Cardiotoxicity Associated with Chemotherapy Used in Gastrointestinal Tumours
Abstract
:1. Introduction
2. Mechanism of Cardiotoxicity
2.1. Anthracyclines
2.2. Fluoropyrimidines
2.3. Platinum-Based Compounds
2.4. Human Epidermal Growth Factor Receptor 2 (HER2) Antagonists
2.5. Immune Checkpoint Inhibitors (ICI)
2.6. Angiogenesis Inhibitors
3. Diagnosis Methods of Chemotherapy-Induced Cardiotoxicity in GI Cancers
3.1. Biomarkers
3.1.1. Troponins
3.1.2. BNP
3.1.3. Other Biomarkers of Use in Detecting Cardiotoxicity
3.2. Echocardiography
3.3. Cardiac Magnetic Resonance Imaging
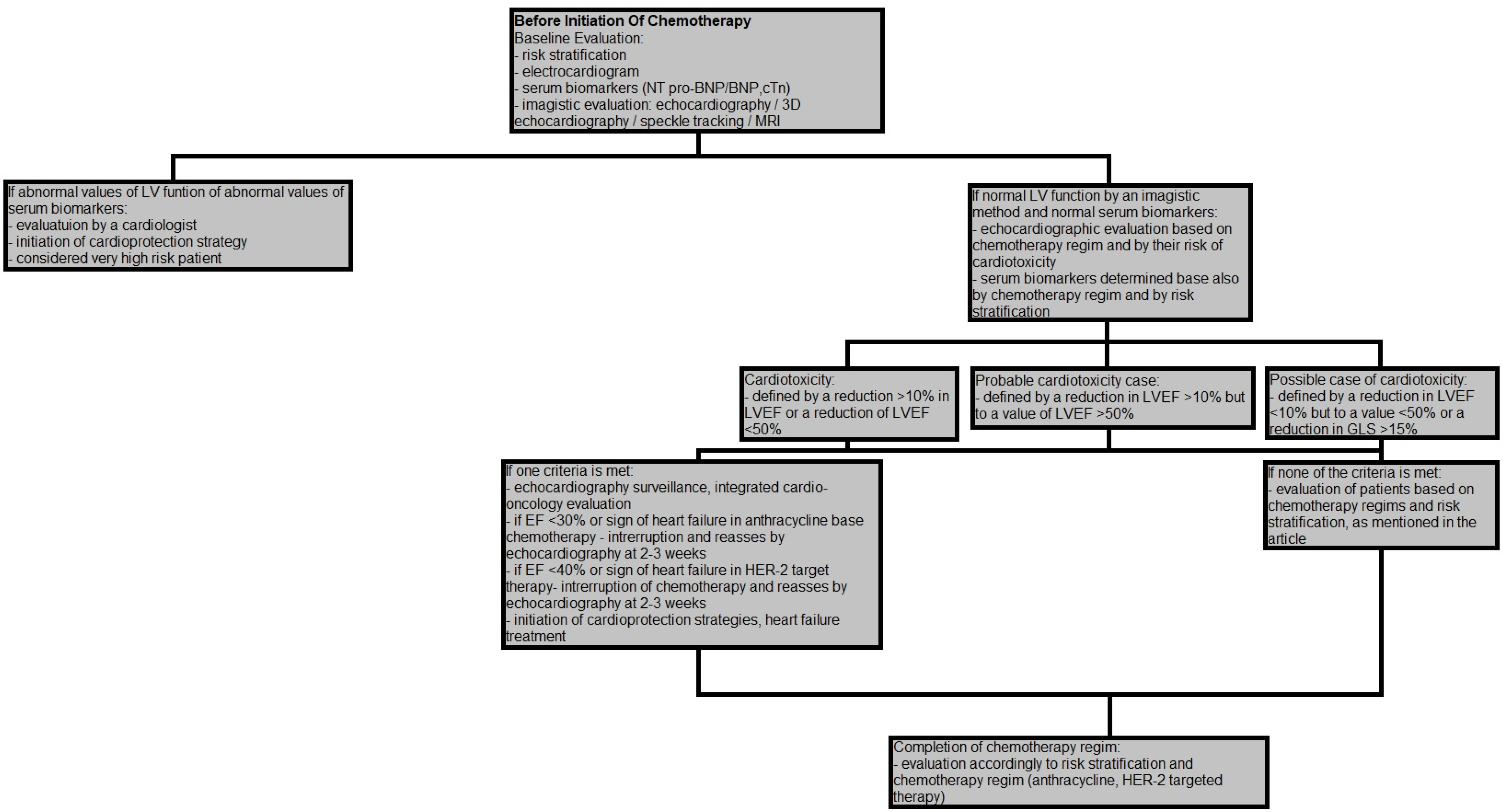
4. Risk Stratification and Surveillance during and after Chemotherapy
5. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arnold, M.; Abnet, C.C.; Neale, R.E.; Vignat, J.; Giovannucci, E.L.; McGlynn, K.A.; Bray, F. Global Burden of 5 Major Types of Gastrointestinal Cancer. Gastroenterology 2020, 159, 335–349.e15. [Google Scholar] [CrossRef]
- Rawla, P.; Sunkara, T.; Barsouk, A. Epidemiology of colorectal cancer: Incidence, mortality, survival, and risk factors. Gastroenterol. Rev. 2019, 14, 89–103. [Google Scholar] [CrossRef]
- Lipshultz, S.E.; Adams, M.J.; Colan, S.D.; Constine, L.S.; Herman, E.H.; Hsu, D.T.; Hudson, M.M.; Kremer, L.C.; Landy, D.C.; Miller, T.L.; et al. Long-term Cardiovascular Toxicity in Children, Adolescents, and Young Adults Who Receive Cancer Therapy: Pathophysiology, Course, Monitoring, Management, Prevention, and Research Directions. Circulation 2013, 128, 1927–1995. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E.; Drazner, M.H.; Fonarow, G.C.; Geraci, S.A.; Horwich, T.; Januzzi, J.L.; et al. 2013 ACCF/AHA Guideline for the Management of Heart Failure. J. Am. Coll. Cardiol. 2013, 62, e147–e239. [Google Scholar] [CrossRef] [Green Version]
- Lenneman, A.J.; Wang, L.; Wigger, M.; Frangoul, H.; Harrell, F.E.; Silverstein, C.; Sawyer, D.B.; Lenneman, C.G. Heart Transplant Survival Outcomes for Adriamycin-Dilated Cardiomyopathy. Am. J. Cardiol. 2013, 111, 609–612. [Google Scholar] [CrossRef] [Green Version]
- Armenian, S.H.; Lacchetti, C.; Barac, A.; Carver, J.; Constine, L.S.; Denduluri, N.; Dent, S.; Douglas, P.S.; Durand, J.-B.; Ewer, M.; et al. Prevention and Monitoring of Cardiac Dysfunction in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol. 2017, 35, 893–911. [Google Scholar] [CrossRef]
- Čelutkienė, J.; Pudil, R.; López-Fernández, T.; Grapsa, J.; Nihoyannopoulos, P.; Bergler-Klein, J.; Cohen-Solal, A.; Farmakis, D.; Tocchetti, C.G.; Haehling, S.; et al. Role of cardiovascular imaging in cancer patients receiving cardiotoxic therapies: A position statement on behalf of the Heart Failure Association (HFA), the European Association of Cardiovascular Imaging (EACVI) and the Cardio-Oncology Council of the European Society of Cardiology (ESC). Eur. J. Heart Fail. 2020, 22, 1504–1524. [Google Scholar] [CrossRef]
- Lyon, A.R.; Dent, S.; Stanway, S.; Earl, H.; Brezden-Masley, C.; Cohen-Solal, A.; Tocchetti, C.G.; Moslehi, J.J.; Groarke, J.D.; Bergler-Klein, J.; et al. Baseline cardiovascular risk assessment in cancer patients scheduled to receive cardiotoxic cancer therapies: A position statement and new risk assessment tools from the Cardio-Oncology Study Group of the Heart Failure Association of the European Society of Cardiology in collaboration with the International Cardio-Oncology Society. Eur. J. Heart Fail. 2020, 22, 1945–1960. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Kong, L.; Tang, M.; Zhang, J.; Zhou, X.; Li, G.; Wang, H.; Fu, F. Protective effect of ocotillol against doxorubicin-induced acute and chronic cardiac injury. Mol. Med. Rep. 2014, 9, 360–364. [Google Scholar] [CrossRef] [Green Version]
- Curigliano, G.; Cardinale, D.; Dent, S.; Criscitiello, C.; Aseyev, O.; Lenihan, D.; Cipolla, C.M. Cardiotoxicity of anticancer treatments: Epidemiology, detection, and management. CA Cancer J. Clin. 2016, 66, 309–325. [Google Scholar] [CrossRef] [Green Version]
- Hamo, C.E.; Bloom, M.W. Getting to the Heart of the Matter: An Overview of Cardiac Toxicity Related to Cancer Therapy. Clin. Med. Insights Cardiol. 2015, 9 (Suppl. 2). [Google Scholar] [CrossRef] [PubMed]
- Moslehi, J.J.; Deininger, M. Tyrosine Kinase Inhibitor–Associated Cardiovascular Toxicity in Chronic Myeloid Leukemia. J. Clin. Oncol. 2015, 33, 4210–4218. [Google Scholar] [CrossRef] [PubMed]
- Gori, T.; Polimeni, A.; Indolfi, C.; Räber, L.; Adriaenssens, T.; Münzel, T. Predictors of stent thrombosis and their implications for clinical practice. Nat. Rev. Cardiol. 2019, 16, 243–256. [Google Scholar] [CrossRef]
- Douxfils, J.; Haguet, H.; Mullier, F.; Chatelain, C.; Graux, C.; Dogné, J.-M. Association Between BCR-ABL Tyrosine Kinase Inhibitors for Chronic Myeloid Leukemia and Cardiovascular Events, Major Molecular Response, and Overall Survival. JAMA Oncol. 2016, 2, 625. [Google Scholar] [CrossRef]
