The Use of Virtual Therapy in Cardiac Rehabilitation of Female Patients with Heart Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Outcome Measures
2.4. Data Analysis
3. Results
3.1. Participants Characteristics
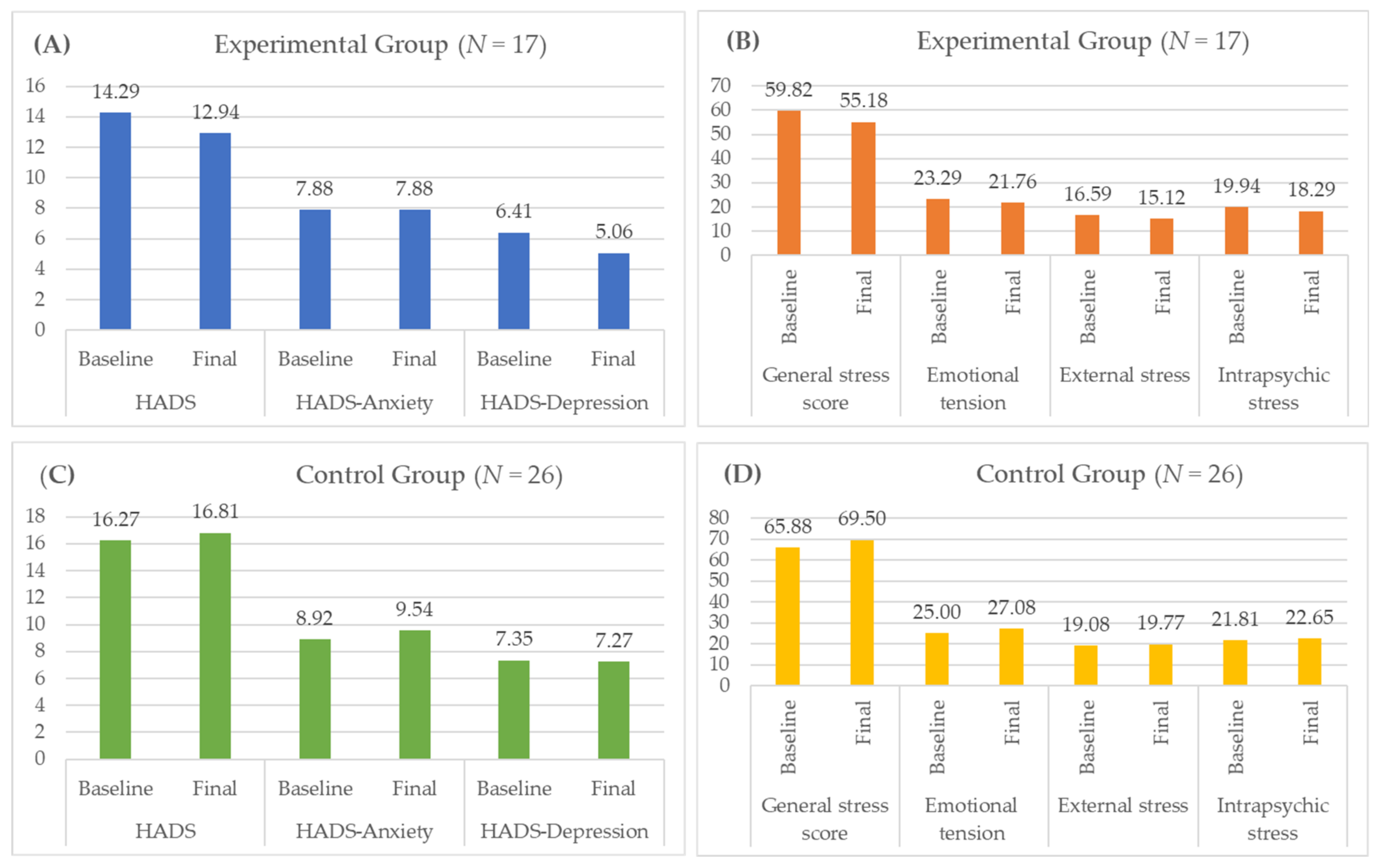
3.2. Results for the Mental State in the Studied Groups
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Strzelecki, Z.; Szymborski, J. Incidence and Mortality from Cardiovascular Diseases and the demographic SITUATION of Poland; Rządowa Rada Ludnościowa: Warszawa, Poland, 2015. [Google Scholar]
- Anand, S.S.; Islam, S.; Rosengren, A.; Franzosi, M.G.; Steyn, K.; Yusufali, A.H.; Keltai, M.; Diaz, R.; Rangarajan, S.; Yusuf, S.; et al. Risk factors for myocardial infarction in women and men: Insights from the INTERHEART study. Eur. Heart J. 2008, 29, 932–940. [Google Scholar] [CrossRef] [Green Version]
- Peltzer, S.; Müller, H.; Köstler, U.; Blaschke, K.; Schulz-Nieswandt, F.; Jessen, F.; Albus, C. Quality of health care with regard to detection and treatment of mental disorders in patients with coronary heart disease (MenDis-CHD): Study protocol. BMC Psychol. 2019, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bucciarelli, V.; Caterino, A.L.; Bianco, F.; Caputi, C.G.; Salerni, S.; Sciomer, S.; Maffei, S.; Gallina, S. Depression and cardiovascular disease: The deep blue sea of women’s heart. Trends Cardiovasc. Med. 2020, 30, 170–176. [Google Scholar] [CrossRef]
- Zdrojewski, T.; Rutkowski, M.; Bandosz, P.; Gaciong, Z.; Jędrzejczyk, T.; Solnica, B.; Pencina, M.; Drygas, W.; Wojtyniak, B.; Grodzicki, T.; et al. Prevalence and control of cardiovascular risk factors in Poland. Assumptions and objectives of the NATPOL 2011 Survey. Kardiologia Pol. Pol. Heart J. 2013, 71, 381–392. [Google Scholar] [CrossRef] [Green Version]
- Piwoński, J.; Piwońska, A.; Jędrusik, P.; Stokwiszewski, J.; Rutkowski, M.; Bandosz, P.; Drygas, W.; Zdrojewski, T. Depressive symptoms and cardiovascular diseases in the adult Polish population. Results of the NATPOL2011 study. Kardiol. Pol. 2019, 77, 18–23. [Google Scholar] [CrossRef] [Green Version]
- Steiner, M.; Dunn, E.; Born, L. Hormones and mood: From menarche to menopause and beyond. J. Affect. Disord. 2003, 74, 67–83. [Google Scholar] [CrossRef]
- Saeed, A.; Kampangkaew, J.; Nambi, V. Prevention of Cardiovascular Disease in Women. Methodist DeBakey Cardiovasc. J. 2017, 13, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Cieślik, B.; Mazurek, J.; Rutkowski, S.; Kiper, P.; Turolla, A.; Szczepańska-Gieracha, J. Virtual reality in psychiatric disorders: A systematic review of reviews. Complement. Ther. Med. 2020, 52, 102480. [Google Scholar] [CrossRef] [PubMed]
- Wallach, H.S.; Bar-Zvi, M. Virtual-reality-assisted treatment of flight phobia. Isr. J. Psychiatry Relat. Sci. 2007, 44, 29–32. [Google Scholar]
