The Potential Mechanisms of High-Velocity, Low-Amplitude, Controlled Vertebral Thrusts on Neuroimmune Function: A Narrative Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Research Investigating a Link between HVLA Controlled Vertebral Thrusts and Immune Function
3.1.1. Effect of HVLA Controlled Vertebral Thrusts on Immune Mediators
3.1.2. Effects of HVLA Controlled Vertebral Thrust on the Autonomic Nervous System
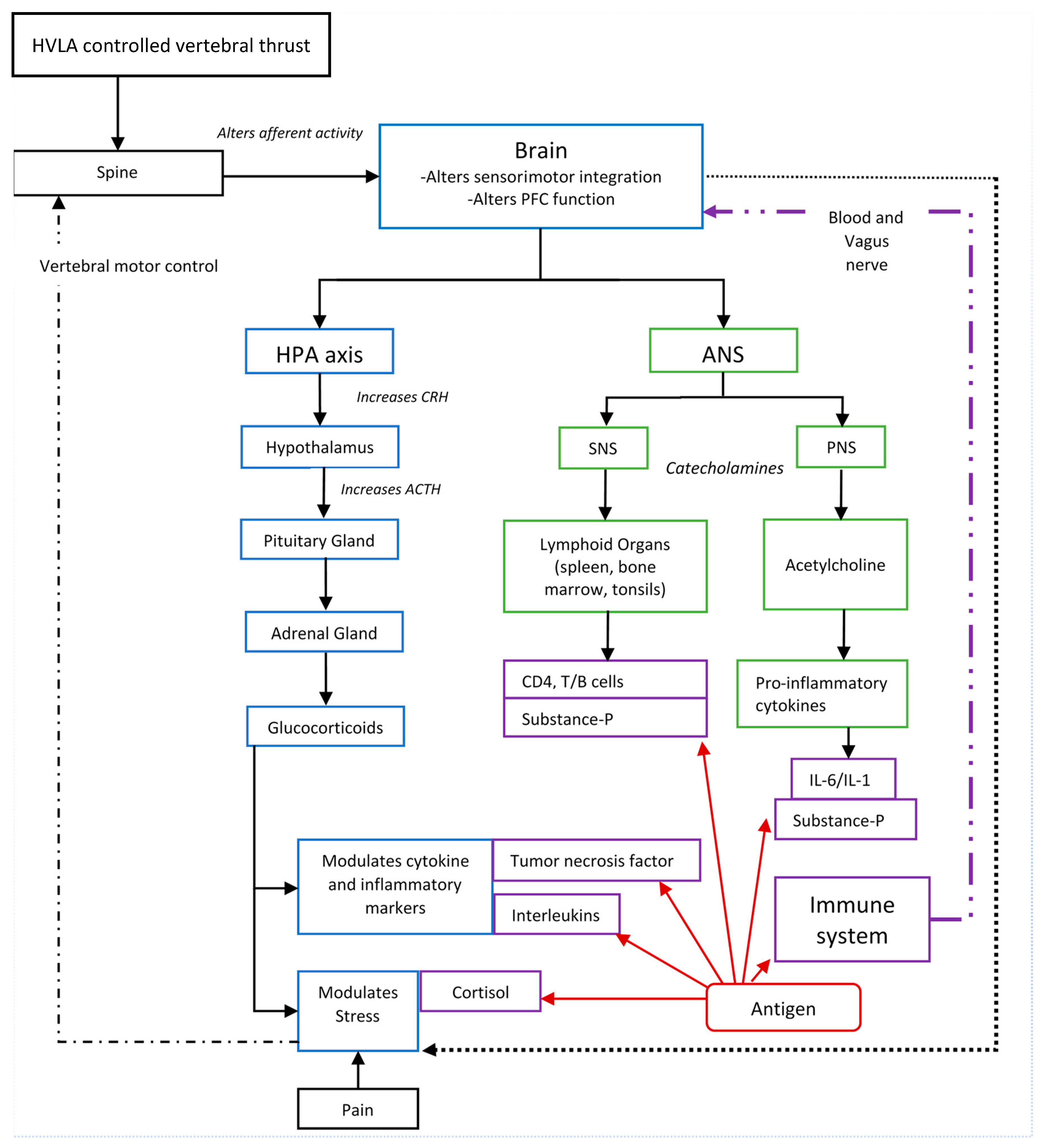
3.2. Potential Mechanisms That Link HVLA Controlled Vertebral Thrusts with Immune Function
3.2.1. The Link between HVLA Controlled Vertebral Thrust and the Central Nervous System
3.2.2. The Link between the Central Nervous System and the Immune System
3.2.3. The Neuroendocrine System
3.2.4. HPA Axis
3.2.5. The ANS
3.2.6. The SNS
3.2.7. The PNS
3.2.8. The Sensory System and the Meningeal Lymphatic System
3.2.9. Stress Negatively Impacts Immune Function and Vertebral Motor Control
3.2.10. Summary of the Neuroimmune Link
4. Implications, limitations, and Recommendations for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ranasinghe, C.; Ozemek, C.; Arena, R. Exercise and well-being during COVID 19-Time to boost your immunity. Expert Rev. Anti Infect. Ther. 2020. [Google Scholar] [CrossRef]
- Wortham, J.M.; Lee, J.T.; Althomsons, S.; Latash, J.; Davidson, A.; Guerra, K. Characteristics of Persons Who Died with COVID-19—United States, February 12–May 18, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 923–929. [Google Scholar] [CrossRef]
- Lai, Q.; Spoletini, G.; Bianco, G.; Graceffa, D.; Agnes, S.; Rossi, M.; Lerut, J. SARS-CoV2 and immunosuppression: A double-edged sword. Transpl. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Sadia, A.; Basra, M.A.R. Therapeutic dilemma in the repression of severe acute respiratory syndrome coronavirus-2 proteome. Drug Dev. Res. 2020. [Google Scholar] [CrossRef]
- Florindo, H.F.; Kleiner, R.; Vaskovich-Koubi, D.; Acúrcio, R.C.; Carreira, B.; Yeini, E.; Tiram, G.; Liubomirski, Y.; Satchi-Fainaro, R. Immune-mediated approaches against COVID-19. Nat. Nanotechnol. 2020. [Google Scholar] [CrossRef]
- De Geest, B.; Ye, T.; Zhong, Z.; García-Sastre, A.; Schotsaert, M. Current status of COVID-19 (pre)clinical vaccine development. Angew Chem. Int. Ed. Engl. 2020. [Google Scholar] [CrossRef]
- Gao, Z.; Lee, J.E.; McDonough, D.J.; Albers, C. Virtual Reality Exercise as a Coping Strategy for Health and Wellness Promotion in Older Adults during the COVID-19 Pandemic. J. Clin. Med. 2020, 9, 1986. [Google Scholar] [CrossRef] [PubMed]
- Dicker, D.; Bettini, S.; Farpour-Lambert, N.; Frühbeck, G.; Golan, R.; Goossens, G.; Halford, J.; O’Malley, G.; Mullerova, D.; Ramos Salas, X.; et al. Obesity and COVID-19: The Two Sides of the Coin. Obes. Facts 2020, 13, 430–438. [Google Scholar] [CrossRef] [PubMed]
- De Faria Coelho-Ravagnani, C.; Corgosinho, F.C.; Sanches, F.F.Z.; Prado, C.M.M.; Laviano, A.; Mota, J.F. Dietary recommendations during the COVID-19 pandemic. Nutr. Rev. 2020. [Google Scholar] [CrossRef]
- Kwon, C.Y.; Kwak, H.Y.; Kim, J.W. Using Mind-Body Modalities via Telemedicine during the COVID-19 Crisis: Cases in the Republic of Korea. Int. J. Environ. Res. Public Health 2020, 17, 4477. [Google Scholar] [CrossRef]
- El Morr, C.; Ritvo, P.; Ahmad, F.; Moineddin, R. Effectiveness of an Eight-Week Web-Based Mindfulness Virtual Community Intervention for University Students on Symptoms of Stress, Anxiety, and Depression: A Randomized Controlled Trial. JMIR Ment. Health 2020. [Google Scholar] [CrossRef]
- Viswanathan, R.; Myers, M.F.; Fanous, A.H. Support Groups and Individual Mental Health Care via Video Conferencing for Frontline Clinicians During the COVID-19 Pandemic. Psychosomatics 2020. [Google Scholar] [CrossRef]
- Daluiso-King, G.; Hebron, C. Is the biopsychosocial model in musculoskeletal physiotherapy adequate? An evolutionary concept analysis. Physiother. Theory Pract. 2020, 1–17. [Google Scholar] [CrossRef]
- Gliedt, J.A.; Schneider, M.J.; Evans, M.W.; King, J.; Eubanks, J.E., Jr. The biopsychosocial model and chiropractic: A commentary with recommendations for the chiropractic profession. Chiropr. Man. Ther. 2017, 25, 16. [Google Scholar] [CrossRef] [PubMed]
- Brennan, P.C.; Kokjohn, K.; Kaltinger, C.J.; Lohr, G.E.; Glendening, C.; Hondras, M.A.; McGregor, M.; Triano, J.J. Enhanced phagocytic cell respiratory burst induced by spinal manipulation: Potential role of substance P. J. Manip. Physiol. Ther. 1991, 14, 399–408. [Google Scholar]
- Brennan, P.C.; Graham, M.A.; Triano, J.J.; Hondras, M.A.; Anderson, R.J. Lymphocyte profiles in patients with chronic low back pain enrolled in a clinical trial. J. Manip. Physiol. Ther. 1994, 17, 219–227. [Google Scholar]
- Selano, J.; Hightower, B.; Pfleger, B.; Collins, K.; Grostic, J. The effects of specific upper cervical adjustments on the CD4 counts of HIV positive patients. Chiropr. Res. J. 1994, 3, 32–39. [Google Scholar]
- Davison, S.; Parkin-Smith, G. The possible effect of upper cervical chiropractic manipulation on short-term lymphocytic response: A pilot study. Eur. J. Chiropr. 2003, 51, 19–28. [Google Scholar]
- Teodorczyk-Injeyan, J.A.; Injeyan, H.S.; Ruegg, R. Spinal manipulative therapy reduces inflammatory cytokines but not substance P production in normal subjects. J. Manip. Physiol. Ther. 2006, 29, 14–21. [Google Scholar] [CrossRef]
- Teodorczyk-Injeyan, J.A.; Injeyan, H.S.; McGregor, M.; Harris, G.M.; Ruegg, R. Enhancement of in vitro interleukin-2 production in normal subjects following a single spinal manipulative treatment. Chiropr. Osteopathy 2008, 16, 5. [Google Scholar] [CrossRef]
- Teodorczyk-Injeyan, J.A.; McGregor, M.; Ruegg, R.; Injeyan, H.S. Interleukin 2-regulated in vitro antibody production following a single spinal manipulative treatment in normal subjects. Chiropr. Osteopathy 2010, 18, 1–8. [Google Scholar] [CrossRef][Green Version]
- Teodorczyk-Injeyan, J.A.; McGregor, M.; Triano, J.J.; Injeyan, S.H. Elevated production of nociceptive CC chemokines and sE-selectin in patients with low back pain and the effects of spinal manipulation: A nonrandomized clinical trial. Clin. J. Pain 2018, 34, 68. [Google Scholar] [CrossRef]
- Teodorczyk-Injeyan, J.A.; Triano, J.J.; Gringmuth, R.; DeGraauw, C.; Chow, A.; Injeyan, H.S. Effects of spinal manipulative therapy on inflammatory mediators in patients with non-specific low back pain: A non-randomized controlled clinical trial. Chiropr. Man. Ther. 2021, 29, 3. [Google Scholar] [CrossRef]
- Roy, R.A.; Boucher, J.P.; Comtois, A.S. Inflammatory response following a short-term course of chiropractic treatment in subjects with and without chronic low back pain. J. Chiropr. Med. 2010, 9, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Padayachy, K.; Vawda, G.H.M.; Shaik, J.; McCarthy, P.W. The immediate effect of low back manipulation on serum cortisol levels in adult males with mechanical low back pain. Clin. Chiropr. 2010, 13, 246–252. [Google Scholar] [CrossRef]
- Licciardone, J.C.; Kearns, C.M.; Hodge, L.M.; Bergamini, M.V. Associations of cytokine concentrations with key osteopathic lesions and clinical outcomes in patients with nonspecific chronic low back pain: Results from the OSTEOPATHIC Trial. J. Am. Osteopath. Assoc. 2012, 112, 596–605. [Google Scholar] [CrossRef]
- Licciardone, J.C.; Kearns, C.M.; Hodge, L.M.; Minotti, D.E. Osteopathic manual treatment in patients with diabetes mellitus and comorbid chronic low back pain: Subgroup results from the OSTEOPATHIC Trial. J. Am. Osteopath. Assoc. 2013, 113, 468–478. [Google Scholar]
- Molina-Ortega, F.; Lomas-Vega, R.; Hita-Contreras, F.; Manzano, G.P.; Achalandabaso, A.; Ramos-Morcillo, A.J.; Martínez-Amat, A. Immediate effects of spinal manipulation on nitric oxide, substance P and pain perception. Man. Ther. 2014, 19, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Plaza-Manzano, G.; Molina, F.; Lomas-Vega, R.; Martínez-Amat, A.; Achalandabaso, A.; Hita-Contreras, F. Changes in biochemical markers of pain perception and stress response after spinal manipulation. J. Orthop. Sports Phys. Ther. 2014, 44, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Sampath, K.K.; Botnmark, E.; Mani, R.; Cotter, J.D.; Katare, R.; Munasinghe, P.E.; Tumilty, S. Neuroendocrine response following a thoracic spinal manipulation in healthy men. J. Orthop. Sports Phys. Ther. 2017, 47, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Degenhardt, B.F.; Johnson, J.C.; Fossum, C.; Andicochea, C.T.; Stuart, M.K. Changes in cytokines, sensory tests, and self-reported pain levels after manual treatment of low back pain. Clin. Spine Surg. 2017, 30, E690–E701. [Google Scholar] [CrossRef]