- Hadzijusufovic, E.; Albrecht-Schgoer, K.; Huber, K.; Hoermann, G.; Grebien, F.; Eisenwort, G.; Schgoer, W.; Herndlhofer, S.; Kaun, C.; Theurl, M.; et al. Nilotinib-induced vasculopathy: Identification of vascular endothelial cells as a primary target site. Leukemia 2017, 31, 2388–2397. [Google Scholar] [CrossRef] [Green Version]
- Latifi, Y.; Moccetti, F.; Wu, M.; Xie, A.; Packwood, W.; Qi, Y.; Ozawa, K.; Shentu, W.; Brown, E.; Shirai, T.; et al. Thrombotic microangiopathy as a cause of cardiovascular toxicity from the BCR-ABL1 tyrosine kinase inhibitor ponatinib. Blood 2019, 133, 1597–1606. [Google Scholar] [CrossRef] [Green Version]
- Fradley, M.G.; Gliksman, M.; Emole, J.; Viganego, F.; Rhea, I.; Welter-Frost, A.; Armanious, M.; Lee, D.H.; Walko, C.; Shah, B.; et al. Rates and Risk of Atrial Arrhythmias in Patients Treated with Ibrutinib Compared with Cytotoxic Chemotherapy. Am. J. Cardiol. 2019, 124, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Guha, A.; Derbala, M.H.; Zhao, Q.; Wiczer, T.E.; Woyach, J.A.; Byrd, J.C.; Awan, F.T.; Addison, D. Ventricular Arrhythmias Following Ibrutinib Initiation for Lymphoid Malignancies. J. Am. Coll. Cardiol. 2018, 72, 697–698. [Google Scholar] [CrossRef]
- Mordente, A.; Meucci, E.; Martorana, G.E.; Tavian, D.; Silvestrini, A. Topoisomerases and Anthracyclines: Recent Advances and Perspectives in Anticancer Therapy and Prevention of Cardiotoxicity. Curr. Med. Chem. 2017, 24. [Google Scholar] [CrossRef]
- Aminkeng, F.; Ross, C.J.D.; Rassekh, S.R.; Rieder, M.J.; Bhavsar, A.P.; Sanatani, S.; Bernstein, D.; Hayden, M.R.; Amstutz, U.; Carleton, B.C. Pharmacogenomic screening for anthracycline-induced cardiotoxicity in childhood cancer. Br. J. Clin. Pharmacol. 2017, 83, 1143–1145. [Google Scholar] [CrossRef] [Green Version]
- Couture, L.; Nash, J.A.; Turgeon, J. The ATP-Binding Cassette Transporters and Their Implication in Drug Disposition: A Special Look at the Heart. Pharmacol. Rev. 2006, 58, 244–258. [Google Scholar] [CrossRef]
- Orogo, A.M.; Gonzalez, E.R.; Kubli, D.A.; Baptista, I.L.; Ong, S.-B.; Prolla, T.A.; Sussman, M.A.; Murphy, A.N.; Gustafsson, Å.B. Accumulation of mitochondrial DNA mutations disrupts cardiac progenitor cell function and reduces survival. J. Biol. Chem. 2017, 292, 11348. [Google Scholar] [CrossRef] [Green Version]
- Lipshultz, S.E.; Cochran, T.R.; Franco, V.I.; Miller, T.L. Treatment-related cardiotoxicity in survivors of childhood cancer. Nat. Rev. Clin. Oncol. 2013, 10, 697–710. [Google Scholar] [CrossRef]
- Cardinale, D.; Colombo, A.; Bacchiani, G.; Tedeschi, I.; Meroni, C.A.; Veglia, F.; Civelli, M.; Lamantia, G.; Colombo, N.; Curigliano, G.; et al. Early Detection of Anthracycline Cardiotoxicity and Improvement with Heart Failure Therapy. Circulation 2015, 131, 1981–1988. [Google Scholar] [CrossRef] [Green Version]
- Kanduri, J.; More, L.A.; Godishala, A.; Asnani, A. Fluoropyrimidine-Associated Cardiotoxicity. Cardiol. Clin. 2019, 37, 399–405. [Google Scholar] [CrossRef]
- Wacker, A.; Lersch, C.; Scherpinski, U.; Reindl, L.; Seyfarth, M. High Incidence of Angina pectoris in Patients Treated with 5-Fluorouracil. Oncology 2003, 65, 108–112. [Google Scholar] [CrossRef] [Green Version]
- Bartelink, H.; Roelofsen, F.; Eschwege, F.; Rougier, P.; Bosset, J.F.; Gonzalez, D.G.; Peiffert, D.; van Glabbeke, M.; Pierart, M. Concomitant radiotherapy and chemotherapy is superior to radiotherapy alone in the treatment of locally advanced anal cancer: Results of a phase III randomized trial of the European Organization for Research and Treatment of Cancer Radiotherapy and Gastro. J. Clin. Oncol. 1997, 15, 2040–2049. [Google Scholar] [CrossRef]
- Curtin, N.J.; Harris, A.L.; Aherne, G.W. Mechanism of cell death following thymidylate synthase inhibition: 2′-deoxyuridine-5′-triphosphate accumulation, DNA damage, and growth inhibition following exposure to CB3717 and dipyridamole. Cancer Res. 1991, 51, 2346–2352. [Google Scholar]
- Layoun, M.E.; Wickramasinghe, C.D.; Peralta, M.V.; Yang, E.H. Fluoropyrimidine-Induced Cardiotoxicity: Manifestations, Mechanisms, and Management. Curr. Oncol. Rep. 2016, 18, 35. [Google Scholar] [CrossRef] [Green Version]
- Atar, A.; Korkmaz, M.E.; Ozin, B. Two cases of coronary vasospasm induced by 5-fluorouracil. Anadolu Kardiyol. Derg. Anatol. J. Cardiol. 2010, 10, 461–462. [Google Scholar] [CrossRef]
- Mosseri, M.; Fingert, H.J.; Varticovski, L.; Chokshi, S.; Isner, J.M. In vitro evidence that myocardial ischemia resulting from 5-fluorouracil chemotherapy is due to protein kinase C-mediated vasoconstriction of vascular smooth muscle. Cancer Res. 1993, 53, 3028–3033. [Google Scholar] [PubMed]
