Multiparametric Monitoring of Hypnosis and Nociception-Antinociception Balance during General Anesthesia—A New Era in Patient Safety Standards and Healthcare Management
Abstract
1. Introduction
2. Multimodal Monitoring Techniques for the Degree of Hypnosis
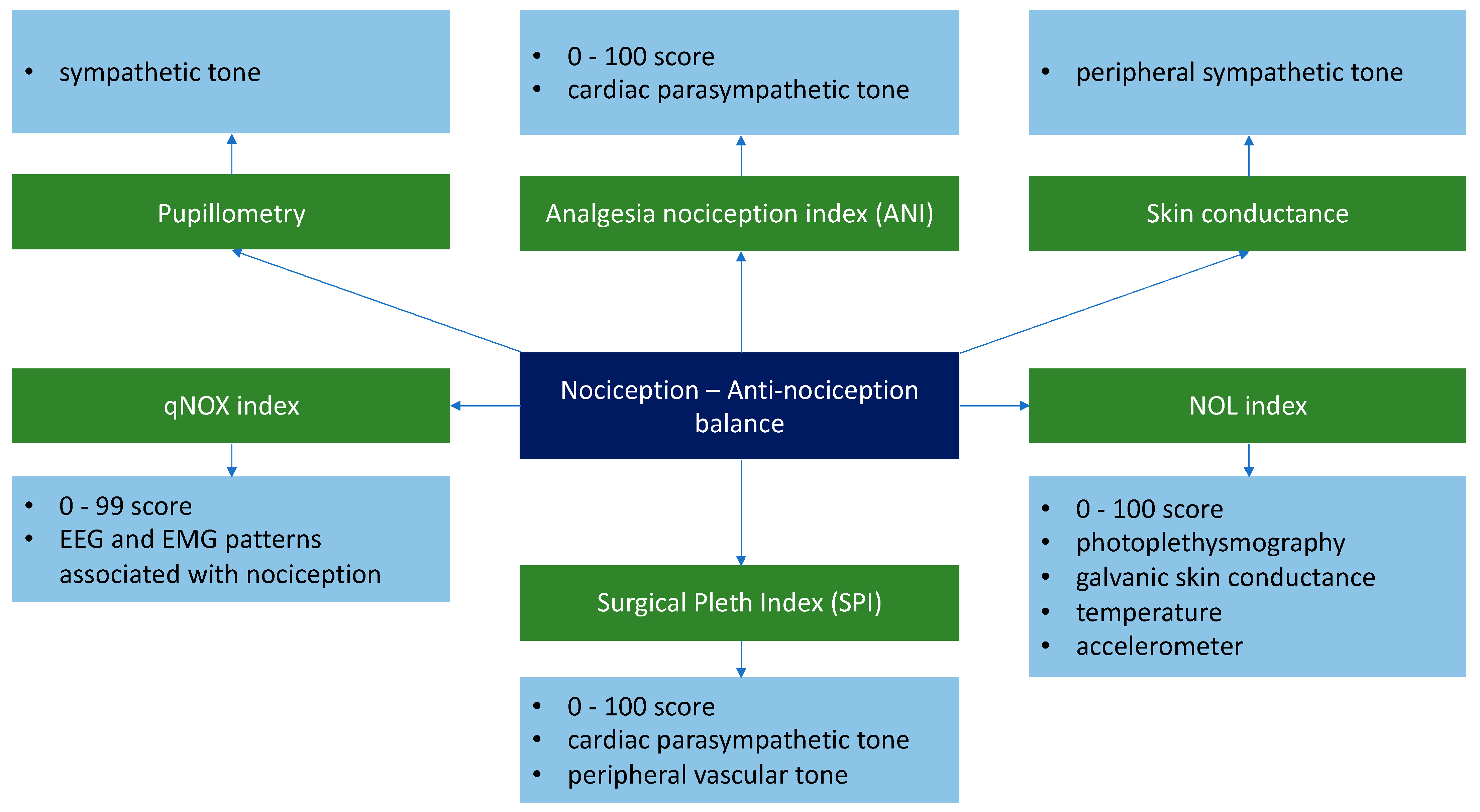
3. Monitoring Techniques for the Nociception-Antinociception Balance
4. The Impact of Multimodal Monitoring on the Hemodynamic Status
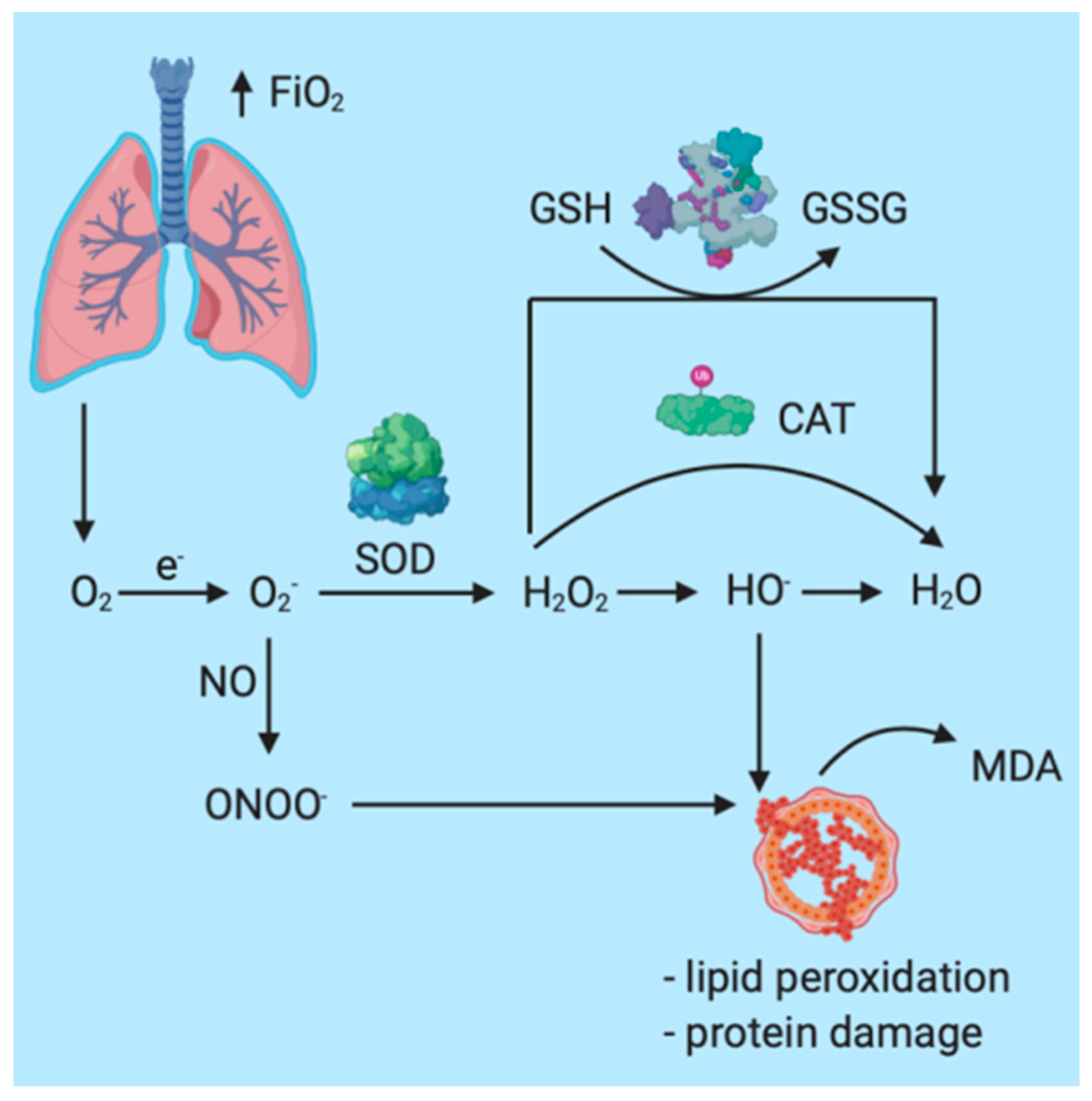
5. The Impact of General Anesthesia Multimodal Monitoring on Inflammation/Redox
6. The Impact of Multiparametric Monitoring on Drug Consumption and Recovery
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosenberger, P.; Drexler, B. Development of Anaesthesia-Related Mortality and Impact on Perioperative Outcome. Anasthesiol. Intensivmed. Notfallmed. Schmerzther. 2017, 52, 486–497. [Google Scholar] [CrossRef] [PubMed]
- Guerrero, J.L.; Matute, E.; Alsina, E.; Del Blanco, B.; Gilsanz, F. Response entropy changes after noxius stimulus. J. Clin. Monit. Comput. 2012, 26, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, A.; Schmidt, M.; Zeitler, C.; Kiessling, A.-H.; Isgro, F.; Boldt, J. Bispectral index and electroencephalographic entropy in patients undergoing aortocoronary bypass grafting. Eur. J. Anaesthesiol. 2007, 24, 751–760. [Google Scholar] [CrossRef] [PubMed]
- Medical Advisory Secretariat. Bispectral index monitor: An evidence-based analysis. Ont. Health Technol. Assess. Ser. 2004, 4, 1–70. [Google Scholar]
- Hebb, M.O.; McArthur, D.L.; Alger, J.; Etchepare, M.; Glenn, T.C.; Bergsneider, M.; Martin, N.; Vespa, P.M. Impaired percent alpha variability on continuous electroencephalography is associated with thalamic injury and predicts poor long-term outcome after human traumatic brain injury. J. Neurotrauma 2007, 24, 579–590. [Google Scholar] [CrossRef] [PubMed]
- Petras, M.; Tatarkova, Z.; Kovalska, M.; Mokra, D.; Dobrota, D.; Lehotsky, J.; Drgova, A. Hyperhomocysteinemia as a risk factor for the neuronal system disorders. J. Physiol. Pharmacol. 2014, 65, 15–23. [Google Scholar] [CrossRef]
- Sleigh, J.; Harvey, M.; Voss, L.; Denny, B. Ketamine—More mechanisms of action than just NMDA blockade. Trends Anaesth. Crit. Care 2014, 4, 76–81. [Google Scholar] [CrossRef]
- Abushik, P.A.; Niittykoski, M.; Giniatullina, R.; Shakirzyanova, A.; Bart, G.; Fayuk, D.; Sibarov, D.A.; Antonov, S.M.; Giniatullin, R. The role of NMDA and mGluR5 receptors in calcium mobilization and neurotoxicity of homocysteine in trigeminal and cortical neurons and glial cells. J. Neurochem. 2014, 129, 264–274. [Google Scholar] [CrossRef]
- Dinu, A.R.; Rogobete, A.F.; Popovici, S.E.; Bedreag, O.H.; Papurica, M.; Dumbuleu, C.M.; Velovan, R.R.; Toma, D.; Georgescu, C.M.; Trache, L.I.; et al. Impact of general anesthesia guided by state entropy (SE) and response entropy (RE) on perioperative stability in elective laparoscopic cholecystectomy patients—A prospective observational randomized monocentric study. Entropy 2020, 22, 356. [Google Scholar] [CrossRef]
- Bergmann, I.; Göhner, A.; Crozier, T.A.; Hesjedal, B.; Wiese, C.H.; Popov, A.F.; Bauer, M.; Hinz, J.M. Surgical pleth index-guided remifentanil administration reduces remifentanil and propofol consumption and shortens recovery times in outpatient anaesthesia. Br. J. Anaesth. 2013, 110, 622–628. [Google Scholar] [CrossRef]
- Aho, A.J.; Kamata, K.; Jäntti, V.; Kulkas, A.; Hagihira, S.; Huhtala, H.; Yli-Hankala, A. Comparison of Bispectral Index and Entropy values with electroencephalogram during surgical anaesthesia with sevoflurane. Br. J. Anaesth. 2015, 115, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Freye, E.; Levy, J.V. Cerebral Monitoring in the Operating Room and the Intensive Care Unit: An Introductory for the Clinician and a Guide for the Novice Wanting to Open a Window to the Brain; Springer: Dordrecht, The Netherlands, 2005; Volume 19, ISBN 1087700507. [Google Scholar]