- Lohman, E.B.; Pacheco, G.R.; Gharibvand, L.; Daher, N.; Devore, K.; Bains, G.; AlAmeri, M.; Berk, L.S. The immediate effects of cervical spine manipulation on pain and biochemical markers in females with acute non-specific mechanical neck pain: A randomized clinical trial. J. Man. Manip. 2019, 27, 186–196. [Google Scholar] [CrossRef] [PubMed]
- Pickar, J.G.; Wheeler, J.D. Response of muscle proprioceptors to spinal manipulative-like loads in the anesthetized cat. JMPT 2001, 24, 2–11. [Google Scholar] [CrossRef]
- Sung, P.S.; Kang, Y.M.; Pickar, J.G. Effect of spinal manipulation duration on low threshold mechanoreceptors in lumbar paraspinal muscles: A preliminary report. Spine 2005, 30, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Pickar, J.G.; Kang, Y.M. Paraspinal muscle spindle responses to the duration of a spinal manipulation under force control. J. Manip. Physiol. 2006, 29, 22–31. [Google Scholar] [CrossRef]
- Pickar, J.G.; Sung, P.S.; Kang, Y.M.; Ge, W. Response of lumbar paraspinal muscles spindles is greater to spinal manipulative loading compared with slower loading under length control. Spine J. 2007, 7, 583–595. [Google Scholar] [CrossRef]
- Cao, D.; Reed, W.; Long, C.; Kawchuk, G.; Pickar, J. Effects of thrust amplitude and duration of high-velocity, low-amplitude spinal manipulation on lumbar muscle spindle responses to vertebral position and movement. J. Manip. Physiol. Ther. 2013, 36, 68–77. [Google Scholar] [CrossRef][Green Version]
- Brown, S.H.; Gregory, D.E.; Carr, J.A.; Ward, S.R.; Masuda, K.; Lieber, R.L. ISSLS prize winner: Adaptations to the multifidus muscle in response to experimentally induced intervertebral disc degeneration. Spine 2011, 36, 1728–1736. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.; Holm, A.K.; Hansson, T.; Holm, S. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine 2006, 31, 2926–2933. [Google Scholar] [CrossRef]
- Hodges, P.W.; Galea, M.P.; Holm, S.; Holm, A.K. Corticomotor excitability of back muscles is affected by intervertebral disc lesion in pigs. Eur. J. Neurosci. 2009, 29, 1490–1500. [Google Scholar] [CrossRef]
- Hodges, P.W.; James, G.; Blomster, L.; Hall, L.; Schmid, A.B.; Shu, C.; Little, C.; Melrose, J. Can proinflammatory cytokine gene expression explain multifidus muscle fiber changes after an intervertebral disc lesion? Spine 2014, 39, 1010–1017. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W.; James, G.; Blomster, L.; Hall, L.; Schmid, A.; Shu, C.; Little, C.; Melrose, J. Multifidus Muscle Changes After Back Injury Are Characterized by Structural Remodeling of Muscle, Adipose and Connective Tissue, but Not Muscle Atrophy: Molecular and Morphological Evidence. Spine 2015, 40, 1057–1071. [Google Scholar] [CrossRef]
- James, G.; Blomster, L.; Hall, L.; Schmid, A.B.; Shu, C.C.; Little, C.B.; Melrose, J.; Hodges, P.W. Mesenchymal Stem Cell Treatment of Intervertebral Disc Lesion Prevents Fatty Infiltration and Fibrosis of the Multifidus Muscle, but not Cytokine and Muscle Fiber Changes. Spine 2016, 41, 1208–1217. [Google Scholar] [CrossRef]
- Cooley, J.R.; Walker, B.F.; Ardakani, E.M.; Kjaer, P.; Jensen, T.S.; Hebert, J.J. Relationships between paraspinal muscle morphology and neurocompressive conditions of the lumbar spine: A systematic review with meta-analysis. BMC Musculoskelet. Disord. 2018, 19, 351. [Google Scholar] [CrossRef] [PubMed]
- Pedler, A.; McMahon, K.; Galloway, G.; Durbridge, G.; Sterling, M. Intramuscular fat is present in cervical multifidus but not soleus in patients with chronic whiplash associated disorders. PLoS ONE 2018, 13, e0197438. [Google Scholar] [CrossRef] [PubMed]
- Elliott, J.M.; Courtney, D.M.; Rademaker, A.; Pinto, D.; Sterling, M.M.; Parrish, T.B. The rapid and progressive degeneration of the cervical multifidus in whiplash: A MRI study of fatty infiltration. Spine 2015, 40, E694. [Google Scholar] [CrossRef]
- Burns, E.; Chipchase, L.S.; Schabrun, S.M. Primary sensory and motor cortex function in response to acute muscle pain: A systematic review and meta-analysis. Eur. J. Pain 2016, 20, 1203–1213. [Google Scholar] [CrossRef]
- Chang, W.-J.; Buscemi, V.; Liston, M.B.; McAuley, J.H.; Hodges, P.W.; Schabrun, S.M. Sensorimotor cortical activity in acute low back pain: A cross-sectional study. J. Pain 2019, 20, 819–829. [Google Scholar] [CrossRef]
- Meier, M.L.; Vrana, A.; Schweinhardt, P. Low Back Pain: The Potential Contribution of Supraspinal Motor Control and Proprioception. Neuroscientist 2018. [Google Scholar] [CrossRef]
- Christian, G.F.; Stanton, G.J.; Sissons, D.; How, H.Y.; Jamison, J.; Alder, B.; Fullerton, M.; Funder, J.W. Immunoreactive ACTH, beta-endorphin, and cortisol levels in plasma following spinal manipulative therapy. Spine 1988, 13, 1411–1417. [Google Scholar] [CrossRef]
- Luisetto, G.; Spano, D.; Steiner, W.; Tagliaro, F.; Darling, P.; Campacci, R. Plasma Levels of Beta-Endorphin and Calcitonin Before and After Manipulative Treatment of Patients with Cervical Arthrosis and Barre’s Syndrome. In Chiropractic Interprofessional Research; Edizioni Minerva: Torino, Italy, 1982; pp. 47–52. [Google Scholar]
- Tuchin, P.J. The effect of chiropractic spinal manipulative therapy on salivary cortisol levels. Australas. Chiropr. Osteopathy 1998, 7, 86. [Google Scholar]
- Whelan, T.L.; Dishman, J.D.; Burke, J.; Levine, S.; Sciotti, V. The effect of chiropractic manipulation on salivary cortisol levels. J. Manip. Physiol. Ther. 2002, 25, 149–153. [Google Scholar] [CrossRef]
- Puhl, A.A.; Injeyan, H.S. Short-term effects of manipulation to the upper thoracic spine of asymptomatic subjects on plasma concentrations of epinephrine and norepinephrine-a randomized and controlled observational study. J. Manip. Physiol. Ther. 2012, 35, 209–215. [Google Scholar] [CrossRef]
- Kovanur-Sampath, K.; Mani, R.; Cotter, J.; Gisselman, A.S.; Tumilty, S. Changes in biochemical markers following spinal manipulation-a systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2017, 29, 120–131. [Google Scholar] [CrossRef]
- Colombi, A.; Testa, M. The Effects Induced by Spinal Manipulative Therapy on the Immune and Endocrine Systems. Medicina 2019, 55, 448. [Google Scholar] [CrossRef]
- Pothoulakis, C.; Castagliuolo, I.; Leeman, S.E. Neuroimmune Mechanisms of Intestinal Responses to Stress: Role of Corticotropin-Releasing Factor and Neurotensin. Ann. N. Y. Acad. Sci. 1998, 840, 635–648. [Google Scholar] [CrossRef]
- Tyler-McMahon, B.M.; Boules, M.; Richelson, E. Neurotensin: Peptide for the next millennium. Regul. Pept. 2000, 93, 125–136. [Google Scholar] [CrossRef]
- Kalafatakis, K.; Triantafyllou, K. Contribution of neurotensin in the immune and neuroendocrine modulation of normal and abnormal enteric function. Regul. Pept. 2011, 170, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, L.; Neves, B.M.; Moura, L.; Cruz, M.T.; Carvalho, E. Neurotensin downregulates the pro-inflammatory properties of skin dendritic cells and increases epidermal growth factor expression. Biochim. Biophys. Acta BBA Mol. Cell Res. 2011, 1813, 1863–1871. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Wang, P.; Wang, S.C.; Wang, Y.-F. Approaches mediating oxytocin regulation of the immune system. Front. Immunol. 2017, 7, 693. [Google Scholar] [CrossRef] [PubMed]
- Insel, T.R. The challenge of translation in social neuroscience: A review of oxytocin, vasopressin, and affiliative behavior. Neuron 2010, 65, 768–779. [Google Scholar] [CrossRef]
- Mashaghi, A.; Marmalidou, A.; Tehrani, M.; Grace, P.M.; Pothoulakis, C.; Dana, R. Neuropeptide substance P and the immune response. Cell. Mol. Life Sci. 2016, 73, 4249–4264. [Google Scholar] [CrossRef] [PubMed]
- Johnson, M.; Young, A.D.; Marriott, I. The therapeutic potential of targeting substance P/NK-1R interactions in inflammatory CNS disorders. Front. Cell. Neurosci. 2017, 10, 296. [Google Scholar] [CrossRef] [PubMed]
- Vink, R.; Gabrielian, L.; Thornton, E. The role of substance P in secondary pathophysiology after traumatic brain injury. Front. Neurol. 2017, 8, 304. [Google Scholar] [CrossRef]
- Roviš, D.; Vasiljev, V.; Jenko-Pražnikar, Z.; Petelin, A.; Drevenšek, G.; Peruč, D.; Černelič-Bizjak, M. Mental health and drug use severity: The role of substance P, neuropeptide Y, self-reported childhood history of trauma, parental bonding and current resiliency. J. Ment. Health 2021, 30, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Buckingham, J.C.; Loxley, H.D.; Christian, H.C.; Philip, J.G. Activation of the HPA axis by immune insults: Roles and interactions of cytokines, eicosanoids, and glucocorticoids. Pharmacol. Biochem. Behav. 1996, 54, 285–298. [Google Scholar] [CrossRef]