- Hong, Y.-J.; Kim, H.E.; Jung, Y.H.; Kyeong, S.; Kim, J.-J. Usefulness of the Mobile Virtual Reality Self-Training for Overcoming a Fear of Heights. Cyberpsychol. Behav. Soc. Netw. 2017, 20, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Rothbaum, B.O.; Hodges, L.F.; Kooper, R.; Opdyke, D.; Williford, J.S.; North, M. Effectiveness of computer-generated (virtual reality) graded exposure in the treatment of acrophobia. Am. J. Psychiatry 1995, 152, 626–628. [Google Scholar] [CrossRef] [PubMed]
- Jerdan, S.W.; Grindle, M.; van Woerden, H.C.; Kamel Boulos, M.N. Head-Mounted Virtual Reality and Mental Health: Critical Review of Current Research. JMIR Serious Games 2018, 6, e14. [Google Scholar] [CrossRef] [Green Version]
- Zeng, N.; Pope, Z.; Lee, J.E.; Gao, Z. Virtual Reality Exercise for Anxiety and Depression: A Preliminary Review of Current Research in an Emerging Field. J. Clin. Med. 2018, 7, 42. [Google Scholar] [CrossRef] [Green Version]
- Maples-Keller, J.L.; Bunnell, B.E.; Kim, S.-J.; Rothbaum, B.O. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv. Rev. Psychiatry 2017, 25, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Son, J.; Kim, J.; Yoon, B. Individualized feedback-based virtual reality exercise improves older women’s self-perceived health: A randomized controlled trial. Arch. Gerontol. Geriatr. 2015, 61, 154–160. [Google Scholar] [CrossRef]
- Huffman, J.C.; Smith, F.A.; Blais, M.A.; Beiser, M.E.; Januzzi, J.L.; Fricchione, G.L. Recognition and treatment of depression and anxiety in patients with acute myocardial infarction. Am. J. Cardiol. 2006, 98, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Rutkowski, S.; Szczegielniak, J.; Szczepańska-Gieracha, J. Evaluation of the Efficacy of Immersive Virtual Reality Therapy as a Method Supporting Pulmonary Rehabilitation: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 352. [Google Scholar] [CrossRef]
- Szczepańska-Gieracha, J.; Jóźwik, S.; Cieślik, B.; Mazurek, J.; Gajda, R. Immersive Virtual Reality Therapy As a Support for Cardiac Rehabilitation: A Pilot Randomized-Controlled Trial. Cyberpsychol. Behav. Soc. Netw. 2021. [Google Scholar] [CrossRef]
- Szczepańska-Gieracha, J.; Cieślik, B.; Serweta, A.; Klajs, K. Virtual Therapeutic Garden: A Promising Method Supporting the Treatment of Depressive Symptoms in Late-Life: A Randomized Pilot Study. J. Clin. Med. 2021, 10, 1942. [Google Scholar] [CrossRef] [PubMed]
- Jóźwik, S.; Cieślik, B.; Gajda, R.; Szczepańska-Gieracha, J. Evaluation of the Impact of Virtual Reality-Enhanced Cardiac Rehabilitation on Depressive and Anxiety Symptoms in Patients with Coronary Artery Disease: A Randomised Controlled Trial. J. Clin. Med. 2021, 10, 2148. [Google Scholar] [CrossRef] [PubMed]
- Plopa, M.; Makarowski, R. Perception of Stress Questionnaire; VIZJA Press&IT: Warsaw, Poland, 2010. [Google Scholar]
- Smarr, K.L.; Keefer, A.L. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care Res. 2011, 63 (Suppl. 11), S454–S466. [Google Scholar] [CrossRef]
