‘De Novo’ Brain AVMs—Hypotheses for Development and a Systematic Review of Reported Cases
Abstract
1. Introduction
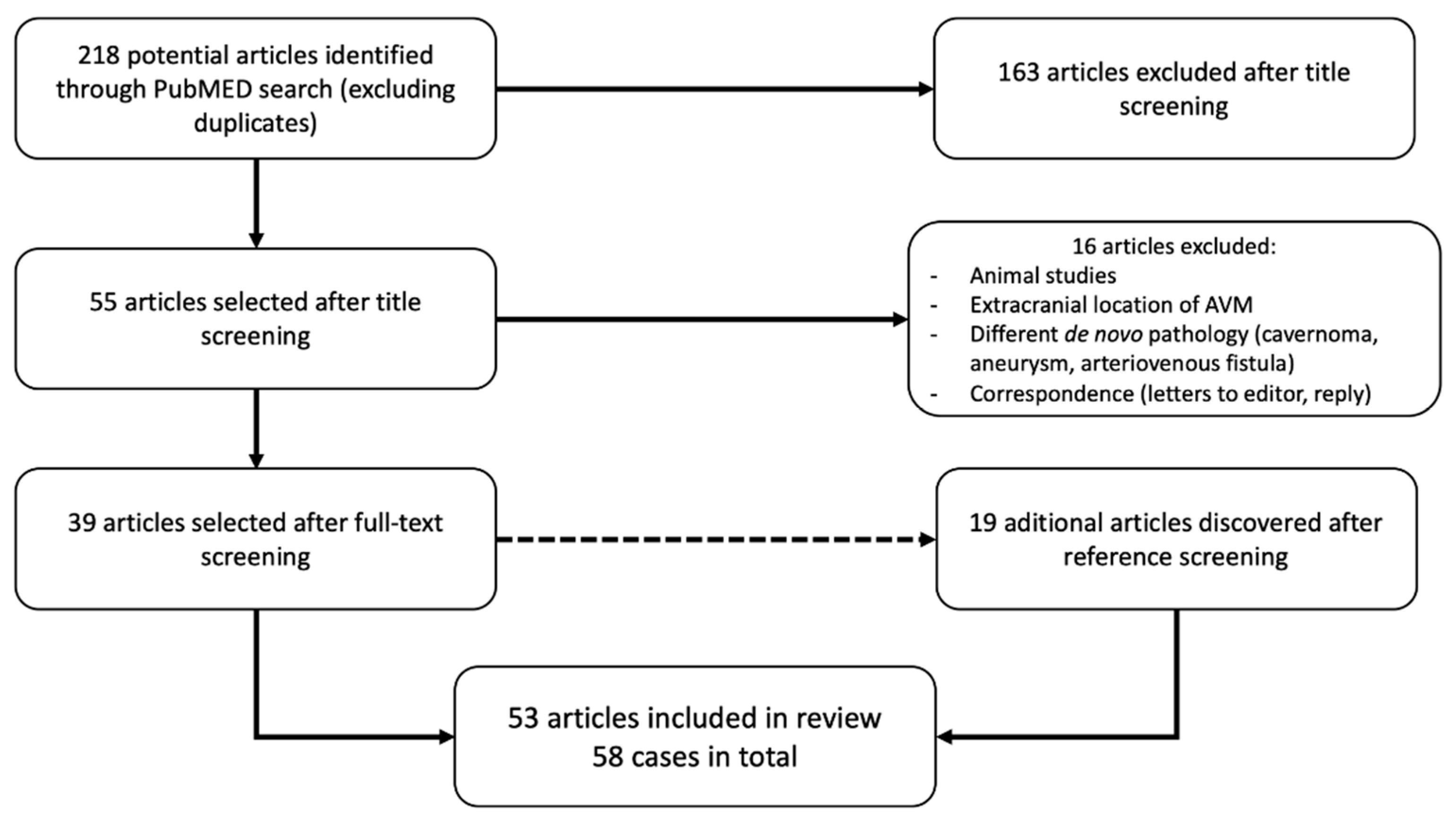
2. Material and Methods
3. Results
3.1. Literature Data
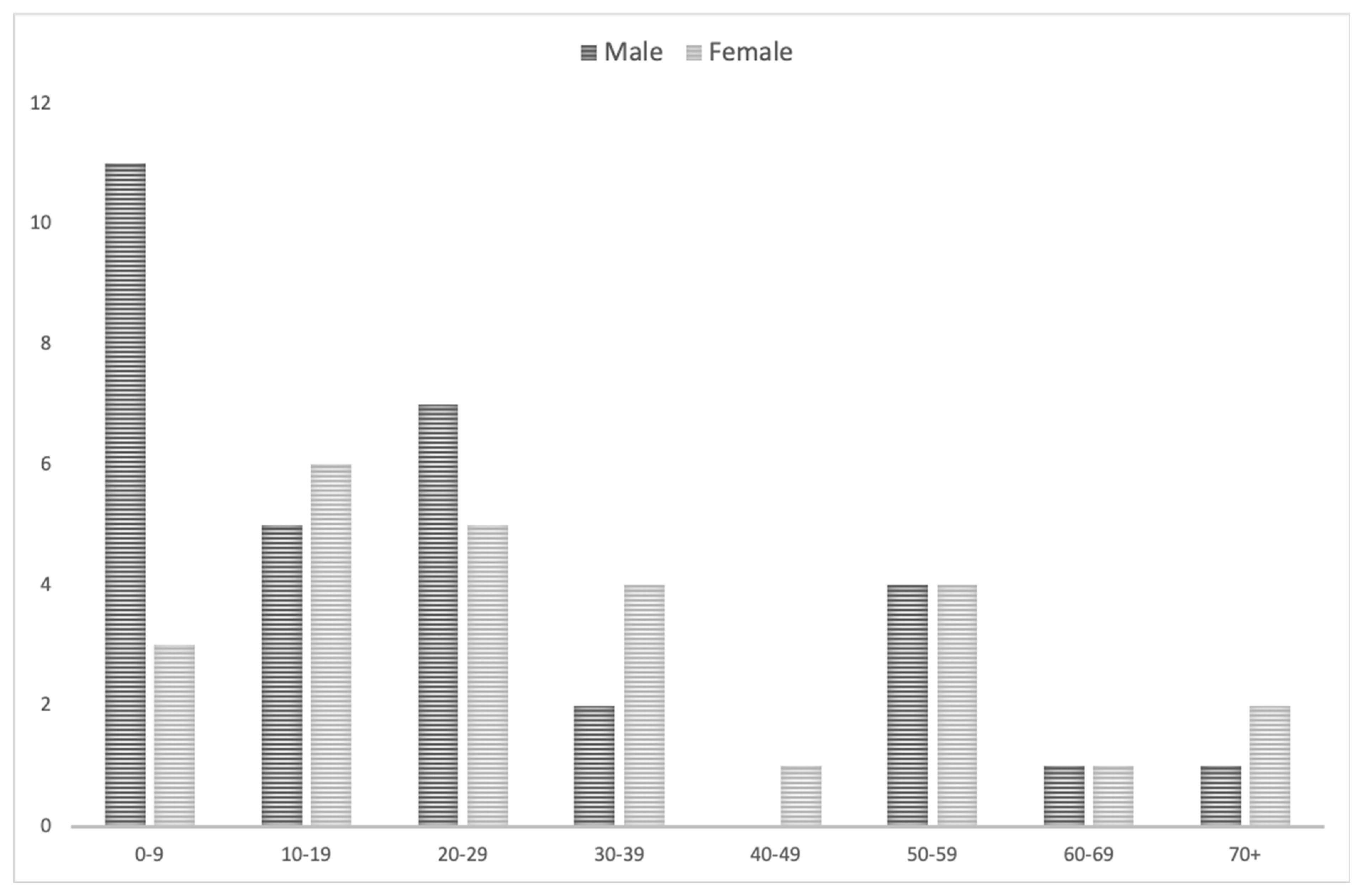
3.2. Demographic Data and Descriptive Statistics
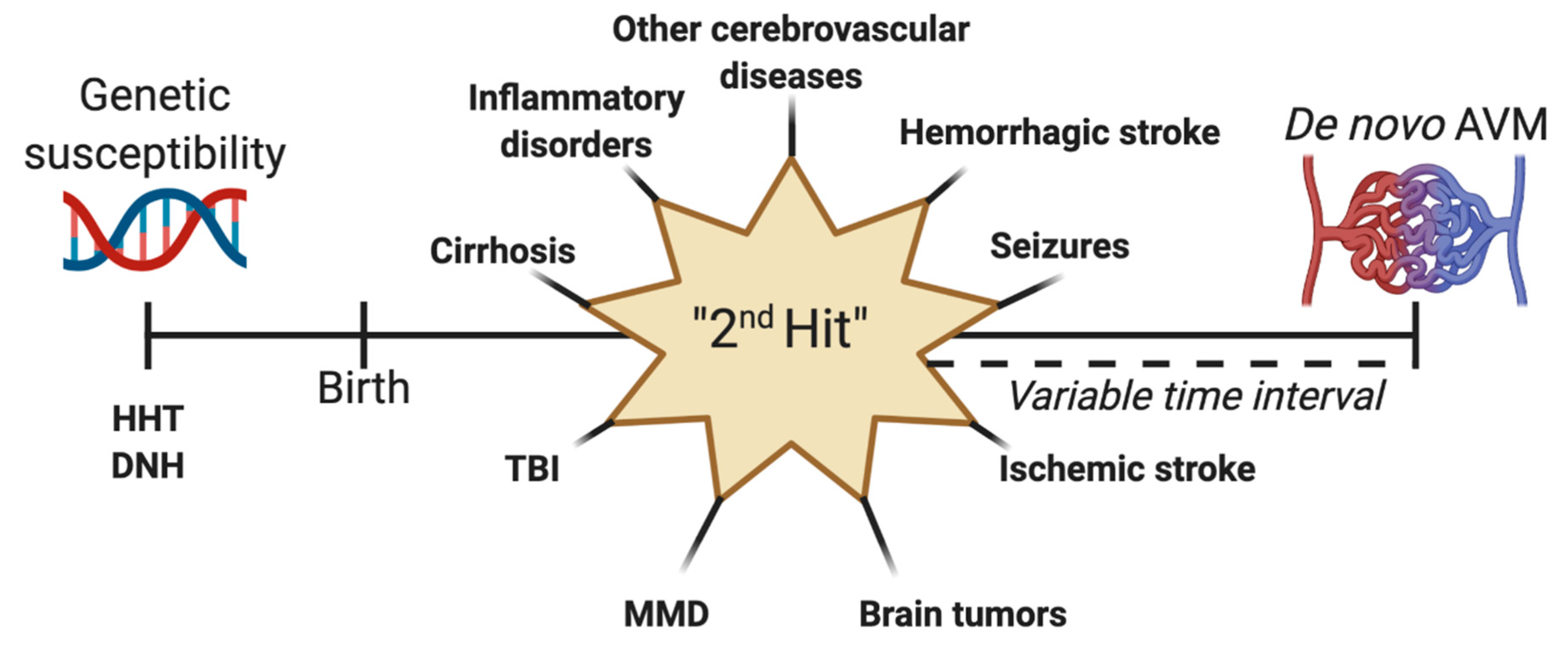
4. Discussion
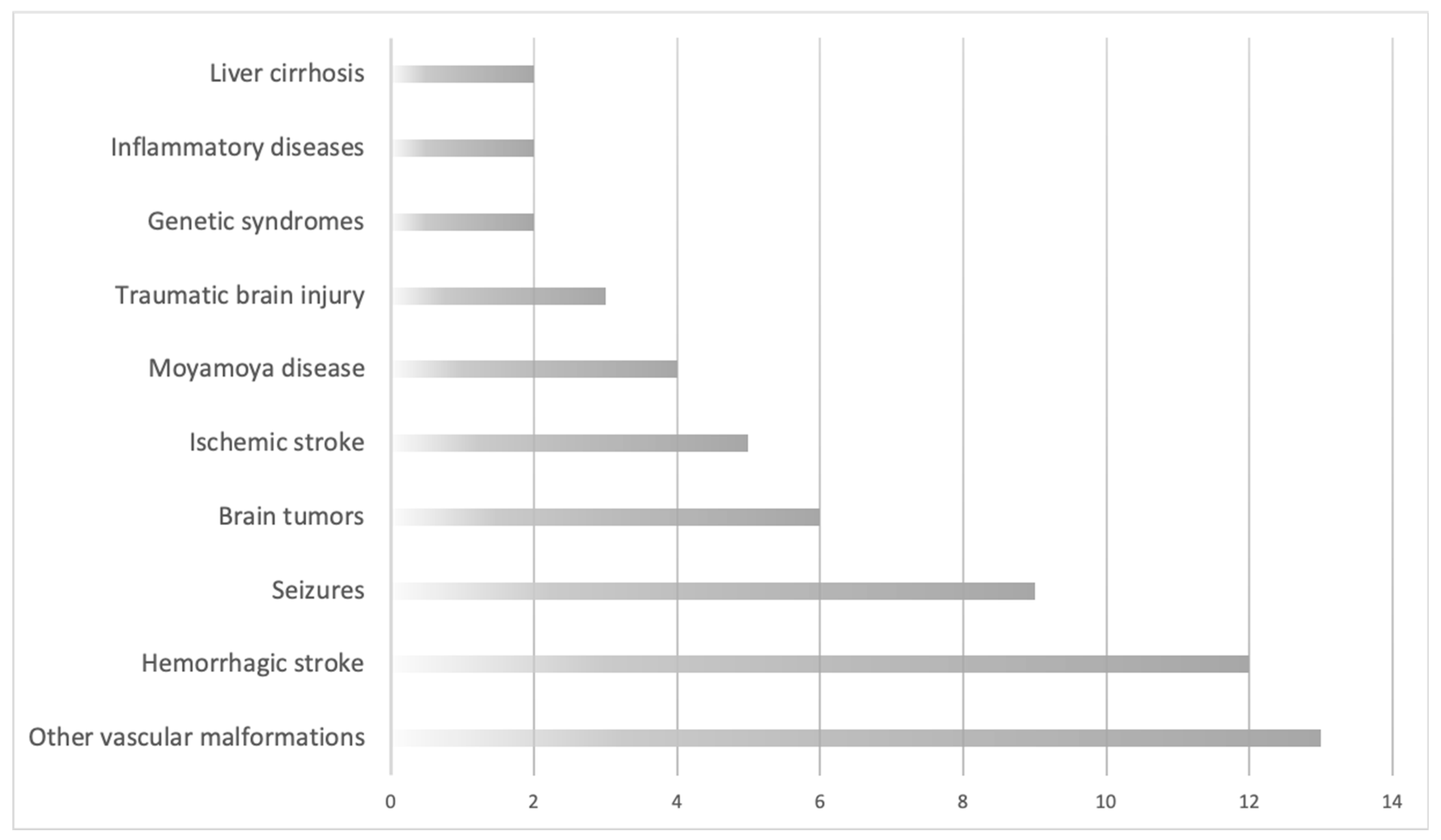
4.1. Data Review
4.2. Finding the Culprit—Hypothesized Causes for De Novo AVMs
4.2.1. Intracranial Vascular Malformations and Aneurysms
4.2.2. Hemorrhagic Stroke
4.2.3. Seizures
4.2.4. Brain Tumors
4.2.5. Ischemic Stroke, Venous Sinus Thrombosis, and Transient Ischemic Attacks (TIA)
4.2.6. Moyamoya Disease (MMD)
4.2.7. Traumatic Brain Injury (TBI)
4.2.8. Genetic Syndromes
4.2.9. Inflammatory Diseases
4.2.10. Liver Cirrhosis
4.3. Past, Present, Future, and Personal Opinions
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Florian, I.A.; Stan, H.M.; Florian, I.; Cheptea, M.; Berindan-Neagoe, I. Prognostic Factors in the Neurosurgical Treatment of Cerebral Arteriovenous Malformations. In World Federation of Neurosurgical Societies Symposia 2018 Proceeding Book; Kandasamy, R., Ed.; Editografica: Bolognia, Italy, 2019; pp. 232–241. [Google Scholar]
- Florian, I.S.; Baritchii, A.; Trifoi, S. Arterio-venous Mallformations. In Tratat de Chirurgie, 2nd ed.; Popescu, I., Ciuce, C., Eds.; Editura Academiei Romane: Cluj-Napoca, Romania, 2014; Volume 6, pp. 402–410. [Google Scholar]
- Florian, I.S.; Perju-Dumbravă, L. (Eds.) Therapeutic Options in Hemorrhagic Strokes; Editura Medicală Universitară, Iuliu Hațieganu: Cluj-Napoca, Romania, 2007; pp. 331–346. [Google Scholar]
- Kalb, S.; Gross, B.A.; Nakaji, P. 20-Vascular Malformations (Arteriovenous Malformations and Dural Arteriovenous Fistulas). In Principles of Neurological Surgery, 4th ed.; Content Repository Only: Philadelphia, PA, USA, 2018. [Google Scholar]
- Dalton, A.; Dobson, G.; Prasad, M.; Mukerji, N. De novo intracerebral arteriovenous malformations and a review of the theories of their formation. Br. J. Neurosurg. 2018, 32, 305–311. [Google Scholar] [CrossRef]
- Morales-Valero, S.F.; Bortolotti, C.; Sturiale, C.; Lanzino, G. Are parenchymal AVMs congenital lesions? Neurosurg. Focus 2014, 37, E2. [Google Scholar] [CrossRef]
- Tasiou, A.; Tzerefos, C.; Alleyne, C.H., Jr.; Boccardi, E.; Karlsson, B.; Kitchen, N.; Spetzler, R.F.; Tolias, C.M.; Fountas, K.N. Arteriovenous Malformations: Congenital or Acquired Lesions? World Neurosurg. 2020, 134, e799–e807. [Google Scholar] [CrossRef]
- Chen, Y.; Li, Z.; Shi, Y.; Huang, G.; Chen, L.; Tan, H.; Wang, Z.; Yin, C.; Hu, J. Deep Sequencing of Small RNAs in Blood of Patients with Brain Arteriovenous Malformations. World Neurosurg. 2018, 115, e570–e579. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Song, J.; Qu, M.; Wang, Y.; An, Q.; Song, Y.; Yan, W.; Wang, B.; Wang, X.; Zhang, S.; et al. MicroRNA-137 and microRNA-195* inhibit vasculogenesis in brain arteriovenous malformations. Ann. Neurol. 2017, 82, 371–384. [Google Scholar] [CrossRef]
- Weinsheimer, S.; Bendjilali, N.; Nelson, J.; Guo, D.E.; Zaroff, J.G.; Sidney, S.; Mcculloch, C.E.; Al-Shahi Salman, R.; Berg, J.N.; Koeleman, B.P.; et al. Genome-wide association study of sporadic brain arteriovenous malformations. J. Neurol. Neurosurg. Psychiatry 2016, 87, 916–923. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.W.; Berg, J.N.; Baldwin, M.A.; Gallione, C.J.; Marondel, I.; Yoon, S.J.; Stenzel, T.T.; Speer, M.; Pericak-Vance, M.A.; Diamond, A.; et al. Mutations in the activin receptor-like kinase 1 gene in hereditary haemorrhagic telangiectasia type 2. Nat. Genet. 1996, 13, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Mcallister, K.A.; Grogg, K.M.; Johnson, D.W.; Gallione, C.J.; Baldwin, M.A.; Jackson, C.E.; Helmbold, E.A.; Markel, D.S.; Mckinnon, W.C.; Murrell, J.; et al. Endoglin, a TGF-beta binding protein of endothelial cells, is the gene for hereditary haemorrhagic telangiectasia type 1. Nat. Genet. 1994, 8, 345–351. [Google Scholar] [CrossRef]
- Gallione, C.J.; Repetto, G.M.; Legius, E.; Rustgi, A.K.; Schelley, S.L.; Tejpar, S.; Mitchell, G.; Drouin, E.; Westermann, C.J.; Marchuk, D.A. A combined syndrome of juvenile polyposis and hereditary haemorrhagic telangiectasia associated with mutations in MADH4 (SMAD4). Lancet 2004, 363, 852–859. [Google Scholar] [CrossRef]
- Garrido-Martin, E.M.; Nguyen, H.L.; Cunningham, T.A.; Choe, S.W.; Jiang, Z.; Arthur, H.M.; Lee, Y.J.; Oh, S.P. Common and distinctive pathogenetic features of arteriovenous malformations in hereditary hemorrhagic telangiectasia 1 and hereditary hemorrhagic telangiectasia 2 animal models--brief report. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 2232–2236. [Google Scholar] [CrossRef]
- Park, S.O.; Wankhede, M.; Lee, Y.J.; Choi, E.J.; Fliess, N.; Choe, S.W.; Oh, S.H.; Walter, G.; Raizada, M.K.; Sorg, B.S.; et al. Real-time imaging of de novo arteriovenous malformation in a mouse model of hereditary hemorrhagic telangiectasia. J. Clin. Investig. 2009, 119, 3487–3496. [Google Scholar] [CrossRef] [PubMed]