- Chrousos, G.P. The hypothalamic–pituitary–adrenal axis and immune-mediated inflammation. N. Engl. J. Med. 1995, 332, 1351–1363. [Google Scholar] [CrossRef]
- Godbout, J.P.; Glaser, R. Stress-induced immune dysregulation: Implications for wound healing, infectious disease and cancer. J. Neuroimmune Pharmacol. 2006, 1, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Herkenham, M.; Kigar, S.L. Contributions of the adaptive immune system to mood regulation: Mechanisms and pathways of neuroimmune interactions. Prog. Neuro Psychopharmacol. Biol. Psychiatry 2017, 79, 49–57. [Google Scholar] [CrossRef]
- Mulla, A.; Buckingham, J.C. Regulation of the hypothalamo–pituitary–adrenal axis by cytokines. Best Pract. Res. Clin. Endocrinol. Metab. 1999, 13, 503–521. [Google Scholar] [CrossRef]
- Dedovic, K.; Duchesne, A.; Andrews, J.; Engert, V.; Pruessner, J.C. The brain and the stress axis: The neural correlates of cortisol regulation in response to stress. Neuroimage 2009, 47, 864–871. [Google Scholar] [CrossRef]
- Blackburn-Munro, G.; Blackburn-Munro, R. Pain in the brain: Are hormones to blame? Trends Endocrinol. Metab. 2003, 14, 20–27. [Google Scholar] [CrossRef]
- McEwen, B.S.; Kalia, M. The role of corticosteroids and stress in chronic pain conditions. Metabolism 2010, 59, S9–S15. [Google Scholar] [CrossRef] [PubMed]
- Fries, E.; Hesse, J.; Hellhammer, J.; Hellhammer, D.H. A new view on hypocortisolism. Psychoneuroendocrinology 2005, 30, 1010–1016. [Google Scholar] [CrossRef] [PubMed]
- Heim, C.; Ehlert, U.; Hellhammer, D.H. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology 2000, 25, 1–35. [Google Scholar] [CrossRef]
- Sorrells, S.F.; Caso, J.R.; Munhoz, C.D.; Sapolsky, R.M. The stressed CNS: When glucocorticoids aggravate inflammation. Neuron 2009, 64, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Banchereau, J.; Pascual, V.; O’garra, A. From IL-2 to IL-37: The expanding spectrum of anti-inflammatory cytokines. Nat. Immunol. 2012, 13, 925. [Google Scholar] [CrossRef]
- Olejniczak, K.A.; Kasprzak, A.A. Biological properties of interleukin 2 and its role in pathogenesis of selected diseases—A review. Med. Sci. Monit. 2008, 14, RA179–RA189. [Google Scholar] [PubMed]
- Evans, D.W. Mechanisms and effects of spinal high-velocity, low-amplitude thrust manipulation: Previous theories. J. Manip. Physiol. Ther. 2002, 25, 251–262. [Google Scholar] [CrossRef]
- Evans, D.W.; Breen, A.C. A biomechanical model for mechanically efficient cavitation production during spinal manipulation: Prethrust position and the neutral zone. J. Manip. Physiol. Ther. 2006, 29, 72–82. [Google Scholar] [CrossRef]
- Reggars, J.W. The therapeutic benefit of the audible release associated with spinal manipulative therapy: A critical review of the literature. Australas. Chiropr. Osteopathy 1998, 7, 80. [Google Scholar] [PubMed]
- Ross, S.H.; Cantrell, D.A. Signaling and function of interleukin-2 in T lymphocytes. Annu. Rev. Immunol. 2018, 36, 411–433. [Google Scholar] [CrossRef]
- Marcovecchio, M.L.; Wicker, L.S.; Dunger, D.B.; Dutton, S.J.; Kopijasz, S.; Scudder, C.; Todd, J.A.; Johnson, P.R. Interleukin-2 Therapy of Autoimmunity in Diabetes (ITAD): A phase 2, multicentre, double-blind, randomized, placebo-controlled trial. Wellcome Open Res. 2020, 5, 49. [Google Scholar] [CrossRef]
- Charych, D.; Khalili, S.; Dixit, V.; Kirk, P.; Chang, T.; Langowski, J.; Rubas, W.; Doberstein, S.K.; Eldon, M.; Hoch, U. Modeling the receptor pharmacology, pharmacokinetics, and pharmacodynamics of NKTR-214, a kinetically-controlled interleukin-2 (IL2) receptor agonist for cancer immunotherapy. PLoS ONE 2017, 12, e0179431. [Google Scholar] [CrossRef]
- Mann, T.K.; Dail, R.B.; Bailey, D.E., Jr. Cognitive and Affective Symptoms Experienced by Cancer Patients Receiving High-Dose Intravenous Interleukin-2 Therapy: An Integrative Literature Review. Cancer Nurs. 2016, 39, 349. [Google Scholar] [CrossRef]
- Hannibal, K.E.; Bishop, M.D. Chronic stress, cortisol dysfunction, and pain: A psychoneuroendocrine rationale for stress management in pain rehabilitation. Phys. Ther. 2014, 94, 1816–1825. [Google Scholar] [CrossRef]
- Balon, J.; Aker, P.D.; Crowther, E.R.; Danielson, C.; Cox, P.G.; O’Shaughnessy, D.; Walker, C.; Goldsmith, C.H.; Duku, E.; Sears, M.R. A Comparison of Active and Simulated Chiropr.actic Manipulation as Adjunctive Treatment for Childhood Asthma. N. Engl. J. Med. 1998, 339, 1013–1020. [Google Scholar] [CrossRef] [PubMed]
- Bronfort, G.; Haas, M.; Evans, R.; Leininger, B.; Triano, J. Effectiveness of manual therapies: The UK evidence report. Chiropr. Osteopat. 2010, 18, 3. [Google Scholar] [CrossRef]
- Hondras, M.A.; Linde, K.; Jones, A.P. Manual therapy for asthma. Cochrane Database Syst Rev. 2002, 4, CD001002. [Google Scholar] [CrossRef]
- Kaminskyj, A.; Frazier, M.; Johnstone, K.; Gleberzon, B.J. Chiropr.actic care for patients with asthma: A systematic review of the literature. J. Can. Chiropr. Assoc. 2010, 54, 24–32. [Google Scholar] [PubMed]
- Ernst, E. Spinal manipulation for asthma: A systematic review of randomised clinical trials. Respir. Med. 2009, 103, 1791–1795. [Google Scholar] [CrossRef] [PubMed]
- Pearce, B.D.; Biron, C.A.; Miller, A.H. Neuroendocrine-immune interactions during viral infections. In Advances in Virus Research; Academic Press: Cambridge, MA, USA, 2001; Volumn 56, pp. 469–513. [Google Scholar]
- Thayer, J.F. Vagal tone and the inflammatory reflex. Cleve Clin. J. Med. 2009, 76, S23–S26. [Google Scholar] [CrossRef] [PubMed]
- Pavlov, V.A.; Wang, H.; Czura, C.J.; Friedman, S.G.; Tracey, K.J. The cholinergic anti-inflammatory pathway: A missing link in neuroimmunomodulation. Mol. Med. 2003, 9, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Felten, S.Y.; Madden, K.S.; Bellinger, D.L.; Kruszewska, B.; Moynihan, J.A.; Felten, D.L. The Role of the Sympathetic Nervous System in the Modulation of Immune Responses. In Advances in Pharmacology; Goldstein, D.S., Eisenhofer, G., McCarty, R., Eds.; Academic Press: Cambridge, MA, USA, 1997; Volumn 42, pp. 583–587. [Google Scholar]
- Kohm, A.P.; Sanders, V.M. Norepinephrine: A messenger from the brain to the immune system. Immunol. Today 2000, 21, 539–542. [Google Scholar] [CrossRef]
- Kiecolt-Glaser, J.K.; Gouin, J.-P.; Hantsoo, L. Close relationships, inflammation, and health. Neurosci. Biobehav. Rev. 2010, 35, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Pavlov, V.A.; Tracey, K.J. The vagus nerve and the inflammatory reflex—linking immunity and metabolism. Nat. Rev. Endocrinol. 2012, 8, 743. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 2019, 56, 774–786. [Google Scholar] [CrossRef]
- Dube, S.R.; Fairweather, D.; Pearson, W.S.; Felitti, V.J.; Anda, R.F.; Croft, J.B. Cumulative childhood stress and autoimmune diseases in adults. Psychosom. Med. 2009, 71, 243. [Google Scholar] [CrossRef]
- Naudé, P.J.; Roest, A.M.; Stein, D.J.; de Jonge, P.; Doornbos, B. Anxiety disorders and CRP in a population cohort study with 54,326 participants: The LifeLines study. World J. Biol. Psychiatry 2018, 19, 461–470. [Google Scholar] [CrossRef]
- White, J.; Kivimäki, M.; Jokela, M.; Batty, G.D. Association of inflammation with specific symptoms of depression in a general population of older people: The English Longitudinal Study of Ageing. Brain Behav. Immun. 2017, 61, 27–30. [Google Scholar] [CrossRef]
- Melhem, N.M.; Munroe, S.; Marsland, A.; Gray, K.; Brent, D.; Porta, G.; Douaihy, A.; Laudenslager, M.L.; DePietro, F.; Diler, R. Blunted HPA axis activity prior to suicide attempt and increased inflammation in attempters. Psychoneuroendocrinology 2017, 77, 284–294. [Google Scholar] [CrossRef]
- Leonard, B.E. Inflammation and depression: A causal or coincidental link to the pathophysiology? Acta Neuropsychiatr. 2018, 30, 1–16. [Google Scholar] [CrossRef]
- Köhler-Forsberg, O.; Buttenschøn, H.N.; Tansey, K.E.; Maier, W.; Hauser, J.; Dernovsek, M.Z.; Henigsberg, N.; Souery, D.; Farmer, A.; Rietschel, M. Association between C-reactive protein (CRP) with depression symptom severity and specific depressive symptoms in major depression. Brain Behav. Immun. 2017, 62, 344–350. [Google Scholar] [CrossRef]
- Tayefi, M.; Shafiee, M.; Kazemi-Bajestani, S.M.R.; Esmaeili, H.; Darroudi, S.; Khakpouri, S.; Mohammadi, M.; Ghaneifar, Z.; Azarpajouh, M.R.; Moohebati, M. Depression and anxiety both associate with serum level of hs-CRP: A gender-stratified analysis in a population-based study. Psychoneuroendocrinology 2017, 81, 63–69. [Google Scholar] [CrossRef]
- Tabatabaeizadeh, S.-A.; Abdizadeh, M.F.; Meshkat, Z.; Khodashenas, E.; Darroudi, S.; Fazeli, M.; Ferns, G.A.; Avan, A.; Ghayour-Mobarhan, M. There is an association between serum high-sensitivity C-reactive protein (hs-CRP) concentrations and depression score in adolescent girls. Psychoneuroendocrinology 2018, 88, 102–104. [Google Scholar] [CrossRef]
