Treatment of Intertrochanteric Femur Fractures with Hip Arthroplasty in Older Patients: A Narrative Review of Indications and Outcomes
Abstract
1. Introduction
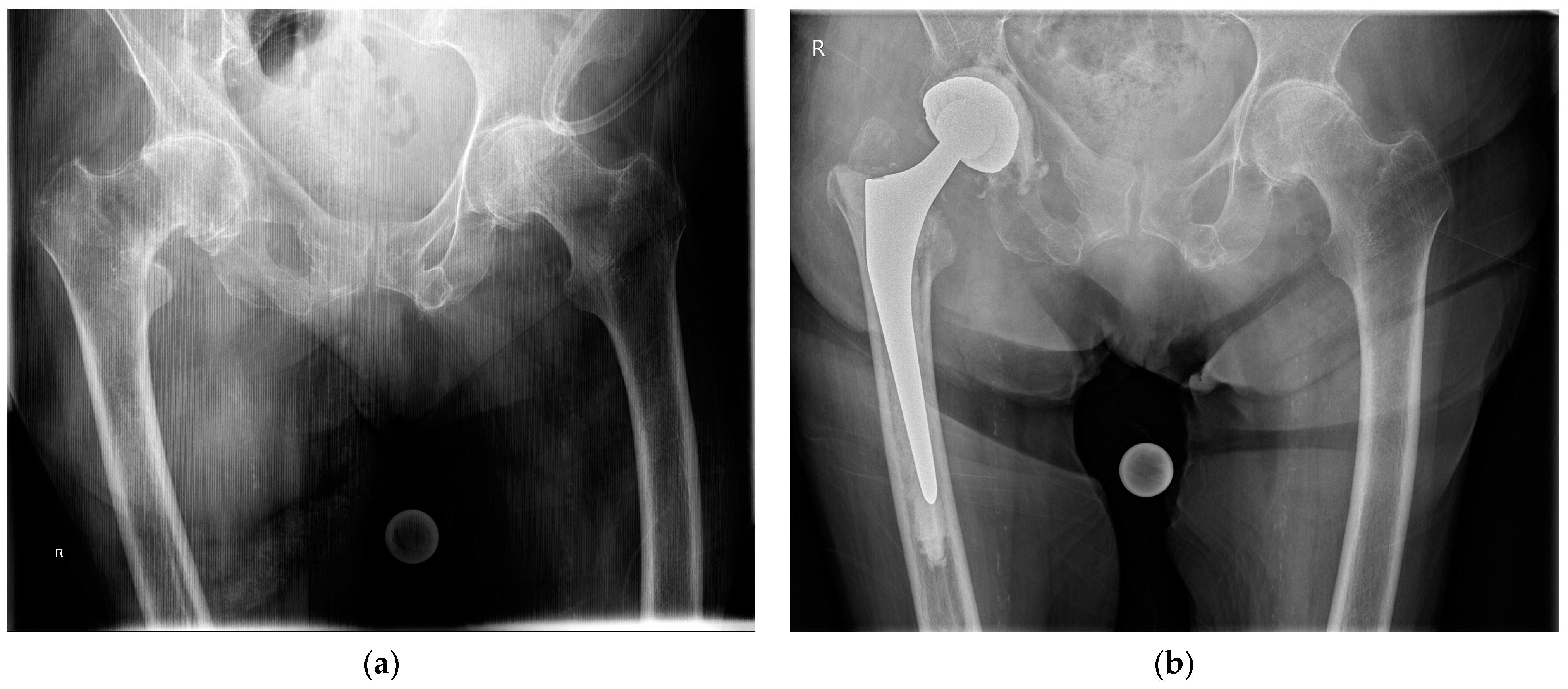
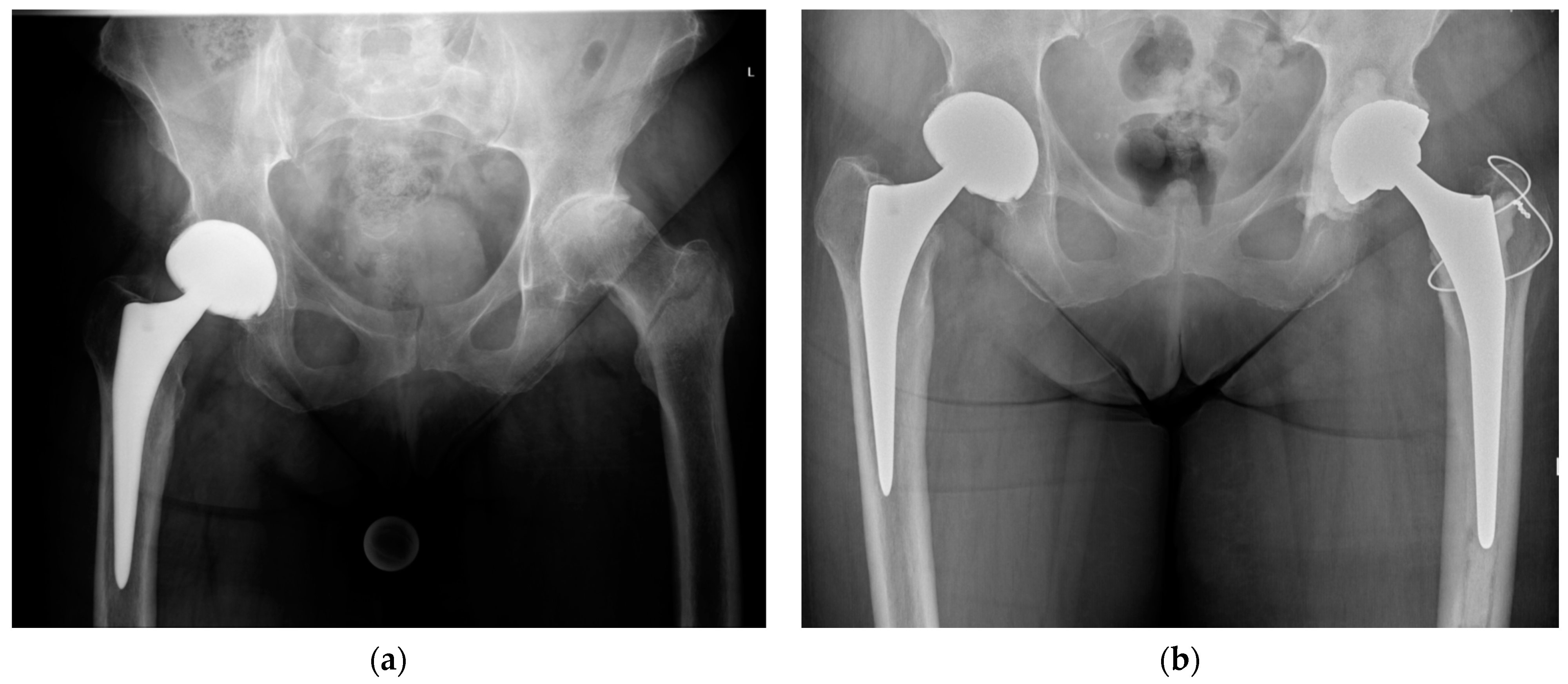
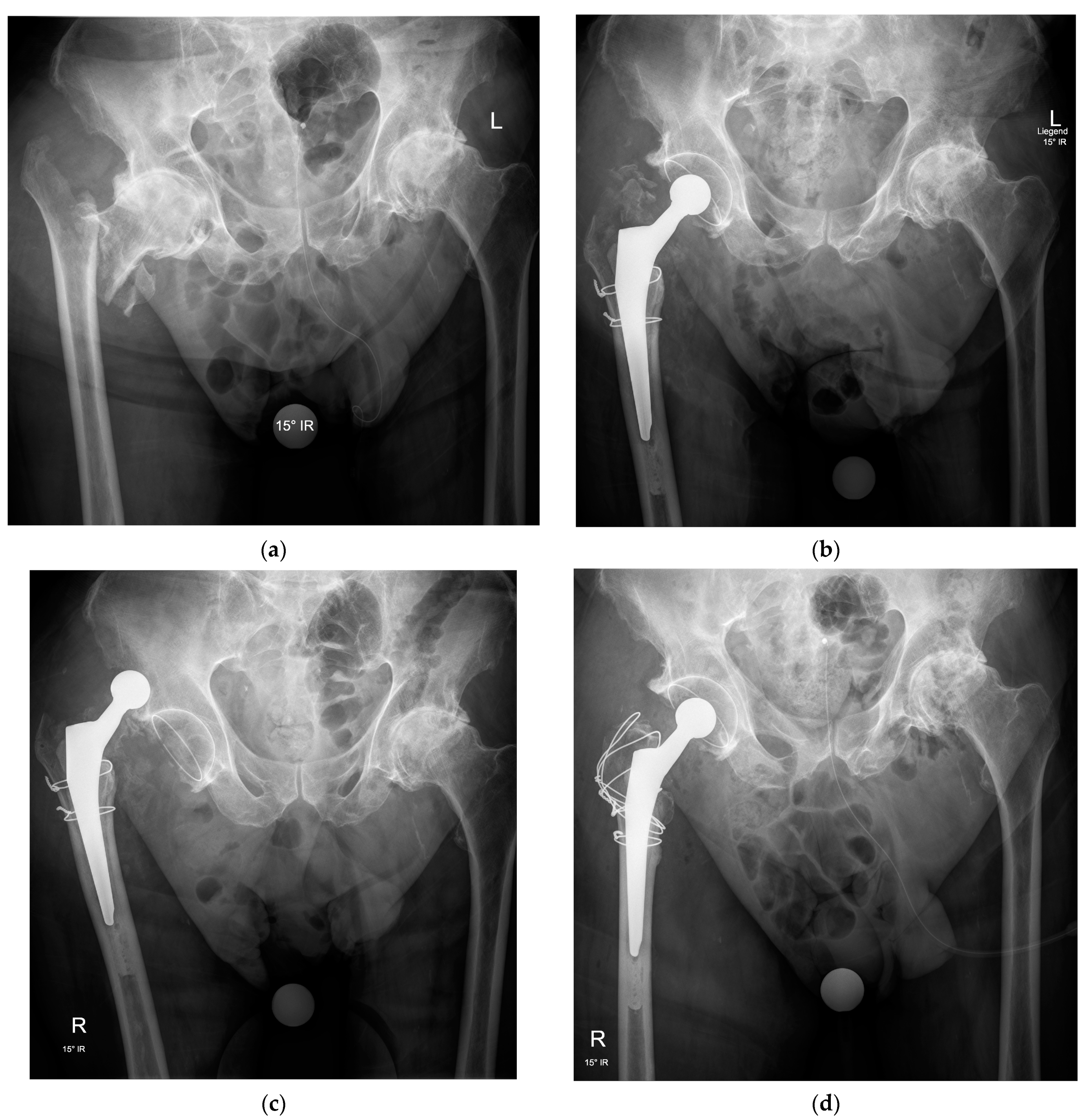
2. Indications
3. Surgical Technique
3.1. Surgical Approach
3.2. Implant Selection
3.3. Hip Abductor Mechanism Repair
4. Results
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J. Bone Miner. Res. 2007, 22, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Roth, T.; Kammerlander, C.; Gosch, M.; Luger, T.J.; Blauth, M. Outcome in geriatric fracture patients and how it can be improved. Osteoporos. Int. 2010, 21, S615–S619. [Google Scholar] [CrossRef]
- Huusko, T.M.; Karppi, P.; Avikainen, V.; Kautiainen, H.; Sulkava, R. Randomised, clinically controlled trial of intensive geriatric rehabilitation in patients with hip fracture: Subgroup analysis of patients with dementia. BMJ 2000, 321, 1107–1111. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, K.; Miyamoto, R.; Levine, B.R.; Egol, K.A.; Zuckerman, J.D. Surgical management of hip fractures: An evidence-based review of the literature. II: Intertrochanteric fractures. J. Am. Acad. Orthop. Surg. 2008, 16, 665–673. [Google Scholar] [CrossRef] [PubMed]
- Socci, A.R.; Casemyr, N.E.; Leslie, M.P.; Baumgaertner, M.R. Implant options for the treatment of intertrochanteric fractures of the hip: Rationale, evidence, and recommendations. Bone Jt. J. 2017, 99, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Tronzo, R.G. The use of an endoprosthesis for severely comminuted trochanteric fractures. Orthop. Clin. N. Am. 1974, 5, 679–681. [Google Scholar] [CrossRef]
- Stern, M.B.; Goldstein, T.B. The use of the Leinbach prosthesis in intertrochanteric fractures of the hip. Clin. Orthop. Relat. Res. 1977, 128, 325–331. [Google Scholar] [CrossRef]
