Comparative Study of Oral Health-Related Quality of Life (OHRQL) between Different Types of Orthodontic Treatment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
- Adult patients aged over 18 years.
- Patients presenting good oral health (without caries or periodontal disease).
- Patients presenting good general health.
2.2. Exclusion Criteria
- Patients who were to undergo orthognathic surgery.
- Patients who had undergone previous orthodontic treatment.
- Patients who missed more than three appointments.
- Patients presenting systemic disease.
- Incomplete protocol due to a lack of patient collaboration: (1) failure to follow the treatment regimen; (2) forms completed incorrectly.
- Patients unwilling to take part in the study.
2.3. Study Design
- (T0): Before the start of orthodontic treatment.
- (T1): Six months after the start of orthodontic treatment.
- (T2): At the end of orthodontic treatment.
2.4. Statistical Analysis
3. Results
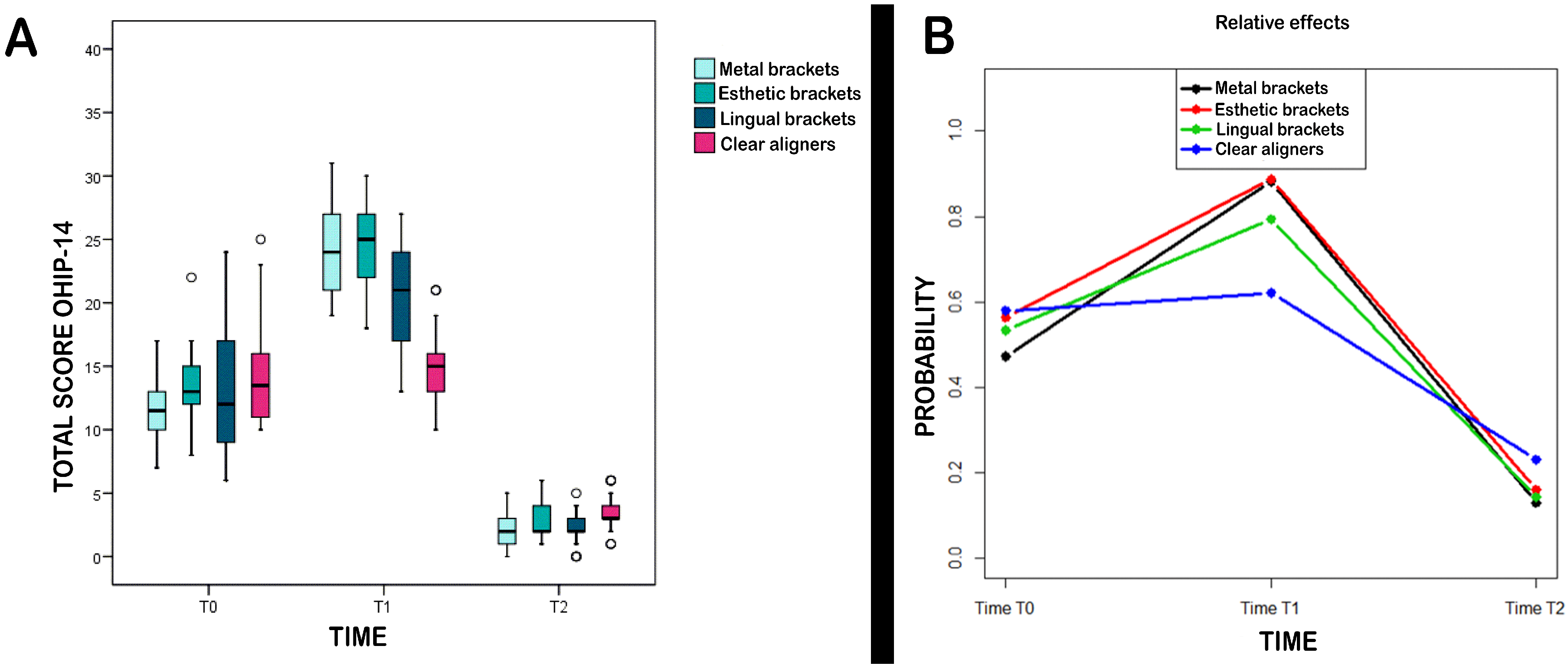
3.1. Evolution of Total OHIP-14 Scores
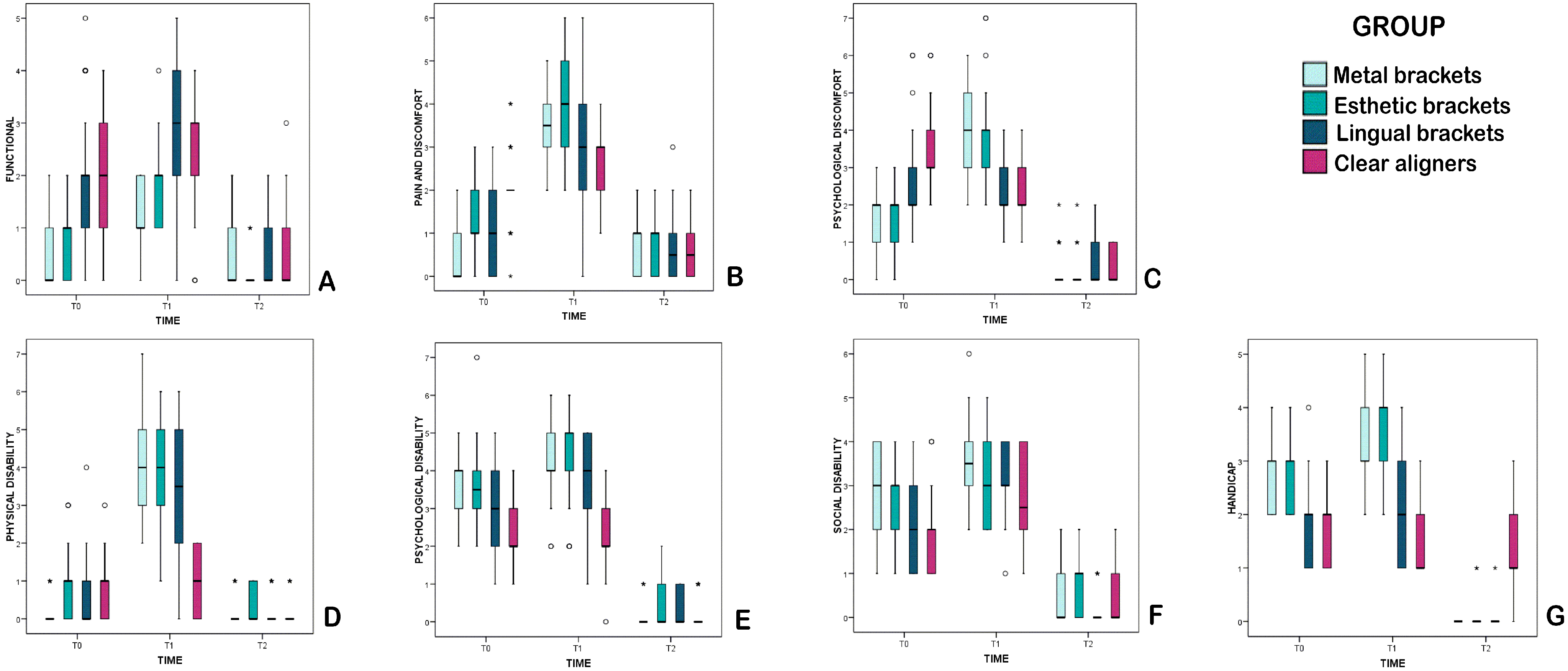
3.2. Evolution of Individual OHIP-14 Domains
3.2.1. Functional Limitation
3.2.2. Physical Pain
3.2.3. Psychological Discomfort
3.2.4. Physical Disability
3.2.5. Psychological Disability
3.2.6. Social Disability
3.2.7. General Handicap
3.3. Gender Differences
3.4. Effects of Individual Variables
4. Discussion
- General Evaluation
- Evaluation of Individual OHIP-14 Domains
5. Conclusions
- In general, patients underwent a significant reduction in quality of life during treatment in comparison with their pre-treatment condition but enjoyed significant improvements at the end of treatment.