- Smagula, S.F.; Ancoli-Israel, S.; Barrett-Connor, E.; Lane, N.E.; Redline, S.; Stone, K.L.; Cauley, J.A.; Group, O.F.i.M.R. Inflammation, sleep disturbances, and depressed mood among community-dwelling older men. J. Psychosom. Res. 2014, 76, 368–373. [Google Scholar] [CrossRef]
- Serrats, J.; Grigoleit, J.-S.; Alvarez-Salas, E.; Sawchenko, P.E. Pro-inflammatory immune-to-brain signaling is involved in neuroendocrine responses to acute emotional stress. Brain Behav. Immun. 2017, 62, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Serafini, G.; Pompili, M.; Seretti, M.E.; Stefani, H.; Palermo, M.; Coryell, W.; Girardi, P. The role of inflammatory cytokines in suicidal behavior: A systematic review. Eur. Neuropsychopharmacol. 2013, 23, 1672–1686. [Google Scholar] [CrossRef] [PubMed]
- O’Donovan, A.; Rush, G.; Hoatam, G.; Hughes, B.M.; McCrohan, A.; Kelleher, C.; O’Farrelly, C.; Malone, K.M. Suicidal ideation is associated with elevated inflammation in patients with major depressive disorder. Depress. Anxiety 2013, 30, 307–314. [Google Scholar] [CrossRef]
- Rotenberg, S.; McGrath, J.J. Inter-relation between autonomic and HPA axis activity in children and adolescents. Biol. Psychol. 2016, 117, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Picchiottino, M.; Honoré, M.; Leboeuf-Yde, C.; Gagey, O.; Cottin, F.; Hallman, D.M. The effect of a single spinal manipulation on cardiovascular autonomic activity and the relationship to pressure pain threshold: A randomized, cross-over, sham-controlled trial. Chiropr. Man. Ther. 2020, 28, 7. [Google Scholar] [CrossRef]
- Picchiottino, M.; Leboeuf-Yde, C.; Gagey, O.; Hallman, D.M. The acute effects of joint manipulative techniques on markers of autonomic nervous system activity: A systematic review and meta-analysis of randomized sham-controlled trials. Chiropr. Man. Ther. 2019, 27, 17. [Google Scholar] [CrossRef]
- Kipnis, J. The Seventh Sense. Sci. Am. 2018, 319, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Elenkov, I.J.; Wilder, R.L.; Chrousos, G.P.; Vizi, E.S. The sympathetic nerve—an integrative interface between two supersystems: The brain and the immune system. Pharmacol. Rev. 2000, 52, 595–638. [Google Scholar] [PubMed]
- Baarbé, J.; Yielder, P.; Haavik, H.; Holmes, M.; Debison-Larabie, C.; Murphy, B. Enhanced cerebellar disinhibition when cervical manipulation precedes motor learning in patients with subclinical neck pain. In Proceedings of the WFC 13th Biennial Congress Proceedings, Athens, Greece, 13–16 May 2015; pp. 115–116. [Google Scholar]
- Baarbé, J.K.; Yielder, P.; Haavik, H.; Holmes, M.W.; Murphy, B.A. Subclinical recurrent neck pain and its treatment impacts motor training-induced plasticity of the cerebellum and motor cortex. PLoS ONE 2018, 13, e0193413. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, T.L.; Niazi, I.K.; Holt, K.; Nedergaard, R.W.; Duehr, J.; Allen, K.; Marshall, P.; Türker, K.S.; Hartvigsen, J.; Haavik, H. The effects of a single session of spinal manipulation on strength and cortical drive in athletes. Eur. J. Appl. Physiol. 2018, 118, 737–749. [Google Scholar] [CrossRef]
- Daligadu, J.; Haavik, H.; Yielder, P.; Baarbe, J.; Murphy, B. Alterations in cortical and cerebellar motor processingt in sub-clinical neck pain patients following spinal manipulation. J. Manip. Physiol. Ther. 2013, 36, 10. [Google Scholar]
- Haavik, H.; Murphy, B. Subclinical neck pain and the effects of cervical manipulation on elbow joint position sense. J. Manip. Physiol. Ther. 2011, 34, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Haavik, H.; Murphy, B. The role of spinal manipulation in addressing disordered sensorimotor integration and altered motor control. J. Electromyogr. Kinesiol. 2012, 22, 768–776. [Google Scholar] [CrossRef] [PubMed]
- Haavik, H.; Niazi, I.; Jochumsen, M.; Sherwin, D.; Flavel, S.; Türker, K. Impact of Spinal Manipulation on Cortical Drive to Upper and Lower Limb Muscles. Brain Sci. 2017, 7, 2. [Google Scholar] [CrossRef]
- Haavik, H.; Niazi, I.K.; Holt, K.; Murphy, B. Effects of 12 Weeks of Chiropr.actic Care on Central Integration of Dual Somatosensory Input in Chronic Pain Patients: A Preliminary Study. J. Manip. Physiol. Ther. 2017, 40, 127–138. [Google Scholar] [CrossRef]
- Haavik, H.; Niazi, I.K.; Jochumsen, M.; Uginčius, P.; Sebik, O.; Yılmaz, G.; Navid, M.S.; Özyurt, M.G.; Türker, K.S. Chiropr.actic spinal manipulation alters TMS induced I-wave excitability and shortens the cortical silent period. J. Electromyogr. Kinesiol. 2018, 42, 24–35. [Google Scholar] [CrossRef]
- Haavik Taylor, H.; Murphy, B. Transient modulation of intracortical inhibition following spinal manipulation. Chiropr. J. Aust. 2007, 37, 106–116. [Google Scholar]
- Haavik Taylor, H.; Murphy, B. Altered sensorimotor integration with cervical spine manipulation. J. Manip. Physiol. Ther. 2008, 31, 115–126. [Google Scholar] [CrossRef]
- Haavik Taylor, H.; Murphy, B. Altered Central Integration of Dual Somatosensory Input Following Cervical Spine Manipulation. J. Manip. Physiol. Ther. 2010, 33, 178–188. [Google Scholar] [CrossRef]
- Haavik Taylor, H.; Murphy, B. The effects of spinal manipulation on central integration of dual somatosensory input observed following motor training: A crossover study. J. Manip. Physiol. Ther. 2010, 33, 261–272. [Google Scholar] [CrossRef]
- Haavik Taylor, H.; Murphy, B. Cervical spine manipulation alters sensorimotor integration: A somatosensory evoked potential study. Clin. Neurophysiol. 2007, 118, 391–402. [Google Scholar] [CrossRef]
- Holt, K.; Haavik, H.; Murphy, B.; Chi Lun Lee, A.; Elley, C. Effectiveness of Chiropr.actic Care to Improve Sensorimotor Function Associated with Falls Risk in Older People: A Randomized Controlled Trial. J. Manip. Physiol. Ther. 2016, 39, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Holt, K.; Niazi, I.K.; Nedergaard, R.W.; Duehr, J.; Amjad, I.; Shafique, M.; Anwar, M.N.; Ndetan, H.; Turker, K.S.; Haavik, H. The effects of a single session of chiropractic care on strength, cortical drive, and spinal excitability in stroke patients. Sci. Rep. 2019, 9, 2673. [Google Scholar] [CrossRef] [PubMed]
- Lelic, D.; Niazi, I.K.; Holt, K.; Jochumsen, M.; Dremstrup, K.; Yielder, P.; Murphy, B.; Drewes, A.M.; Haavik, H. Manipulation of Dysfunctional Spinal Joints Affects Sensorimotor Integration in the Prefrontal Cortex: A Brain Source Localization Study. Neural Plast. 2016, 2016, 3704964. [Google Scholar] [CrossRef]
- Niazi, I.K.; Türker, K.S.; Flavel, S.; Kinget, M.; Duehr, J.; Haavik, H. Changes in H-reflex and V-waves following spinal manipulation. Exp. Brain Res. 2015, 233, 1165–1173. [Google Scholar] [CrossRef]
- Haavik Taylor, H.; Holt, K.; Murphy, B. Exploring the neuromodulatory effects of the vertebral subluxation and chiropractic care. Chiropr. J. Aust 2010, 40, 37–44. [Google Scholar]
- Du Rose, A.; Breen, A. Relationships between paraspinal muscle activity and lumbar inter-vertebral range of motion. Healthcare 2016, 4, 4. [Google Scholar] [CrossRef] [PubMed]
- Park, K.-N.; Kwon, O.-Y.; Kim, S.-J.; Kim, S.-H. Asymmetry of neck motion and activation of the cervical paraspinal muscles during prone neck extension in subjects with unilateral posterior neck pain. J. Back Musculoskelet. Rehabil. 2017, 30, 751–758. [Google Scholar] [CrossRef]
- Kent, C. Models of vertebral subluxation: A review. J. Vertebr. Subluxation Res. 1996, 1, 1. [Google Scholar]
- Henderson, C.N. The basis for spinal manipulation: Chiropr.actic perspective of indications and theory. J. Electromyogr. Kinesiol. 2012, 22, 632–642. [Google Scholar] [CrossRef]
- Alcantara, J.; Alcantara, J.D.; Alcantara, J. Spinal Subluxation. In Pediatric Chiropractic, 2nd ed.; Anrig, C., Plaugher, G., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013; pp. 27–48. [Google Scholar]
- Baarbe, J.K.; Holmes, M.W.; Murphy, H.E.; Haavik, H.; Murphy, B.A. Influence of Subclinical Neck Pain on the Ability to Perform a Mental Rotation Task: A 4-Week Longitudinal Study With a Healthy Control Group Comparison. J. Manip. Physiol. Ther. 2016, 39, 23–30. [Google Scholar] [CrossRef]
- Faw, B. Pre-frontal executive committee for perception, working memory, attention, long-term memory, motor control, and thinking: A tutorial review. Conscious. Cogn. 2003, 12, 83–139. [Google Scholar] [CrossRef]