- Han, C.; Choe, S.; Kim, Y.H.; Acharya, A.P.; Keselowsky, B.G.; Sorg, B.S.; Lee, Y.-J.; Oh, S.P. VEGF neutralization can prevent and normalize arteriovenous malformations in an animal model for hereditary hemorrhagic telangiectasia 2. Angiogenesis 2014, 17, 823–830. [Google Scholar] [CrossRef]
- Bameri, O.; Salarzaei, M.; Parooie, F. KRAS/BRAF mutations in brain arteriovenous malformations: A systematic review and meta-analysis. Interv. Neuroradiol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Goss, J.A.; Huang, A.Y.; Smith, E.; Konczyk, D.J.; Smits, P.J.; Sudduth, C.L.; Stapleton, C.; Patel, A.; Alexandrescu, S.; Warman, M.L.; et al. Somatic mutations in intracranial arteriovenous malformations. PLoS ONE 2019, 14, e0226852. [Google Scholar] [CrossRef] [PubMed]
- Priemer, D.S.; Vortmeyer, A.O.; Zhang, S.; Chang, H.Y.; Curless, K.L.; Cheng, L. Activating KRAS mutations in arteriovenous malformations of the brain: Frequency and clinicopathologic correlation. Hum. Pathol. 2019, 89, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Pawlikowska, L.; Tran, M.N.; Achrol, A.S.; Ha, C.; Burchard, E.; Choudhry, S.; Zaroff, J.; Lawton, M.T.; Castro, R.; Mcculloch, C.E.; et al. Polymorphisms in transforming growth factor-beta-related genes ALK1 and ENG are associated with sporadic brain arteriovenous malformations. Stroke 2005, 36, 2278–2280. [Google Scholar] [CrossRef]
- Simon, M.; Franke, D.; Ludwig, M.; Aliashkevich, A.F.; Köster, G.; Oldenburg, J.; Boström, A.; Ziegler, A.; Schramm, J. Association of a polymorphism of the ACVRL1 gene with sporadic arteriovenous malformations of the central nervous system. J. Neurosurg. 2006, 104, 945–949. [Google Scholar] [CrossRef]
- Kim, H.; Hysi, P.G.; Pawlikowska, L.; Poon, A.; Burchard, E.G.; Zaroff, J.G.; Sidney, S.; Ko, N.U.; Achrol, A.S.; Lawton, M.T.; et al. Common variants in interleukin-1-Beta gene are associated with intracranial hemorrhage and susceptibility to brain arteriovenous malformation. Cerebrovasc. Dis. 2009, 27, 176–182. [Google Scholar] [CrossRef]
- Chen, H.; Gu, Y.; Wu, W.; Chen, D.; Li, P.; Fan, W.; Lu, D.; Zhao, F.; Qiao, N.; Qiu, H.; et al. Polymorphisms of the vascular endothelial growth factor A gene and susceptibility to sporadic brain arteriovenous malformation in a Chinese population. J. Clin. Neurosci. 2011, 18, 549–553. [Google Scholar] [CrossRef]
- Pabaney, A.H.; Rammo, R.A.; Tahir, R.A.; Seyfried, D. Development of De Novo Arteriovenous Malformation Following Ischemic Stroke: Case Report and Review of Current Literature. World Neurosurg. 2016, 96, 608.e5–608.e12. [Google Scholar] [CrossRef] [PubMed]
- Dogan, S.N.; Bagcilar, O.; Mammadov, T.; Kizilkilic, O.; Islak, C.; Kocer, N. De Novo Development of a Cerebral Arteriovenous Malformation: Case Report and Review of the Literature. World Neurosurg. 2019, 126, 257–260. [Google Scholar] [CrossRef]
- Torres-Quinones, C.; Koch, M.J.; Raymond, S.B.; Patel, A. Left Thalamus Arteriovenous Malformation Secondary to Radiation Therapy of Original Vermian Arteriovenous Malformation: Case Report. J. Stroke Cerebrovasc. Dis. 2019, 28, e53–e59. [Google Scholar] [CrossRef]
- Lo Presti, A.; Rogers, J.M.; Assaad, N.N.A.; Rodriguez, M.L.; Stoodley, M.A.; Morgan, M.K. De novo brain arteriovenous malformation after tumor resection: Case report and literature review. Acta Neurochir. 2018, 160, 2191–2197. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues De Oliveira, L.F.; Castro-Afonso, L.H.; Freitas, R.K.; Colli, B.O.; Abud, D.G. De Novo Intracranial Arteriovenous Malformation-Case Report and Literature Review. World Neurosurg. 2020, 138, 349–351. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, L.F.; Bristol, R.E.; Porter, R.W.; Spetzler, R.F. De novo presentation of an arteriovenous malformation. Case report and review of the literature. J. Neurosurg. 2005, 102, 726–729. [Google Scholar] [CrossRef] [PubMed]
- Mohr, J.P.; Yaghi, S. Management of unbled brain arteriovenous malformation study. Neurol. Clin. 2015, 33, 347–359. [Google Scholar] [CrossRef] [PubMed]
- Solomon, R.A.; Connolly, E.S., Jr. Arteriovenous Malformations of the Brain. N. Engl. J. Med. 2017, 377, 498. [Google Scholar] [CrossRef]
- Song, J.K.; Niimi, Y.; Kupersmith, M.J.; Berenstein, A. Postnatal growth and development of a cerebral arteriovenous malformation on serial magnetic resonance imaging in a child with hemangiomatosis. Case report. J. Neurosurg. 2007, 106, 384–387. [Google Scholar]
- Mendelow, A.D.; Erfurth, A.; Grossart, K.; Macpherson, P. Do cerebral arteriovenous malformations increase in size? J. Neurol. Neurosurg. Psychiatry 1987, 50, 980–987. [Google Scholar] [CrossRef] [PubMed]
- Du, R.; Hashimoto, T.; Tihan, T.; Young, W.L.; Perry, V.; Lawton, M.T. Growth and regression of arteriovenous malformations in a patient with hereditary hemorrhagic telangiectasia. Case report. J. Neurosurg. 2007, 106, 470–477. [Google Scholar] [CrossRef]
- Yeo, J.J.; Low, S.Y.; Seow, W.T.; Low, D.C. Pediatric de novo cerebral AVM: Report of two cases and review of literature. Childs Nerv. Syst. 2015, 31, 609–614. [Google Scholar] [CrossRef]
- Ozsarac, M.; Aksay, E.; Kiyan, S.; Unek, O.; Gulec, F.F. De novo cerebral arteriovenous malformation: Pink Floyd’s song “Brick in the Wall” as a warning sign. J. Emerg. Med. 2012, 43, e17–e20. [Google Scholar] [CrossRef]