- The short medium-term (6 months) negative impact of orthodontic treatment on quality of life was greater among patients treated with buccal brackets. In the lingual brackets group, psychological discomfort and general handicap did not worsen during treatment. In the clear aligners group, physical and psychological disability did not worsen during treatment.
- Regarding overall changes in quality of life from pre-treatment to post-treatment, almost all the OHIP-14 domains underwent improvements in all groups. The only exceptions were that functional limitation remained unchanged in the metal brackets group, as did physical pain suffered by patients treated with esthetic/ceramic brackets and lingual orthodontics.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferrando-Magraner, E.; Garcia-Sanz, V.; Bellot-Arcis, C.; Montiel-Company, J.M.; Almerich-Silla, J.M.; Paredes-Gallardo, V. Oral health-related quality of life of adolescents after orthodontic treatment. A systematic review. J. Clin. Exp. Dent. 2019, 11, e194–e202. [Google Scholar] [CrossRef]
- Adina, S.; Dipalma, G.; Bordea, I.R.; Lucaciu, O.; Feurdean, C.; Inchingolo, A.D.; Septimiu, R.; Malcangi, G.; Cantore, S.; Martin, D.; et al. Orthopedic joint stability influences growth and maxillary development: Clinical aspects. J. Biol. Regul. Homeost. Agents 2020, 34, 747–756. [Google Scholar]
- Coloccia, G.; Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Montenegro, V.; Patano, A.; Marinelli, G.; Laudadio, C.; Limongelli, L.; Di Venere, D.; et al. Effectiveness of Dental and Maxillary Transverse Changes in Tooth-Borne, Bone-Borne, and Hybrid Palatal Expansion through Cone-Beam Tomography: A Systematic Review of the Literature. Medicina 2021, 57, 288. [Google Scholar] [CrossRef]
- Fenton, G.D.; Cazaly, M.H.M.; Rolland, S.L.; Vernazza, C.R. Eliciting Preferences for Adult Orthodontic Treatment: A Discrete Choice Experiment. JDR Clin. Trans. Res. 2021, 6, 23800844211012670. [Google Scholar]
- Ferrans, C.E.; Zerwic, J.J.; Wilbur, J.E.; Larson, J.L. Conceptual model of health-related quality of life. J. Nurs. Scholarsh. 2005, 37, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Zheng, D.H.; Wang, X.X.; Su, Y.R.; Zhao, S.Y.; Xu, C.; Kong, C.; Zhang, J. Assessing changes in quality of life using the Oral Health Impact Profile (OHIP) in patients with different classifications of malocclusion during comprehensive orthodontic treatment. BMC Oral. Health 2015, 15, 148. [Google Scholar] [CrossRef] [Green Version]
- Benson, P.E.; Da’as, T.; Johal, A.; Mandall, N.A.; Williams, A.C.; Baker, S.R.; Marshman, Z. Relationships between dental appearance, self-esteem, socio-economic status, and oral health-related quality of life in UK schoolchildren: A 3-year cohort study. Eur. J. Orthod. 2015, 37, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Kragt, L.; Jaddoe, V.; Wolvius, E.; Ongkosuwito, E. The association of subjective orthodontic treatment need with oral health-related quality of life. Community Dent. Oral Epidemiol. 2017, 45, 365–371. [Google Scholar] [CrossRef]
- Feu, D.; Miguel, J.A.; Celeste, R.K.; Oliveira, B.H. Effect of orthodontic treatment on oral health-related quality of life. Angle Orthod. 2013, 83, 892–898. [Google Scholar] [CrossRef]