- Moench, K.M.; Wellman, C.L. Review article: Stress-induced alterations in prefrontal dendritic spines: Implications for post-traumatic stress disorder. Neurosci. Lett. 2015, 601, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Ahern, G.L.; Sollers, J.J.; Lane, R.D.; Labiner, D.M.; Herring, A.M.; Weinand, M.E.; Hutzler, R.; Thayer, J.F. Heart rate and heart rate variability changes in the intracarotid sodium amobarbital test. Epilepsia 2001, 42, 912–921. [Google Scholar] [CrossRef]
- Berthoud, H.-R.; Neuhuber, W.L. Functional and chemical anatomy of the afferent vagal system. Auton. Neurosci. 2000, 85, 1–17. [Google Scholar] [CrossRef]
- Thayer, J.F.; Sternberg, E.M. Neural aspects of immunomodulation: Focus on the vagus nerve. Brain Behav. Immun. 2010, 24, 1223–1228. [Google Scholar] [CrossRef]
- Bankenahally, R.; Krovvidi, H. Autonomic nervous system: Anatomy, physiology, and relevance in anaesthesia and critical care medicine. BJA Educ. 2016, 16, 381–387. [Google Scholar] [CrossRef]
- Kul’chyns’kyi, A.B.; Kyjenko, V.M.; Zukow, W.; Popovych, I.L. Causal neuro-immune relationships at patients with chronic pyelonephritis and cholecystitis. correlations between parameters EEG, HRV and white blood cell count. Open Med. 2017, 12, 201–213. [Google Scholar] [CrossRef]
- Ohira, H.; Matsunaga, M.; Osumi, T.; Fukuyama, S.; Shinoda, J.; Yamada, J.; Gidron, Y. Vagal nerve activity as a moderator of brain–immune relationships. J. Neuroimmunol. 2013, 260, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Thayer, J.F.; Åhs, F.; Fredrikson, M.; Sollers, J.J.; Wager, T.D. A meta-analysis of heart rate variability and neuroimaging studies: Implications for heart rate variability as a marker of stress and health. Neurosci. Biobehav. Rev. 2012, 36, 747–756. [Google Scholar] [CrossRef]
- McCraty, R.; Shaffer, F. Heart Rate Variability: New Perspectives on Physiological Mechanisms, Assessment of Self-regulatory Capacity, and Health Risk. Glob. Adv. Health Med. 2015, 4, 46–61. [Google Scholar] [CrossRef]
- Hänsel, A.; Von Känel, R. The ventro-medial prefrontal cortex: A major link between the autonomic nervous system, regulation of emotion, and stress reactivity? Biopsychosoc. Med. 2008, 2, 21. [Google Scholar] [CrossRef]
- Diorio, D.; Viau, V.; Meaney, M.J. The role of the medial prefrontal cortex (cingulate gyrus) in the regulation of hypothalamic-pituitary-adrenal responses to stress. J. Neurosci. 1993, 13, 3839–3847. [Google Scholar] [CrossRef]
- Lorenz, J.; Minoshima, S.; Casey, K. Keeping pain out of mind: The role of the dorsolateral prefrontal cortex in pain modulation. Brain 2003, 126, 1079–1091. [Google Scholar] [CrossRef]
- Apkarian, A.V.; Bushnell, M.C.; Treede, R.D.; Zubieta, J.K. Human brain mechanisms of pain perception and regulation in health and disease. Eur. J. Pain: EJP 2005, 9, 463–484. [Google Scholar] [CrossRef] [PubMed]
- Apkarian, A.V.; Sosa, Y.; Sonty, S.; Levy, R.M.; Harden, R.N.; Parrish, T.B.; Gitelman, D.R. Chronic Back Pain Is Associated with Decreased Prefrontal and Thalamic Gray Matter Density. J. Neurosci. 2004, 24, 10410–10415. [Google Scholar] [CrossRef]
- Arnsten, A.F.T.; Raskind, M.A.; Taylor, F.B.; Connor, D.F. blair. Neurobiol. Stress 2015, 1, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Eden, A.S.; Schreiber, J.; Anwander, A.; Keuper, K.; Laeger, I.; Zwanzger, P.; Zwitserlood, P.; Kugel, H.; Dobel, C. Emotion regulation and trait anxiety are predicted by the microstructure of fibers between amygdala and prefrontal cortex. J. Neurosci. 2015, 35, 6020–6027. [Google Scholar] [CrossRef]
- Etkin, A.; Büchel, C.; Gross, J.J. The neural bases of emotion regulation. Nat. Rev. Neurosci. 2015, 16, 693. [Google Scholar] [CrossRef]
- Ghosal, S.; Hare, B.D.; Duman, R.S. Prefrontal cortex GABAergic deficits and circuit dysfunction in the pathophysiology and treatment of chronic stress and depression. Curr. Opin. Behav. Sci. 2017, 14, 1–8. [Google Scholar] [CrossRef]
- Johnston-Wilson, N.L.; Sims, C.D.; Hofmann, J.P.; Anderson, L.; Shore, A.D.; Torrey, E.F.; Yolken, R.H. Disease-specific alterations in frontal cortex brain proteins in schizophrenia, bipolar disorder, and major depressive disorder. Mol. Psychiatry 2000, 5, 142. [Google Scholar] [CrossRef]
- Motzkin, J.C.; Philippi, C.L.; Wolf, R.C.; Baskaya, M.K.; Koenigs, M. Ventromedial prefrontal cortex is critical for the regulation of amygdala activity in humans. Biol. Psychiatry 2015, 77, 276–284. [Google Scholar] [CrossRef]
- Kawli, T.; He, F.; Tan, M.-W. It takes nerves to fight infections: Insights on neuro-immune interactions from C. elegans. Dis. Models Mech. 2010, 3, 721–731. [Google Scholar] [CrossRef]
- Godinho-Silva, C.; Cardoso, F.; Veiga-Fernandes, H. Neuro–immune cell units: A new paradigm in physiology. Annu. Rev. Immunol. 2019, 37, 19–46. [Google Scholar] [CrossRef] [PubMed]
- Sanders, V.M.; Kohm, A.P. Sympathetic nervous system interaction with the immune system. Int. Rev. Neurobiol. 2002, 52, 17–41. [Google Scholar] [PubMed]
- Sternberg, E.M. Neural regulation of innate immunity: A coordinated nonspecific host response to pathogens. Nat. Rev. Immunol. 2006, 6, 318–328. [Google Scholar] [CrossRef]
- Louveau, A.; Herz, J.; Alme, M.N.; Salvador, A.F.; Dong, M.Q.; Viar, K.E.; Herod, S.G.; Knopp, J.; Setliff, J.C.; Lupi, A.L. CNS lymphatic drainage and neuroinflammation are regulated by meningeal lymphatic vasculature. Nat. Neurosci. 2018, 21, 1380–1391. [Google Scholar] [CrossRef] [PubMed]
- Chiu, I.M.; Heesters, B.A.; Ghasemlou, N.; Von Hehn, C.A.; Zhao, F.; Tran, J.; Wainger, B.; Strominger, A.; Muralidharan, S.; Horswill, A.R. Bacteria activate sensory neurons that modulate pain and inflammation. Nature 2013, 501, 52–57. [Google Scholar] [CrossRef]
- Schiller, M.; Ben-Shaanan, T.L.; Rolls, A. Neuronal regulation of immunity: Why, how and where? Nat. Rev. Immunol 2020. [Google Scholar] [CrossRef]
- Dantzer, R. Neuroimmune interactions: From the brain to the immune system and vice versa. Physiol. Rev. 2018, 98, 477–504. [Google Scholar] [CrossRef] [PubMed]
- Kamimura, D.; Ohki, T.; Arima, Y.; Ota, M.; Murakami, M. Gateway reflex: Local neuroimmune interactions that regulate blood vessels. Neurochem. Int. 2019, 130, 104303. [Google Scholar] [CrossRef]
- Imeri, L.; Opp, M.R. How (and why) the immune system makes us sleep. Nat. Rev. Neurosci. 2009, 10, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Krueger, J.M. The role of cytokines in sleep regulation. Curr. Pharm. Des. 2008, 14, 3408–3416. [Google Scholar] [CrossRef] [PubMed]
- Ahima, R.S.; Antwi, D.A. Brain regulation of appetite and satiety. Endocrinol. Metab. Clin. N. Am. 2008, 37, 811–823. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, J.B.; Johnson, R.W. Regulation of food intake by inflammatory cytokines in the brain. Neuroendocrinology 2007, 86, 183–190. [Google Scholar] [CrossRef]
- Marin, I.; Kipnis, J. Learning and memory and the immune system. Learn. Mem. 2013, 20, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Filiano, A.J.; Xu, Y.; Tustison, N.J.; Marsh, R.L.; Baker, W.; Smirnov, I.; Overall, C.C.; Gadani, S.P.; Turner, S.D.; Weng, Z. Unexpected role of interferon-γ in regulating neuronal connectivity and social behaviour. Nature 2016, 535, 425–429. [Google Scholar] [CrossRef]
- Bay-Richter, C.; Janelidze, S.; Hallberg, L.; Brundin, L. Changes in behaviour and cytokine expression upon a peripheral immune challenge. Behav. Brain Res. 2011, 222, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Müller, N.; Riedel, M.; Gruber, R.; Ackenheil, M.; Schwarz, M.J. The immune system and schizophrenia: An integrative view. Ann. N. Y. Acad. Sci. 2000, 917, 456–467. [Google Scholar] [CrossRef]
- Heppner, F.L.; Ransohoff, R.M.; Becher, B. Immune attack: The role of inflammation in Alzheimer disease. Nat. Rev. Neurosci. 2015, 16, 358–372. [Google Scholar] [CrossRef] [PubMed]
- Enck, P.; Benedetti, F.; Schedlowski, M. New insights into the placebo and nocebo responses. Neuron 2008, 59, 195–206. [Google Scholar] [CrossRef]
- Benedetti, F. Placebo Effects; Oxford University Press: New York, NY, USA, 2014. [Google Scholar]
- Wong, C.H.; Jenne, C.N.; Lee, W.-Y.; Léger, C.; Kubes, P. Functional innervation of hepatic iNKT cells is immunosuppressive following stroke. Science 2011, 334, 101–105. [Google Scholar] [CrossRef]
- Miller, H.; Tilston, J.; Langhorne, P.; Stott, D.J. Risk Factors for Chest Infection in Acute Stroke. Stroke 2007, 38, 2284–2291. [Google Scholar]
- Moshel, Y.A.; Durkin, H.G.; Amassian, V.E. Lateralized neocortical control of T lymphocyte export from the thymus: I. Increased export after left cortical stimulation in behaviorally active rats, mediated by sympathetic pathways in the upper spinal cord. J. Neuroimmunol. 2005, 158, 3–13. [Google Scholar] [CrossRef]
- Neveu, P.; Barnéoud, P.; Vitiello, S.; Betancur, C.; Le Moal, M. Brain modulation of the immune system: Association between lymphocyte responsiveness and paw preference in mice. Brain Res. 1988, 457, 392–394. [Google Scholar] [CrossRef]