- Klockars, J.G.M.; Hiller, A.; Münte, S.; Van Gils, M.J.; Taivainen, T. Spectral entropy as a measure of hypnosis and hypnotic drug effect of total intravenous anesthesia in children during slow induction and maintenance. Anesthesiology 2012, 116, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Bibian, S.; Dumont, G.A.; Zikov, T. Dynamic behavior of BIS, M-entropy and neuroSENSE brain function monitors. J. Clin. Monit. Comput. 2011, 25, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Shortal, B.P.; Hickman, L.B.; Mak-McCully, R.A.; Wang, W.; Brennan, C.; Ung, H.; Litt, B.; Tarnal, V.; Janke, E.; Picton, P.; et al. Duration of EEG suppression does not predict recovery time or degree of cognitive impairment after general anaesthesia in human volunteers. Br. J. Anaesth. 2019, 123, 206–218. [Google Scholar] [CrossRef]
- Schultz, A.; Siedenberg, M.; Grouven, U.; Kneif, T.; Schultz, B. Comparison of narcotrend index, bispectral index, spectral and entropy parameters during induction of propofol-remifentanil anaesthesia. J. Clin. Monit. Comput. 2008, 22, 103–111. [Google Scholar] [CrossRef]
- Singh, S.; Bansal, S.; Kumar, G.; Gupta, I.; Thakur, J.R. Entropy as an indicator to measure depth of anaesthesia for Laryngeal Mask Airway (LMA) insertion during sevoflurane and propofol anaesthesia. J. Clin. Diagn. Res. 2017, 11, UC01–UC03. [Google Scholar] [CrossRef]
- Iannuzzi, M.; Iannuzzi, E.; Rossi, F.; Berrino, L.; Chiefari, M. Relationship between Bispectral Index, electroencephalographic state entropy and effect-site EC 50 for propofol at different clinical endpoints. Br. J. Anaesth. 2005, 94, 492–495. [Google Scholar] [CrossRef]
- Wildemeersch, D.; Peeters, N.; Saldien, V.; Vercauteren, M.; Hans, G. Pain assessment by pupil dilation reflex in response to noxious stimulation in anaesthetized adults. Acta Anaesthesiol. Scand. 2018, 62, 1050–1056. [Google Scholar] [CrossRef]
- Kumar, A.; Anand, S. A depth of anaesthesia index from linear regression of EEG parameters. J. Clin. Monit. Comput. 2006, 20, 67–73. [Google Scholar] [CrossRef]
- Jagadeesan, N.; Wolfson, M.; Chen, Y.; Willingham, M.; Avidan, M.S. Brain monitoring during general anesthesia. Trends Anaesth. Crit. Care 2013, 3, 13–18. [Google Scholar] [CrossRef]
- Johansen, J.W.; Sebel, P.S. Development and clinical application electroencephalographic bispectrum monitoring. Anesthesiology 2000, 93, 1336–1344. [Google Scholar] [CrossRef] [PubMed]
- Rogobete, A.F.; Bedreag, O.H.; Sandesc, D. Entropy-Guided Depth of Anesthesia in Critically Ill Polytrauma Patients. J. Interdiscip. Med. 2017, 2, 7–8. [Google Scholar] [CrossRef][Green Version]
- Klockars, J.G.M.; Hiller, A.; Ranta, S.; Talja, P.; Van Gils, M.J.; Taivainen, T. Spectral entropy as a measure of hypnosis in children. Anesthesiology 2006, 104, 708–717. [Google Scholar] [CrossRef] [PubMed]
- Cotae, A.; Grinţescu, I.M. Entropy—The Need of an Ally for Depth of Anesthesia Monitoring in Emergency Surgery. CEACR 2019, 13–15. [Google Scholar] [CrossRef]
- Lonjaret, L.; Lairez, O.; Minville, V.; Geeraerts, T. Optimal perioperative management of arterial blood pressure. Integr. Blood Press. Control 2014, 7, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Südfeld, S.; Brechnitz, S.; Wagner, J.Y.; Reese, P.C.; Pinnschmidt, H.O.; Reuter, D.A.; Saugel, B. Post-induction hypotension and early intraoperative hypotension associated with general anaesthesia. Br. J. Anaesth. 2017, 119, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Hoppe, P.; Kouz, K.; Saugel, B. Perioperative hypotension: Clinical impact, diagnosis, and therapeutic approaches. J. Emerg. Crit. Care Med. 2020, 4, 8. [Google Scholar] [CrossRef]
- Barnard, J.P.; Bennett, C.; Voss, L.J.; Sleigh, J.W.; Hospital, W.; Zealand, N. Neurosciences and neuroanaesthesia can anaesthetists be taught to interpret the effects of general anaesthesia on the electroencephalogram? Comparison of performance with the BIS and spectral entropy. Br. J. Anaesth. 2007, 99, 532–537. [Google Scholar] [CrossRef]
- Chen, S.J.; Peng, C.J.; Chen, Y.C.; Hwang, Y.R.; Lai, Y.S.; Fan, S.Z.; Jen, K.K. Comparison of FFT and marginal spectra of EEG using empirical mode decomposition to monitor anesthesia. Comput. Methods Programs Biomed. 2016, 137, 77–85. [Google Scholar] [CrossRef]
- Kreuer, S.; Wilhelm, W. The Narcotrend monitor. Best Pract. Res. Clin. Anaesthesiol. 2006, 20, 111–119. [Google Scholar] [CrossRef]
- Kreuer, S.; Bruhn, J.; Larsen, R.; Bialas, P.; Wilhelm, W. Comparability of NarcotrendTM index and bispectral index during propofol anaesthesia. Br. J. Anaesth. 2004, 93, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Kreuer, S.; Biedler, A.; Larsen, R.; Schoth, S.; Altmann, S.; Wilhelm, W. The Narcotrend—A new EEG monitor designed to measure the depth of anaesthesia. A comparison with bispectral index monitoring during propofol-remifentanil-anaesthesia. Anaesthesist 2001, 50, 921–925. [Google Scholar] [CrossRef] [PubMed]