- Baumgaertner, M.R.; Curtin, S.L.; Lindskog, D.M.; Keggi, J.M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J. Bone Jt. Surg. Am. 1995, 77, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Bojan, A.J.; Beimel, C.; Taglang, G.; Collin, D.; Ekholm, C.; Jönsson, A. Critical factors in cut-out complication after Gamma Nail treatment of proximal femoral fractures. BMC Musculoskelet. Disord. 2013, 14, 1. [Google Scholar] [CrossRef]
- Shen, J.; Wang, D.L.; Chen, G.X.; Yang, H.L.; Li, L.; Wei, M.X.; Cai, X.Q.; Yu, Z.H.; Cheng, L.; Zhang, X.X.; et al. Bipolar hemiarthroplasty compared with internal fixation for unstable intertrochanteric fractures in elderly patients. J. Orthop. Sci. 2012, 17, 722–729. [Google Scholar] [CrossRef]
- Gallagher, C.A.; Jones, C.W.; Kimmel, L.; Wylde, C.; Osbrough, A.; Bulsara, M.; Hird, K.; Yates, P. Osteoarthritis is associated with increased failure of proximal femoral fracture fixation. Int. Orthop. 2019, 43, 1223–1230. [Google Scholar] [CrossRef]
- Haentjens, P.; Lamraski, G. Endoprosthetic replacement of unstable, comminuted intertrochanteric fracture of the femur in the elderly, osteoporotic patient: A review. Disabil. Rehabil. 2005, 27, 1167–1180. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Liu, J.; Zhen, P.; Shen, W.; Chang, Y.; Zhang, H.; Zhu, Q.; Li, X. Proximal femoral nail anti-rotation versus cementless bipolar hemiarthroplasty for unstable femoral intertrochanteric fracture in the elderly: A retrospective study. BMC Musculoskelet. Disord. 2019, 20, 500. [Google Scholar] [CrossRef]
- Park, B.J.; Cho, H.M.; Min, W.B. A Comparison of Internal Fixation and Bipolar Hemiarthroplasty for the Treatment of Reverse Oblique Intertrochanteric Femoral Fractures in Elderly Patients. Hip Pelvis 2015, 27, 152–163. