossRef]
- Spoto, S.; Cella, E.; De Cesaris, M.; Locorriere, L.; Mazzaroppi, S.; Nobile, E.; Lanotte, A.M.; Pedicino, L.; Fogolari, M.; Costantino, S.; et al. Procalcitonin and MR-Proadrenomedullin Combination with SOFA and qSOFA Scores for Sepsis Diagnosis and Prognosis: A Diagnostic Algorithm. Shock 2018, 50, 44–52. [Google Scholar] [CrossRef]
- Angeletti, S.; Ciccozzi, M.; Fogolari, M.; Spoto, S.; Lo Presti, A.; Costantino, S.; Dicuonzo, G. Procalcitonin and MR-proAdrenomedullin combined score in the diagnosis and prognosis of systemic and localized bacterial infections. J. Infect. 2016, 72, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Povoa, P.; Almeida, E.; Moreira, P.; Fernandes, A.; Mealha, R.; Aragao, A.; Sabino, H. C-reactive protein as an indicator of sepsis. Intensive Care Med. 1998, 24, 1052–1056. [Google Scholar] [CrossRef]
- Reny, J.L.; Vuagnat, A.; Ract, C.; Benoit, M.O.; Safar, M.; Fagon, J.Y. Diagnosis and follow-up of infections in intensive care patients: Value of C-reactive protein compared with other clinical and biological variables. Crit. Care Med. 2002, 30, 529–535. [Google Scholar] [CrossRef]
- de Jager, C.P.; van Wijk, P.T.; Mathoera, R.B.; de Jongh-Leuvenink, J.; van der Poll, T.; Wever, P.C. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit. Care 2010, 14, R192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Jager, C.P.; Wever, P.C.; Gemen, E.F.; Kusters, R.; van Gageldonk-Lafeber, A.B.; van der Poll, T.; Laheij, R.J.F. The neutrophil-lymphocyte count ratio in patients with community-acquired pneumonia. PLoS ONE 2012, 7, e46561. [Google Scholar] [CrossRef]
- Zhiwei, H.; Zhaoyin, F.; Wujun, H.; Kegang, H. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: A meta-analysis. Am. J. Emerg. Med. 2020, 38, 641–647. [Google Scholar]
- Forget, P.; Khalifa, C.; Defour, J.P.; Latinne, D.; Van Pel, M.C.; De Kock, M. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res. Notes 2017, 10, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.S.; Kim, N.Y.; Na, S.H.; Youn, Y.H.; Shin, C.S. Reference values of neutrophil lymphocyte ratio, lymphocyte-monocyte ratio, platelet-lymphocyte ratio, and mean platelet volume in healthy adults in South Korea. Medicine 2018, 97, e11138. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Liu, R.; Yu, X.; Yang, R.; Xu, H.; Mao, Z.; Wang, Y. The neutrophil-lymphocyte count ratio as a diagnostic marker for bacteraemia: A systematic review and meta-analysis. Am. J. Emerg. Med. 2019, 37, 1482–1489. [Google Scholar] [CrossRef]
- Zhang, H.B.; Chen, J.; Lan, Q.F.; Ma, X.J.; Zhang, S.Y. Diagnostic values of red cell distribution width, platelet distribution width and neutrophil-lymphocyte count ratio for sepsis. Exp. Ther. Med. 2016, 12, 2215–2219. [Google Scholar] [CrossRef] [Green Version]
- Laukemann, S.; Kasper, N.; Kulkarni, P.; Steiner, D.; Rast, A.C.; Kutz, A.; Felder, S.; Haubitz, S.; Faessler, L.; Huber, A.; et al. Can we reduce negative blood cultures with clinical scores and blood markers? Results from an observational cohort study. Medicine 2015, 94, e2264. [Google Scholar] [CrossRef]