- Dennhardt, N.; Arndt, S.; Beck, C.; Boethig, D.; Heiderich, S.; Schultz, B.; Weber, F.; Sümpelmann, R. Effect of age on Narcotrend Index monitoring during sevoflurane anesthesia in children below 2 years of age. Paediatr. Anaesth. 2018, 28, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Suo, P.; Yuan, X.; Yao, X. Use of auditory evoked potentials for intra-operative awareness in anesthesia: A consciousness-based conceptual model. Cell Biochem. Biophys. 2015, 71, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Mantzaridis, H.; Kenny, G.N. Auditory evoked potential index: A quantitative measure of changes in auditory evoked potentials during general anaesthesia. Anaesthesia 1997, 52, 1030–1036. [Google Scholar] [CrossRef]
- Khan, J.; Mariappan, R.; Venkatraghavan, L. Entropy as an indicator of cerebral perfusion in patients with increased intracranial pressure. J. Anaesthesiol. Clin. Pharmacol. 2014, 30, 409. [Google Scholar] [CrossRef] [PubMed]
- Illman, H.; Antila, H.; Olkkola, K.T. Reversal of neuromuscular blockade by sugammadex does not affect EEG derived indices of depth of anesthesia. J. Clin. Monit. Comput. 2010, 24, 371–376. [Google Scholar] [CrossRef]
- Schartner, M.M.; Carhart-Harris, R.L.; Barrett, A.B.; Seth, A.K.; Muthukumaraswamy, S.D. Increased spontaneous MEG signal diversity for psychoactive doses of ketamine, LSD and psilocybin. Sci. Rep. 2017, 7, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Abdelmageed, W.M.; Al Taher, W.M. Preoperative paracetamol infusion reduces sevoflurane consumption during thyroidectomy under general anesthesia with spectral entropy monitoring. Egypt. J. Anaesth. 2014, 30, 115–122. [Google Scholar] [CrossRef]
- Tiefenthaler, W.; Colvin, J.; Steger, B.; Pfeiffer, K.P.; Moser, P.L.; Walde, J.; Lorenz, I.H.; Kolbitsch, C. How bispectral index compares to spectral entropy of the EEG and A-line ARX index in the same patient. Open Med. 2018, 13, 583–596. [Google Scholar] [CrossRef]
- Sullivan, C.A.; Egbuta, C.; Park, R.S.; Lukovits, K.; Cavanaugh, D.; Mason, K.P. The Use of Bispectral Index Monitoring Does Not Change Intraoperative Exposure to Volatile Anesthetics in Children. J. Clin. Med. 2020, 9, 2437. [Google Scholar] [CrossRef] [PubMed]
- Maksimow, A.; Särkelä, M.; Långsjö, J.W.; Salmi, E.; Kaisti, K.K.; Yli-Hankala, A.; Hinkka-Yli-Salomäki, S.; Scheinin, H.; Jääskeläinen, S.K. Increase in high frequency EEG activity explains the poor performance of EEG spectral entropy monitor during S-ketamine anesthesia. Clin. Neurophysiol. 2006, 117, 1660–1668. [Google Scholar] [CrossRef]
- Davidson, A.J.; Huang, G.H.; Rebmann, C.S.; Ellery, C. Performance of entropy and Bispectral Index as measures of anaesthesia effect in children of different ages. Br. J. Anaesth. 2005, 95, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Choi, W. Effect of preoperative anxiety on spectral entropy during induction with propofol. Korean J. Anesthesiol. 2013, 65, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Wang, P.; Liao, W.; Shih, T.; Chang, K.; Lin, K.; Chou, A. Use of Spectral Entropy Monitoring in Reducing the Quantity of Sevoflurane as Sole Inhalational Anesthetic and in Decreasing the Need for Antihypertensive Drugs in Total Knee Replacement Surgery. Acta Anaesthesiol. Taiwanica 2008, 46, 106–111. [Google Scholar] [CrossRef]
- Vakkuri, A.; Yli-hankala, A.; Sandin, R.; Mustola, S. Spectral Entropy Monitoring Is Associated with Reduced Propofol Use and Faster Emergence in Propofol—Nitrous Oxide—Alfentanil Anesthesia. J. Am. Soc. Anesthesiol. 2005, 103, 274–279. [Google Scholar] [CrossRef]
- Talawar, P.; Chhabra, A.; Trikha, A.; Arora, M.K. Chandralekha Entropy monitoring decreases isoflurane concentration and recovery time in pediatric day care surgery—A randomized controlled trial. Paediatr. Anaesth. 2010, 20, 1105–1110. [Google Scholar] [CrossRef]
- Elgebaly, A.S.; El Mourad, M.B.; Fathy, S.M. The role of entropy monitoring in reducing propofol requirements during open heart surgeries. A prospective randomized study. Ann. Card. Anaesth. 2020, 23, 272–276. [Google Scholar] [CrossRef]