- Jensen, S.A.; Sørensen, J.B. 5-Fluorouracil-based therapy induces endovascular injury having potential significance to development of clinically overt cardiotoxicity. Cancer Chemother. Pharmacol. 2012, 69, 57–64. [Google Scholar] [CrossRef]
- Lker, D.; Muammer Karaayvaz, M. Reduced Antioxidant Defense Capacity in Myocardial Tissue from Guinea Pigs Treated with 5-fluorouracil. J. Toxicol. Environ. Heal. Part A 2000, 59, 585–589. [Google Scholar] [CrossRef]
- Karabay, C.; Gecmen, C.; Aung, S.; Guler, A.; Candan, O.; Batgerel, U.; Kalayci, A.; Kirma, C. Is 5-fluorouracil-induced vasospasm a Kounis syndrome? A diagnostic challenge. Perfusion 2011, 26, 542–545. [Google Scholar] [CrossRef]
- Dugbartey, G.J.; Peppone, L.J.; de Graaf, I.A.M. An integrative view of cisplatin-induced renal and cardiac toxicities: Molecular mechanisms, current treatment challenges and potential protective measures. Toxicology 2016, 371, 58–66. [Google Scholar] [CrossRef] [Green Version]
- Santandreu, F.M.; Roca, P.; Oliver, J. Uncoupling protein-2 knockdown mediates the cytotoxic effects of cisplatin. Free Radic. Biol. Med. 2010, 49, 658–666. [Google Scholar] [CrossRef]
- Ma, H.; Jones, K.R.; Guo, R.; Xu, P.; Shen, Y.; Ren, J. Cisplatin compromises myocardial contractile function and mitochondrial ultrastructure: Role of endoplasmic reticulum stress. Clin. Exp. Pharmacol. Physiol. 2010, 37, 460–465. [Google Scholar] [CrossRef]
- Pretnar-Oblak, J.; Zaletel, M.; Jagodic, M.; Zaletel, M. Thrombosis of Internal Carotid Artery after Cisplatin-Based Chemotherapy. Eur. Neurol. 2007, 57, 109–110. [Google Scholar] [CrossRef] [PubMed]
- Glendenning, J.L.; Barbachano, Y.; Norman, A.R.; Dearnaley, D.P.; Horwich, A.; Huddart, R.A. Long-term neurologic and peripheral vascular toxicity after chemotherapy treatment of testicular cancer. Cancer 2010. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.F.; Yadav, N.U.; Lung, B.Y.; Eaton, A.A.; Thaler, H.T.; Hudis, C.A.; Dang, C.T.; Steingart, R.M. Trastuzumab interruption and treatment-induced cardiotoxicity in early HER2-positive breast cancer. Breast Cancer Res. Treat. 2015, 149, 489–495. [Google Scholar] [CrossRef] [Green Version]
- Takegawa, N.; Yonesaka, K. HER2 as an Emerging Oncotarget for Colorectal Cancer Treatment After Failure of Anti-Epidermal Growth Factor Receptor Therapy. Clin. Colorectal Cancer 2017, 16, 247–251. [Google Scholar] [CrossRef]
- Slamon, D.J.; Leyland-Jones, B.; Shak, S.; Fuchs, H.; Paton, V.; Bajamonde, A.; Fleming, T.; Eiermann, W.; Wolter, J.; Pegram, M.; et al. Use of Chemotherapy plus a Monoclonal Antibody against HER2 for Metastatic Breast Cancer That Overexpresses HER2. N. Engl. J. Med. 2001, 344, 783–792. [Google Scholar] [CrossRef]
- Swain, S.M.; Baselga, J.; Kim, S.-B.; Ro, J.; Semiglazov, V.; Campone, M.; Ciruelos, E.; Ferrero, J.-M.; Schneeweiss, A.; Heeson, S.; et al. Pertuzumab, Trastuzumab, and Docetaxel in HER2-Positive Metastatic Breast Cancer. N. Engl. J. Med. 2015, 372, 724–734. [Google Scholar] [CrossRef] [Green Version]
- Odiete, O.; Hill, M.F.; Sawyer, D.B. Neuregulin in Cardiovascular Development and Disease. Circ. Res. 2012, 111, 1376–1385. [Google Scholar] [CrossRef] [Green Version]
- Crone, S.A.; Zhao, Y.-Y.; Fan, L.; Gu, Y.; Minamisawa, S.; Liu, Y.; Peterson, K.L.; Chen, J.; Kahn, R.; Condorelli, G.; et al. ErbB2 is essential in the prevention of dilated cardiomyopathy. Nat. Med. 2002, 8, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Hedhli, N.; Huang, Q.; Kalinowski, A.; Palmeri, M.; Hu, X.; Russell, R.R.; Russell, K.S. Endothelium-Derived Neuregulin Protects the Heart Against Ischemic Injury. Circulation 2011, 123, 2254–2262. [Google Scholar] [CrossRef] [Green Version]
- Mohan, N.; Shen, Y.; Endo, Y.; ElZarrad, M.K.; Wu, W.J. Trastuzumab, but not pertuzumab, dysregulates HER2 signaling to mediate inhibition of autophagy and increase in reactive oxygen species production in human cardiomyocytes. Mol. Cancer Ther. 2016, 15, 1321–1331. [Google Scholar] [CrossRef] [Green Version]
- Kitani, T.; Ong, S.-G.; Lam, C.K.; Rhee, J.-W.; Zhang, J.Z.; Oikonomopoulos, A.; Ma, N.; Tian, L.; Lee, J.; Telli, M.L.; et al. Human-Induced Pluripotent Stem Cell Model of Trastuzumab-Induced Cardiac Dysfunction in Patients with Breast Cancer. Circulation 2019, 139, 2451–2465. [Google Scholar] [CrossRef]