- Lowsby, R.; Gomes, C.; Jarman, I.; Lisboa, P.; Nee, P.A.; Vardhan, M.; Eckersley, T.; Saleh, R.; Mills, H. Neutrophil to lymphocyte count ratio as an early indicator of blood stream infection in the emergency department. Emerg. Med. J. 2015, 32, 531–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loonen, A.J.M.; de Jager, C.P.; Tosserams, J.; Kusters, R.; Hilbink, M.; Wever, P.C.; van den Brule, A.J. Biomarkers and molecular analysis to improve bloodstream infection diagnostics in an emergency care unit. PLoS ONE 2014, 9, e87315. [Google Scholar] [CrossRef] [Green Version]
- Ljungstrom, L.; Pernestig, A.K.; Jacobsson, G.; Andersson, R.; Usener, B.; Tilevik, D. Diagnostic accuracy of procalcitonin, neutrophil-lymphocyte count ratio, C-reactive protein, and lactate in patients with suspected bacterial sepsis. PLoS ONE 2017, 12, e0181704. [Google Scholar] [CrossRef]
- Russell, C.D.; Parajuli, A.; Gale, H.J.; Bulteel, N.S.; Schuetz, P.; de Jager, C.P.; Loonen, A.J.M.; Merekoulias, G.I.; Baillie, J.K. The utility of peripheral blood leucocyte ratios as biomarkers in infectious diseases: A systematic review and meta-analysis. J. Infect. 2019, 78, 339–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Djordjevic, D.; Rondovic, G.; Surbatovic, M.; Stanojevic, I.; Udovicic, I.; Andjelic, T.; Zeba, S.; Milosavljevic, S.; Stankovic, N.; Abazovic, D.; et al. Neutrophil-to-Lymphocyte Ratio, Monocyte-to-Lymphocyte Ratio, Platelet-to-Lymphocyte Ratio, and Mean Platelet Volumeto- Platelet Count Ratio as Biomarkers in Critically Ill and Injured Patients: Which Ratio to Choose to Predict Outcome and Nature of Bacteremia? Mediat. Inflamm. 2018, 2018, 3758068. [Google Scholar]
- Cheung, K.C.P.; Fanti, S.; Mauro, C.; Wang, G.; Nair, A.S.; Fu, H.; Angeletti, S.; Spoto, S.; Fogolari, M.; Romano, F.; et al. Preservation of microvascular barrier function requires CD31 receptor-induced metabolic reprogramming. Nat. Commun. 2020, 11, 3595. [Google Scholar] [CrossRef] [PubMed]
- Angeletti, S.; Fogolari, M.; Morolla, D.; Capone, F.; Costantino, S.; Spoto, S.; De Cesaris, M.; Lo Presti, A.; Ciccozzi, M.; Dicuonzo, G. Role of neutrophil gelatinase-associated lipocalin in the diagnosis and early treatment of acute kidney injury in a case series of patients with acute decompensated heart failure: A case series. Cardiol. Res. Pract. 2016, 2016, 3708210. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ATS. Guidelines for the management of adults with hospital acquired, ventilator-associated, and healthcare-associated pneumonia. Am. J. Respir. Crit. Care. Med. 2005, 171, 388–416. [Google Scholar] [CrossRef] [PubMed]
- CDC. Urinary Tract Infection (Catheter-Associated Urinary Tract Infection [CAUTI] and Non-Catheter-Associated Urinary Tract Infection [UTI]) and Other Urinary System Infection [USI]) Events; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2016. [Google Scholar]