- Bhardwaj, N.; Yaddanapudi, S. A randomized trial of propofol consumption and recovery profile with BIS-guided anesthesia compared to standard practice in children. Paediatr. Anaesth. 2010, 20, 160–167. [Google Scholar] [CrossRef]
- Aime, I.; Taylor, G. Does Monitoring Bispectral Index or Spectral Entropy Reduce Sevoflurane Use? Anesth. Analg. 2006, 103. [Google Scholar] [CrossRef]
- Liao, W.-W.; Wang, J.-J.; Wu, G.-J.; Kuo, C.-D. The effect of cerebral monitoring on recovery after sevoflurane anesthesia in ambulatory setting in children: A comparison among bispectral index, A-line autoregressive index, and standard practice. J. Chin. Med. Assoc. 2011, 74, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Weber, F.; Geerts, N.J.E.; Roeleveld, H.G.; Warmenhoven, A.T.; Liebrand, C.A. The predictive value of the heart rate variability-derived Analgesia Nociception Index in children anaesthetized with sevoflurane: An observational pilot study. Eur. J. Pain 2018, 22, 1597–1605. [Google Scholar] [CrossRef] [PubMed]
- Lai, R.-C.; Lu, Y.-L.; Huang, W.; Xu, M.-X.; Lai, J.-L.; Xie, J.-D.; Wang, X.-D. [Application of a narcotrend-assisted anesthesia in-depth monitor in the microwave coagulation for liver cancer during total intravenous anesthesia with propofol and fentanyl]. Chin. J. Cancer 2010, 29, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Rundshagen, I.; Hardt, T.; Cortina, K.; Pragst, F.; Fritzsche, T.; Spies, C. Narcotrend-assisted propofol/remifentanil anaesthesia vs clinical practice: Does it make a difference? Br. J. Anaesth. 2007, 99, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Sebel, P.S.; Bowdle, T.A.; Ghoneim, M.M.; Rampil, I.J.; Padilla, R.E.; Gan, T.J.; Domino, K.B. The incidence of awareness during anesthesia: A multicenter United States study. Anesth. Analg. 2004, 99, 833–839. [Google Scholar] [CrossRef]
- Ekman, A.; Lindholm, M.-L.; Lennmarken, C.; Sandin, R. Reduction in the incidence of awareness using BIS monitoring. Acta Anaesthesiol. Scand. 2004, 48, 20–26. [Google Scholar] [CrossRef]
- Fiedler, M.O.; Schätzle, E.; Contzen, M.; Gernoth, C.; Weiß, C.; Walter, T.; Viergutz, T.; Kalenka, A. Evaluation of Different Positive End-Expiratory Pressures Using SupremeTM Airway Laryngeal Mask during Minor Surgical Procedures in Children. Medicina 2020, 56, 551. [Google Scholar] [CrossRef]
- Bonhomme, V.; Uutela, K.; Hans, G.; Maquoi, I.; Born, J.D.; Brichant, J.F.; Lamy, M.; Hans, P. Comparison of the Surgical Pleth IndexTM with haemodynamic variables to assess nociception-anti-nociception balance during general anaesthesia. Br. J. Anaesth. 2011, 106, 101–111. [Google Scholar] [CrossRef]
- Boselli, E.; Bouvet, L.; Bégou, G.; Dabouz, R.; Davidson, J.; Deloste, J.Y.; Rahali, N.; Zadam, A.; Allaouchiche, B. Prediction of immediate postoperative pain using the analgesia/nociception index: A prospective observational study. Br. J. Anaesth. 2014, 112, 715–721. [Google Scholar] [CrossRef]
- Ledowski, T.; Ang, B.; Schmarbeck, T.; Rhodes, J. Monitoring of sympathetic tone to assess postoperative pain: Skin conductance vs surgical stress index. Anaesthesia 2009, 64, 727–731. [Google Scholar] [CrossRef]
- Nie, F.; Liu, T.; Zhong, L.; Yang, X.; Liu, Y.; Xia, H.; Liu, X.; Wang, X.; Liu, Z.; Zhou, L.I.; et al. MicroRNA-148b enhances proliferation and apoptosis in human renal cancer cells via directly targeting MAP3K9. Mol. Med. Rep. 2016, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Jess, G.; Pogatzki-Zahn, E.M.; Zahn, P.K.; Meyer-Frießem, C.H. Monitoring heart rate variability to assess experimentally induced pain using the analgesia nociception index. Eur. J. Anaesthesiol. 2016, 33, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Edry, R.; Recea, V.; Dikust, Y.; Sessler, D.I. Preliminary Intraoperative Validation of the Nociception Level Index: A Noninvasive Nociception Monitor. Anesthesiology 2016, 125, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Gruenewald, M.; Dempfle, A. Analgesia/nociception monitoring for opioid guidance: Meta-Analysis of randomized clinical trials. Minerva Anestesiol. 2017, 83, 200–213. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.L.; Kong, X.Q.; Ji, F.H. Effect of dexmedetomidine on intraoperative Surgical Pleth Index in patients undergoing video-assisted thoracoscopic lung lobectomy. J. Cardiothorac. Surg. 2020, 15, 1–7. [Google Scholar] [CrossRef]