- Robert, C.; Thomas, L.; Bondarenko, I.; O’Day, S.; Weber, J.; Garbe, C.; Lebbe, C.; Baurain, J.-F.; Testori, A.; Grob, J.-J.; et al. Ipilimumab plus Dacarbazine for Previously Untreated Metastatic Melanoma. N. Engl. J. Med. 2011, 364, 2517–2526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Love, V.A.; Grabie, N.; Duramad, P.; Stavrakis, G.; Sharpe, A.; Lichtman, A. CTLA-4 Ablation and Interleukin-12–Driven Differentiation Synergistically Augment Cardiac Pathogenicity of Cytotoxic T Lymphocytes. Circ. Res. 2007, 101, 248–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yun, S.; Vincelette, N.D.; Mansour, I.; Hariri, D.; Motamed, S. Late Onset Ipilimumab-Induced Pericarditis and Pericardial Effusion: A Rare but Life Threatening Complication. Case Rep. Oncol. Med. 2015, 2015, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, S.S.; Fradley, M.G.; Cohen, J.V.; Nohria, A.; Reynolds, K.L.; Heinzerling, L.M.; Sullivan, R.J.; Damrongwatanasuk, R.; Chen, C.L.; Gupta, D.; et al. Myocarditis in Patients Treated with Immune Checkpoint Inhibitors. J. Am. Coll. Cardiol. 2018, 71, 1755–1764. [Google Scholar] [CrossRef]
- Escudier, M.; Cautela, J.; Malissen, N.; Ancedy, Y.; Orabona, M.; Pinto, J.; Monestier, S.; Grob, J.-J.; Scemama, U.; Jacquier, A.; et al. Clinical Features, Management, and Outcomes of Immune Checkpoint Inhibitor–Related Cardiotoxicity. Circulation 2017, 136, 2085–2087. [Google Scholar] [CrossRef] [PubMed]
- Moslehi, J.J.; Salem, J.-E.; Sosman, J.A.; Lebrun-Vignes, B.; Johnson, D.B. Increased reporting of fatal immune checkpoint inhibitor-associated myocarditis. Lancet 2018, 391, 933. [Google Scholar] [CrossRef] [Green Version]
- Lees, C.; Yazdan-Ashoori, P.; Jerzak, K.J.; Gandhi, S. Takotsubo Cardiomyopathy During Anti-HER2 Therapy for Metastatic Breast Cancer. Oncologist 2019, 24, e80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ylä-Herttuala, S.; Rissanen, T.T.; Vajanto, I.; Hartikainen, J. Vascular Endothelial Growth Factors. J. Am. Coll. Cardiol. 2007, 49, 1015–1026. [Google Scholar] [CrossRef] [Green Version]
- Sugrue, M.M.; Yi, J.; Purdie, D.; Dong, W.; Grothey, A.; Kozloff, M. Serious arterial thromboembolic events (sATE) in patients (pts) with metastatic colorectal cancer (mCRC) treated with bevacizumab (BV): Results from the BRiTE registry. J. Clin. Oncol. 2007, 25, 4136. [Google Scholar] [CrossRef]
- Chintalgattu, V.; Ai, D.; Langley, R.R.; Zhang, J.; Bankson, J.A.; Shih, T.L.; Reddy, A.K.; Coombes, K.R.; Daher, I.N.; Pati, S.; et al. Cardiomyocyte PDGFR-β signaling is an essential component of the mouse cardiac response to load-induced stress. J. Clin. Investig. 2010, 120, 472–484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thavendiranathan, P.; Wintersperger, B.J.; Flamm, S.D.; Marwick, T.H. Cardiac MRI in the Assessment of Cardiac Injury and Toxicity from Cancer Chemotherapy. Circ. Cardiovasc. Imaging 2013, 6, 1080–1091. [Google Scholar] [CrossRef]
- Zuo, P.-Y.; Chen, X.-L.; Liu, Y.-W.; Xiao, C.-L.; Liu, C.-Y. Increased Risk of Cerebrovascular Events in Patients with Cancer Treated with Bevacizumab: A Meta-Analysis. PLoS ONE 2014, 9, e102484. [Google Scholar] [CrossRef] [Green Version]
- Zhang, P.; Hu, X.; Xu, X.; Fassett, J.; Zhu, G.; Viollet, B.; Xu, W.; Wiczer, B.; Bernlohr, D.A.; Bache, R.J.; et al. AMP Activated Protein Kinase-α2 Deficiency Exacerbates Pressure-Overload–Induced Left Ventricular Hypertrophy and Dysfunction in Mice. Hypertension 2008, 52, 918–924. [Google Scholar] [CrossRef] [Green Version]
- Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clin. Pharmacol. Ther. 2001, 69, 89–95. [CrossRef] [PubMed]
- Makavos, G.; Ikonomidis, I.; Palios, J.; Rigopoulos, A.; Katogiannis, K.; Parissis, J.; Paraskevaidis, I.; Noutsias, M. Cardiac imaging in cardiotoxicity: A focus on clinical practice. Heart Fail. Rev. 2020. [Google Scholar] [CrossRef]
- Luis Zamorano, J.; Lancellotti, P.; Rodriguez Muñ oz, D.; Aboyans, V.; Asteggiano, R.; Galderisi, M.; Habib, G.; Lenihan, D.J.; Lip, G.Y.H.; Lyon, A.R.; et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 36, 2768–2801. [Google Scholar] [CrossRef] [PubMed]
- Cardinale, D.; Sandri, M.T.; Colombo, A.; Colombo, N.; Boeri, M.; Lamantia, G.; Civelli, M.; Peccatori, F.; Martinelli, G.; Fiorentini, C.; et al. Prognostic Value of Troponin I in Cardiac Risk Stratification of Cancer Patients Undergoing High-Dose Chemotherapy. Circulation 2004, 109, 2749–2754. [Google Scholar] [CrossRef] [Green Version]
- Jones, M.; O’Gorman, P.; Kelly, C.; Mahon, N.; Fitzgibbon, M.C. High-sensitive cardiac troponin-I facilitates timely detection of subclinical anthracycline-mediated cardiac injury. Ann. Clin. Biochem. Int. J. Lab. Med. 2017, 54, 149–157. [Google Scholar] [CrossRef]
- Garrone, O.; Crosetto, N.; Lo Nigro, C.; Catzeddu, T.; Vivenza, D.; Monteverde, M.; Merlano, M.; Feola, M. Prediction of Anthracycline Cardiotoxicity after Chemotherapy by Biomarkers Kinetic Analysis. Cardiovasc. Toxicol. 2012, 12, 135–142. [Google Scholar] [CrossRef]