- Pizzi, C.; Santarella, L.; Manfrini, O.; Chiavaroli, M.; Agushi, E.; Cordioli, E.; Costa, G.M.; Bugiardini, R. Ischemic heart disease and depression: An underestimated clinical association. G. Ital. Cardiol. 2006 2013, 14, 526–537. [Google Scholar] [CrossRef]
- Lichtman, J.H.; Froelicher, E.S.; Blumenthal, J.A.; Carney, R.M.; Doering, L.V.; Frasure-Smith, N.; Freedland, K.E.; Jaffe, A.S.; Leifheit-Limson, E.C.; Sheps, D.S.; et al. Depression as a risk factor for poor prognosis among patients with acute coronary syndrome: Systematic review and recommendations: A scientific statement from the American Heart Association. Circulation 2014, 129, 1350–1369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Figueredo, V.M. The time has come for physicians to take notice: The impact of psychosocial stressors on the heart. Am. J. Med. 2009, 122, 704–712. [Google Scholar] [CrossRef] [Green Version]
- Halaris, A. Comorbidity between depression and cardiovascular disease. Int. Angiol. J. Int. Union Angiol. 2009, 28, 92–99. [Google Scholar]
- Raič, M. Depression and Heart Diseases: Leading Health Problems. Psychiatr. Danub. 2017, 29 (Suppl. 4), 770–777. [Google Scholar]
- Sokoreli, I.; de Vries, J.J.G.; Pauws, S.C.; Steyerberg, E.W. Depression and anxiety as predictors of mortality among heart failure patients: Systematic review and meta-analysis. Heart Fail. Rev. 2016, 21, 49–63. [Google Scholar] [CrossRef]
- Albus, C.; Ladwig, K.-H.; Herrmann-Lingen, C. Psychocardiology: Clinically relevant recommendations regarding selected cardiovascular diseases. Dtsch. Med. Wochenschr. 1946 2014, 139, 596–601. [Google Scholar] [CrossRef]
- Barnes, D.E.; Alexopoulos, G.S.; Lopez, O.L.; Williamson, J.D.; Yaffe, K. Depressive symptoms, vascular disease, and mild cognitive impairment: Findings from the Cardiovascular Health Study. Arch. Gen. Psychiatry 2006, 63, 273–279. [Google Scholar] [CrossRef] [Green Version]
- Ladwig, K.-H.; Lederbogen, F.; Albus, C.; Angermann, C.; Borggrefe, M.; Fischer, D.; Fritzsche, K.; Haass, M.; Jordan, J.; Jünger, J.; et al. Position paper on the importance of psychosocial factors in cardiology: Update 2013. Ger. Med. Sci. GMS E-J 2014, 12, Doc09. [Google Scholar] [CrossRef]
- Piepenburg, S.M.; Faller, H.; Störk, S.; Ertl, G.; Angermann, C.E. Symptom patterns and clinical outcomes in women versus men with systolic heart failure and depression. Clin. Res. Cardiol. Off. J. Ger. Card. Soc. 2019, 108, 244–253. [Google Scholar] [CrossRef]
- Szczepańska-Gieracha, J.; Cieślik, B.; Rutkowski, S.; Kiper, P.; Turolla, A. What can virtual reality offer to stroke patients? A narrative review of the literature. NeuroRehabilitation 2020, 47, 109–120. [Google Scholar] [CrossRef]
- Urech, A.; Krieger, T.; Chesham, A.; Mast, F.W.; Berger, T. Virtual Reality-Based Attention Bias Modification Training for Social Anxiety: A Feasibility and Proof of Concept Study. Front. Psychiatry 2015, 6. [Google Scholar] [CrossRef] [Green Version]