- Kim, J.H.; Jwa, E.K.; Choung, Y.; Yeon, H.J.; Kim, S.Y.; Kim, E. Comparison of Pupillometry With Surgical Pleth Index Monitoring on Perioperative Opioid Consumption and Nociception During Propofol–Remifentanil Anesthesia: A Prospective Randomized Controlled Trial. Anesth. Analg. 2020, 131, 1589–1598. [Google Scholar] [CrossRef]
- Huiku, M.; Uutela, K.; van Gils, M.; Korhonen, I.; Kymalainen, M.; Merilainen, P.; Paloheimo, M.; Rantanen, M.; Takala, P.; Viertio-Oja, H.; et al. Assessment of surgical stress during general anaesthesia. Br. J. Anaesth. 2007, 98, 447–455. [Google Scholar] [CrossRef]
- Dostalova, V.; Schreiberova, J.; Bartos, M.; Kukralova, L.; Dostal, P. Surgical pleth index and analgesia nociception index for intraoperative analgesia in patients undergoing neurosurgical spinal procedures: A comparative randomized study. Minerva Anestesiol. 2019, 85, 1265–1272. [Google Scholar] [CrossRef]
- Funcke, S.; Saugel, B.; Koch, C.; Schulte, D.; Zajonz, T.; Sander, M.; Gratarola, A.; Ball, L.; Pelosi, P.; Spadaro, S.; et al. Individualized, perioperative, hemodynamic goal-directed therapy in major abdominal surgery (iPEGASUS trial): Study protocol for a randomized controlled trial. Trials 2018, 19, 273. [Google Scholar] [CrossRef]
- Jain, N.; Gera, A.; Sharma, B.; Sood, J.; Chugh, P. Comparison of Surgical Pleth Index-guided analgesia using fentanyl versus conventional analgesia technique in laparoscopic cholecystectomy. Minerva Anestesiol. 2019, 85, 358–365. [Google Scholar] [CrossRef]
- Won, Y.J.; Lim, B.G.; Lee, S.H.; Park, S.; Kim, H.; Lee, I.O.; Kong, M.H. Comparison of relative oxycodone consumption in surgical pleth index-guided analgesia versus conventional analgesia during sevoflurane anesthesia. Medicina 2016, 95, e4743. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Thee, C.; Gruenewald, M.; Ilies, C.; Höcker, J.; Hanss, R.; Steinfath, M.; Bein, B. Correlation of Surgical Pleth Index with Stress Hormones during Propofol-Remifentanil Anaesthesia. Sci. World J. 2012, 2012, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Theerth, K.A.; Sriganesh, K.; Reddy, K.M.; Chakrabarti, D.; Umamaheswara Rao, G.S. Analgesia Nociception Index-guided intraoperative fentanyl consumption and postoperative analgesia in patients receiving scalp block versus incision-site infiltration for craniotomy. Minerva Anestesiol. 2018, 84, 1361–1368. [Google Scholar] [CrossRef] [PubMed]
- Soral, M.; Altun, G.T.; Dinçer, P.Ç.; Arslantaş, M.K.; Aykaç, Z. Effectiveness of the analgesia nociception index monitoring in patients who undergo colonoscopy with sedo-analgesia. Turk. J. Anaesthesiol. Reanim. 2020, 48, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Gall, O.; Champigneulle, B.; Schweitzer, B.; Deram, T.; Maupain, O.; Montmayeur Verchere, J.; Orliaguet, G. Postoperative pain assessment in children: A pilot study of the usefulness of the analgesia nociception index. Br. J. Anaesth. 2015, 115, 890–895. [Google Scholar] [CrossRef]
- Jensen, E.W.; Valencia, J.F.; López, A.; Anglada, T.; Agustí, M.; Ramos, Y.; Serra, R.; Jospin, M.; Pineda, P.; Gambus, P. Monitoring hypnotic effect and nociception with two EEG-derived indices, qCON and qNOX, during general anaesthesia. Acta Anaesthesiol. Scand. 2014, 58, 933–941. [Google Scholar] [CrossRef]
- Reich, D.L.; Hossain, S.; Krol, M.; Baez, B.; Patel, P.; Bernstein, A.; Bodian, C.A. Predictors of hypotension after induction of general anesthesia. Anesth. Analg. 2005, 101, 622–628, table of contents. [Google Scholar] [CrossRef]
- Hug, C.C.J.; McLeskey, C.H.; Nahrwold, M.L.; Roizen, M.F.; Stanley, T.H.; Thisted, R.A.; Walawander, C.A.; White, P.F.; Apfelbaum, J.L.; Grasela, T.H. Hemodynamic effects of propofol: Data from over 25,000 patients. Anesth. Analg. 1993, 77, S21–S29. [Google Scholar]
- Thwaites, A.; Edmends, S.; Smith, I. Inhalation induction with sevoflurane: A double-blind comparison with propofol. Br. J. Anaesth. 1997, 78, 356–361. [Google Scholar] [CrossRef]
- Liu, T.J.; Zhang, J.C.; Gao, X.Z.; Tan, Z.B.; Wang, J.J.; Zhang, P.P.; Cheng, A.B.; Zhang, S.B. Effect of sevoflurane on the ATPase activity of hippocampal neurons in a rat model of cerebral ischemia-reperfusion injury via the cAMP-PKA signaling pathway. Kaohsiung J. Med. Sci. 2018, 34, 22–33. [Google Scholar] [CrossRef]