- Sawaya, H.; Sebag, I.A.; Plana, J.C.; Januzzi, J.L.; Ky, B.; Tan, T.C.; Cohen, V.; Banchs, J.; Carver, J.R.; Wiegers, S.E.; et al. Assessment of Echocardiography and Biomarkers for the Extended Prediction of Cardiotoxicity in Patients Treated with Anthracyclines, Taxanes, and Trastuzumab. Circ. Cardiovasc. Imaging 2012, 5, 596–603. [Google Scholar] [CrossRef] [Green Version]
- Kitayama, H.; Kondo, T.; Sugiyama, J.; Kurimoto, K.; Nishino, Y.; Kawada, M.; Hirayama, M.; Tsuji, Y. High-sensitive troponin T assay can predict anthracycline- and trastuzumab-induced cardiotoxicity in breast cancer patients. Breast Cancer 2017, 24, 774–782. [Google Scholar] [CrossRef] [PubMed]
- Ky, B.; Putt, M.; Sawaya, H.; French, B.; Januzzi, J.L.; Sebag, I.A.; Plana, J.C.; Cohen, V.; Banchs, J.; Carver, J.R.; et al. Early Increases in Multiple Biomarkers Predict Subsequent Cardiotoxicity in Patients with Breast Cancer Treated with Doxorubicin, Taxanes, and Trastuzumab. J. Am. Coll. Cardiol. 2014, 63, 809–816. [Google Scholar] [CrossRef] [Green Version]
- Morris, P.G.; Chen, C.; Steingart, R.; Fleisher, M.; Lin, N.; Moy, B.; Come, S.; Sugarman, S.; Abbruzzi, A.; Lehman, R.; et al. Troponin I and C-Reactive Protein Are Commonly Detected in Patients with Breast Cancer Treated with Dose-Dense Chemotherapy Incorporating Trastuzumab and Lapatinib. Clin. Cancer Res. 2011, 17, 3490–3499. [Google Scholar] [CrossRef] [Green Version]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.-C.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lenihan, D.J.; Stevens, P.L.; Massey, M.; Plana, J.C.; Araujo, D.M.; Fanale, M.A.; Fayad, L.E.; Fisch, M.J.; Yeh, E.T.H. The Utility of Point-of-Care Biomarkers to Detect Cardiotoxicity During Anthracycline Chemotherapy: A Feasibility Study. J. Card. Fail. 2016, 22, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Skovgaard, D.; Hasbak, P.; Kjaer, A. BNP Predicts Chemotherapy-Related Cardiotoxicity and Death: Comparison with Gated Equilibrium Radionuclide Ventriculography. PLoS ONE 2014, 9, e96736. [Google Scholar] [CrossRef]
- De Iuliis, F.; Salerno, G.; Taglieri, L.; De Biase, L.; Lanza, R.; Cardelli, P.; Scarpa, S. Serum biomarkers evaluation to predict chemotherapy-induced cardiotoxicity in breast cancer patients. Tumor Biol. 2016, 37, 3379–3387. [Google Scholar] [CrossRef]
- Putt, M.; Hahn, V.S.; Januzzi, J.L.; Sawaya, H.; Sebag, I.A.; Plana, J.C.; Picard, M.H.; Carver, J.R.; Halpern, E.F.; Kuter, I.; et al. Longitudinal changes in multiple biomarkers are associated with cardiotoxicity in breast cancer patients treated with doxorubicin, taxanes, and trastuzumab. Clin. Chem. 2015, 61, 1164–1172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frères, P.; Bouznad, N.; Servais, L.; Josse, C.; Wenric, S.; Poncin, A.; Thiry, J.; Moonen, M.; Oury, C.; Lancellotti, P.; et al. Variations of circulating cardiac biomarkers during and after anthracycline-containing chemotherapy in breast cancer patients. BMC Cancer 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Dobson, R.; Ghosh, A.K.; Ky, B.; Marwick, T.; Stout, M.; Harkness, A.; Steeds, R.; Robinson, S.; Oxborough, D.; Adlam, D.; et al. British Society for Echocardiography and British Cardio-Oncology Society guideline for transthoracic echocardiographic assessment of adult cancer patients receiving anthracyclines and/or trastuzumab. Echo. Res. Pract. 2021, 8, G1–G18. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Hear. J. Cardiovasc. Imaging 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Yu, E.H.C.; Sloggett, C.E.; Iwanochko, R.M.; Rakowski, H.; Siu, S.C. Feasibility and Accuracy of Left Ventricular Volumes and Ejection Fraction Determination by Fundamental, Tissue Harmonic, and Intravenous Contrast Imaging in Difficult-to-Image Patients. J. Am. Soc. Echocardiogr. 2000, 13, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Thavendiranathan, P.; Grant, A.D.; Negishi, T.; Plana, J.C.; Popović, Z.B.; Marwick, T.H. Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: Application to patients undergoing cancer chemotherapy. J. Am. Coll. Cardiol. 2013, 61, 77–84. [Google Scholar] [CrossRef] [Green Version]
- Turan, T.; Agac, M.T.; Aykan, A.Ç.; Kul, S.; Akyüz, A.R.; Gökdeniz, T.; Gül, İ.; Cengiz, E.; Boyacı, F.; Erkan, H.; et al. Usefulness of Heart-Type Fatty Acid-Binding Protein and Myocardial Performance Index for Early Detection of 5-Fluorouracil Cardiotoxicity. Angiology 2017, 68, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Eidem, B.W.; Sapp, B.G.; Suarez, C.R.; Cetta, F. Usefulness of the myocardial performance index for early detection of anthracycline-induced cardiotoxicity in children. Am. J. Cardiol. 2001, 87, 1120–1122. [Google Scholar] [CrossRef]
- Yu, A.F.; Moskowitz, C.S.; Lee Chuy, K.; Yang, J.; Dang, C.T.; Liu, J.E.; Oeffinger, K.C.; Steingart, R.M. Cardiotoxicity Surveillance and Risk of Heart Failure During HER2 Targeted Therapy. JACC Cardio Oncol. 2020, 2, 166–175. [Google Scholar] [CrossRef]