- Harris, O.A.; Chang, S.D.; Harris, B.T.; Adler, J.R. Acquired cerebral arteriovenous malformation induced by an anaplastic astrocytoma: An interesting case. Neurol. Res. 2000, 22, 473–477. [Google Scholar] [CrossRef]
- Mckinney, J.S.; Steineke, T.; Nochlin, D.; Brisman, J.L. De novo formation of large arteriovenous shunting and a vascular nidus mimicking an arteriovenous malformation within an anaplastic oligodendroglioma: Treatment with embolization and resection. J. Neurosurg. 2008, 109, 1098–1102. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, A.; Manchandia, T.C.; Gould, G.; Bulsara, K.R. De novo arteriovenous malformations: Case report and review of the literature. Neurosurg. Rev. 2010, 33, 115–119. [Google Scholar] [CrossRef]
- Akimoto, H.; Komatsu, K.; Kubota, Y. Symptomatic de novo arteriovenous malformation appearing 17 years after the resection of two other arteriovenous malformations in childhood: Case report. Neurosurgery 2003, 52, 228–231; discussion 231–232. [Google Scholar] [PubMed]
- Kawashima, M.; Hasegawa, H.; Kurita, H.; Suzuki, K.; Shin, M.; Ikemura, M.; Saito, N. Ectopic Recurrence of Arteriovenous Malformation After Radiosurgery: Case Report and Insight Regarding Pathogenesis. World Neurosurg. 2020, 135, 63–67. [Google Scholar] [CrossRef]
- Nussbaum, E.S.; Heros, R.C.; Madison, M.T.; Awasthi, D.; Truwit, C.L. The pathogenesis of arteriovenous malformations: Insights provided by a case of multiple arteriovenous malformations developing in relation to a developmental venous anomaly. Neurosurgery 1998, 43, 347–351; discussion 351–352. [Google Scholar] [CrossRef] [PubMed]
- Nagm, A.; Horiuchi, T.; Ichinose, S.; Hongo, K. Unique double recurrence of cerebral arteriovenous malformation. Acta Neurochir. 2015, 157, 1461–1466. [Google Scholar] [CrossRef]
- Koch, M.J.; Agarwalla, P.K.; Stapleton, C.J.; Ogilvy, C.S.; Loeffler, J.S. De novo development of a cerebral arteriovenous malformation following radiation therapy: Case report and an update to classical arteriovenous malformation nomenclature. J. Clin. Neurosci. 2016, 28, 162–167. [Google Scholar] [CrossRef]
- Shi, S.; Gupta, R.; Moore, J.M.; Griessenauer, C.J.; Adeeb, N.; Motiei-Langroudi, R.; Thomas, A.J.; Ogilvy, C.S. De novo AVM formation following venous sinus thrombosis and prior AVM resection in adults: Report of 2 cases. J. Neurosurg. 2018, 128, 506–510. [Google Scholar] [CrossRef]
- Shimoda, Y.; Osanai, T.; Nakayama, N.; Ushikoshi, S.; Hokari, M.; Shichinohe, H.; Abumiya, T.; Kazumata, K.; Houkin, K. De novo arteriovenous malformation in a patient with hereditary hemorrhagic telangiectasia. J. Neurosurg. Pediatr. 2016, 17, 330–335. [Google Scholar] [CrossRef]
- Zhou, D.; Huang, X.; Xie, Y.; Deng, Z.; Guo, J.; Huang, H. Astrocytes-derived VEGF exacerbates the microvascular damage of late delayed RBI. Neuroscience 2019, 408, 14–21. [Google Scholar] [CrossRef]
- Zhou, G.; Xu, Y.; He, B.; Ma, R.; Wang, Y.; Chang, Y.; Xie, Y.; Wu, L.; Huang, J.; Xiao, Z. Ionizing radiation modulates vascular endothelial growth factor expression through STAT3 signaling pathway in rat neonatal primary astrocyte cultures. Brain Behav. 2020, 10, e01529. [Google Scholar] [CrossRef] [PubMed]
- Alvarez, H.; Perry, V.; Solle, M.; Castillo, M. De novo cerebral arteriovenous malformation in a child with previous cavernous malformation and developmental venous anomaly. J. Neurosurg. Pediatr. 2012, 9, 327–330. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Rivera, V.; Sheriff, F.G.; Sandberg, D.I.; Blackburn, S.; Dannenbaum, M.; Sheth, S.A.; Day, A.L.; Chen, P.R. De novo thalamic arteriovenous malformation in a boy with a brainstem cavernous malformation. J. Clin. Neurosci. 2020, 76, 226–228. [Google Scholar] [CrossRef] [PubMed]
- Leblanc, G.G.; Golanov, E.; Awad, I.A.; Young, W.L. Biology of vascular malformations of the brain. Stroke 2009, 40, e694–e702. [Google Scholar] [CrossRef]
- Sure, U.; Butz, N.; Schlegel, J.; Siegel, A.M.; Wakat, J.P.; Mennel, H.D.; Bien, S.; Bertalanffy, H. Endothelial proliferation, neoangiogenesis, and potential de novo generation of cerebrovascular malformations. J. Neurosurg. 2001, 94, 972–977. [Google Scholar] [CrossRef]
- Bai, Y.; He, C.; Zhang, H.; Ling, F. De novo multiple dural arteriovenous fistulas and arteriovenous malformation after embolization of cerebral arteriovenous fistula: Case report. Childs Nerv. Syst. 2012, 28, 1981–1983. [Google Scholar] [CrossRef]
- Friedman, J.A.; Pollock, B.E.; Nichols, D.A. Development of a cerebral arteriovenous malformation documented in an adult by serial angiography. Case report. J. Neurosurg. 2000, 93, 1058–1061. [Google Scholar] [CrossRef] [PubMed]
- Shidoh, S.; Kobayashi, M.; Akaji, K.; Kano, T.; Tanizaki, Y.; Mihara, B. De Novo Arteriovenous Malformation after Aneurysm Clipping. NMC Case Rep. J. 2017, 4, 89–92. [Google Scholar] [CrossRef]
- Miyasaka, Y.; Nakahara, K.; Takagi, H.; Hagiwara, H. Development of multiple cerebral arteriovenous malformations documented in an adult by serial angiography. Case report. J. Neurosurg. 2003, 98, 190–193. [Google Scholar] [CrossRef]
- Porter, A.J.; Bull, J. Some aspects of the natural history of cerebral arteriovenous malformation. Br. J. Radiol. 1969, 42, 667–675. [Google Scholar] [CrossRef]