- Chen, M.; Wang, D.W.; Wu, L.P. Fixed orthodontic appliance therapy and its impact on oral health-related quality of life in Chinese patients. Angle Orthod. 2010, 80, 49–53. [Google Scholar] [CrossRef] [Green Version]
- Chen, M.; Feng, Z.C.; Liu, X.; Li, Z.M.; Cai, B.; Wang, D.W. Impact of malocclusion on oral health-related quality of life in young adults. Angle Orthod. 2015, 85, 986–991. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antoun, J.S.; Fowler, P.V.; Jack, H.C.; Farella, M. Oral health-related quality of life changes in standard, cleft, and surgery patients after orthodontic treatment. Am. J. Orthod. Dentofacial. Orthop. 2015, 148, 568–575. [Google Scholar] [CrossRef]
- Healey, D.L.; Gauld, R.D.; Thomson, W.M. Treatment-associated changes in malocclusion and oral health-related quality of life: A 4-year cohort study. Am. J. Orthod. Dentofacial. Orthop. 2016, 150, 811–817. [Google Scholar] [CrossRef]
- Seehra, J.; Newton, J.T.; Dibiase, A.T. Interceptive orthodontic treatment in bullied adolescents and its impact on self-esteem and oral-heal- th-related quality of life. Eur. J. Orthod. 2013, 35, 615–621. [Google Scholar] [CrossRef]
- Montero-Martín, J.; Bravo-Pérez, M.; Albaladejo-Martínez, A.; Hernández-Martín, L.A.; Rosel-Gallardo, E.M. Validation the Oral Health Impact Profile (OHIP-14sp) for adults in Spain. Med. Oral. Patol. Oral. Cir. Bucal. 2009, 14, E44–E50. [Google Scholar]
- Allen, P.F. Assessment of oral health related quality of life. Health Qual. Life Outcomes 2003, 1, 40. [Google Scholar] [CrossRef] [Green Version]
- Flores-Mir, C.; Brandelli, J.; Pacheco-Pereira, C. Patient satisfaction and quality of life status after 2 treatment modalities: Invisalign and conventional fixed appliances. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 639–644. [Google Scholar] [CrossRef]
- Miller, K.B.; McGorray, S.P.; Womack, R.; Quintero, J.C.; Perelmuter, M.; Gibson, J.; Dolan, T.A.; Wheeler, T.T. A comparison of treatment impacts between Invisalign aligner and fixed appliance therapy during the first week of treatment. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 302. [Google Scholar] [CrossRef]
- AlSeraidi, M.; Hansa, I.; Dhaval, F.; Ferguson, D.J.; Vaid, N.R. The effect of vestibular, lingual, and aligner appliances on the quality of life of adult patients during the initial stages of orthodontic treatment. Prog. Orthod. 2021, 22, 3. [Google Scholar] [CrossRef]
- De Oliveira, C.M.; Sheiham, A. Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J. Orthod. 2004, 31, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; McGrath, C.; Hägg, U. Changes in oral health-related quality of life during fixed orthodontic appliance therapy: An 18-month prospective longitudinal study. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 214–219. [Google Scholar] [CrossRef]
- Mandava, P.; Singaraju, G.S.; Obili, S.; Nettam, V.; Vatturu, S.; Erugu, S. Impact of self-esteem on the relationship between orthodontic treatment and the oral health-related quality of life in patients after orthodontic treatment—A systematic review. Med. Pharm. Rep. 2021, 94, 158–169. [Google Scholar]
- Zhang, M.; McGrath, C.; Hägg, U. Changes in oral health-related quality of life during fixed orthodontic appliance therapy. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 25–29. [Google Scholar] [CrossRef]