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Zhou, H. Primary cemented hemiarthroplasty for unstable intertrochanteric fractures in elderly severe osteoporotic patients. Injury 2020, 51, 670–673. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, A.; Iltar, S.; Alemdaroğlu, K.B.; Dinçel, V.E.; Özmeriç, A.; Gökgöz, B. Is functional outcome better after arthroplasty for trochanteric fractures in older adults? Acta Ortop. Bras. 2018, 26, 8–10. [Google Scholar] [CrossRef]
- Grune, S.; Füchtmeier, B.; Müller, F. Endoprosthetic treatment of pertrochanteric femoral fractures with concomitant coxarthrosis: A consecutive observational study with a control group. Unfallchirurg 2021. [Google Scholar] [CrossRef]
- Fichman, S.G.; Mäkinen, T.J.; Safir, O.; Vincent, A.; Lozano, B.; Kashigar, A.; Kuzyk, P.R. Arthroplasty for unstable pertrochanteric hip fractures may offer a lower re-operation rate as compared to cephalomedullary nailing. Int. Orthop. 2016, 40, 15–20. [Google Scholar] [CrossRef]
- Geiger, F.; Zimmermann-Stenzel, M.; Heisel, C.; Lehner, B.; Daecke, W. Trochanteric fractures in the elderly: The influence of primary hip arthroplasty on 1-year mortality. Arch. Orthop. Trauma Surg. 2007, 127, 959–966. [Google Scholar] [CrossRef]
- Bonnevialle, P.; Saragaglia, D.; Ehlinger, M.; Tonetti, J.; Maisse, N.; Adam, P.; Le Gall, C.; French Hip and Knee Society; Trauma Surgery Academy. Trochanteric locking nail versus arthroplasty in unstable intertrochanteric fracture in patients aged over 75 years. Orthop. Traumatol. Surg. Res. 2011, 97, S95–S100. [Google Scholar] [CrossRef]
- Grote, S.; Stegmeyer, F.; Bogner, V.; Biberthaler, P.; Mutschler, W. Treatment results after cemented hemiprosthesis for care of unstable pertrochanteric femoral fractures in the elderly. Unfallchirurg 2012, 115, 234–242. [Google Scholar] [CrossRef]