- Peeters, F.L. Angiographically demonstrated larger vascular malformation in a patient with a normal angiogram 23 years before. Neuroradiology 1982, 23, 113–114. [Google Scholar] [CrossRef] [PubMed]
- Fuse, T.; Niwa, Y.; Umezu, M.; Yamada, K. Growth of occult arteriovenous malformation after cerebral hemorrhage demonstrated by serial magnetic resonance imaging—Case report. Neurol. Med. Chir. 2001, 41, 83–86. [Google Scholar] [CrossRef][Green Version]
- Jeffree, R.L.; Stoodley, M.A. Postnatal development of arteriovenous malformations. Pediatr. Neurosurg. 2009, 45, 296–304. [Google Scholar] [CrossRef]
- Morioka, T.; Nishio, S.; Hikita, T.; Chung, L.H.; Soejima, T. Marked growth of an angiographically occult arteriovenous malformation: Case report. Neurosurgery 1988, 23, 101–103. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, M.; Samii, A.; Lang, J.M.; Götz, F.; Samii, M.; Krauss, J.K. De Novo Arteriovenous Malformation Growth Secondary to Implantation of Genetically Modified Allogeneic Mesenchymal Stem Cells in the Brain. Neurosurgery 2016, 78, E596–E600. [Google Scholar] [CrossRef]
- Nakamura, M.; Krauss, J.K. In Reply: De Novo Arteriovenous Malformation Growth Secondary to Implantation of Genetically Modified Allogeneic Mesenchymal Stem Cells in the Brain. Neurosurgery 2016, 78, E602–E603. [Google Scholar] [CrossRef]
- Kilbourn, K.J.; Spiegel, G.; Killory, B.D.; Kureshi, I. Case report of a de novo brainstem arteriovenous malformation in an 18-year-old male and review of the literature. Neurosurg. Rev. 2014, 37, 685–691. [Google Scholar] [CrossRef]
- Laura, K.; Markham, M.A.H. De Novo Arteriovenous Malformation in a 4 Year-Old Boy with Headache, with No Previous Cerebrovascular Disease. J. Neurol. Neurosci. 2015, 6, 3. [Google Scholar]
- Neil, J.A.; Li, D.; Stiefel, M.F.; Hu, Y.C. Symptomatic de novo arteriovenous malformation in an adult: Case report and review of the literature. Surg. Neurol. Int. 2014, 5, 148. [Google Scholar]
- Stevens, J.; Leach, J.L.; Abruzzo, T.; Jones, B.V. De novo cerebral arteriovenous malformation: Case report and literature review. Am. J. Neuroradiol. 2009, 30, 111–112. [Google Scholar] [CrossRef]
- Wu, J.; Li, Y.; Cao, Y.; Wang, S. De novo cerebral arteriovenous malformations: Is epileptic seizure a potential trigger? Childs Nerv. Syst. 2014, 30, 1277–1281. [Google Scholar] [CrossRef]
- Abecassis, I.J.; Xu, D.S.; Batjer, H.H.; Bendok, B.R. Natural history of brain arteriovenous malformations: A systematic review. Neurosurg. Focus 2014, 37, E7. [Google Scholar] [CrossRef] [PubMed]
- Castillo, M.; Thompson, J.E.; Mukherji, S.K. Association of an intracranial arteriovenous malformation and a meningioma. Neuroradiology 1998, 40, 574–576. [Google Scholar] [CrossRef] [PubMed]
- Croll, S.D.; Goodman, J.H.; Scharfman, H.E. Vascular endothelial growth factor (VEGF) in seizures: A double-edged sword. Adv. Exp. Med. Biol. 2004, 548, 57–68. [Google Scholar]
- Sun, F.J.; Wei, Y.J.; Li, S.; Guo, W.; Chen, X.; Liu, S.Y.; He, J.J.; Yin, Q.; Yang, H.; Zhang, C.Q. Elevated Expression of VEGF-C and Its Receptors, VEGFR-2 and VEGFR-3, in Patients with Mesial Temporal Lobe Epilepsy. J. Mol. Neurosci. 2016, 59, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Vezzani, A. VEGF and seizures: Cross-talk between endothelial and neuronal environments. Epilepsy Curr. 2005, 5, 72–74. [Google Scholar] [CrossRef] [PubMed]
- Castañeda-Cabral, J.L.; Beas-Zárate, C.; Rocha-Arrieta, L.L.; Orozco-Suárez, S.A.; Alonso-Vanegas, M.; Guevara-Guzmán, R.; Ureña-Guerrero, M.E. Increased protein expression of VEGF-A, VEGF-B, VEGF-C and their receptors in the temporal neocortex of pharmacoresistant temporal lobe epilepsy patients. J. Neuroimmunol. 2019, 328, 68–72. [Google Scholar] [CrossRef]
- Lange, C.; Storkebaum, E.; De Almodóvar, C.R.; Dewerchin, M.; Carmeliet, P. Vascular endothelial growth factor: A neurovascular target in neurological diseases. Nat. Rev. Neurol. 2016, 12, 439–454. [Google Scholar] [CrossRef]
- Nicoletti, J.N.; Lenzer, J.; Salerni, E.A.; Shah, S.K.; Elkady, A.; Khalid, S.; Quinteros, D.; Rotella, F.; Betancourth, D.; Croll, S.D. Vascular endothelial growth factor attenuates status epilepticus-induced behavioral impairments in rats. Epilepsy Behav. 2010, 19, 272–277. [Google Scholar] [CrossRef]
- Ureña-Guerrero, M.E.; Castañeda-Cabral, J.L.; Rivera-Cervantes, M.C.; Macias-Velez, R.J.; Jarero-Basulto, J.J.; Gudiño-Cabrera, G.; Beas-Zárate, C. Neuroprotective and Neurorestorative Effects of Epo and VEGF: Perspectives for New Therapeutic Approaches to Neurological Diseases. Curr. Pharm. Des. 2020, 26, 1263–1276. [Google Scholar] [CrossRef]
- Franco, A.; Pimentel, J.; Campos, A.R.; Morgado, C.; Pinelo, S.; Ferreira, A.G.; Bentes, C. Stimulation of the bilateral anterior nuclei of the thalamus in the treatment of refractory epilepsy: Two cases of subcortical band heterotopia. Epileptic. Disord. 2016, 18, 426–430. [Google Scholar] [CrossRef]
- Parrini, E.; Conti, V.; Dobyns, W.B.; Guerrini, R. Genetic Basis of Brain Malformations. Mol. Syndromol. 2016, 7, 220–233. [Google Scholar] [CrossRef]
- Sahu, S.; Buhler, E.; Vermoyal, J.C.; Watrin, F.; Represa, A.; Manent, J.B. Spontaneous epileptiform activity in a rat model of bilateral subcortical band heterotopia. Epilepsia 2019, 60, 337–348. [Google Scholar] [CrossRef]
