Meta-Analysis of Prevalence of Depression in Dental Students during COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
2.3. Methodological Quality Assessment
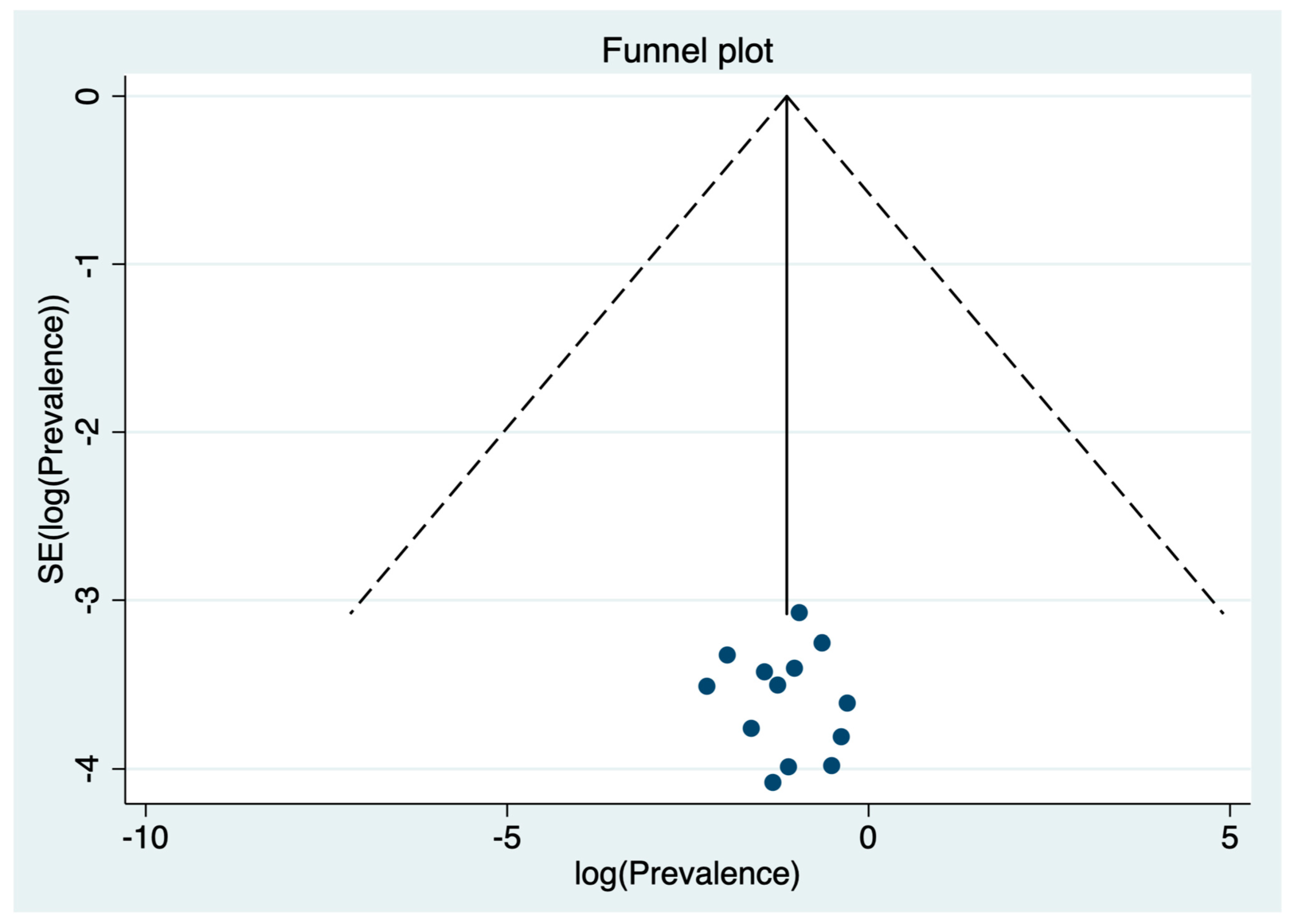
2.4. Data Extraction and Statistical Analysis
3. Results
4. Discussion
4.1. Summary of Main Findings
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mahase, E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ 2020, 368, m1036. [Google Scholar] [CrossRef] [PubMed]
- WHO. Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 1 September 2021).