- Kim, E.K.; Cho, J.; Kim, J.-Y.; Chang, S.-A.; Park, S.-J.; Choi, J.O.; Lee, S.C.; Ahn, J.S.; Park, S.W.; Im, Y.-H.; et al. Early Decline in Left Ventricular Ejection Fraction Can Predict Trastuzumab-Related Cardiotoxicity in Patients with Breast Cancer: A Study Using 13 Years of Registry Data. Cancer Res. Treat. 2019, 51, 727–736. [Google Scholar] [CrossRef]
- Stoddard, M.F.; Seeger, J.; Liddell, N.E.; Hadley, T.J.; Sullivan, D.M.; Kupersmith, J. Prolongation of isovolumetric relaxation time as assessed by Doppler echocardiography predicts doxorubicin-induced systolic dysfunction in humans. J. Am. Coll. Cardiol. 1992, 20, 62–69. [Google Scholar] [CrossRef] [Green Version]
- Tassan-Mangina, S.; Codorean, D.; Metivier, M.; Costa, B.; Himberlin, C.; Jouannaud, C.; Blaise, A.M.; Elaerts, J.; Nazeyrollas, P. Tissue Doppler imaging and conventional echocardiography after anthracycline treatment in adults: Early and late alterations of left ventricular function during a prospective study. Eur. J. Echocardiogr. 2006, 7, 141–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lange, S.A.; Ebner, B.; Wess, A.; Kögel, M.; Gajda, M.; Hitschold, T.; Jung, J. Echocardiography signs of early cardiac impairment in patients with breast cancer and trastuzumab therapy. Clin. Res. Cardiol. 2012, 101, 415–426. [Google Scholar] [CrossRef]
- Armstrong, G.T.; Plana, J.C.; Zhang, N.; Srivastava, D.; Green, D.M.; Ness, K.K.; Daniel Donovan, F.; Metzger, M.L.; Arevalo, A.; Durand, J.-B.; et al. Screening Adult Survivors of Childhood Cancer for Cardiomyopathy: Comparison of Echocardiography and Cardiac Magnetic Resonance Imaging. J. Clin. Oncol. 2012, 30, 2876–2884. [Google Scholar] [CrossRef]
- Walker, J.; Bhullar, N.; Fallah-Rad, N.; Lytwyn, M.; Golian, M.; Fang, T.; Summers, A.R.; Singal, P.K.; Barac, I.; Kirkpatrick, I.D.; et al. Role of Three-Dimensional Echocardiography in Breast Cancer: Comparison with Two-Dimensional Echocardiography, Multiple-Gated Acquisition Scans, and Cardiac Magnetic Resonance Imaging. J. Clin. Oncol. 2010, 28, 3429–3436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toro-Salazar, O.H.; Ferranti, J.; Lorenzoni, R.; Walling, S.; Mazur, W.; Raman, S.V.; Davey, B.T.; Gillan, E.; O’Loughlin, M.; Klas, B.; et al. Feasibility of Echocardiographic Techniques to Detect Subclinical Cancer Therapeutics–Related Cardiac Dysfunction among High-Dose Patients When Compared with Cardiac Magnetic Resonance Imaging. J. Am. Soc. Echocardiogr. 2016, 29, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Kleijn, S.A.; Aly, M.F.A.; Terwee, C.B.; van Rossum, A.C.; Kamp, O. Three-Dimensional Speckle Tracking Echocardiography for Automatic Assessment of Global and Regional Left Ventricular Function Based on Area Strain. J. Am. Soc. Echocardiogr. 2011, 24, 314–321. [Google Scholar] [CrossRef] [Green Version]
- Miyoshi, T.; Tanaka, H.; Kaneko, A.; Tatsumi, K.; Matsumoto, K.; Minami, H.; Kawai, H.; Hirata, K. Left ventricular endocardial dysfunction in patients with preserved ejection fraction after receiving anthracycline. Echocardiography 2014, 31, 848–857. [Google Scholar] [CrossRef]
- Mor-Avi, V.; Patel, M.B.; Maffessanti, F.; Singh, A.; Medvedofsky, D.; Zaidi, S.J.; Mediratta, A.; Narang, A.; Nazir, N.; Kachenoura, N.; et al. Fusion of Three-Dimensional Echocardiographic Regional Myocardial Strain with Cardiac Computed Tomography for Noninvasive Evaluation of the Hemodynamic Impact of Coronary Stenosis in Patients with Chest Pain. J. Am. Soc. Echocardiogr. 2018, 31, 664–673. [Google Scholar] [CrossRef]
- Zhang, L.; Awadalla, M.; Mahmood, S.S.; Groarke, J.D.; Nohria, A.; Liu, S.; Hassan, M.Z.O.; Cohen, J.V.; Jones-O’Connor, M.; Murphy, S.P.T.; et al. Late Gadolinium Enhancement in Patients with Myocarditis from Immune Checkpoint Inhibitors. J. Am. Coll. Cardiol. 2019, 73, 675. [Google Scholar] [CrossRef]
- Motoki, H.; Koyama, J.; Nakazawa, H.; Aizawa, K.; Kasai, H.; Izawa, A.; Tomita, T.; Miyashita, Y.; Kumazaki, S.; Takahashi, M.; et al. Torsion analysis in the early detection of anthracycline-mediated cardiomyopathy. Eur. Heart J. Cardiovasc. Imaging 2012, 13, 95–103. [Google Scholar] [CrossRef]
- Tan, T.C.; Scherrer-Crosbie, M. Assessing the Cardiac Toxicity of Chemotherapeutic Agents: Role of Echocardiography. Curr. Cardiovasc. Imaging Rep. 2012, 5, 403–409. [Google Scholar] [CrossRef] [Green Version]
- McKillop, J.H.; Bristow, M.R.; Goris, M.L.; Billingham, M.E.; Bockemuehl, K. Sensitivity and specificity of radionuclide ejection fractions in doxorubicin cardiotoxicity. Am. Heart J. 1983, 106, 1048–1056. [Google Scholar] [CrossRef]