- Borges, L.R.; Malheiros, S.M.; Pelaez, M.P.; Stávale, J.N.; Santos, A.J.; Carrete, H., Jr.; Nogueira, R.G.; Ferraz, F.A.; Gabbai, A.A. Arteriovenous malformation-glioma association: Study of four cases. Arq. Neuropsiquiatr. 2003, 61, 426–429. [Google Scholar] [CrossRef][Green Version]
- Goodkin, R.; Zaias, B.M.; Michelsen, W.J. Arteriovenous malformation and glioma: Coexistent or sequential? Case report. J. Neurosurg. 1990, 72, 798–805. [Google Scholar] [CrossRef]
- Soria, E.; Fine, E.; Hajdu, I. Association of intracranial meningioma with arteriovenous malformation. Surg. Neurol. 1990, 34, 111–117. [Google Scholar] [CrossRef]
- Suzuki, H.; Uenohara, H.; Utsunomiya, A.; Kurihara, N.; Suzuki, S.; Tadokoro, M.; Iwasaki, Y.; Sakurai, Y.; Takei, H.; Tezuka, F. A case of angioglioma composed of astrocytoma with a papillary growth pattern: Immunohistochemical and ultrastructural studies. Brain Tumor Pathol. 2002, 19, 111–116. [Google Scholar] [CrossRef] [PubMed]
- Bennett, E.E.; Otvos, B.; Kshettry, V.R.; Gonzalez-Martinez, J. Delayed presentation of an arteriovenous malformation after cerebellar hemangioblastoma resection-Case report. Int. J. Surg. Case Rep. 2016, 23, 47–51. [Google Scholar] [CrossRef]
- Mathon, B.; Blauwblomme, T.; Bolle, S.; Dufour, C.; Nagarra, O.; Brunelle, F.; Puget, S. De novo arteriovenous malformation after brain radiotherapy for medulloblastoma in a child. Neurology 2013, 81, 398–399. [Google Scholar] [CrossRef]
- Medvedev, Y.A.; Matsko, D.E.; Zubkov, Y.N.; Pak, V.A.; Alexander, L.F. Coexistent hemangioblastoma and arteriovenous malformation of the cerebellum. Case report. J. Neurosurg. 1991, 75, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Kaido, T.; Hoshida, T.; Uranishi, R.; Akita, N.; Kotani, A.; Nishi, N.; Sakaki, T. Radiosurgery-induced brain tumor. Case report. J. Neurosurg. 2001, 95, 710–713. [Google Scholar] [CrossRef] [PubMed]
- Koshimura, I.; Takeda, N.; Ohtomo, T.; Shimada, J.; Sugano, K.; Mori, H.; Mizuno, Y.; Sato, K. A 32-year-old man who developed a posterior fossa mass 12 years after the radiation therapy for cerebellar arteriovenous malformation. No Shinkei 1996, 48, 81–89. [Google Scholar]
- Wolf, A.; Naylor, K.; Tam, M.; Habibi, A.; Novotny, J.; Liščák, R.; Martinez-Moreno, N.; Martinez-Alvarez, R.; Sisterson, N.; Golfinos, J.G.; et al. Risk of radiation-associated intracranial malignancy after stereotactic radiosurgery: A retrospective, multicentre, cohort study. Lancet Oncol. 2019, 20, 159–164. [Google Scholar] [CrossRef]
- Dore-Duffy, P.; Lamanna, J.C. Physiologic angiodynamics in the brain. Antioxid. Redox Signal. 2007, 9, 1363–1371. [Google Scholar] [CrossRef]
- Santos, R.; Aguilar-Salinas, P.; Entwistle, J.J.; Aldana, P.R.; Beier, A.D.; Hanel, R.A. De Novo Arteriovenous Malformation in a Pediatric Patient: Case Report and Review of the Literature. World Neurosurg. 2018, 111, 341–345. [Google Scholar] [CrossRef]
- Komiyama, M. Revised perspective of cerebral arteriovenous malformation. Jpn. J. Neurosurg. 2011, 20, 4–11. [Google Scholar] [CrossRef]
- Ozawa, T.; Miyasaka, Y.; Tanaka, R.; Kurata, A.; Fujii, K. Dural-pial arteriovenous malformation after sinus thrombosis. Stroke 1998, 29, 1721–1724. [Google Scholar] [CrossRef] [PubMed]
- Fujimura, M.; Kimura, N.; Ezura, M.; Niizuma, K.; Uenohara, H.; Tominaga, T. Development of a de novo arteriovenous malformation after bilateral revascularization surgery in a child with moyamoya disease. J. Neurosurg. Pediatr. 2014, 13, 647–649. [Google Scholar] [CrossRef]
- Noh, J.H.; Yeon, J.Y.; Park, J.H.; Shin, H.J. Cerebral arteriovenous malformation associated with moyamoya disease. J. Korean Neurosurg. Soc. 2014, 56, 356–360. [Google Scholar] [CrossRef]
- O’shaughnessy, B.A.; Dipatri, A.J., Jr.; Parkinson, R.J.; Batjer, H.H. Development of a de novo cerebral arteriovenous malformation in a child with sickle cell disease and moyamoya arteriopathy. Case report. J. Neurosurg. 2005, 102, 238–243. [Google Scholar] [CrossRef]
- Schmit, B.P.; Burrows, P.E.; Kuban, K.; Goumnerova, L.; Scott, R.M. Acquired cerebral arteriovenous malformation in a child with moyamoya disease. Case report. J. Neurosurg. 1996, 84, 677–680. [Google Scholar] [CrossRef]
- Kayama, T.; Suzuki, S.; Sakurai, Y.; Nagayama, T.; Ogawa, A.; Yoshimoto, T. A case of moyamoya disease accompanied by an arteriovenous malformation. Neurosurgery 1986, 18, 465–468. [Google Scholar] [CrossRef]
- Mawad, M.E.; Hilal, S.K.; Michelsen, W.J.; Stein, B.; Ganti, S.R. Occlusive vascular disease associated with cerebral arteriovenous malformations. Radiology 1984, 153, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Montanera, W.; Marotta, T.R.; Terbrugge, K.G.; Lasjaunias, P.; Willinsky, R.; Wallace, M.C. Cerebral arteriovenous malformations associated with moyamoya phenomenon. Am. J. Neuroradiol. 1990, 11, 1153–1156. [Google Scholar] [PubMed]
- Anami, H.; Aihara, Y.; Kawashima, A.; Yamaguchi, K.; Nagahara, A.; Okada, Y. A case report of a pediatric traumatic aneurysm with arteriovenous (A-V) fistula CASE-BASED UPDATE. Childs Nerv. Syst. 2014, 30, 2003–2008. [Google Scholar] [CrossRef] [PubMed]
