The Patient-Reported Outcome Measures Used with Low Back Pain and the Attitude of Primary Healthcare Practitioners in Saudi Arabia toward Them †
Abstract
1. Background
2. Methods
2.1. Design and Setting
2.2. Outcome Measure
2.3. Data Analyses
3. Results
3.1. Participants and Their Characteristics
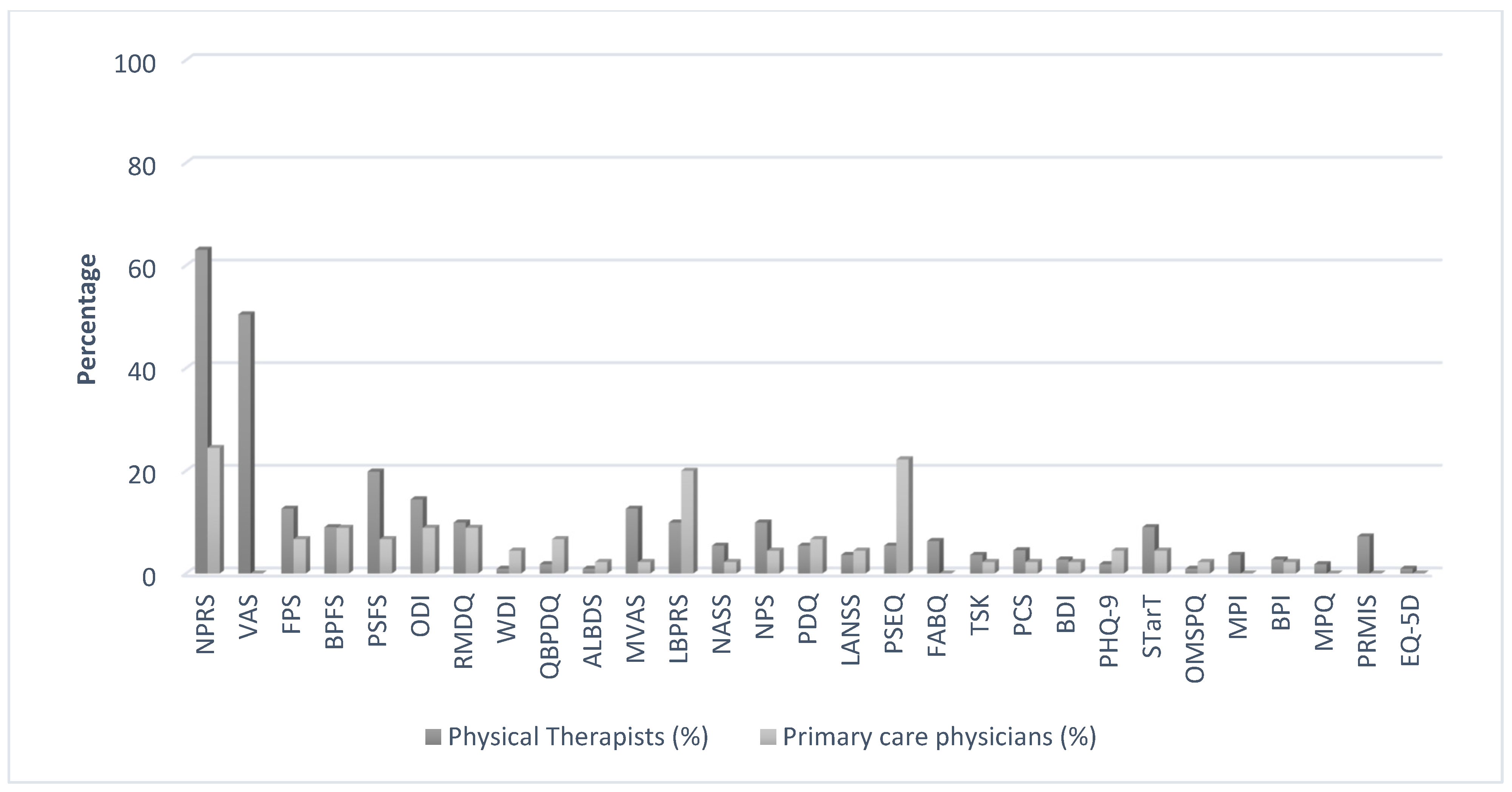
3.2. Use of PROMs
3.3. Attitudes, Knowledge, and Beliefs about the Use of PROMs
4. Discussion
4.1. Statement of Principal Findings
4.2. Interpretation within the Context of the Wider Literature
4.3. Strengths and Limitations
4.4. Implications for Policy, Practice, and Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LBP | Low back pain |
| MSK | Musculoskeletal |
| NRS | Numeric pain rating scale |
| VAS | Visual analogue scale |
| PROMs | Patient-reported outcome measures |
| SPSS | Statistical Package for the Social Sciences |
References
- Buchbinder, R.; Blyth, F.M.; March, L.M.; Brooks, P.; Woolf, A.D.; Hoy, D.G. Placing the global burden of low back pain in context. Best Pract. Res. Clin. Rheumatol. 2013, 27, 575–589. [Google Scholar] [CrossRef] [PubMed]
- Gore, M.; Sadosky, A.; Stacey, B.R.; Tai, K.S.; Leslie, D. The burden of chronic low back pain: Clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine 2012, 37, E668–E677. [Google Scholar] [CrossRef] [PubMed]
- Hoy, D.G.; Smith, E.; Cross, M.; Sanchez-Riera, L.; Buchbinder, R.; Blyth, F.M.; Brooks, P.; Woolf, A.D.; Osborne, R.H.; Fransen, M.; et al. The global burden of musculoskeletal conditions for 2010: An overview of methods. Ann. Rheum. Dis. 2014, 73, 982–989. [Google Scholar] [CrossRef]
- Hurwitz, E.L.; Randhawa, K.; Yu, H.; Cote, P.; Haldeman, S. The Global Spine Care Initiative: A summary of the global burden of low back and neck pain studies. Eur. Spine J. 2018, 27, 796–801. [Google Scholar] [CrossRef]
- Memish, Z.A.; Jaber, S.; Mokdad, A.H.; AlMazroa, M.A.; Murray, C.J.; Al Rabeeah, A.A.; Saudi Burden of Disease Collaborators. Burden of disease, injuries, and risk factors in the Kingdom of Saudi Arabia, 1990–2010. Prev. Chronic Dis. 2014, 11, E169. [Google Scholar] [CrossRef]
- Frymoyer, J.W. Predicting disability from low back pain. Clin. Orthop. Relat. Res. 1992, 279, 101–109. [Google Scholar] [CrossRef]
- Loney, P.L.; Stratford, P.W. The prevalence of low back pain in adults: A methodological review of the literature. Phys. Ther. 1999, 79, 384–396. [Google Scholar] [CrossRef] [PubMed]
- Oleske, D.M.; Lavender, S.A.; Andersson, G.B.; Morrissey, M.J.; Zold-Kilbourn, P.; Allen, C.; Taylor, E. Risk factors for recurrent episodes of work-related low back disorders in an industrial population. Spine 2006, 31, 789–798. [Google Scholar] [CrossRef]