- Spoto, S.; Costantino, S.; Fogolari, M.; Valeriani, E.; Ciccozzi, M.; Angeletti, S. An algorithm of good clinical practice to reduce intra-hospital 90-day mortality and need for Intensive Care Unit transfer: A new approach for septic patient management. Ital. J. Med. 2020, 14, 14–21. [Google Scholar] [CrossRef]
| Variables | Patients with Sepsis N = 251 | Patients without Sepsis N = 126 | p-Value |
|---|---|---|---|
| Age, y | 73.0 (65.0, 80.0) | 80.0 (68.5, 86.0) | 0.001 |
| Male sex, n (%) | 132 (52.6) | 63 (50.4) | 0.771 |
| Steroid use, n (%) | 62 (24.8) | 27 (21.6) | 0.577 |
| Ongoing chemotherapy, n (%) | 7 (2.8) | 1 (0.8) | 0.376 |
| Septic shock, n (%) | 100 (39.8) | 0 (0.0) | <0.001 |
| Smoke history (%) | <0.001 | ||
| Never | 180 (71.7) | 55 (44.0) | |
| Former | 61 (24.3) | 52 (41.6) | |
| Current | 10 (4.0) | 18 (14.4) | |
| Diabetes mellitus type 2, n (%) | 56 (22.3) | 29 (23.0) | 0.981 |
| Cancer, n (%) | 92 (36.7) | 30 (23.8) | 0.016 |
| Lung disease, n (%) | 58 (23.1) | 43 (34.1) | 0.031 |
| Heart disease, n (%) | 137 (54.6) | 74 (59.2) | 0.459 |
| Liver disease, n (%) | 24 (9.6) | 8 (6.3) | 0.390 |
| Chronic kidney disease, n (%) | 73 (29.1) | 34 (27.0) | 0.760 |
| Chronic cerebrovascular disease, n (%) | 68 (27.1) | 19 (15.1) | 0.013 |
| SIRS, median values [IQR] | 2 (1, 3) | 0 (0, 1) | <0.001 |
| q-SOFA, median values [IQR] | 2 (1, 2) | 0 (0, 0) | <0.001 |
| SOFA, median values [IQR] | 4 (2, 6) | 2 (1, 3) | <0.001 |
| NLR, median [IQR] | 10.7 (6.3, 18.7) | 5.4 (3.7, 7.4) | <0.001 |
| PLR, median [IQR] | 228.7 (147.8, 407.9) | 219.7 (147.1, 308.2) | 0.049 |
| CRP, median [IQR] | 107.5 (41.8, 173.7) | 8.5 (2.3, 16.5) | <0.001 |
| PCT, median [IQR] | 1.2 (0.4, 5.2) | 0.1 (0.1, 0.3) | <0.001 |
| MR-proADM, median [IQR] | 1.2 (0.8, 1.9) | 2.8 (1.8, 4.5) | <0.001 |
| Lenght of stay, median [IQR] | 15.0 (11.0, 25.5) | 10.0 (7.0, 13.0) | <0.001 |
| ICU admission, n (%) | 47 (18.7) | 0 (0.0) | <0.001 |
| 90-day mortality | 69 (27.5) | 1 (0.8) | <0.001 |
| Model | Cut-Off | Sensibility | Specificity | AUC | p | PPV | NPV |
|---|---|---|---|---|---|---|---|
| NLR | 7.97 | 64.26 | 80.16 | 0.74 | <0.001 | 86.49 | 53.18 |
| PLR | 370.59 | 29.3 | 92.1 | 0.56 | 0.037 | 87.99 | 39.72 |
| PCR | 37.88 | 78.75 | 93.51 | 0.92 | <0.0001 | 95.93 | 60.46 |
| PCT | 0.41 | 79.6 | 81.00 | 0.88 | <0.001 | 89.26 | 60.67 |
| MR-proADM | 1.83 | 80.1 | 74.6 | 0.86 | <0.0001 | 85.51 | 66.68 |
| SIRS | ≥2 | 67.3 | 89.7 | 0.57 | <0.001 | 96.77 | 43.30 |
| q-SOFA | ≥2 | 51.4 | 99.2 | 0.87 | <0.001 | 99.23 | 50.21 |
| SOFA | ≥2 | 69.7 | 71.4 | 0.77 | <0.001 | 82.94 | 54.21 |
| Model * | PPV | NPV |
|---|---|---|
| NLR | 86.49 | 53.18 |
| PLR | 87.99 | 39.73 |
| PCR | 95.93 | 69.46 |
| PCT | 89.26 | 66.68 |
| MR-proADM | 85.52 | 66.68 |
| SIRS | 96.77 | 43.31 |
| qSOFA | 99.23 | 50.21 |
| SOFA | 82.94 | 54.21 |
| NLR + PLR | 96.00 | 83.00 |
| NLR + PCR | 98.70 | 59.00 |