- Cuoco, J.A.; Guilliams, E.L.; Klein, B.J.; Malaty, G.R.; Witcher, M.R.; Entwistle, J.J. N-butyl cyanoacrylate embolization of a traumatic pseudoaneurysm and arteriovenous fistula of the middle meningeal artery. Radiol. Case Rep. 2020, 15, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Tokairin, K.; Osanai, T.; Kazumata, K.; Sawaya, R.; Houkin, K. Contrecoup Injury-Induced Middle Meningeal Arteriovenous Fistula Detected by Time-of-Flight Magnetic Resonance Angiography and Magnetic Resonance Arterial Spin Labeling: Case Report and Review of the Literature. World Neurosurg. 2019, 127, 79–84. [Google Scholar] [CrossRef]
- Miller, B.A.; Bass, D.I.; Chern, J.J. Development of a de novo arteriovenous malformation after severe traumatic brain injury. J. Neurosurg. Pediatr. 2014, 14, 418–420. [Google Scholar] [CrossRef]
- Krayenbühl, H.A. Angiographic contribution to the problem of enlargement of cerebral arteriovenous malformations. Acta Neurochir. 1977, 36, 215–242. [Google Scholar] [CrossRef]
- Dotan, M.; Lorber, A. Congestive heart failure with diffuse neonatal hemangiomatosis—Case report and literature review. Acta Paediatr. 2013, 102, e232–e238. [Google Scholar] [CrossRef]
- Patiroglu, T.; Sarici, D.; Unal, E.; Yikilmaz, A.; Tucer, B.; Karakukcu, M.; Ozdemir, M.A.; Canoz, O.; Akcakus, M. Cerebellar hemangioblastoma associated with diffuse neonatal hemangiomatosis in an infant. Childs Nerv. Syst. 2012, 28, 1801–1805. [Google Scholar] [CrossRef]
- Bulsara, K.R.; Alexander, M.J.; Villavicencio, A.T.; Graffagnino, C. De novo cerebral arteriovenous malformation: Case report. Neurosurgery 2002, 50, 1137–1140; discussion 1140–1141. [Google Scholar]
- Gondar, R.; El Rahal, A.; Kulcsár, Z.; Schaller, K.; Momjian, S. Spontaneous appearance of de novo intracranial arteriovenous malformation in hepatic cirrhosis. Neurochirurgie 2019, 65, 393–396. [Google Scholar] [CrossRef]
- Shimoda, Y.; Kuroda, S.; Kashiwazaki, D.; Asano, T.; Yamashita, K.; Taniguchi, M.; Suzuki, T.; Shimamura, T.; Furukawa, H.; Nakayama, N.; et al. Spontaneous disappearance of intracranial arteriovenous malformation after living-donor liver transplantation: A case report. No Shinkei Geka 2011, 39, 589–594. [Google Scholar]
- Chen, W.; Sun, Z.; Han, Z.; Jun, K.; Camus, M.; Wankhede, M.; Mao, L.; Arnold, T.; Young, W.L.; Su, H. De novo cerebrovascular malformation in the adult mouse after endothelial Alk1 deletion and angiogenic stimulation. Stroke 2014, 45, 900–902. [Google Scholar] [CrossRef]
- Walker, E.J.; Su, H.; Shen, F.; Choi, E.J.; Oh, S.P.; Chen, G.; Lawton, M.T.; Kim, H.; Chen, Y.; Chen, W.; et al. Arteriovenous malformation in the adult mouse brain resembling the human disease. Ann. Neurol. 2011, 69, 954–962. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Saw, D.; Weiss, M.; Sun, Z.; Wei, M.; Shaligram, S.; Wang, S.; Su, H. Induction of Brain Arteriovenous Malformation Through CRISPR/Cas9-Mediated Somatic Alk1 Gene Mutations in Adult Mice. Transl. Stroke Res. 2019, 10, 557–565. [Google Scholar] [CrossRef]
- Fujii, M.; Ichikawa, M.; Iwatate, K.; Bakhit, M.; Yamada, M.; Kuromi, Y.; Sato, T.; Sakuma, J.; Sato, H.; Kikuta, A.; et al. Secondary brain tumors after cranial radiation therapy: A single-institution study. Rep. Pract. Oncol. Radiother. 2020, 25, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Mariniello, G.; De Liso, M.; Russo, C.; Del Vecchio, W.; De Divitiis, O.; Bruno, F.; Maggialetti, N.; Arrigoni, F.; Brunese, L.; Caranci, F. Radiation-induced brain cavernomas in elderly: Review of the literature and a rare case report. Acta Biomed. 2019, 90, 77–83. [Google Scholar]
- Sheen, J.J.; Lee, D.H.; Lee, D.H.; Song, Y.; Kwon, D.H. Long-Term Outcome of Gamma Knife Radiosurgery for Brain Cavernoma: Factors Associated with Subsequent De Novo Cavernoma Formation. World Neurosurg. 2018, 120, e17–e23. [Google Scholar] [CrossRef]
- Isayama, Y.; Nakagawara, J.; Takeda, R.; Wada, K.; Hyogo, T.; Sasaki, T.; Nakamura, J.; Suematsu, K. A case of cerebral arteriovenous malformation revealed at repeated subcortical hematoma with initially normal angiogram. No Shinkei Geka 1991, 19, 1175–1180. [Google Scholar]

| Authors | Sex | Age (yrs.)—De Novo AVM | Initial Symptoms | Imaging (−) | Associated Pathology | Symptoms—De Novo | Imaging (+) | Diagnosis Interval (yrs.) | AVM location | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Akimoto et al., 2003 | F | 27 | Intraventricular hemorrhage (10 yrs. old) | CTA DSA | Splenium AVM & L Occipital AVM − ruptured + resected | Headache, R sided numbness | CTA DSA MRI | 17 | Cingulate gyrus & corpus callosum | MS | Favorable |
| Alvarez et al., 2012 | M | 8 | Seizures | CT MRI | Giant R T-O cavernoma | ASX | MRI DSA | 2 | Pineal | C | Favorable |
| Bai et al., 2012 | M | 7 | Generalized tonic-clinic seizure | MRI DSA | Dural AVF, embolization; multiple dAVFs simultaneous with AVM | Seizure relapse | MRI DSA | 4 | L medial Occipital | E | Favorable |
| de Oliveira et al., 2020 | F | 16 | Headache | MRI DSA | Ruptured R occipital cavernoma, operated | Headache | MRI DSA | 10 | R Temporal | E+MS | Favorable |
| Friedman et al., 2000 | M | 68 | Vertigo and vomiting | CT DSA MRI | R tentorial DAVF, treated via SRS and embolization | ASX; 2 years later (age 70)-vertigo and nausea | CT DSA MRI | 7 | Sup. Vermis | SRS | Favorable |