- Walker, B.F.; Muller, R.; Grant, W.D. Low back pain in Australian adults: Prevalence and associated disability. J. Manip. Physiol. Ther. 2004, 27, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, J. The applications of PROs in clinical practice: What are they, do they work, and why? Qual. Life Res. 2009, 18, 115–123. [Google Scholar] [CrossRef]
- Lin, X.-J.; Lin, I.-M.; Fan, S.-Y. Methodological issues in measuring health-related quality of life. Tzu Chi Med. J. 2013, 25, 8–12. [Google Scholar] [CrossRef]
- Sajid, M.S.; Tonsi, A.; Baig, M.K. Health-related quality of life measurement. Int. J. Health Care Qual. Assur. 2008, 21, 365–373. [Google Scholar] [CrossRef]
- Westaway, M.D.; Stratford, P.W.; Binkley, J.M. The patient-specific functional scale: Validation of its use in persons with neck dysfunction. J. Orthop. Sports Phys. Ther. 1998, 27, 331–338. [Google Scholar] [CrossRef]
- Kamper, S.J.; Stanton, T.R.; Williams, C.M.; Maher, C.G.; Hush, J.M. How is recovery from low back pain measured? A systematic review of the literature. Eur. Spine J. 2011, 20, 9–18. [Google Scholar] [CrossRef]
- Kennedy, D.M.; Stratford, P.W.; Robarts, S.; Gollish, J.D. Using outcome measure results to facilitate clinical decisions the first year after total hip arthroplasty. J. Orthop. Sports Phys. Ther. 2011, 41, 232–240. [Google Scholar] [CrossRef]
- Alshehri, F.; Alarabi, A.; Alharthi, M.; Alanazi, T.; Alohali, A.; Alsaleem, M. Use of patient-reported outcome measures (PROMs) by orthopedic surgeons in Saudi Arabia. J. Orthop. Surg. Res. 2020, 15, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Al-Muqiren, T.N.; Al-Eisa, E.S.; Alghadir, A.H.; Anwer, S. Implementation and use of standardized outcome measures by physical therapists in Saudi Arabia: Barriers, facilitators and perceptions. BMC Health Serv. Res. 2017, 17, 748. [Google Scholar] [CrossRef]
- El-Sobkey, S.B.; Helmy, A.M. Evidence-based practice and standardized outcome measures: Egyptian physical therapists’ beliefs, perceptions and adoption. World Appl. Sci. J. 2012, 16, 1282–1291. [Google Scholar]
- Van Peppen, R.P.; Maissan, F.J.; Van Genderen, F.R.; Van Dolder, R.; Van Meeteren, N.L. Outcome measures in physiotherapy management of patients with stroke: A survey into self-reported use, and barriers to and facilitators for use. Physiother. Res. Int. 2008, 13, 255–270. [Google Scholar] [CrossRef]
- Swinkels, R.A.; van Peppen, R.P.; Wittink, H.; Custers, J.W.; Beurskens, A.J. Current use and barriers and facilitators for implementation of standardised measures in physical therapy in the Netherlands. BMC Musculoskelet. Disord. 2011, 12, 106. [Google Scholar] [CrossRef]