- Ihmig, F.R.; Neurohr-Parakenings, F.; Schäfer, S.K.; Lass-Hennemann, J.; Michael, T. On-line anxiety level detection from biosignals: Machine learning based on a randomized controlled trial with spider-fearful individuals. PLoS ONE 2020, 15, e0231517. [Google Scholar] [CrossRef]
- Garcia-Palacios, A.; Hoffman, H.; Carlin, A.; Furness, T.A.; Botella, C. Virtual reality in the treatment of spider phobia: A controlled study. Behav. Res. Ther. 2002, 40, 983–993. [Google Scholar] [CrossRef]
- Bouchard, S.; Côté, S.; St-Jacques, J.; Robillard, G.; Renaud, P. Effectiveness of virtual reality exposure in the treatment of arachnophobia using 3D games. Technol. Health Care Off. J. Eur. Soc. Eng. Med. 2006, 14, 19–27. [Google Scholar] [CrossRef]
- Carlin, A.S.; Hoffman, H.G.; Weghorst, S. Virtual reality and tactile augmentation in the treatment of spider phobia: A case report. Behav. Res. Ther. 1997, 35, 153–158. [Google Scholar] [CrossRef]
- Gebara, C.M.; Barros-Neto, T.P.; Gertsenchtein, L.; Lotufo-Neto, F. Virtual reality exposure using three-dimensional images for the treatment of social phobia. Rev. Bras. Psiquiatr. Sao Paulo Braz. 1999 2016, 38, 24–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bouchard, S.; Dumoulin, S.; Robillard, G.; Guitard, T.; Klinger, É.; Forget, H.; Loranger, C.; Roucaut, F.X. Virtual reality compared with in vivo exposure in the treatment of social anxiety disorder: A three-arm randomised controlled trial. Br. J. Psychiatry J. Ment. Sci. 2017, 210, 276–283. [Google Scholar] [CrossRef] [Green Version]
- Park, M.J.; Kim, D.J.; Lee, U.; Na, E.J.; Jeon, H.J. A Literature Overview of Virtual Reality (VR) in Treatment of Psychiatric Disorders: Recent Advances and Limitations. Front. Psychiatry 2019, 10, 505. [Google Scholar] [CrossRef] [PubMed]
- Lindner, P.; Hamilton, W.; Miloff, A.; Carlbring, P. How to Treat Depression With Low-Intensity Virtual Reality Interventions: Perspectives on Translating Cognitive Behavioral Techniques Into the Virtual Reality Modality and How to Make Anti-Depressive Use of Virtual Reality–Unique Experiences. Front. Psychiatry 2019, 10. [Google Scholar] [CrossRef] [Green Version]
- Migoya-Borja, M.; Delgado-Gómez, D.; Carmona-Camacho, R.; Porras-Segovia, A.; López-Moriñigo, J.-D.; Sánchez-Alonso, M.; Albarracín García, L.; Guerra, N.; Barrigón, M.L.; Alegría, M.; et al. Feasibility of a Virtual Reality-Based Psychoeducational Tool (VRight) for Depressive Patients. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.; Bullock, K.; Bailenson, J. Virtual Reality Behavioral Activation as an Intervention for Major Depressive Disorder: Case Report. JMIR Ment. Health 2020, 7, e24331. [Google Scholar] [CrossRef]