| Kawashima et al., 2019 | F | 29 | Cerebellar hemorrhage, ataxia | CT DSA MRI | R cerebellar AVM, ruptured, treated with SRS | headache, vomiting, and worsened ataxia | CT DSA MRI | 20 | R cerebellar, ectopic | E+MS | Favorable |
| Lopez-Rivera et al., 2020 | M | 6 | Midbrain hemorrhage | MRI DSA | Midbrain cavernoma, ruptured | Headaches | MRI DSA | 2 | R Thalamus | C | N/S |
| Nagm et al., 2015 | F | 23 | Severe headache, seizures | DSA | R frontal AVM, E+MS; ectopic recurrence, reoperated | ASX | MRI DSA | 18 | R Frontal, ectopic | C | N/S |
| Nussbaum et al., 1998 | M | 34 | Headache, vertigo, blurred vision | DSA | R cerebellar AVM, C treatment | Recurrence of headache and vertigo | DSA | 10 | R cerebellar, ectopic | E | Favorable |
| Rodriguez-Arias, 2000 | F | 11 | Seizures | CT DSA MRI | R parietal AVM, treated via SRS | ASX | MRI DSA | 2 | R Parietal (medial) | SRS | Favorable |
| Shi et al., 2018 | M | 72 | Gait instability | CTA DSA | L Frontal AVM (ruptured), resected | L Hemianopsia | CTA DSA | 11 | R Temporooccipital | MS | Favorable |
| Shidoh et al., 2016 | F | 73 | ASX | DSA | Unruptured R MCA aneurysm, clipped | ASX | MRI DSA | 5 | R Parietal (postcentral) | SRS | Favorable |
| Torres-Quinones et al., 2019 | M | 80 | Vertigo | CT DSA MRI | R superior cerebellar aneurysm, hypertension, vermian AVM treated via radiosurgery | Gait instability | MRI DSA | 10 | L Thalamus | N/S | N/S |
| Fuse et al., 2001 | M | 23 | L hemiparesis | CT DSA | R frontal cerebral hemorrhage | ASX | MRI DSA | 4 | R Frontal | MS | Favorable |
| Isayama et al., 1991 | M | 20 | Subcortical hemorrhage | CT DSA | L temporal subcortical hemorrhage, evacuated surgically | Second L temporal hemorrhage | DSA | 2 | L Temporal | MS | N/S |
| Jeffree et al., 2009 | M | 18 | Headache, facial droop, speech deficit, vomiting, LOC | CT DSA MRI | L Parietal hematoma | Facial droop, aphasia, vomiting, LOC | CT DSA | 10 | R Parietooccipital | MS | Favorable |
| Jeffree et al., 2009 | M | 15 | N/S | DSA | R temporo-parietal IPH | ASX | DSA | 5 | R Temporoparietal | MS | Favorable |
| Jeffree et al., 2009 | M | 5 | Irritability, poor feeding, vomiting and jaundice | TUS CT MRI | R temporo-parietal IPH at 17 days after birth | Vomiting, episodes of LOC | CT DSA | 5 | R Sylvian and basal ganglia | SRS | Unfavorable, died 3 months later |
| Lv et al., 2018 | F | 22 | IPH | DSA | Hemorrhage from N/S cause | Seizures and headaches | MRI DSA | 4 | R Parietal | N/S | N/S |
| Mendelow et al., 1987 | N/S | N/S | SAH | Angio. | SAH of N/S origin | SAH | Angio. | 14 | R Occipital | C | N/S |
| Miyasaka et al., 2003 | F | 58 | Headache, vomiting, L hemiparesis | CT Angio. | R parietal IPH | Severe headache, vomiting | CT DSA MRI | 8 | R Frontal, R Parietal, L Occipital | SRS | N/S |
| Morioka et al., 1988 | M | 23 | SAH, LOC | Angio. | SAH of N/S origin | Generalized seizures, postictal R hemiparesis | CT Angio. | 7 | L Frontal | MS | Favorable |
| Nakamura et al., 2016 | M | 53 | L frontal IPH | MRI DSA | IPH, evacuated; local implantation of MSCs producing GLP-1 | Aphasia, focal seizures, new L frontal cerebral hemorrhage | CTA DSA | 3 | L Frontal | MS | Favorable |
| Peeters, 1982 | M | 26 | SAH | Angio. | SAH of N/S origin | Seizures | Angio. | 23 | R Frontal | N/S | N/S |
| Porter and Bull, 1969 | M | 24 | SAH | Angio. | SAH of N/S origin | SAH | Angio. | 2 | R Occipital | N/S | N/S |
| Dogan et al., 2019 | M | 25 | Seizures, recurrent | MRI | R parietal parafalcine arachnoid cyst, seizures | Recurrent seizures | MRI DSA | 14 | L Frontal | C | N/S |
| Kilbourn et al., 2014 | M | 18 | N/S | CT MRI | HCP, absence seizures, autism | Headache, vomiting followed by LOC | CTA DSA MRI | 17 | Pons | C | N/S |
| Markham et al., 2015 | M | 4 | Seizures | MRI | Seizures | Severe headache | MRI DSA | 3 | L Temporal | MS | N/S |
| Neil et al., 2014 | M | 24 | Seizures | MRI | Epilepsy and head trauma | Seizures | MRI DSA | 9 | L Parietal | E+MS | Favorable |
| Ozsarac et al., 2012 | M | 50 | Epilepsy | Angio. | Generalized tonic-clonic seizures | AH (Pink Floyd’s “Another Brick in the Wall”) | CTA | 25 | L Temporoparietal | C | N/S |
| Stevens et al., 2009 | F | 9 | Seizures, developmental delay | MRI | SBH (L temporo-occipital) | Seizures, behav. change, ataxia, and aphasia | CT DSA MRI | 3 | L Parietooccipital | SRS | N/S |
| Wu et al., 2014 | M | 7 | Fever, convulsions | MRI | Febrile seizure | Seizures, L visual scotoma | MRI DSA | 4 | R Occipital | MS | Favorable |
| Yeo et al., 2014 | F | 16 | Single episode of seizures | MRI | Epileptic seizure of N/S cause | Intermittent headaches | MRI | 9 | L Temporal | MS | N/S |
| Yeo et al., 2014 | M | 7 | Seizures | MRI | Epilepsy | Recurrent seizures | MRI DSA | 6 | L cerebellar | SRS | N/S |
| Bennet et al., 2016 | F | 45 | headache, vertigo, nausea, vomiting | CT MRI | Vermian hemangioblastoma | headaches, dizziness | CTA DSA MRI | 1 | L cerebellar (posterior) | MS | Favorable |
| Harris et al., 2000 | M | 57 | headaches, confusion, L sided weakness and numbness | CT carotid Doppler Angio. | R carotid stenosis, malignant R thalamic astrocytoma | Nausea, vomiting, weight loss | MRI Angio. | 0,25 | R Thalamus | Biopsy, SRS | Unfavorable, died 4 months later |