- Copeland, J.M.; Taylor, W.J.; Dean, S.G. Factors influencing the use of outcome measures for patients with low back pain: A survey of New Zealand physical therapists. Phys. Ther. 2008, 88, 1492–1505. [Google Scholar] [CrossRef] [PubMed]
- Boyce, M.B.; Browne, J.P.; Greenhalgh, J. The experiences of professionals with using information from patient-reported outcome measures to improve the quality of healthcare: A systematic review of qualitative research. BMJ Qual. Saf. 2014, 23, 508–518. [Google Scholar] [CrossRef]
- Calvert, M.; Brundage, M.; Jacobsen, P.B.; Schunemann, H.J.; Efficace, F. The CONSORT Patient-Reported Outcome (PRO) extension: Implications for clinical trials and practice. Health Qual. Life Outcomes 2013, 11, 184. [Google Scholar] [CrossRef] [PubMed]
- Hatfield, D.R.; Ogles, B.M. The Use of Outcome Measures by Psychologists in Clinical Practice. Prof. Psychol. Res. Pract. 2004, 35, 485. [Google Scholar] [CrossRef]
- Hughes, E.F.; Wu, A.W.; Carducci, M.A.; Snyder, C.F. What can I do? Recommendations for responding to issues identified by patient-reported outcomes assessments used in clinical practice. J. Supportive Oncol. 2012, 10, 143. [Google Scholar] [CrossRef][Green Version]
- Lydick, E.; Epstein, R.S. Interpretation of quality of life changes. Qual Life Res. 1993, 2, 221–226. [Google Scholar] [CrossRef]
- Buchbinder, R.; van Tulder, M.; Oberg, B.; Costa, L.M.; Woolf, A.; Schoene, M.; Croft, P.; Lancet Low Back Pain Series Working Group. Low back pain: A call for action. Lancet 2018, 391, 2384–2388. [Google Scholar] [CrossRef]
- Traeger, A.C.; Buchbinder, R.; Elshaug, A.G.; Croft, P.R.; Maher, C.G. Care for low back pain: Can health systems deliver? Bull. World Health Organ. 2019, 97, 423. [Google Scholar] [CrossRef]
- Jette, D.U.; Halbert, J.; Iverson, C.; Miceli, E.; Shah, P. Use of standardized outcome measures in physical therapist practice: Perceptions and applications. Phys. Ther. 2009, 89, 125–135. [Google Scholar] [CrossRef]
- Stokes, E.K.; O’Neill, D. The use of standardised assessments by physiotherapists. Br. J. Ther. Rehabil. 1999, 6, 560–565. [Google Scholar] [CrossRef]
- Östhols, S.; Boström, C.; Rasmussen-Barr, E. Clinical assessment and patient-reported outcome measures in low-back pain–A survey among primary health care physiotherapists. Disabil. Rehabil. 2019, 41, 2459–2467. [Google Scholar] [CrossRef]
- Campbell, P.; Foster, N.E.; Thomas, E.; Dunn, K.M. Prognostic indicators of low back pain in primary care: Five-year prospective study. J. Pain 2013, 14, 873–883. [Google Scholar] [CrossRef]