- Bijker, J.B.; Van Klei, W.A.; Kappen, T.H.; Van Wolfswinkel, L.; Moons, K.G.M.; Kalkman, C.J. Incidence of intraoperative hypotension as a function of the chosen definition: Literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology 2007, 107, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.S.; Hongo, K.; Nakagawa, H. Adverse effects of limited hypotensive anesthesia on the outcome of patients with subarachnoid hemorrhage. J. Neurosurg. 2000, 92, 971–975. [Google Scholar] [CrossRef] [PubMed]
- Monk, T.G. Processed EEG and patient outcome. Best Pract. Res. Clin. Anaesthesiol. 2006, 20, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Wesselink, E.M.; Kappen, T.H.; Torn, H.M.; Slooter, A.J.C.; van Klei, W.A. Intraoperative hypotension and the risk of postoperative adverse outcomes: A systematic review. Br. J. Anaesth. 2018, 121, 706–721. [Google Scholar] [CrossRef]
- Ristovic, V.; de Roock, S.; Mesana, T.; van Diepen, S.; Sun, L. The Impact of Preoperative Risk on the Association between Hypotension and Mortality after Cardiac Surgery: An Observational Study. J. Clin. Med. 2020, 9, 2057. [Google Scholar] [CrossRef]
- Walsh, M.; Kurz, A.; Turan, A.; Rodseth, R.N.; Cywinski, J.; Thabane, L.; Sessler, D.I. Relationship between Intraoperative Mean. Anesthesiology 2013, 119, 507–515. [Google Scholar] [CrossRef]
- Bedreag, O.H.; Sandesc, D.; Chiriac, S.D.; Rogobete, A.F.; Cradigati, A.C.; Sarandan, M.; Dumache, R.; Nartita, R.; Papurica, M. The Use of Circulating miRNAs as Biomarkers for Oxidative Stress in Critically Ill Polytrauma Patients. Clin. Lab. 2016, 62, 263–274. [Google Scholar] [CrossRef]
- Bratu, L.M.; Rogobete, A.F.; Sandesc, D.; Bedreag, O.H.; Tanasescu, S.; Nitu, R.; Popovici, S.E.; Crainiceanu, Z.P. The Use of Redox Expression and Associated Molecular Damage to Evaluate the Inflammatory Response in Critically Ill Patient with Severe Burn. Biochem. Genet. 2016, 54. [Google Scholar] [CrossRef]
- Bedreag, O.H.; Rogobete, A.F.; Sandesc, D.; Cradigati, C.A.; Sarandan, M.; Popovici, S.E.; Dumache, R.; Horhat, F.G.; Vernic, C.; Sima, L.V.; et al. Modulation of the Redox Expression and Inflammation Response in the Critically Ill Polytrauma Patient with Thoracic Injury. Statistical Correlations between Antioxidant Therapy. Clin. Lab. 2016, 62, 1747–1759. [Google Scholar] [CrossRef]
- Papurica, M.; Rogobete, A.F.; Sandesc, D.; Dumache, R.; Nartita, R.; Sarandan, M.; Cradigati, A.C.; Luca, L.; Vernic, C.; Bedreag, O.H. Redox Changes Induced by General Anesthesia in Critically Ill Patients with Multiple Traumas. Mol. Biol. Int. 2015, 2015, 238586. [Google Scholar] [CrossRef]
- Dinu, A.R.; Rogobete, A.F.; Bratu, T.; Popovici, S.E.; Bedreag, O.H.; Papurica, M.; Bratu, L.M.; Sandesc, D. Cannabis Sativa Revisited—Crosstalk between microRNA Expression, Inflammation, Oxidative Stress, and Endocannabinoid Response System in Critically Ill Patients with Sepsis. Cells 2020, 9, 307. [Google Scholar] [CrossRef] [PubMed]
- Nunes, R.R.; Nora, F.S.; Maia, D.; Dumaresq, H.; Maria, R.; Cavalcante, A.; Costa, A.A.; Moreira, L.; Carneiro, M.; Cesar, J.; et al. Influence of Total Intravenous Anesthesia, Entropy and Laparoscopy on Oxidative Stress. Braz. J. Anesthesiol. 2012, 62, 484–501. [Google Scholar] [CrossRef][Green Version]
- Gruber, J.; Fong, S.; Chen, C.; Yoong, S.; Pastorin, G.; Schaffer, S.; Cheah, I.; Halliwell, B. Mitochondria-targeted antioxidants and metabolic modulators as pharmacological interventions to slow ageing. Biotechnol. Adv. 2013, 31, 563–592. [Google Scholar] [CrossRef] [PubMed]
- Lipina, C.; Hundal, H.S. Modulation of cellular redox homeostasis by the endocannabinoid system. Open Biol. 2016, 6, 150276. [Google Scholar] [CrossRef] [PubMed]
- Heyland, D.K.; Dhaliwal, R.; Suchner, U.; Berger, M.M. Antioxidant nutrients: A systematic review of trace elements and vitamins in the critically ill patient. Intensive Care Med. 2005, 31, 327–337. [Google Scholar] [CrossRef]
- Sailaja Rao, P.; Kalva, S.; Yerramilli, A.; Mamidi, S. Free Radicals and Tissue Damage: Role of Antioxidants. Free Radic. Antioxid. 2011, 1, 2–7. [Google Scholar] [CrossRef]
- Hagar, H.H. An insight into the possible protective effect of pyrrolidine dithiocarbamate against lipopolysaccharide-induced oxidative stress and acute hepatic injury in rats. Saudi Pharm. J. 2009, 17, 259–267. [Google Scholar] [CrossRef]