- Betancur, C.; Neveu, P.J.; Vitiello, S.; Le Moal, M. Natural killer cell activity is associated with brain asymmetry in male mice. Brain Behav. Immun. 1991, 5, 162–169. [Google Scholar] [CrossRef]
- Neveu, P. Asymmetrical brain modulation of the immune response. Brain Res. Rev. 1992, 17, 101–107. [Google Scholar] [CrossRef]
- Tarkowski, E.; Ekelund, P.; Tarkowski, A. Enhancement of antigen-specific T-cell reactivity on the affected side in stroke patients. J. Neuroimmunol. 1991, 34, 61–67. [Google Scholar] [CrossRef]
- Wittling, W.; Block, A.; Schweiger, E.; Genzel, S. Hemisphere asymmetry in sympathetic control of the human myocardium. Brain Cogn. 1998, 38, 17–35. [Google Scholar] [CrossRef]
- Meyer, S.; Strittmatter, M.; Fischer, C.; Georg, T.; Schmitz, B. Lateralization in autononic dysfunction in ischemic stroke involving the insular cortex. Neuroreport 2004, 15, 357–361. [Google Scholar] [CrossRef]
- Guo, C.C.; Sturm, V.E.; Zhou, J.; Gennatas, E.D.; Trujillo, A.J.; Hua, A.Y.; Crawford, R.; Stables, L.; Kramer, J.H.; Rankin, K. Dominant hemisphere lateralization of cortical parasympathetic control as revealed by frontotemporal dementia. Proc. Natl. Acad. Sci. USA 2016, 113, E2430–E2439. [Google Scholar] [CrossRef] [PubMed]
- Wittling, W.; Block, A.; Genzel, S.; Schweiger, E. Hemisphere asymmetry in parasympathetic control of the heart. Neuropsychologia 1998, 36, 461–468. [Google Scholar] [CrossRef]
- Aich, P.; Potter, A.A.; Griebel, P.J. Modern approaches to understanding stress and disease susceptibility: A review with special emphasis on respiratory disease. Int. J. Gen. Med. 2009, 2, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Dorshkind, K.; Horseman, N.D. Anterior pituitary hormones, stress, and immune system homeostasis. BioEssays 2001, 23, 288–294. [Google Scholar] [CrossRef]
- Leonard, B.E. HPA and Immune Axes in Stress: Involvement of the Serotonergic System. Neuroimmunomodulation 2006, 13, 268–276. [Google Scholar] [CrossRef] [PubMed]
- Meisel, C.; Schwab, J.M.; Prass, K.; Meisel, A.; Dirnagl, U. Central nervous system injury-induced immune deficiency syndrome. Nat. Rev. Neurosci. 2005, 6, 775–786. [Google Scholar] [CrossRef]
- Piedimonte, G. Contribution of neuroimmune mechanisms to airway inflammation and remodeling during and after respiratory syncytial virus infection. Pediatr. Infect. Dis. J. 2003, 22, S66–S75. [Google Scholar] [CrossRef] [PubMed]
- Shimada, A.; Yokota, T. Physiological and pathological brain-immune system interactions. Clin. Exp. Neuroimmunol. 2020, 11, 3–4. [Google Scholar] [CrossRef]
- Silverman, M.N.; Pearce, B.D.; Biron, C.A.; Miller, A.H. Immune modulation of the hypothalamic-pituitary-adrenal (HPA) axis during viral infection. Viral Immunol. 2005, 18, 41–78. [Google Scholar] [CrossRef]
- Sharma, H.S.; Winkler, T.; Stålberg, E.; Mohanty, S.; Westman, J. p-Chlorophenylalanine, an inhibitor of serotonin synthesis reduces blood-brain barrier permeability, cerebral blood flow, edema formation and cell injury following trauma to the rat brain. In Brain Edema XI; Springer: Berlin/Heidelberg, Germany, 2000; pp. 91–95. [Google Scholar]
- Korin, B.; Avraham, S.; Azulay-Debby, H.; Farfara, D.; Hakim, F.; Rolls, A. Short-term sleep deprivation in mice induces B cell migration to the brain compartment. Sleep 2020, 43, zsz222. [Google Scholar] [CrossRef]
- Kertser, A.; Baruch, K.; Deczkowska, A.; Weiner, A.; Croese, T.; Kenigsbuch, M.; Cooper, I.; Tsoory, M.; Ben-Hamo, S.; Amit, I. Corticosteroid signaling at the brain-immune interface impedes coping with severe psychological stress. Sci. Adv. 2019, 5, eaav4111. [Google Scholar] [CrossRef]
- Liu, Y.U.; Ying, Y.; Li, Y.; Eyo, U.B.; Chen, T.; Zheng, J.; Umpierre, A.D.; Zhu, J.; Bosco, D.B.; Dong, H. Neuronal network activity controls microglial process surveillance in awake mice via norepinephrine signaling. Nat. Neurosci. 2019, 22, 1–11. [Google Scholar] [CrossRef]
- Stowell, R.D.; Sipe, G.O.; Dawes, R.P.; Batchelor, H.N.; Lordy, K.A.; Whitelaw, B.S.; Stoessel, M.B.; Bidlack, J.M.; Brown, E.; Sur, M. Noradrenergic signaling in the wakeful state inhibits microglial surveillance and synaptic plasticity in the mouse visual cortex. Nat. Neurosci. 2019, 22, 1782–1792. [Google Scholar] [CrossRef]
- Van Wagoner, N.J.; Benveniste, E.N. Interleukin-6 expression and regulation in astrocytes. J. Neuroimmunol. 1999, 100, 124–139. [Google Scholar] [CrossRef]
- Cannella, B.; Raine, C.S. Multiple sclerosis: Cytokine receptors on oligodendrocytes predict innate regulation. Ann. Neurol. 2004, 55, 46–57. [Google Scholar] [CrossRef]
- Vezzani, A.; Viviani, B. Neuromodulatory properties of inflammatory cytokines and their impact on neuronal excitability. Neuropharmacology 2015, 96, 70–82. [Google Scholar] [CrossRef]
- Cámara-Lemarroy, C.R.; Cordero-Perez, P.; Ibarra-Hernandez, J.M.; Muñoz-Espinosa, L.E.; Fernandez-Garza, N.E. Gemfibrozil attenuates the inflammatory response and protects rats from abdominal sepsis. Exp. Ther. Med. 2015, 9, 1018–1022. [Google Scholar] [CrossRef]
- Budd, A.; Alleva, L.; Alsharifi, M.; Koskinen, A.; Smythe, V.; Müllbacher, A.; Wood, J.; Clark, I. Increased survival after gemfibrozil treatment of severe mouse influenza. Antimicrob. Agents Chemother. 2007, 51, 2965–2968. [Google Scholar] [CrossRef] [PubMed]
- Demas, G.E. The energetics of immunity: A neuroendocrine link between energy balance and immune function. Horm. Behav. 2004, 45, 173–180. [Google Scholar] [CrossRef]
- Derting, T.L.; Compton, S. Immune response, not immune maintenance, is energetically costly in wild white-footed mice (Peromyscus leucopus). Physiol. Biochem. Zool. 2003, 76, 744–752. [Google Scholar] [CrossRef] [PubMed]
- Muehlenbein, M.P.; Hirschtick, J.L.; Bonner, J.Z.; Swartz, A.M. Toward quantifying the usage costs of human immunity: Altered metabolic rates and hormone levels during acute immune activation in men. Am. J. Hum. Biol. J. Hum. Biol. Assoc. 2010, 22, 546–556. [Google Scholar] [CrossRef]
- Gillette, M.U.; Tischkau, S.A. Suprachiasmatic nucleus: The brain’s circadian clock. Recent Prog. Horm. Res. 1999, 54, 33–58. [Google Scholar] [PubMed]
- Scheiermann, C.; Kunisaki, Y.; Frenette, P.S. Circadian control of the immune system. Nat. Rev. Immunol. 2013, 13, 190–198. [Google Scholar] [CrossRef]
- Druzd, D.; Matveeva, O.; Ince, L.; Harrison, U.; He, W.; Schmal, C.; Herzel, H.; Tsang, A.H.; Kawakami, N.; Leliavski, A. Lymphocyte circadian clocks control lymph node trafficking and adaptive immune responses. Immunity 2017, 46, 120–132. [Google Scholar] [CrossRef]
- Allen, G.V.; Saper, C.B.; Hurley, K.M.; Cechetto, D.F. Organization of visceral and limbic connections in the insular cortex of the rat. J. Comp. Neurol. 1991, 311, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Craig, A.D. Interoception: The sense of the physiological condition of the body. Curr. Opin. Neurobiol. 2003, 13, 500–505. [Google Scholar] [CrossRef]
- Pacheco-López, G.; Niemi, M.-B.; Kou, W.; Härting, M.; Fandrey, J.; Schedlowski, M. Neural substrates for behaviorally conditioned immunosuppression in the rat. J. Neurosci. 2005, 25, 2330–2337. [Google Scholar] [CrossRef]
- Ader, R.; Cohen, N. Behaviorally conditioned immunosuppression. Psychosom. Med. 1975, 37, 333–340. [Google Scholar] [CrossRef]
- Hyman, S.E.; Malenka, R.C.; Nestler, E.J. Neural mechanisms of addiction: The role of reward-related learning and memory. Annu. Rev. Neurosci. 2006, 29, 565–598. [Google Scholar] [CrossRef]
- Russo, S.J.; Nestler, E.J. The brain reward circuitry in mood disorders. Nat. Rev. Neurosci. 2013, 14, 609–625. [Google Scholar] [CrossRef] [PubMed]
- Tsai, H.-C.; Zhang, F.; Adamantidis, A.; Stuber, G.D.; Bonci, A.; De Lecea, L.; Deisseroth, K. Phasic firing in dopaminergic neurons is sufficient for behavioral conditioning. Science 2009, 324, 1080–1084. [Google Scholar] [CrossRef]
- Ben-Shaanan, T.L.; Azulay-Debby, H.; Dubovik, T.; Starosvetsky, E.; Korin, B.; Schiller, M.; Green, N.L.; Admon, Y.; Hakim, F.; Shen-Orr, S.S. Activation of the reward system boosts innate and adaptive immunity. Nat. Med. 2016, 22, 940–944. [Google Scholar] [CrossRef] [PubMed]
- Pinho-Ribeiro, F.A.; Verri, W.A., Jr.; Chiu, I.M. Nociceptor sensory neuron–immune interactions in pain and inflammation. Trends Immunol. 2017, 38, 5–19. [Google Scholar] [CrossRef]
- Hoffman, K.E.; Maslonek, K.A.; Dykstra, L.A.; Lysle, D.T. Effects of central administration of morphine on immune status in Lewis and Wistar rats. In The Brain Immune Axis and Substance Abuse; Springer: Berlin/Heidelberg, Germany, 1995; pp. 155–159. [Google Scholar]