- Johal, A.; Alyaqoobi, I.; Patel, R.; Cox, S. The impact of orthodontic treatment on quality of life and self-esteem in adult patients. Eur. J. Orthod. 2015, 37, 233–237. [Google Scholar] [CrossRef]
- Jung, M.H. Evaluation of the effects of malocclusion and orthodontic treatment on self-esteem in an adolescent population. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 160–166. [Google Scholar] [CrossRef]
- Vontroodt, S.; Lemiere, J.; Cadenas de Llano-Pérula, M.; Verdonck, A.; Laenen, A.; Willems, G. The evolution of self-esteem before, during and after orthodontic treatment in adolescents with dental malocclusion, a prospective cohort study. Eur. J. Orthod. 2020, 42, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Wong, H.M.; McGrath, C.P. Relationship Between the Severity of Malocclusion and Oral Health Related Quality of Life: A Systematic Review and Meta-analysis. Oral. Health Prev. Dent. 2017, 15, 503–517. [Google Scholar] [PubMed]
- Zhang, M.; McGrath, C.; Hägg, U. The impact of malocclusion and its treatment on quality of life: A literature review. Int. J. Paediatr. Dent. 2006, 16, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Bordea, I.R.; Sîrbu, A.; Lucaciu, O.; Ilea, A.; Campian, R.; Todea, D.; Alexescu, T.; Aluaș, M.; Budin, C.; Pop, A. Microleakage—The Main Culprit in Bracket Bond Failure? J. Mind Med. Sci. 2019, 6, 86–94. [Google Scholar] [CrossRef] [Green Version]
| p-Value | |
|---|---|
| Q1. Problems with pronunciation | <0.001 *** |
| Q2. Bad sense of taste | <0.001 *** |
| Q3. Pain | <0.001 *** |
| Q4. Discomfort when eating | <0.001 *** |
| Q5. Concern for the mouth | 0.046 * |
| Q6. Self-consciousness | <0.001 *** |
| Q7. Dissatisfaction with food intake | 0.008 ** |
| Q8. Interruption of meals | 0.328 |
| Q9. Dificulty in relaxing | 0.120 |
| Q10. Embarrassement | <0.001 *** |
| Q11. Irritability | 0.071 |
| Q12. Problems at work | 0.016 * |
| Q13. Less satisfying life | 0.003 ** |
| Q14. Complete inability to function | <0.001 *** |
| T0 | T1 | T2 | TIME | T0 vs. T1 | T1 vs. T2 | T0 vs. T2 | p-Value | |
|---|---|---|---|---|---|---|---|---|
| Metal brackets (M) | 11.5 (7–17) | 24.0 (19–31) | 2.0 (0–5) | <0.001 *** | <0.001 *** | <0.001 *** | <0.001 *** | Time p < 0.001 *** Group p = 0.023 * Interaction p < 0.001 *** |
| Esthetic Brackets (E) | 13.0 (8–22) | 25.0 (18–30) | 2.0 (1–6) | <0.001 *** | <0.001 *** | <0.001 *** | <0.001 *** | |
| Lingual Brackets (L) | 12.0 (6–24) | 21.0 (13–27) | 2.0 (0–5) | <0.001 *** | <0.001 *** | <0.001 *** | <0.001 *** | |
| Clear aligners (C) | 13.5 (10–25) | 15.0 (10–21) | 3.0 (1–6) | <0.001 *** | 0.003 ** | <0.001 *** | <0.001 *** | |
| GROUP | 0.013 * | <0.001 *** | <0.001 *** | |||||
| M vs. E | 0.006 ** | 1.000 | 1.000 | |||||
| M vs. L | 1.000 | 0.018 * | 1.000 | |||||
| M vs. C | 0.018 * | <0.001 *** | <0.001 *** | |||||
| E vs. L | 1.000 | 0.006 ** | 1.000 | |||||
| E vs. C | 1.000 | <0.001 *** | 0.036 * | |||||
| L vs. C | 0.924 | <0.001 *** | <0.001 *** |
| p-Value | |
|---|---|
| Q1 + Q2. Functional Limitation | <0.001 *** |
| Q3 + Q4. Physical pain | <0.001 *** |
| Q5 + Q6. Psychological discomfort | <0.001 *** |
| Q7 + Q8. Physical disability | 0.011 * |
| Q9 + Q10. Psychological disability | <0.001 *** |
| Q11 + Q12. Social disability | 0.002 ** |