- Sorato, E.; Menazza, S.; Zulian, A.; Sabatelli, P.; Gualandi, F.; Merlini, L.; Bonaldo, P.; Canton, M.; Bernardi, P.; Di Lisa, F. Monoamine oxidase inhibition prevents mitochondrial dysfunction and apoptosis in myoblasts from patients with collagen VI myopathies. Free Radic. Biol. Med. 2014, 75, 40–47. [Google Scholar] [CrossRef]
- Horhat, F.G.; Rogobete, A.F.; Papurica, M.; Sandesc, D.; Tanasescu, S.; Dumitrascu, V.; Licker, M.; Nitu, R.; Cradigati, C.A.; Sarandan, M.; et al. The Use of Lipid Peroxidation Expression as a Biomarker for the Molecular Damage in the Critically Ill Polytrauma Patient. Clin. Lab. 2016, 1–7. [Google Scholar] [CrossRef]
- Moise, A.; Balescu-Arion, C. The Vitamin D and the Immune System. When? Why? How? CEACR 2020, 2, 1–9. [Google Scholar] [CrossRef]
- Georgescu, D.; Reisz, D.; Petre, I.; Ionita, I. Ischemic Stroke Secondary to Cerebral Venous Thrombosis: A Case Report. CEACR 2019, 1–7. [Google Scholar] [CrossRef]
- Timar, C.; Negrău, M.; Pantiș, C.; Daina, C.; Stanciu, S.-D.; Hodoșan, V.; Cotrău, P. Septic Shock with Chlamydia Pneumoniae Secondary to Prostatic Abscess: A Rare Case Report. CEACR 2019, 1, 1. [Google Scholar] [CrossRef]
- Papurica, M.; Rogobete, A.F.; Sandesc, D.; Dumache, R.; Cradigati, C.A.; Sarandan, M.; Nartita, R.; Popovici, S.E.; Bedreag, O.H. Advances in biomarkers in critical ill polytrauma patients. Clin. Lab. 2016, 62, 977–986. [Google Scholar] [CrossRef]
- Ferrari, R.S.; Andrade, C.F. Oxidative Stress and Lung Ischemia-Reperfusion Injury. Oxidative Med. Cell. Longev. 2015, 2015, 14. [Google Scholar] [CrossRef] [PubMed]
- da Costa Paes, E.R.; Braz, M.G.; de Lima, J.T.; Gomes da Silva, M.R.; Bentes de Sousa, L.; Lima, E.S.; Carvalho de Vasconcellos, M.; Cerqueira Braz, J.R. DNA damage and antioxidant status in medical residents occupationally exposed to waste anesthetic gases. Acta Cir. Bras. 2014, 29, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Gan, T.J.; Diemunsch, P.; Habib, A.S.; Kovac, A.; Kranke, P.; Meyer, T.A.; Watcha, M.; Chung, F.; Angus, S.; Apfel, C.C.; et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth. Analg. 2014, 118, 85–113. [Google Scholar] [CrossRef]
- Song, D.; Hamza, M.; White, P.F.; Klein, K.; Recart, A.; Khodaparast, O. The pharmacodynamic effects of a lower-lipid emulsion of propofol: A comparison with the standard propofol emulsion. Anesth. Analg. 2004, 98, 687–691, table of contents. [Google Scholar] [CrossRef]
- El Hor, T.; Van Der Linden, P.; De Hert, S.; Melot, C.; Bidgoli, J. Impact of entropy monitoring on volatile anesthetic uptake. Anesthesiology 2013, 118, 868–873. [Google Scholar] [CrossRef]
- Tewari, S.; Bhadoria, P.; Wadhawan, S.; Prasad, S.; Kohli, A. Entropy vs standard clinical monitoring using total intravenous anesthesia during transvaginal oocyte retrieval in patients for in vitro fertilization. J. Clin. Anesth. 2016, 34, 105–112. [Google Scholar] [CrossRef]
- Refaat, E.K.; Yassein, T.E. Reduced sevoflurane consumption in cirrhotic compared to non-cirrhotic patients undergoing major hepatic surgery: During entropy monitored general anesthesia. Egypt. J. Anaesth. 2013, 29, 61–65. [Google Scholar] [CrossRef][Green Version]
| Author | Parameter/Monitoring Technique | Type of General Anesthesia | Observations | Reference |
|---|---|---|---|---|
| Kim et al. | State Entropy (SE) | 78 children (age: 3–12) Sevoflurane | ↓ sevoflurane consumption ↓ postoperative recovery time | [44] |
| Wu et al. | State Entropy (SE) | 64 patients Sevoflurane | ↓ sevoflurane consumption ↓ consumption of antihypertensive drugs ↑ hemodynamic stability | [45] |
| Vakkuri et al. | State Entropy (SE) | 368 patients propofol-alfentanil-N2O | ↓ propofol consumption ↓ postoperative recovery time | [46] |
| Talawar et al. | Entropy (SE/RE) | 50 patients isofluran-N2O | ↓ postoperative recovery time | [47] |
| Elgebaly et al. | Entropy (SE/RE) | propofol | ↓ propofol consumption ↑ hemodynamic stability | [48] |
| Gan et al. | Bispectral index (BIS) | 302 patients propofol-alfentanil-N2O | ↓ propofol consumption ↓ postoperative recovery time | |
| Liu et al. | Bispectral index (BIS) | 1383 patients Day surgery | ↓ consumption of anesthetic drugs ↓ incidence of adverse effects (nausea, vomiting) ↓ postoperative recovery time | |