- Noda, M.; Saegusa, Y.; Takahashi, M.; Noguchi, C.; Yoshikawa, C.; Mikami, H.; Gotouda, A. Comparison of Post-Operative Muscular Strength Between Gamma Nailing and Hemiarthroplasty System in Femoral Intertrochanteric Fractures. Open Orthop. J. 2017, 11, 255–262. [Google Scholar] [CrossRef]
- Özkayın, N.; Okçu, G.; Aktuğlu, K. Intertrochanteric femur fractures in the elderly treated with either proximal femur nailing or hemiarthroplasty: A prospective randomised clinical study. Injury 2015, 46 (Suppl. 2), S3–S8. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Kim, Y.G.; Hwang, J.K. Cementless calcar-replacement hemiarthroplasty compared with intramedullary fixation of unstable intertrochanteric fractures: A prospective, randomized study. J. Bone Jt. Surg. Am. 2005, 87, 2186–2192. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jolly, A.; Bansal, R.; More, A.R.; Pagadala, M.B. Comparison of complications and functional results of unstable intertrochanteric fractures of femur treated with proximal femur nails and cemented hemiarthroplasty. J. Clin. Orthop. Trauma 2019, 10, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Agar, A.; Sahin, A.; Gunes, O.; Gulabi, D.; Erturk, C. Comparison of Cementless Calcar-Replacement Hemiarthroplasty With Proximal Femoral Nail for the Treatment of Unstable Intertrochanteric Fractures at Older Age Group. Cureus 2021, 13, e12854. [Google Scholar] [CrossRef] [PubMed]
- Çiloğlu, O.; Karaali, E.; Kuşvuran Özkan, A.; Ekiz, T. Distally-fixed non-modular monoblock fluted long-stem hemiarthroplasty versus proximal femoral nailing for elderly patients with an osteoporotic intertrochanteric fracture: A retrospective comparative study. Hip Int. 2020. [Google Scholar] [CrossRef]
- Ucpunar, H.; Camurcu, Y.; Çöbden, A.; Sofu, H.; Kis, M.; Demirel, H. Comparative evaluation of postoperative health status and functional outcome in patients treated with either proximal femoral nail or hemiarthroplasty for unstable intertrochanteric fracture. J. Orthop. Surg. 2019, 27. [Google Scholar] [CrossRef]