- Gomez-Flores, R.; Weber, R.J. Inhibition of interleukin-2 production and downregulation of IL-2 and transferrin receptors on rat splenic lymphocytes following PAG morphine administration: A role in natural killer and T cell suppression. J. Interferon Cytokine Res. 1999, 19, 625–630. [Google Scholar] [CrossRef]
- Gomez-Flores, R.; Suo, J.; Weber, R.J. Suppression of splenic macrophage functions following acute morphine action in the rat mesencephalon periaqueductal gray. Brain Behav. Immun. 1999, 13, 212–224. [Google Scholar] [CrossRef] [PubMed]
- Demetrikopoulos, M.K.; Siegel, A.; Schleifer, S.J.; Obedi, J.; Keller, S.E. Electrical stimulation of the dorsal midbrain periaqueductal gray suppresses peripheral blood natural killer cell activity. Brain Behav. Immun. 1994, 8, 218–228. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bushnell, M.C.; Čeko, M.; Low, L.A. Cognitive and emotional control of pain and its disruption in chronic pain. Nat. Rev. Neurosci. 2013, 14, 502–511. [Google Scholar] [CrossRef]
- Dhabhar, F.S.; Malarkey, W.B.; Neri, E.; McEwen, B.S. Stress-induced redistribution of immune cells—From barracks to boulevards to battlefields: A tale of three hormones–Curt Richter Award Winner. Psychoneuroendocrinology 2012, 37, 1345–1368. [Google Scholar] [CrossRef]
- Schedlowski, M.; Jacobs, R.; Stratmann, G.; Richter, S.; Hädicke, A.; Tewes, U.; Wagner, T.O.; Schmidt, R.E. Changes of natural killer cells during acute psychological stress. J. Clin. Immunol. 1993, 13, 119–126. [Google Scholar] [CrossRef]
- Nance, D.M.; Sanders, V.M. Autonomic innervation and regulation of the immune system (1987–2007). Brain Behav. Immun. 2007, 21, 736–745. [Google Scholar] [CrossRef]
- Elmquist, J.K.; Scammell, T.E.; Jacobson, C.D.; Saper, C.B. Distribution of Fos-like immunoreactivity in the rat brain following intravenous lipopolysaccharide administration. J. Comp. Neurol. 1996, 371, 85–103. [Google Scholar] [CrossRef]
- Soto-Tinoco, E.; Guerrero-Vargas, N.N.; Buijs, R.M. Interaction between the hypothalamus and the immune system. Exp. Physiol. 2016, 101, 1463–1471. [Google Scholar] [CrossRef] [PubMed]
- Hefco, V.; Olariu, A.; Hefco, A.; Nabeshima, T. The modulator role of the hypothalamic paraventricular nucleus on immune responsiveness. Brain Behav. Immun. 2004, 18, 158–165. [Google Scholar] [CrossRef]
- Sakic, B.; Vlajkovic, S. Self-stimulation behavior: Consequences upon immunity? Brain Behav. Immun. 1990, 4, 255–264. [Google Scholar] [CrossRef]
- Wrona, D.; Jurkowski, M.; Luszawska, D.; Tokarski, J.; Trojniar, W. The effects of lateral hypothalamic lesions on peripheral blood natural killer cell cytotoxicity in rats hyper-and hyporesponsive to novelty. Brain Behav. Immun. 2003, 17, 453–461. [Google Scholar] [CrossRef]
- Churchland, P.S.; Winkielman, P. Modulating social behavior with oxytocin: How does it work? What does it mean? Horm. Behav. 2012, 61, 392–399. [Google Scholar] [CrossRef]
- Neumann, I.D. Brain oxytocin: A key regulator of emotional and social behaviours in both females and males. J. Neuroendocrinol. 2008, 20, 858–865. [Google Scholar] [CrossRef] [PubMed]
- Boone, M.; Deen, P.M. Physiology and pathophysiology of the vasopressin-regulated renal water reabsorption. Pflügers Arch. Eur. J. Physiol. 2008, 456, 1005. [Google Scholar] [CrossRef]
- Butterworth, M.; McClellan, B.; Aklansmith, M. Influence of sex on immunoglobulin levels. Nature 1967, 214, 1224–1225. [Google Scholar] [CrossRef] [PubMed]
- Von Haam, E.; Rosenfeld, I. The effect of estrone on antibody-production. J. Immunol. 1942, 43, 109–117. [Google Scholar]
- Mangalam, A.K.; Taneja, V.; David, C.S. HLA class II molecules influence susceptibility versus protection in inflammatory diseases by determining the cytokine profile. J. Immunol. 2013, 190, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Ngo, S.T.; Steyn, F.J.; McCombe, P.A. Gender differences in autoimmune disease. Front. Neuroendocrinol. 2014, 35, 347–369. [Google Scholar] [CrossRef]
- Barreiro Arcos, M.a.L.; Gorelik, G.; Klecha, A.; Genaro, A.M.; Cremaschi, G.A. Thyroid hormones increase inducible nitric oxide synthase gene expression downstream from PKC-ζ in murine tumor T lymphocytes. Am. J. Physiol. Cell Physiol. 2006, 291, C327–C336. [Google Scholar] [CrossRef][Green Version]
- Klecha, A.J.; Genaro, A.M.; Gorelik, G.; Arcos, M.L.B.; Silberman, D.M.; Schuman, M.; Garcia, S.I.; Pirola, C.; Cremaschi, G.A. Integrative study of hypothalamus–pituitary–thyroid–immune system interaction: Thyroid hormone-mediated modulation of lymphocyte activity through the protein kinase C signaling pathway. J. Endocrinol. 2006, 189, 45–55. [Google Scholar] [CrossRef]
- Tan, T.L.; Rajeswaran, H.; Haddad, S.; Shahi, A.; Parvizi, J. Increased risk of periprosthetic joint infections in patients with hypothyroidism undergoing total joint arthroplasty. J. Arthroplast. 2016, 31, 868–871. [Google Scholar] [CrossRef] [PubMed]
- Nóbrega, M.M.; Auge, A.P.F.; de Toledo, L.G.M.; da Silva Carramão, S.; Frade, A.B.; Salles, M.J.C. Bacteriuria and urinary tract infection after female urodynamic studies: Risk factors and microbiological analysis. Am. J. Infect. Control. 2015, 43, 1035–1039. [Google Scholar] [CrossRef]
- Baker, E.; Lui, F. Neuroanatomy, Vagal Nerve Nuclei (Nucleus Vagus); StatPearls [Internet]: Treasure Island, FL, USA, 2019. [Google Scholar]
- Guyenet, P.G. The sympathetic control of blood pressure. Nat. Rev. Neurosci. 2006, 7, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Samuels, E.; Szabadi, E. Functional neuroanatomy of the noradrenergic locus coeruleus: Its roles in the regulation of arousal and autonomic function part II: Physiological and pharmacological manipulations and pathological alterations of locus coeruleus activity in humans. Curr. Neuropharmacol. 2008, 6, 254–285. [Google Scholar] [CrossRef]
- Jansen, A.S.; Van Nguyen, X.; Karpitskiy, V.; Mettenleiter, T.C.; Loewy, A.D. Central command neurons of the sympathetic nervous system: Basis of the fight-or-flight response. Science 1995, 270, 644–646. [Google Scholar] [CrossRef] [PubMed]
- Kanbar, R.; Depuy, S.D.; West, G.H.; Stornetta, R.L.; Guyenet, P.G. Regulation of visceral sympathetic tone by A5 noradrenergic neurons in rodents. J. Physiol. 2011, 589, 903–917. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Matsumura, K.; Kaneko, T.; Kobayashi, S.; Katoh, H.; Negishi, M. The rostral raphe pallidus nucleus mediates pyrogenic transmission from the preoptic area. J. Neurosci. 2002, 22, 4600–4610. [Google Scholar] [CrossRef]
- Morrison, S.F.; Sved, A.F.; Passerin, A.M. GABA-mediated inhibition of raphe pallidus neurons regulates sympathetic outflow to brown adipose tissue. Am. J. Physiol. Regul. Integr. Comp. Physiol. 1999, 276, R290–R297. [Google Scholar] [CrossRef]
- Navarro, X.; Verdu, E.; Wendelschafer-Crabb, G.; Kennedy, W. Innervation of cutaneous structures in the mouse hind paw: A confocal microscopy immunohistochemical study. J. Neurosci. Res. 1995, 41, 111–120. [Google Scholar] [CrossRef]
- Ishida-Yamamoto, A.; Senba, E.; Tohyama, M. Distribution and fine structure of calcitonin gene-related peptide-like immunoreactive nerve fibers in the rat skin. Brain Res. 1989, 491, 93–101. [Google Scholar] [CrossRef]
- Arnsten, A.F. Stress signalling pathways that impair prefrontal cortex structure and function. Nat. Rev. Neurosci. 2009, 10, 410. [Google Scholar] [CrossRef]
- Amat, J.; Baratta, M.V.; Paul, E.; Bland, S.T.; Watkins, L.R.; Maier, S.F. Medial prefrontal cortex determines how stressor controllability affects behavior and dorsal raphe nucleus. Nat. Neurosci. 2005, 8, 365. [Google Scholar] [CrossRef]
- Arco, A.D.; Mora, F. Neurotransmitters and prefrontal cortex–limbic system interactions: Implications for plasticity and psychiatric disorders. J. Neural Transm. 2009, 116, 941–952. [Google Scholar] [CrossRef]
- Elstad, J.I.; Vabø, M. Job stress, sickness absence and sickness presenteeism in Nordic elderly care. Scand. J. Public Health 2008, 36, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.D.; O’Connor, K.A.; Hansen, M.K.; Watkins, L.R.; Maier, S.F. Effects of prior stress on LPS-induced cytokine and sickness responses. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2003, 284, R422–R432. [Google Scholar] [CrossRef] [PubMed]
- Wulsin, L.R.; Vaillant, G.E.; Wells, V.E. A systematic review of the mortality of depression. Psychosom. Med. 1999, 61, 6–17. [Google Scholar] [CrossRef] [PubMed]
- Eyre, H.; Baune, B.T. Neuroplastic changes in depression: A role for the immune system. Psychoneuroendocrinology 2012, 37, 1397–1416. [Google Scholar] [CrossRef]
- Pittenger, C.; Duman, R.S. Stress, depression, and neuroplasticity: A convergence of mechanisms. Neuropsychopharmacology 2008, 33, 88–109. [Google Scholar] [CrossRef]