- Douglas, P.S.; Carr, J.J.; Cerqueira, M.D.; Cummings, J.E.; Gerber, T.C.; Mukherjee, D.; Taylor, A.J. Developing an Action Plan for Patient Radiation Safety in Adult Cardiovascular Medicine. J. Am. Coll. Cardiol. 2012, 59, 1833–1847. [Google Scholar] [CrossRef] [Green Version]
- Civelli, M.; Cardinale, D.; Martinoni, A.; Lamantia, G.; Colombo, N.; Colombo, A.; Gandini, S.; Martinelli, G.; Fiorentini, C.; Cipolla, C.M. Early reduction in left ventricular contractile reserve detected by dobutamine stress echo predicts high-dose chemotherapy-induced cardiac toxicity. Int. J. Cardiol. 2006, 111, 120–126. [Google Scholar] [CrossRef]
- Friedrich, M.G.; Abdel-Aty, H.; Taylor, A.; Schulz-Menger, J.; Messroghli, D.; Dietz, R. The Salvaged Area at Risk in Reperfused Acute Myocardial Infarction as Visualized by Cardiovascular Magnetic Resonance. J. Am. Coll. Cardiol. 2008, 51, 1581–1587. [Google Scholar] [CrossRef] [Green Version]
- Nousiainen, T.; Vanninen, E.; Jantunen, E.; Puustinen, J.; Remes, J.; Rantala, A.; Hartikainen, J. Comparison of echocardiography and radionuclide ventriculography in the follow-up of left ventricular systolic function in adult lymphoma patients during doxorubicin therapy. J. Intern. Med. 2001, 249, 297–303. [Google Scholar] [CrossRef] [Green Version]
- Ferreira de Souza, T.; Quinaglia, A.C.; Silva, T.; Osorio Costa, F.; Shah, R.; Neilan, T.G.; Velloso, L.; Nadruz, W.; Brenelli, F.; Sposito, A.C.; et al. Anthracycline Therapy is Associated with Cardiomyocyte Atrophy and Preclinical Manifestations of Heart Disease. JACC Cardiovasc. Imaging 2018, 11, 1045–1055. [Google Scholar] [CrossRef] [PubMed]
- Carbone, I.; Childs, H.; Aljizeeri, A.; Merchant, N.; Friedrich, M.G. Importance of Reference Muscle Selection in Quantitative Signal Intensity Analysis of T2-Weighted Images of Myocardial Edema Using a T2 Ratio Method. Biomed Res. Int. 2015, 2015, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Farhad, H.; Staziaki, P.V.; Addison, D.; Coelho-Filho, O.R.; Shah, R.V.; Mitchell, R.N.; Szilveszter, B.; Abbasi, S.A.; Kwong, R.Y.; Scherrer-Crosbie, M.; et al. Characterization of the Changes in Cardiac Structure and Function in Mice Treated with Anthracyclines Using Serial Cardiac Magnetic Resonance Imaging. Circ. Cardiovasc. Imaging 2016, 9. [Google Scholar] [CrossRef] [Green Version]
- Sarwar, A.; Shapiro, M.D.; Abbara, S.; Cury, R.C. Cardiac Magnetic Resonance Imaging for the Evaluation of Ventricular Function. Semin. Roentgenol. 2008, 43, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Drafts, B.C.; Twomley, K.M.; D’Agostino, R.; Lawrence, J.; Avis, N.; Ellis, L.R.; Thohan, V.; Jordan, J.; Melin, S.A.; Torti, F.M.; et al. Low to Moderate Dose Anthracycline-Based Chemotherapy Is Associated with Early Noninvasive Imaging Evidence of Subclinical Cardiovascular Disease. JACC Cardiovasc. Imaging 2013, 6, 877–885. [Google Scholar] [CrossRef] [Green Version]
- Neilan, T.G.; Pena-Herrera, D.; Coelho-Filho, O.R.; Jerosch-Herold, M.; Moslehi, J.; Kwong, R. Left ventricular mass by cardiac magnetic resonance imaging and adverse cardiovascular outcomes in patients treated with anthracycline-based chemotherapy. J. Cardiovasc. Magn. Reson. 2012, 14, O30. [Google Scholar] [CrossRef] [Green Version]
- Jordan, J.H.; Castellino, S.M.; Meléndez, G.C.; Klepin, H.D.; Ellis, L.R.; Lamar, Z.; Vasu, S.; Kitzman, D.W.; Ntim, W.O.; Brubaker, P.H.; et al. Left Ventricular Mass Change After Anthracycline Chemotherapy. Circ. Hear. Fail. 2018, 11. [Google Scholar] [CrossRef]
- Calleja, A.; Poulin, F.; Khorolsky, C.; Shariat, M.; Bedard, P.L.; Amir, E.; Rakowski, H.; McDonald, M.; Delgado, D.; Thavendiranathan, P. Right Ventricular Dysfunction in Patients Experiencing Cardiotoxicity during Breast Cancer Therapy. J. Oncol. 2015, 2015, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ghio, S.; Guazzi, M.; Scardovi, A.B.; Klersy, C.; Clemenza, F.; Carluccio, E.; Temporelli, P.L.; Rossi, A.; Faggiano, P.; Traversi, E.; et al. Different correlates but similar prognostic implications for right ventricular dysfunction in heart failure patients with reduced or preserved ejection fraction. Eur. J. Heart Fail. 2017, 19, 873–879. [Google Scholar] [CrossRef] [Green Version]
- Cojan-Minzat, B.O.; Zlibut, A.; Agoston-Coldea, L. Non-ischemic dilated cardiomyopathy and cardiac fibrosis. Heart Fail. Rev. 2020. [Google Scholar] [CrossRef] [PubMed]
- Cojan-Minzat, B.O.; Zlibut, A.; Muresan, I.D.; Cionca, C.; Horvat, D.; Kiss, E.; Revnic, R.; Florea, M.; Ciortea, R.; Agoston-Coldea, L. Left Ventricular Geometry and Replacement Fibrosis Detected by cMRI Are Associated with Major Adverse Cardiovascular Events in Nonischemic Dilated Cardiomyopathy. J. Clin. Med. 2020, 9, 1997. [Google Scholar] [CrossRef]