- Guillén, V.; Baños, R.M.; Botella, C. Users’ Opinion About a Virtual Reality System as an Adjunct to Psychological Treatment for Stress-Related Disorders: A Quantitative and Qualitative Mixed-Methods Study. Front. Psychol. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Lognoul, M.; Nasello, J.; Triffaux, J.-M. Virtual reality exposure therapy for post-traumatic stress disorders, obsessive-compulsive disorders and anxiety disorders: Indications, added value and limitations. L’Encephale 2020, 46, 293–300. [Google Scholar] [CrossRef]
- Maarsingh, B.M.; Bos, J.; Van Tuijn, C.F.J.; Renard, S.B. Changing Stress Mindset Through Stressjam: A Virtual Reality Game Using Biofeedback. Games Health J. 2019, 8, 326–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldstein, B.I.; Carnethon, M.R.; Matthews, K.A.; McIntyre, R.S.; Miller, G.E.; Raghuveer, G.; Stoney, C.M.; Wasiak, H.; McCrindle, B.W.; American Heart Association Atherosclerosis; et al. Major Depressive Disorder and Bipolar Disorder Predispose Youth to Accelerated Atherosclerosis and Early Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2015, 132, 965–986. [Google Scholar] [CrossRef] [PubMed]
- Tulloch, H.; Heenan, A.; Cupper, L.; Pelletier, R.; O’Farrell, P.; Pipe, A. Depression and Anxiety Screening and Triage Protocol for Cardiac Rehabilitation Programs. J. Cardiopulm. Rehabil. Prev. 2018, 38, 159–162. [Google Scholar] [CrossRef] [PubMed]
- Kustrzycki, W.; Rymaszewska, J.; Malcher, K.; Szczepanska-Gieracha, J.; Biecek, P. Risk factors of depressive and anxiety symptoms 8 years after coronary artery bypass grafting. Eur. J. Cardiothorac. Surg. 2012, 41, 302–306. [Google Scholar] [CrossRef] [Green Version]
- Szczepanska-Gieracha, J.; Morka, J.; Kowalska, J.; Kustrzycki, W.; Rymaszewska, J. The role of depressive and anxiety symptoms in the evaluation of cardiac rehabilitation efficacy after coronary artery bypass grafting surgery. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2012, 42, e108–e114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rizzo, A.S.; Koenig, S.T.; Talbot, T.B. Clinical Virtual Reality: Emerging Opportunities for Psychiatry. Focus Am. Psychiatr. Publ. 2018, 16, 266–278. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total | Experimental Group | Control Group | p |
|---|---|---|---|---|
| N | 43 | 17 | 26 | - |
| Age, years (SD) | 65.40 (7.98) | 65.65 (10.07) | 65.23 (6.49) | 0.87 |
| Body mass, kg (SD) | 70.98 (12.76) | 71.06 (13.26) | 70.92 (12.68) | 0.97 |
| Height, cm (SD) | 161.16 (6.09) | 159.24 (4.72) | 162.42 (6.63) | 0.09 |
| BMI, kg/cm2 (SD) | 27.27 (4.41) | 27.91 (4.46) | 26.85 (4.40) | 0.44 |
| Specific diagnosis, N (%) | ||||
| Pacemaker | 2 (4.65) | 2 (4.65) | 0 | 0.15 |
| PCI | 15 (34.88) | 7 (16.28) | 8 (18.60) | |
| STEMI | 6 (13.95) | 1 (2.32) | 5 (11.63) | |
| NSTEMI | 9 (20.93) | 1 (2.32) | 8 (18.60) | |
| CABG | 3 (6.98) | 2 (4.65) | 1 (2.32) | |
| Heart stimulator | 2 (4.65) | 2 (4.65) | 0 | |
| Replaced electrode | 1 (2.32) | 1 (2.32) | 0 | |