| NLR + PCT | 96.49 | 61.50 |
| NLR + ADM | 95.30 | 63.30 |
| NLR + SIRS | 98.90 | 81.00 |
| NLR + q-SOFA | 99.70 | 76.00 |
| NLR + SOFA | 94.00 | 73.00 |
| NLR + PLR + SIRS | 99.70 | 94.00 |
| NLR + PLR + q-SOFA | 99.90 | 95.60 |
| NLR + PLR + SOFA | 98.30 | 91.60 |
| Model | Cut-Off | Sensibility | Specificity | AUC | p | PPV | NPV |
|---|---|---|---|---|---|---|---|
| NLR | 9.05 | 69.57 | 61.44 | 0.66 | <0.001 | 71.40 | 89.90 |
| PCR | 37.88 | 83.33 | 52.35 | 0.67 | <0.001 | 27.90 | 93.40 |
| PCT | 0.39 | 90.00 | 47.00 | 0.70 | <0.001 | 27.98 | 95.36 |
| MR-proADM | 3.21 | 76.50 | 71.40 | 0.79 | <0.001 | 38.20 | 92.92 |
| SIRS | ≥2 | 44.29 | 79.80 | 0.72 | <0.001 | 33.33 | 86.26 |
| q-SOFA | ≥2 | 25.70 | 91.48 | 0.80 | <0.001 | 40.90 | 84.20 |
| SOFA | ≥2 | 92.86 | 52.44 | 0.82 | <0.001 | 30.80 | 96.98 |
| Model * | PVV | NPV |
|---|---|---|
| NLR | 28.9 | 89.9 |
| NLR + MR-proADM | 52.0 | 50.0 |
| NLR + SIRS | 95.0 | 86.0 |
| NLR + q-SOFA | 96.0 | 88.0 |
| NLR + SOFA | 94.6 | 89.9 |
| Model | OR (95% CI) | p-Values |
|---|---|---|
| NLR | 1.002 (0.968 to 1.037) | 0.912 |
| PLR | 0.999 (0.997 to 1.000) | 0.142 |
| MLR | 0.952 (0.489 to 1.753) | 0.878 |
| CRP | 0.998 (0.994 to 1.002) | 0.270 |
| PCT | 0.989 (0.966 to 1.006) | 0.226 |
| MRproADM | 1.406 (1.219 to 1.657) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Spoto, S.; Lupoi, D.M.; Valeriani, E.; Fogolari, M.; Locorriere, L.; Beretta Anguissola, G.; Battifoglia, G.; Caputo, D.; Coppola, A.; Costantino, S.; et al. Diagnostic Accuracy and Prognostic Value of Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios in Septic Patients outside the Intensive Care Unit. Medicina 2021, 57, 811. https://doi.org/10.3390/medicina57080811
Spoto S, Lupoi DM, Valeriani E, Fogolari M, Locorriere L, Beretta Anguissola G, Battifoglia G, Caputo D, Coppola A, Costantino S, et al. Diagnostic Accuracy and Prognostic Value of Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios in Septic Patients outside the Intensive Care Unit. Medicina. 2021; 57(8):811. https://doi.org/10.3390/medicina57080811
Chicago/Turabian StyleSpoto, Silvia, Domenica Marika Lupoi, Emanuele Valeriani, Marta Fogolari, Luciana Locorriere, Giuseppina Beretta Anguissola, Giulia Battifoglia, Damiano Caputo, Alessandro Coppola, Sebastiano Costantino, and et al. 2021. "Diagnostic Accuracy and Prognostic Value of Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios in Septic Patients outside the Intensive Care Unit" Medicina 57, no. 8: 811. https://doi.org/10.3390/medicina57080811
APA StyleSpoto, S., Lupoi, D. M., Valeriani, E., Fogolari, M., Locorriere, L., Beretta Anguissola, G., Battifoglia, G., Caputo, D., Coppola, A., Costantino, S., Ciccozzi, M., & Angeletti, S. (2021). Diagnostic Accuracy and Prognostic Value of Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios in Septic Patients outside the Intensive Care Unit. Medicina, 57(8), 811. https://doi.org/10.3390/medicina57080811