- Alamam, D.M.; Moloney, N.; Leaver, A.; Alsobayel, H.I.; Mackey, M.G. Multidimensional prognostic factors for chronic low back pain-related disability: A longitudinal study in a Saudi population. Spine J. 2019, 19, 1548–1558. [Google Scholar] [CrossRef]
- Haigh, R.; Tennant, A.; Biering-Sorensen, F.; Grimby, G.; Marincek, C.; Phillips, S.; Ring, H.; Tesio, L.; Thonnard, J.-L. The use of outcome measures in physical medicine and rehabilitation within Europe. J. Rehabil. Med. 2001, 33, 273–278. [Google Scholar]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Steenstra, I.A.; Munhall, C.; Irvin, E.; Oranye, N.; Passmore, S.; Van Eerd, D.; Mahood, Q.; Hogg-Johnson, S. Systematic Review of Prognostic Factors for Return to Work in Workers with Sub Acute and Chronic Low Back Pain. J. Occup. Rehabil. 2017, 27, 369–381. [Google Scholar] [CrossRef]
- Verkerk, K.; Luijsterburg, P.A.; Miedema, H.S.; Pool-Goudzwaard, A.; Koes, B.W. Prognostic factors for recovery in chronic nonspecific low back pain: A systematic review. Phys. Ther. 2012, 92, 1093–1108. [Google Scholar] [CrossRef] [PubMed]
- Ramond, A.; Bouton, C.; Richard, I.; Roquelaure, Y.; Baufreton, C.; Legrand, E.; Huez, J.F. Psychosocial risk factors for chronic low back pain in primary care--a systematic review. Fam. Pract. 2011, 28, 12–21. [Google Scholar] [CrossRef]
- Duncan, E.A.; Murray, J. The barriers and facilitators to routine outcome measurement by allied health professionals in practice: A systematic review. BMC Health Serv. Res. 2012, 12, 96. [Google Scholar] [CrossRef]
- Ferreira, M.L.; Herbert, R.D.; Ferreira, P.H.; Latimer, J.; Ostelo, R.W.; Nascimento, D.P.; Smeets, R.J. A critical review of methods used to determine the smallest worthwhile effect of interventions for low back pain. J. Clin. Epidemiol. 2012, 65, 253–261. [Google Scholar] [CrossRef] [PubMed]
| Primary Care Physicians (n = 45) | Physical Therapists (n = 111) | ||||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Gender | Male | 27 | 60 | 65 | 58.6 |
| Female | 18 | 40 | 46 | 41.4 | |
| Age (years) | 20–30 | 6 | 13.3 | 51 | 45.9 |
| 31–40 | 21 | 46.7 | 48 | 43.2 | |
| 41–50 | 10 | 22.2 | 11 | 9.9 | |
| >50 | 8 | 17.8 | 1 | 0.9 | |
| Nationality | Saudi | 18 | 40 | 104 | 93.7 |
| Non-Saudi | 27 | 60 | 7 | 6.3 | |
| Years of experience | <2 years | 6 | 13.3 | 27 | 24.3 |
| 2–10 years | 21 | 46.7 | 46 | 41.4 | |
| 11–20 years | 10 | 22.2 | 30 | 27.0 | |
| >20 years | 8 | 17.8 | 8 | 7.2 | |
| Number of Selected Outcome Measures | n | % | |
|---|---|---|---|
| Primary care physicians (n = 45) | 0 | 7 | 15.6 |
| 1 | 23 | 51.1 | |
| 2 | 10 | 22.2 | |
| ≥3 | 5 | 11.0 | |
| Physical therapists (n = 111) | 0 | 5 | 4.5 |
| 1 | 30 | 27.0 | |
| 2 | 28 | 25.2 | |
| ≥3 | 48 | 43.2 |