- Desteli, E.E.; Imren, Y.; Erdogan, M.; Aydagun, O. Quality of Life Following Treatment of Trochanteric Fractures with Proximal Femoral Nail versus Cementless Bipolar Hemiarthroplasty in Elderly. Clin. Investig. Med. 2015, 38, E63–E72. [Google Scholar] [CrossRef]
- Ekinci, Y.; Gürbüz, K.; Batın, S.; Kahraman, M.; Doğar, F.; Kaya Erten, Z. A multicenter intertrochanteric fracture study in the elderly: Hemiarthroplasty versus proximal femoral nailing. Jt. Dis. Relat. Surg. 2020, 31, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Tang, P.; Hu, F.; Shen, J.; Zhang, L.; Zhang, L. Proximal femoral nail antirotation versus hemiarthroplasty: A study for the treatment of intertrochanteric fractures. Injury 2012, 43, 876–881. [Google Scholar] [CrossRef] [PubMed]
- Hongku, N.; Woratanarat, P.; Nitiwarangkul, L.; Rattanasiri, S.; Thakkinstian, A. Fracture fixation versus hemiarthroplasty for unstable intertrochanteric fractures in elderly patients: A systematic review and network meta-analysis of randomized controlled trials. Orthop. Traumatol. Surg. Res. 2021, 102838. [Google Scholar] [CrossRef]
- Kiran Kumar, G.N.; Meena, S.; Kumar, V.; Manjunath, S.; Mk, V.R. Bipolar hemiarthroplasty in unstable intertrochanteric fractures in elderly: A prospective study. J. Clin. Diagn. Res. 2013, 7, 1669–1671. [Google Scholar] [CrossRef]
- Nie, B.; Wu, D.; Yang, Z.; Liu, Q. Comparison of intramedullary fixation and arthroplasty for the treatment of intertrochanteric hip fractures in the elderly: A meta-analysis. Medicine 2017, 96, e7446. [Google Scholar] [CrossRef] [PubMed]