| Koch et al., 2016 | F | 24 | developmental regression | MRI | 4th ventricle ependymoma, HCP, treatment with surgery + radiotherapy | Partial complex seizure | MRI DSA | 23 | L Choroidal | SRS | N/S |
| Lo Presti et al., 2018 | F | 67 | Headaches, L frontal lump | CT | Recurrent meningioma, operated, acrylic cranioplasty | L pulsatile tinnitus | MRI DSA | 7 | L Frontal | MS | Favorable |
| Mathon et al., 2013 | M | 9 | N/S | MRI | 4th ventricle MB, operated, chemo+radio | ASX | MRI DSA | 4 | R Sylvian | E+MS | N/S |
| McKinney et al., 2008 | F | 58 | Transient L-sided weakness | MRI | L thalamic hemorrhage; anaplastic ODG in the same region | L sided weakness, dysarthria, L visual field defect | MRI DSA | 3 | R Frontoparietal | MS | Unfavorable, died on postop day 6 |
| Morales-Valero et al., 2014 | M | 56 | TIA | DSA | TIA, cause N/S | Transient neurological event | DSA | 14 | L Frontal | N/S | N/S |
| Ozawa et al., 1998 | M | 39 | Headache, vomiting, weakness in L arm | CT DSA MRI | Thrombosis of SSS and R TS | ASX | MRI DSA | 2 | R Parietal | E+MS | Favorable |
| Pabaney et al., 2016 | F | 52 | R hemiplegia and severe dysarthria | CTA MRI | Acute L frontal ischemic stroke | Generalized tonic-clonic seizure, L frontal IPH | CTA DSA | 8 | L Frontal | MS | N/S |
| Santos et al., 2018 | M | 7 | Mild L hemiparesis | MRI DSA | R PComA aneurysm, R hemispheric stroke; | ASX | DSA | 6 | R Thalamus | C | N/S |
| Shi et al., 2018 | F | 33 | Headache | MRV | L TS thrombosis | ASX | MRI DSA | 2 | L Temporooccipital | C | Favorable |
| Fujimura et al., 2014 | F | 14 | Weakness in upper limbs | MRI | MMD, bilateral revascularization | ASX | MRI DSA | 4 | R Occipital | C | Favorable |
| Noh et al., 2014 | F | 15 | TIA on R side | MRI DSA | MMD | ASX | DSA | 8 | R Frontal interhemispheric | C | Favorable |
| O’Shaughnessy, 2005 | M | 6 | Infarction, dysphasia, R hemiparesis | MRI | SS-disease, MMD, L frontal cerebral infarction | Mild dysphasia, mild R hemiparesis | MRI DSA | 3 | R Sylvian | MS | Favorable |
| Schmidt et al., 1996 | M | 11 | R arm and leg weakness | CT Angio. | MMD, infarction | ASX | MRI DSA SPECT | 8 | L Parietal | N/S | N/S |
| Gonzalez et al., 2005 | F | 7 | Head trauma | MRI | Traffic accident, L frontal hemorrhage | Unremitting seizures | MRI DSA | 4 | R Temporal | SRS | Favorable |
| Krayenbuhl, 1977 | M | 12 | Headache, vomiting, stiffness of the neck | Angio. | SAH of N/S origin, from head trauma | Headache, LOC, meningeal irritation | Angio. | 9 | R Frontal | MS | Favorable |
| Miller et al., 2014 | F | 12 | Head trauma | CT | Severe TBI, L SDH; cranioplasty | Seizures, increased frequency | MRI DSA | 11 | L Parietal | MS | Favorable |
| Shimoda et al., 2015 | M | 5 | ASX—screening for HHT | MRI | HHT | Recurrent epistaxis, thunderclap headache | MRI DSA | 4 | R Parietal | E+MS | Favorable |
| Song et al., 2007 | F | 2,5 | Congestive heart failure | MRI | Cardiomegaly and CHF; hepatic hemangiomas | Intermittent downward gaze, gait instability, DD | MRI DSA | 2,5 | L CPA | E | Initially favorable; died at the age of 6 due to cerebral hemorrhage |
| Bulsara et al., 2002 | F | 32 | Intermittent monocular vision loss, ataxia, diplopia, ptosis, blurred vision, aphasia, gait disturbance | DSA MRI PET | Inflammation/demyelinating lesion in brainstem and diencephalon | Severe headache, nausea, vomiting, ruptured AVM | CTA DSA MRI | 6 | R Temporal | MS | Favorable |
| Mahajan et al., 2009 | F | 30 | Facial nerve palsy | MRI | Bell’s palsy | Migraines, R-sided facial weakness, aphasia | CT DSA MRI | 14 | L Frontoparietal | N/S | N/S |
| Gondar et al., 2019 | F | 57 | Mild head trauma | MRI | Cirrhosis, R pre-central DVA, TBI after alcohol poisoning | Gait imbalance dysarthria, L hemiparesis | CT DSA MRI | 2 | R Frontal precentral | SRS | Unfavorable, died 2 weeks later due to PE |
| Morales-Valero et al., 2014 | F | 35 | Confusion | MRI | Liver cirrhosis, PSE | IPH | MRI DSA | 4 | L Parietooccipital | N/S | N/S |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Florian, I.A.; Beni, L.; Moisoiu, V.; Timis, T.L.; Florian, I.S.; Balașa, A.; Berindan-Neagoe, I. ‘De Novo’ Brain AVMs—Hypotheses for Development and a Systematic Review of Reported Cases. Medicina 2021, 57, 201. https://doi.org/10.3390/medicina57030201
Florian IA, Beni L, Moisoiu V, Timis TL, Florian IS, Balașa A, Berindan-Neagoe I. ‘De Novo’ Brain AVMs—Hypotheses for Development and a Systematic Review of Reported Cases. Medicina. 2021; 57(3):201. https://doi.org/10.3390/medicina57030201
Chicago/Turabian StyleFlorian, Ioan Alexandru, Lehel Beni, Vlad Moisoiu, Teodora Larisa Timis, Ioan Stefan Florian, Adrian Balașa, and Ioana Berindan-Neagoe. 2021. "‘De Novo’ Brain AVMs—Hypotheses for Development and a Systematic Review of Reported Cases" Medicina 57, no. 3: 201. https://doi.org/10.3390/medicina57030201
APA StyleFlorian, I. A., Beni, L., Moisoiu, V., Timis, T. L., Florian, I. S., Balașa, A., & Berindan-Neagoe, I. (2021). ‘De Novo’ Brain AVMs—Hypotheses for Development and a Systematic Review of Reported Cases. Medicina, 57(3), 201. https://doi.org/10.3390/medicina57030201