- Cohen, S.; Tyrrell, D.A.J.; Smith, A.P. Psychological Stress and Susceptibility to the Common Cold. N. Engl. J. Med. 1991, 325, 606–612. [Google Scholar] [CrossRef]
- Danese, A.; Caspi, A.; Williams, B.; Ambler, A.; Sugden, K.; Mika, J.; Werts, H.; Freeman, J.; Pariante, C.; Moffitt, T. Biological embedding of stress through inflammation processes in childhood. Mol. Psychiatry 2011, 16, 244–246. [Google Scholar] [CrossRef]
- Danese, A.; Moffitt, T.E.; Harrington, H.; Milne, B.J.; Polanczyk, G.; Pariante, C.M.; Poulton, R.; Caspi, A. Adverse childhood experiences and adult risk factors for age-related disease: Depression, inflammation, and clustering of metabolic risk markers. Arch. Pediatr. Adolesc. Med. 2009, 163, 1135–1143. [Google Scholar] [CrossRef]
- Danese, A.; Pariante, C.M.; Caspi, A.; Taylor, A.; Poulton, R. Childhood maltreatment predicts adult inflammation in a life-course study. Proc. Natl. Acad. Sci. USA 2007, 104, 1319–1324. [Google Scholar] [CrossRef] [PubMed]
- Ershler, W.B.; Keller, E.T. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annu. Rev. Med. 2000, 51, 245–270. [Google Scholar] [CrossRef] [PubMed]
- Viswanathan, K.; Dhabhar, F.S. Stress-induced enhancement of leukocyte trafficking into sites of surgery or immune activation. Proc. Natl. Acad. Sci. USA 2005, 102, 5808–5813. [Google Scholar] [CrossRef]
- Dhabhar, F.S.; McEwen, B.S. Acute stress enhances while chronic stress suppresses cell-mediated immunityin vivo: A potential role for leukocyte trafficking. Brain Behav. Immun. 1997, 11, 286–306. [Google Scholar] [CrossRef]
- Dhabhar, F.S. Acute stress enhances while chronic stress suppresses skin immunity: The role of stress hormones and leukocyte trafficking. Ann. N. Y. Acad. Sci. 2000, 917, 876–893. [Google Scholar] [CrossRef]
- Kiecolt-Glaser, J.K.; Glaser, R.; Gravenstein, S.; Malarkey, W.B.; Sheridan, J. Chronic stress alters the immune response to influenza virus vaccine in older adults. Proc. Natl. Acad. Sci. USA 1996, 93, 3043–3047. [Google Scholar] [CrossRef] [PubMed]
- Naliboff, B.D.; Benton, D.; Solomon, G.F.; Morley, J.E.; Fahey, J.L.; Bloom, E.T.; Makinodan, T.; Gilmore, S.L. Immunological changes in young and old adults during brief laboratory stress. Psychosom. Med. 1991, 53, 121–132. [Google Scholar] [CrossRef]
- Cole, S.W. Human social genomics. PLoS Genet. 2014, 10, e1004601. [Google Scholar] [CrossRef]
- Baral, P.; Umans, B.D.; Li, L.; Wallrapp, A.; Bist, M.; Kirschbaum, T.; Wei, Y.; Zhou, Y.; Kuchroo, V.K.; Burkett, P.R. Nociceptor sensory neurons suppress neutrophil and γδ T cell responses in bacterial lung infections and lethal pneumonia. Nat. Med. 2018, 24, 417. [Google Scholar] [CrossRef]
- Kihara, N.; De la Fuente, S.; Fujino, K.; Takahashi, T.; Pappas, T.; Mantyh, C. Vanilloid receptor-1 containing primary sensory neurones mediate dextran sulphate sodium induced colitis in rats. Gut 2003, 52, 713–719. [Google Scholar] [CrossRef]
- McEwen, B.S.; Stellar, E. Stress and the individual: Mechanisms leading to disease. Arch. Intern. Med. 1993, 153, 2093–2101. [Google Scholar] [CrossRef] [PubMed]
- Dirnagl, U.; Klehmet, J.; Braun, J.S.; Harms, H.; Meisel, C.; Ziemssen, T.; Prass, K.; Meisel, A. Stroke-induced immunodepression: Experimental evidence and clinical relevance. Stroke 2007, 38, 770–773. [Google Scholar] [CrossRef] [PubMed]
- Jones, G.; Cale, A. Goal difficulty, anxiety and performance. Ergonomics 1997, 40, 319–333. [Google Scholar] [CrossRef] [PubMed]
- Van Galen, G.P.; van Huygevoort, M. Error, stress and the role of neuromotor noise in space oriented behaviour. Biol. Psychol. 2000, 51, 151–171. [Google Scholar] [CrossRef]
- Weinberg, R.S.; Hunt, V.V. The interrelationships between anxiety, motor performance and electromyography. J. Mot. Behav. 1976, 8, 219–224. [Google Scholar] [CrossRef]
- Marras, W.S.; Davis, K.G.; Heaney, C.A.; Maronitis, A.B.; Allread, W.G. The influence of psychosocial stress, gender, and personality on mechanical loading of the lumbar spine. Spine 2000, 25, 3045–3054. [Google Scholar] [CrossRef]
- Ekberg, K.; Eklund, J.; Tuvesson, M.-A.; Örtengren, R.; Odenrick, P.; Ericson, M. Psychological stress and muscle activity during data entry at visual display units. Work Stress 1995, 9, 475–490. [Google Scholar] [CrossRef]
- Butler, D.; Moseley, G.L. Explain Pain; Noigroup Publications: Adelaide, Australia, 2003. [Google Scholar]
- Shahidi, B.; Haight, A.; Maluf, K. Differential effects of mental concentration and acute psychosocial stress on cervical muscle activity and posture. J. Electromyogr. Kinesiol. 2013, 23, 1082–1089. [Google Scholar] [CrossRef]
- Marker, R.J.; Campeau, S.; Maluf, K.S. Psychosocial stress alters the strength of reticulospinal input to the human upper trapezius. J. Neurophysiol. 2017, 117, 457–466. [Google Scholar] [CrossRef]
- Hellström, F.; Roatta, S.; Thunberg, J.; Passatore, M.; Djupsjöbacka, M. Responses of muscle spindles in feline dorsal neck muscles to electrical stimulation of the cervical sympathetic nerve. Exp. Brain Res. 2005, 165, 328–342. [Google Scholar] [CrossRef]
- Passatore, M.; Roatta, S. Influence of sympathetic nervous system on sensorimotor function: Whiplash associated disorders (WAD) as a model. Eur. J. Appl. Physiol. 2006, 98, 423–449. [Google Scholar] [CrossRef]
- Flor, H.; Birbaumer, N.; Schugens, M.M.; Lutzenberger, W. Symptom-Specific Psychophysiological Responses in Chronic Pain Patients. Psychophysiology 1992, 29, 452–460. [Google Scholar] [CrossRef]
- Vlaeyen, J.W.; Seelen, H.A.; Peters, M.; de Jong, P.; Aretz, E.; Beisiegel, E.; Weber, W.E. Fear of movement/(re) injury and muscular reactivity in chronic low back pain patients: An experimental investigation. Pain 1999, 82, 297–304. [Google Scholar] [CrossRef]
- Hodges, P.W.; Moseley, G.L. Pain and motor control of the lumbopelvic region: Effect and possible mechanisms. J. Electromyogr. Kinesiol. 2003, 13, 361–370. [Google Scholar] [CrossRef]
- Biedermann, H.; Shanks, G.; Forrest, W.; Inglis, J. Power spectrum analyses of electromyographic activity. Discriminators in the differential assessment of patients with chronic low-back pain. Spine 1991, 16, 1179–1184. [Google Scholar] [CrossRef] [PubMed]
- Watson, P.J.; Booker, C.K.; Main, C.J. Evidence for the role of psychological factors in abnormal paraspinal activity in patients with chronic low back pain. J. Musculoskelet. Pain 1997, 5, 41–56. [Google Scholar] [CrossRef]
- Nederhand, M.J.; Hermens, H.J.; IJzerman, M.J.; Groothuis, K.G.; Turk, D.C. The effect of fear of movement on muscle activation in posttraumatic neck pain disability. Clin. J. Pain 2006, 22, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Karayannis, N.V.; Smeets, R.J.; van den Hoorn, W.; Hodges, P.W. Fear of movement is related to trunk stiffness in low back pain. PLoS ONE 2013, 8, e67779. [Google Scholar]
- The Rubicon Group. Definition and Position Statement on the Chiropractic Subluxation. 2017. Available online: https://www.therubicongroup.org/policies/ (accessed on 26 May 2021).
- Kawchuk, G.; Goertz, C.; Axén, I.; Descarreaux, M.; French, S.; Haas, M.; Hartvigsen, J.; Kolberg, C.; Maiers, M. The Effect of Spinal Adjustment/Manipulation on Immunity and the Immune System: A Rapid Review of Relevant Literature. World Federation of Chiropractic, 2020. Available online: https://www.wfc.org/website/images/wfc/Latest_News_and_Features/Spinal_Manipulation_Immunity_Review_2020_03_19.pdf (accessed on 26 May 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haavik, H.; Niazi, I.K.; Kumari, N.; Amjad, I.; Duehr, J.; Holt, K. The Potential Mechanisms of High-Velocity, Low-Amplitude, Controlled Vertebral Thrusts on Neuroimmune Function: A Narrative Review. Medicina 2021, 57, 536. https://doi.org/10.3390/medicina57060536
Haavik H, Niazi IK, Kumari N, Amjad I, Duehr J, Holt K. The Potential Mechanisms of High-Velocity, Low-Amplitude, Controlled Vertebral Thrusts on Neuroimmune Function: A Narrative Review. Medicina. 2021; 57(6):536. https://doi.org/10.3390/medicina57060536
Chicago/Turabian StyleHaavik, Heidi, Imran Khan Niazi, Nitika Kumari, Imran Amjad, Jenna Duehr, and Kelly Holt. 2021. "The Potential Mechanisms of High-Velocity, Low-Amplitude, Controlled Vertebral Thrusts on Neuroimmune Function: A Narrative Review" Medicina 57, no. 6: 536. https://doi.org/10.3390/medicina57060536
APA StyleHaavik, H., Niazi, I. K., Kumari, N., Amjad, I., Duehr, J., & Holt, K. (2021). The Potential Mechanisms of High-Velocity, Low-Amplitude, Controlled Vertebral Thrusts on Neuroimmune Function: A Narrative Review. Medicina, 57(6), 536. https://doi.org/10.3390/medicina57060536