| Statements | Strongly Agree n (%) | Agree n (%) | Neutral n (%) | Disagree n (%) | Strongly Disagree n (%) | |
|---|---|---|---|---|---|---|
| I am confident in selecting an outcome measure with known reliability, validity, and demonstrated sensitivity to change. | PCP | 6 (13.3) | 24 (53.3) | 13 (28.9) | 1 (2.2) | 1 (2.2) |
| PT | 24 (21.6) | 54 (48.6) | 29 (26.1) | 3 (2.7) | 1 (0.9) | |
| I often rely on the patient’s history to select the best outcome measure. | PCP | 9 (20.0) | 26 (57.8) | 9 (20.0) | 1 (2.2) | 0 (0.0) |
| PT | 49 (44.1) | 39 (35.1) | 20 (18.0) | 2 (1.8) | 1 (0.9) | |
| I administer the outcome measures on intake, reassessment, and upon discharge and I know the suggested time frame for repeat administration. | PCP | 5 (11.1) | 23 (51.1) | 15 (33.3) | 1 (2.2) | 1 (2.2) |
| PT | 34 (30.6) | 46 (41.4) | 21 (18.9) | 9 (8.1) | 1 (0.9) | |
| I am familiar with the scoring procedure for the outcome measures that I use. | PCP | 2 (4.4) | 16 (35.6) | 17 (37.8) | 8 (17.8) | 2 (4.4) |
| PT | 38 (34.2) | 52 (46.8) | 16 (14.4) | 4 (3.6) | 1 (0.9) | |
| Clinical outcome measures are reflective of the clinical presentation. | PCP | 2 (4.4) | 28 (62.2) | 13 (28.9) | 1 (2.2) | 1 (2.2) |
| PT | 31 (27.9) | 53 (47.7) | 19 (17.1) | 7 (6.3) | 1 (0.9) | |
| I can understand the clinical meaning of the range of scores. | PCP | 2 (4.4) | 24 (53.3) | 14 (31.1) | 4 (8.9) | 0 (0.0) |
| PT | 32 (28.8) | 45 (40.5) | 30 (27.0) | 3 (2.7) | 1 (0.9) | |
| I am familiar with the Minimum Detectable Change (MDC) and the Minimally Clinically Important Difference (MCID). | PCP | 1 (2.2) | 10 (22.2) | 18 (40.0) | 12 (26.7) | 3 (6.7) |
| PT | 13 (11.7) | 31 (27.9) | 36 (32.4) | 24 (21.6) | 7 (6.3) | |
| There is a lack of Arabic versions of pain assessment measures. | PCP | 5 (11.1) | 22 (48.9) | 15 (33.3) | 2 (4.4) | 1 (2.2) |
| PT | 53 (47.7) | 35 (31.5) | 12 (10.8) | 9 (8.1) | 2 (1.8) | |
| Pain outcome measures should be multidimensional rather than unidimensional (i.e., just pain intensity). | PCP | 8 (17.8) | 22 (48.9) | 13 (28.9) | 1 (2.2) | 0 (0.0) |
| PT | 53 (47.7) | 33 (29.7) | 16 (14.4) | 8 (7.2) | 1 (0.9) | |
| I usually don’t have time to administer or track outcome measures with my patients. | PCP | 3 (6.7) | 20 (44.4) | 11 (24.4) | 10 (22.2) | 0 (0.0) |
| PT | 23 (20.7) | 35 (31.5) | 27 (24.3) | 19 (17.1) | 7 (6.3) | |
| Pain intensity outcome measures are primary outcome measures with my LBP patients. | PCP | 3 (6.7) | 26 (57.8) | 15 (33.3) | 1 (2.2) | 0 (0.0) |
| Pain intensity outcome measures are primary outcome measures with my acute LBP patients. | PT | 37 (33.3) | 48 (43.2) | 23 (20.7) | 2 (1.8) | 1 (0.9) |