- Nelson, B.W.; Pettitt, A.; Flannery, J.E.; Allen, N.B. Rapid assessment of psychological and epidemiological correlates of COVID-19 concern, financial strain, and health-related behavior change in a large online sample. PLoS ONE 2020, 15, e0241990. [Google Scholar] [CrossRef] [PubMed]
- Khan, K.S.; Mamun, M.A.; Griffiths, M.D.; Ullah, I. The Mental Health Impact of the COVID-19 Pandemic Across Different Cohorts. Int. J. Ment. Health Addict. 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Batra, K.; Sharma, M.; Batra, R.; Singh, T.; Schvaneveldt, N. Assessing the Psychological Impact of COVID-19 among College Students: An Evidence of 15 Countries. Healthcare 2021, 9, 222. [Google Scholar] [CrossRef]
- Viner, R.M.; Russell, S.J.; Croker, H.; Packer, J.; Ward, J.; Stansfield, C.; Mytton, O.; Bonell, C.; Booy, R. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet 2020, 4, 397–404. [Google Scholar] [CrossRef]
- Al Lily, A.E.; Ismail, A.F.; Abunasser, F.M.; Alqahtani, R.H.A. Distance education as a response to pandemics: Coronavirus and Arab culture. Technol. Soc. 2020, 63, 101317. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef] [PubMed]
- Idoiaga Mondragon, N.; Berasategi Sancho, N.; Eiguren Munitis, A.; Dosil Santamaria, M. Exploring the social and emotional representations used by students from the University of the Basque Country to face the first outbreak of COVID-19 pandemic. Health Educ. Res. 2021, 36, 159–169. [Google Scholar] [CrossRef]
- Sahu, P. Closure of Universities Due to Coronavirus Disease 2019 (COVID-19): Impact on Education and Mental Health of Students and Academic Staff. Cureus 2020, 12, e7541. [Google Scholar] [CrossRef]
- Zhai, Y.; Du, X. Mental health care for international Chinese students affected by the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e22. [Google Scholar] [CrossRef]
- Arango, C. Lessons Learned From the Coronavirus Health Crisis in Madrid, Spain: How COVID-19 Has Changed Our Lives in the Last 2 Weeks. Biol. Psychiatry 2020, 88, e33–e34. [Google Scholar] [CrossRef]
- Chang, J.; Yuan, Y.; Wang, D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao 2020, 40, 171–176. [Google Scholar] [PubMed]
- Kaparounaki, C.K.; Patsali, M.E.; Mousa, D.-P.V.; Papadopoulou, E.V.; Papadopoulou, K.K.; Fountoulakis, K.N. University students’ mental health amidst the COVID-19 quarantine in Greece. Psychiatry Res. 2020, 290, 113111. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin. Neurosci. 2020, 74, 281–282. [Google Scholar] [CrossRef]
- Galan, F.; Ríos-Santos, J.; Polo, J.; Ríos-Carrasco, B.; Bullon, P. Burnout, depression and suicidal ideation in dental students. Med. Oral Patol. Oral Cir. Bucal 2014, 19, e206–e211. [Google Scholar] [CrossRef]
- Stormon, N.; Ford, P.J.; Kisely, S.; Bartle, E.; Eley, D.S. Depression, anxiety and stress in a cohort of Australian dentistry students. Eur. J. Dent. Educ. 2019, 23, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Bs, A.R.L.; Bs, K.K.Y.; Taylor, G.W.; Saeed, S.G. High depressive symptom prevalence in dental students associated with lifestyle and well-being characteristics. J. Dent. Educ. 2020, 84, 771–780. [Google Scholar] [CrossRef]
- Puthran, R.; Zhang, M.W.B.; Tam, W.; Ho, R. Prevalence of depression amongst medical students: A meta-analysis. Med. Educ. 2016, 50, 456–468. [Google Scholar] [CrossRef]
- Alzahem, A.; Van Der Molen, H.T.; Alaujan, A.H.; Schmidt, H.G.; Zamakhshary, M.H. Stress amongst dental students: A systematic review. Eur. J. Dent. Educ. 2011, 15, 8–18. [Google Scholar] [CrossRef]
- Al-Sowygh, Z.H.; Alfadley, A.; Al-Saif, M.I.; Al-Wadei, S.H. Perceived causes of stress among Saudi dental students. King Saud Univ. J. Dent. Sci. 2013, 4, 7–15. [Google Scholar] [CrossRef]
- Basudan, S.; Binanzan, N.; Alhassan, A. Depression, anxiety and stress in dental students. Int. J. Med Educ. 2017, 8, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Prinz, P.; Hertrich, K.; Hirschfelder, U.; De Zwaan, M. Burnout, depression and depersonalisation—Psychological factors and coping strategies in dental and medical students. GMS Z. Med. Ausbild. 2012, 29, 1–14. [Google Scholar] [CrossRef]