- Ju, J.B.; Zhang, P.X.; Jiang, B.G. Hip Replacement as Alternative to Intramedullary Nail in Elderly Patients with Unstable Intertrochanteric Fracture: A Systematic Review and Meta-Analysis. Orthop. Surg. 2019, 11, 745–754. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W.; Shon, H.C.; Song, S.H.; Lee, Y.K.; Koo, K.H.; Ha, Y.C. Reoperation rate, mortality and ambulatory ability after internal fixation versus hemiarthroplasty for unstable intertrochanteric fractures in elderly patients: A study on Korean Hip Fracture Registry. Arch. Orthop. Trauma Surg. 2020, 140, 1611–1618. [Google Scholar] [CrossRef]
- Tu, D.P.; Liu, Z.; Yu, Y.K.; Xu, C.; Shi, X.L. Internal Fixation versus Hemiarthroplasty in the Treatment of Unstable Intertrochanteric Fractures in the Elderly: A Systematic Review and Meta-Analysis. Orthop. Surg. 2020, 12, 1053–1064. [Google Scholar] [CrossRef]
- Gölge, U.H.; Pazarci, O.; Kılınç, S.; Nusran, G.; Kaymaz, B.; Göksel, F.; Kömürcü, E.; Bulut, O. The treatment of intertrochanteric fractures comparison of PFN and hemiarthroplasty 3-year mortality study. Acta Orthop. Belg. 2016, 82, 508–515. [Google Scholar] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martinho, T.; Stoffel, K. Treatment of Intertrochanteric Femur Fractures with Hip Arthroplasty in Older Patients: A Narrative Review of Indications and Outcomes. Medicina 2021, 57, 763. https://doi.org/10.3390/medicina57080763
Martinho T, Stoffel K. Treatment of Intertrochanteric Femur Fractures with Hip Arthroplasty in Older Patients: A Narrative Review of Indications and Outcomes. Medicina. 2021; 57(8):763. https://doi.org/10.3390/medicina57080763
Chicago/Turabian StyleMartinho, Tiago, and Karl Stoffel. 2021. "Treatment of Intertrochanteric Femur Fractures with Hip Arthroplasty in Older Patients: A Narrative Review of Indications and Outcomes" Medicina 57, no. 8: 763. https://doi.org/10.3390/medicina57080763
APA StyleMartinho, T., & Stoffel, K. (2021). Treatment of Intertrochanteric Femur Fractures with Hip Arthroplasty in Older Patients: A Narrative Review of Indications and Outcomes. Medicina, 57(8), 763. https://doi.org/10.3390/medicina57080763