| Pain intensity outcome measures are primary outcome measures with my chronic LBP patients. | PT | 36 (32.4) | 50 (45.0) | 17 (15.3) | 8 (7.2) | 0 (0.0) |
| Functional disability outcome measures are primary outcome measures with my LBP patients. | PCP | 2 (4.4) | 19 (42.2) | 21 (46.7) | 3 (6.7) | 0 (0.0) |
| Functional disability outcome measures are primary outcome measures with my acute LBP patients. | PT | 36 (32.4) | 47 (42.3) | 19 (17.1) | 9 (8.1) | 0 (0.0) |
| Functional disability outcome measures are primary outcome measures with my chronic LBP patients. | PT | 48 (43.2) | 39 (35.1) | 20 (18.0) | 4 (3.6) | 0 (0.0) |
| Psychosocial outcome measures are primary outcome measures with my LBP patients. | PCP | 3 (6.7) | 22 (48.9) | 15 (33.3) | 4 (8.9) | 0 (0.0) |
| Psychosocial outcome measures are primary outcome measures with my acute LBP patients. | PT | 25 (22.5) | 27 (24.3) | 41 (36.9) | 16 (14.4) | 2 (1.8) |
| Psychosocial outcome measures are primary outcome measures with my chronic LBP patients. | PT | 41 (36.9) | 38 (34.2) | 21 (18.9) | 10 (9.0) | 1 (0.9) |
| Quality-of-life outcome measures are primary outcome measures with my LBP patients. | PCP | 8 (17.8) | 22 (48.9) | 10 (22.2) | 2 (4.4) | 1 (2.2) |
| Quality-of-life outcome measures are primary outcome measures with my acute LBP patients. | PT | 25 (22.5) | 45 (40.5) | 23 (20.7) | 16 (14.4) | 2 (1.8) |
| Quality-of-life outcome measures are primary outcome measures with my chronic LBP patients. | PT | 40 (36.0) | 48 (43.2) | 17 (15.3) | 5 (4.5) | 1 (0.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhowimel, A.; Alodaibi, F.; Alotaibi, M.; Alamam, D.; Fritz, J. The Patient-Reported Outcome Measures Used with Low Back Pain and the Attitude of Primary Healthcare Practitioners in Saudi Arabia toward Them. Medicina 2021, 57, 812. https://doi.org/10.3390/medicina57080812
Alhowimel A, Alodaibi F, Alotaibi M, Alamam D, Fritz J. The Patient-Reported Outcome Measures Used with Low Back Pain and the Attitude of Primary Healthcare Practitioners in Saudi Arabia toward Them. Medicina. 2021; 57(8):812. https://doi.org/10.3390/medicina57080812
Chicago/Turabian StyleAlhowimel, Ahmed, Faris Alodaibi, Mazyad Alotaibi, Dalyah Alamam, and Julie Fritz. 2021. "The Patient-Reported Outcome Measures Used with Low Back Pain and the Attitude of Primary Healthcare Practitioners in Saudi Arabia toward Them" Medicina 57, no. 8: 812. https://doi.org/10.3390/medicina57080812
APA StyleAlhowimel, A., Alodaibi, F., Alotaibi, M., Alamam, D., & Fritz, J. (2021). The Patient-Reported Outcome Measures Used with Low Back Pain and the Attitude of Primary Healthcare Practitioners in Saudi Arabia toward Them. Medicina, 57(8), 812. https://doi.org/10.3390/medicina57080812