- Ylänen, K.; Poutanen, T.; Savikurki-Heikkilä, P.; Rinta-Kiikka, I.; Eerola, A.; Vettenranta, K. Cardiac Magnetic Resonance Imaging in the Evaluation of the Late Effects of Anthracyclines Among Long-Term Survivors of Childhood Cancer. J. Am. Coll. Cardiol. 2013, 61, 1539–1547. [Google Scholar] [CrossRef] [Green Version]
- Neilan, T.G.; Coelho-Filho, O.R.; Shah, R.V.; Feng, J.H.; Pena-Herrera, D.; Mandry, D.; Pierre-Mongeon, F.; Heydari, B.; Francis, S.A.; Moslehi, J.; et al. Myocardial Extracellular Volume by Cardiac Magnetic Resonance Imaging in Patients Treated with Anthracycline-Based Chemotherapy. Am. J. Cardiol. 2013, 111, 717–722. [Google Scholar] [CrossRef] [Green Version]
- Lawley, C.; Wainwright, C.; Segelov, E.; Lynch, J.; Beith, J.; Mccrohon, J. Pilot study evaluating the role of cardiac magnetic resonance imaging in monitoring adjuvant trastuzumab therapy for breast cancer. Asia. Pac. J. Clin. Oncol. 2012, 8, 95–100. [Google Scholar] [CrossRef]
- Wassmuth, R.; Lentzsch, S.; Erdbruegger, U.; Schulz-Menger, J.; Doerken, B.; Dietz, R.; Friedrich, M.G. Subclinical cardiotoxic effects of anthracyclines as assessed by magnetic resonance imaging—A pilot study. Am. Heart J. 2001, 141, 1007–1013. [Google Scholar] [CrossRef]
- Coelho-Filho, O.R.; Shah, R.V.; Neilan, T.G.; Mitchell, R.; Moreno, H.; Kwong, R.; Jerosch-Herold, M. Cardiac Magnetic Resonance Assessment of Interstitial Myocardial Fibrosis and Cardiomyocyte Hypertrophy in Hypertensive Mice Treated with Spironolactone. J. Am. Heart Assoc. 2014, 3. [Google Scholar] [CrossRef] [Green Version]
- Vita, T.; Gräni, C.; Abbasi, S.A.; Neilan, T.G.; Rowin, E.; Kaneko, K.; Coelho-Filho, O.; Watanabe, E.; Mongeon, F.-P.; Farhad, H.; et al. Comparing CMR Mapping Methods and Myocardial Patterns Toward Heart Failure Outcomes in Nonischemic Dilated Cardiomyopathy. JACC Cardiovasc. Imaging 2019, 12, 1659–1669. [Google Scholar] [CrossRef]
- Coelho-Filho, O.R.; Shah, R.V.; Mitchell, R.; Neilan, T.G.; Moreno, H.; Simonson, B.; Kwong, R.; Rosenzweig, A.; Das, S.; Jerosch-Herold, M. Quantification of Cardiomyocyte Hypertrophy by Cardiac Magnetic Resonance. Circulation 2013, 128, 1225–1233. [Google Scholar] [CrossRef] [Green Version]
- Friedrich, M.G.; Sechtem, U.; Schulz-Menger, J.; Holmvang, G.; Alakija, P.; Cooper, L.T.; White, J.A.; Abdel-Aty, H.; Gutberlet, M.; Prasad, S.; et al. Cardiovascular Magnetic Resonance in Myocarditis: A JACC White Paper. J. Am. Coll. Cardiol. 2009, 53, 1475–1487. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Awadalla, M.; Mahmood, S.S.; Nohria, A.; Hassan, M.Z.O.; Thuny, F.; Zlotoff, D.A.; Murphy, S.P.; Stone, J.R.; Golden, D.L.A.; et al. Cardiovascular magnetic resonance in immune checkpoint inhibitor-associated myocarditis. Eur. Heart J. 2020, 41, 1733–1743. [Google Scholar] [CrossRef] [PubMed]
- Ganatra, S.; Neilan, T.G. Immune Checkpoint Inhibitor-Associated Myocarditis. Oncologist 2018, 23, 879–886. [Google Scholar] [CrossRef] [Green Version]
- Galán-Arriola, C.; Lobo, M.; Vílchez-Tschischke, J.P.; López, G.J.; de Molina-Iracheta, A.; Pérez-Martínez, C.; Agüero, J.; Fernández-Jiménez, R.; Martín-García, A.; Oliver, E.; et al. Serial Magnetic Resonance Imaging to Identify Early Stages of Anthracycline-Induced Cardiotoxicity. J. Am. Coll. Cardiol. 2019, 73, 779–791. [Google Scholar] [CrossRef]
- Pudil, R.; Mueller, C.; Čelutkienė, J.; Henriksen, P.A.; Lenihan, D.; Dent, S.; Barac, A.; Stanway, S.; Moslehi, J.; Suter, T.M.; et al. Role of serum biomarkers in cancer patients receiving cardiotoxic cancer therapies: A position statement from the Cardio-Oncology Study Group of theHeart Failure Association and the Cardio-Oncology Council of the European Socie. Eur. J. Heart Fail. 2020, 22, 1966–1983. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radulescu, L.M.; Radulescu, D.; Ciuleanu, T.-E.; Crisan, D.; Buzdugan, E.; Romitan, D.-M.; Buzoianu, A.D. Cardiotoxicity Associated with Chemotherapy Used in Gastrointestinal Tumours. Medicina 2021, 57, 806. https://doi.org/10.3390/medicina57080806
Radulescu LM, Radulescu D, Ciuleanu T-E, Crisan D, Buzdugan E, Romitan D-M, Buzoianu AD. Cardiotoxicity Associated with Chemotherapy Used in Gastrointestinal Tumours. Medicina. 2021; 57(8):806. https://doi.org/10.3390/medicina57080806
Chicago/Turabian StyleRadulescu, Liliana Maria, Dan Radulescu, Tudor-Eliade Ciuleanu, Dana Crisan, Elena Buzdugan, Dragos-Mihai Romitan, and Anca Dana Buzoianu. 2021. "Cardiotoxicity Associated with Chemotherapy Used in Gastrointestinal Tumours" Medicina 57, no. 8: 806. https://doi.org/10.3390/medicina57080806
APA StyleRadulescu, L. M., Radulescu, D., Ciuleanu, T.-E., Crisan, D., Buzdugan, E., Romitan, D.-M., & Buzoianu, A. D. (2021). Cardiotoxicity Associated with Chemotherapy Used in Gastrointestinal Tumours. Medicina, 57(8), 806. https://doi.org/10.3390/medicina57080806