| Cardiomyopathy | 1 (2.32) | 1 (2.32) | 0 | |
| Artificial valve implantation | 2 (4.65) | 0 | 2 (4.65) | |
| Takotsubo syndrome | 1 (2.32) | 0 | 1 (2.32) | |
| Paroxysmal atrial fibrillation | 1 (2.32) | 0 | 1 (2.32) | |
| Diabetes, N (%) | 11(25.58) | 4 (9.30) | 7 (16.28) | 0.80 |
| Education, N (%) | 0.31 | |||
| Primary/vocational | 12 (27.90) | 5(11.63) | 7 (16.28) | |
| Secondary | 13 (30.23) | 3 (6.98) | 10 (23.25) | |
| Higher | 18 (41.86) | 9 (20.93) | 9 (20.93) | |
| Marital status, N (%) | 0.14 | |||
| Married | 20 (46.51) | 7 (16.28) | 13 (30.23) | |
| Single | 7 (16.28) | 5 (11.63) | 2 (4.65) | |
| Divorced | 3 (6.98) | 2 (4.65) | 1 (2.32) | |
| Widowed | 13 (30.23) | 3 (6.98) | 10 (23.25) | |
| Employment status, N (%) | 0.22 | |||
| Employed | 6 (13.95) | 1 (2.32) | 5 (11.63) | |
| Disability pension | 3 (6.98) | 1 (2.32) | 2 (4.65) | |
| Retired | 32 (74.42) | 13 (30.23) | 19 (44.19) | |
| Unemployed | 2 (4.65) | 2 (4.65) | 0 | |
| Characteristic | Measurement | Group | p | |
|---|---|---|---|---|
| Experimental (N = 17) | Control (N = 26) | |||
| Mean (SD) | Mean (SD) | |||
| HADS | Baseline | 14.29 (8.04) | 16.27 (7.52) | 0.42 |
| Final | 12.94 (7.08) | 16.81 (7.64) | 0.10 | |
| HADS-Anxiety | Baseline | 7.88 (4.27) | 8.92 (4.21) | 0.44 |
| Final | 7.88 (3.69) | 9.54 (4.17) | 0.19 | |
| HADS-Depression | Baseline | 6.41 (4.21) | 7.35 (3.80) | 0.46 |
| Final | 5.06 (3.88) | 7.27 (4.00) | 0.07 | |
| General stress score | Baseline | 59.82 (20.00) | 65.88 (16.69) | 0.29 |
| Final | 55.18 (16.02) | 69.50 (14.30) | 0.004 | |
| Emotional tension | Baseline | 23.29 (7.92) | 25.00 (6.39) | 0.28 |
| Final | 21.76 (6.54) | 27.08 (5.63) | 0.005 | |
| External stress | Baseline | 16.59 (6.21) | 19.08 (6.15) | 0.20 |
| Final | 15.12 (5.87) | 19.77 (5.53) | 0.01 | |
| Intrapsychic stress | Baseline | 19.94 (8.17) | 21.81 (6.12) | 0.40 |
| Final | 18.29 (6.72) | 22.65 (5.30) | 0.02 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jóźwik, S.; Cieślik, B.; Gajda, R.; Szczepańska-Gieracha, J. The Use of Virtual Therapy in Cardiac Rehabilitation of Female Patients with Heart Disease. Medicina 2021, 57, 768. https://doi.org/10.3390/medicina57080768
Jóźwik S, Cieślik B, Gajda R, Szczepańska-Gieracha J. The Use of Virtual Therapy in Cardiac Rehabilitation of Female Patients with Heart Disease. Medicina. 2021; 57(8):768. https://doi.org/10.3390/medicina57080768
Chicago/Turabian StyleJóźwik, Sandra, Błażej Cieślik, Robert Gajda, and Joanna Szczepańska-Gieracha. 2021. "The Use of Virtual Therapy in Cardiac Rehabilitation of Female Patients with Heart Disease" Medicina 57, no. 8: 768. https://doi.org/10.3390/medicina57080768
APA StyleJóźwik, S., Cieślik, B., Gajda, R., & Szczepańska-Gieracha, J. (2021). The Use of Virtual Therapy in Cardiac Rehabilitation of Female Patients with Heart Disease. Medicina, 57(8), 768. https://doi.org/10.3390/medicina57080768