| Q13 + Q14. Handicap | <0.001 *** |
| OHIP-14 Total score | 0.013 * |
| OHIP-14 Domains | Study Time | Total | Male | Female | p-Value < 0.05 |
|---|---|---|---|---|---|
| Functional limitation | T0 | 1.22 | 1.21 | 1.22 | |
| T1 | 2.12 | 2.15 | 2.08 | ||
| T2 | 0.39 | 0.39 | 0.39 | ||
| Physical pain | T0 | 1.21 | 1.20 | 1.22 | |
| T1 | 3.29 | 3.43 | 3.15 | ||
| T2 | 0.73 | 0.59 | 0.88 | * | |
| Psychological discomfort | T0 | 2.31 | 2.20 | 2.42 | |
| T1 | 3.10 | 3.07 | 3.14 | ||
| T2 | 0.29 | 0.25 | 0.34 | ||
| Physical disability | T0 | 0.61 | 0.62 | 0.59 | |
| T1 | 3.09 | 3.23 | 2.95 | ||
| T2 | 0.18 | 0.08 | 0.29 | * | |
| Psychological disability | T0 | 3.13 | 3.20 | 3.05 | |
| T1 | 3.71 | 3.80 | 3.61 | ||
| T2 | 0.23 | 0.23 | 0.22 | ||
| Social disability | T0 | 2.42 | 2.43 | 2.41 | |
| T1 | 3.13 | 3.25 | 3.02 | ||
| T2 | 0.42 | 0.49 | 0.34 | ||
| Handicap | T0 | 2.26 | 2.26 | 2.25 | |
| T1 | 2.57 | 2.52 | 2.61 | ||
| T2 | 0.35 | 0.34 | 0.36 | ||
| Total score | T0 | 13.14 | 13.11 | 13.17 | |
| T1 | 21.01 | 21.44 | 20.56 | ||
| T2 | 2.59 | 2.38 | 2.81 |
| OHIP-14 Domains | Study Time | Group | Study Time/Group | Gender | Age | Marital Status | Educational Level | IOTN |
|---|---|---|---|---|---|---|---|---|
| Functional limitation | <0.001 *** | <0.001 *** | <0.001 *** | 0.160 | 0.169 | 0.069 | 0.310 | <0.001 *** |
| Physical pain | <0.001 *** | <0.001 *** | <0.001 *** | 0.827 | 0.341 | 0.455 | 0.788 | <0.001 *** |
| Psychological discomfort | <0.001 *** | 0.004 ** | <0.001 *** | 0.465 | 0.909 | 0.464 | 0.260 | <0.001 *** |
| Physical disability | 0.011 * | <0.001 *** | <0.001 *** | 0.709 | 0.118 | 0.150 | 0.061 | 0.138 |
| Psychological disability | <0.001 *** | <0.001 *** | <0.001 *** | 0.181 | 0.775 | 0.394 | 0.477 | <0.001 *** |
| Social disability | 0.002 ** | 0.001 ** | 0.017 * | 0.124 | 0.436 | 0.096 | 0.101 | 0.191 |
| Handicap | <0.001 *** | <0.001 *** | <0.001 *** | 0.284 | 0.149 | 0.033 * | 0.552 | 0.065 |
| OHIP-14 Total score | <0.001 *** | <0.001 *** | <0.001 *** | 0.322 | 0.243 | 0.382 | 0.561 | <0.001 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zamora-Martínez, N.; Paredes-Gallardo, V.; García-Sanz, V.; Gandía-Franco, J.L.; Tarazona-Álvarez, B. Comparative Study of Oral Health-Related Quality of Life (OHRQL) between Different Types of Orthodontic Treatment. Medicina 2021, 57, 683. https://doi.org/10.3390/medicina57070683
Zamora-Martínez N, Paredes-Gallardo V, García-Sanz V, Gandía-Franco JL, Tarazona-Álvarez B. Comparative Study of Oral Health-Related Quality of Life (OHRQL) between Different Types of Orthodontic Treatment. Medicina. 2021; 57(7):683. https://doi.org/10.3390/medicina57070683
Chicago/Turabian StyleZamora-Martínez, Natalia, Vanessa Paredes-Gallardo, Verónica García-Sanz, José Luis Gandía-Franco, and Beatriz Tarazona-Álvarez. 2021. "Comparative Study of Oral Health-Related Quality of Life (OHRQL) between Different Types of Orthodontic Treatment" Medicina 57, no. 7: 683. https://doi.org/10.3390/medicina57070683
APA StyleZamora-Martínez, N., Paredes-Gallardo, V., García-Sanz, V., Gandía-Franco, J. L., & Tarazona-Álvarez, B. (2021). Comparative Study of Oral Health-Related Quality of Life (OHRQL) between Different Types of Orthodontic Treatment. Medicina, 57(7), 683. https://doi.org/10.3390/medicina57070683