| Bhardwaj et al. | Bispectral index (BIS) | 50 pediatric pts propofol | No effects have been observed regarding the consumption of anesthetic drugs No effects on the postoperative recovery time | [49] |
| Aime et al. | Bispectral index (BIS) and Entropy (RE/SE) | 115 patients Sevoflurane; | BIS & Entropy: ↓ sevoflurane consumption | [50] |
| Liao et al. | Bispectral index (BIS) and A-line autoregressive index (AAI) | 116 patients Sevoflurane; | BIS & AAI: ↓ sevoflurane consumption ↓ postoperative recovery time; | [51] |
| Weber et al. | Composite auditory evoked potential index (cAAI) | 20 pediatric patients TIVA propofol and remifentanil; | ↓ propofol consumption ↑ hemodynamic stability | [52] |
| Lai et al. | Narcotrend | 40 patients propofol and fentanyl; | ↓ propofol consumption ↓ postoperative recovery time No effects on PONV | [53] |
| Rundshagen et al. | Narcotrend | 48 patients propofol and remifentanil | No effects on propofol/remifentanil consumption No effects on postoperative recovery time | [54] |
| Author | Technique/Parameter | Type of Anesthesia Type of Intervention | Obervations | Reference |
|---|---|---|---|---|
| Funcke et al. | SPI & Pupillary Pain Index (PPI) & Nociception Level (NOL) | 48 patients radical retropubic prostatectomy | SPI: ↓ hormonal response to stress PPI: ↓ sufentanil consumption, ↑ hormonal response to stress No effect on postoperative recovery time | [69] |
| Bergmann et al. | Surgical Pleth Index (SPI) | 170 patients orthopedic surgery | ↓ propofol consumption ↓ remifentanil consumption ↓ postoperative recovery time | [10] |
| Jain et al. | Surgical Pleth Index (SPI) | 140 patients Laparoscopic cholecystectomy; | ↓ PONV ↓ postoperative pain ↑ fentanyl consumption No impact on hemodynamic stability | [70] |
| Won et al. | Surgical Pleth Index (SPI) | 45 patient; Elective thyroidectomy | ↓ oxycodone consumption ↓ postoperative recovery time ↓ extubation time | [71] |
| Chen et al. | Surgical Stress Index (SSI)–former Surgical Pleth Index (SPI) | 80 patients Elective surgical interventions | ↓ remifentanil consumption ↓ postoperative adverse effects ↑ hemodynamic stability | [72] |
| Theerth et al. | Analgesia Nociception Index (ANI) | 60 patients Oncological surgery | ↓ fentanyl consumption No impact on postoperative pain | [73] |
| Soral et al. | Analgesia Nociception Index (ANI) | 102 patients Procedural sedation | ↓ opioid consumption No impact of propofol and ketamine consumption | [74] |
| Gall et al. | Analgesia Nociception Index (ANI) | 60 patients Bariatric surgery | ↓ sufentanyl consumption No impact on PONV and postoperative pain | [75] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rogobete, A.F.; Bedreag, O.H.; Papurica, M.; Popovici, S.E.; Bratu, L.M.; Rata, A.; Barsac, C.R.; Maghiar, A.; Garofil, D.N.; Negrea, M.; et al. Multiparametric Monitoring of Hypnosis and Nociception-Antinociception Balance during General Anesthesia—A New Era in Patient Safety Standards and Healthcare Management. Medicina 2021, 57, 132. https://doi.org/10.3390/medicina57020132
Rogobete AF, Bedreag OH, Papurica M, Popovici SE, Bratu LM, Rata A, Barsac CR, Maghiar A, Garofil DN, Negrea M, et al. Multiparametric Monitoring of Hypnosis and Nociception-Antinociception Balance during General Anesthesia—A New Era in Patient Safety Standards and Healthcare Management. Medicina. 2021; 57(2):132. https://doi.org/10.3390/medicina57020132
Chicago/Turabian StyleRogobete, Alexandru Florin, Ovidiu Horea Bedreag, Marius Papurica, Sonia Elena Popovici, Lavinia Melania Bratu, Andreea Rata, Claudiu Rafael Barsac, Andra Maghiar, Dragos Nicolae Garofil, Mihai Negrea, and et al. 2021. "Multiparametric Monitoring of Hypnosis and Nociception-Antinociception Balance during General Anesthesia—A New Era in Patient Safety Standards and Healthcare Management" Medicina 57, no. 2: 132. https://doi.org/10.3390/medicina57020132
APA StyleRogobete, A. F., Bedreag, O. H., Papurica, M., Popovici, S. E., Bratu, L. M., Rata, A., Barsac, C. R., Maghiar, A., Garofil, D. N., Negrea, M., Petcu, L. B., Toma, D., Dumbuleu, C. M., Rimawi, S., & Sandesc, D. (2021). Multiparametric Monitoring of Hypnosis and Nociception-Antinociception Balance during General Anesthesia—A New Era in Patient Safety Standards and Healthcare Management. Medicina, 57(2), 132. https://doi.org/10.3390/medicina57020132