- Posse, J.L.; van Harten, M.; Phadraig, C.M.G.; Freitas, M.D.; Faulks, D.; Dougall, A.; Daly, B.; Dios, P.D. The Impact of the First Wave of the COVID-19 Pandemic on Providing Special Care Dentistry: A Survey for Dentists. Int. J. Environ. Res. Public Health 2021, 18, 2970. [Google Scholar] [CrossRef] [PubMed]
- Kateeb, E.; Danadneh, M.; Pokorná, A.; Klugarová, J.; Abdulqader, H.; Klugar, M.; Riad, A. Predictors of Willingness to Receive COVID-19 Vaccine: Cross-Sectional Study of Palestinian Dental Students. Vaccines 2021, 9, 954. [Google Scholar] [CrossRef]
- García, D.; Akinkugbe, A.; Mosavel, M.; Smith, C.; Brickhouse, T. COVID-19 and Dental and Dental Hygiene Students’ Career Plans. JDR Clin. Transl. Res. 2021, 6, 153–160. [Google Scholar] [CrossRef]
- Özdin, S.; Bayrak, Ö.Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Choo, F.N.; Tran, B.; Ho, R.; Sharma, V.K.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Cénat, J.M.; Blais-Rochette, C.; Kokou-Kpolou, C.K.; Noorishad, P.-G.; Mukunzi, J.N.; McIntee, S.-E.; Dalexis, R.D.; Goulet, M.-A.; Labelle, P.R. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2020, 295, 113599. [Google Scholar] [CrossRef]
- Prati, G.; Mancini, A.D. The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021, 51, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Ochnik, D.; Rogowska, A.; Kuśnierz, C.; Jakubiak, M.; Schütz, A.; Held, M.; Arzenšek, A.; Benatov, J.; Berger, R.; Korchagina, E.; et al. A Comparison of Depression and Anxiety among University Students in Nine Countries during the COVID-19 Pandemic. J. Clin. Med. 2021, 10, 2882. [Google Scholar] [CrossRef]
- Lasheras, I.; Gracia-García, P.; Lipnicki, D.M.; Bueno-Notivol, J.; López-Antón, R.; De La Cámara, C.; Lobo, A.; Santabárbara, J. Prevalence of Anxiety in Medical Students during the COVID-19 Pandemic: A Rapid Systematic Review with Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 6603. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetc, R. Systematic reviews of etiology and risk. In Joanna Briggs Institute Reviewer’s Manual; Aromataris, E., Munn, Z., Eds.; The Joanna Briggs Institute: Adelaide, Australia, 2017; Chapter 7; pp. 219–226. [Google Scholar]
- Freeman, M.F.; Tukey, J.W. Transformations Related to the Angular and the Square Root. Ann. Math. Stat. 1950, 21, 607–611. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Von Hippel, P.T. The heterogeneity statistic I 2 can be biased in small meta-analyses. BMC Med Res. Methodol. 2015, 15, 1–8. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Thompson, S.G.; Higgins, J.P.T. How should meta-regression analyses be undertaken and interpreted? Stat. Med. 2002, 21, 1559–1573. [Google Scholar] [CrossRef]
- Egger, M.; Schneider, M.; Smith, G.D. Meta-analysis Spurious precision? Meta-analysis of observational studies. BMJ 1998, 316, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Hunter, J.P.; Saratzis, A.; Sutton, A.J.; Boucher, R.H.; Sayers, R.D.; Bown, M. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J. Clin. Epidemiol. 2014, 67, 897–903. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Found Stat Comput: Vienna, Austria, 2019. [Google Scholar]
- Babadi, F.; Bazmi, A.; Araban, M. Association between the Fear Induced by the COVID-19 and the Level of Depression, Anxiety, and Stress among Dental Students: A Cross-sectional Study. Health Educ. Health Promot. 2021, 9, 19–24. [Google Scholar]
- Chakraborty, T.; Subbiah, G.K.; Damade, Y. Psychological Distress during COVID-19 Lockdown among Dental Students and Practitioners in India: A Cross-Sectional Survey. Eur. J. Dent. 2020, 14, S70–S78. [Google Scholar] [CrossRef]
- Chi, D.L.; Randall, C.L.; Hill, C.M. Dental trainees’ mental health and intention to leave their programs during the COVID-19 pandemic. J. Am. Dent. Assoc. 2021, 152, 526–534. [Google Scholar] [CrossRef]
- Gaş, S.; Özsoy, H.E.; Aydın, K.C. The association between sleep quality, depression, anxiety and stress levels, and temporomandibular joint disorders among Turkish dental students during the COVID-19 pandemic. CRANIO® 2021, 1–6. [Google Scholar] [CrossRef]
- Hakami, Z.; Khanagar, S.B.; Vishwanathaiah, S.; Hakami, A.; Bokhari, A.M.; Jabali, A.H.; Alasmari, D.; Aldrees, A.M. Psychological impact of the coronavirus disease 2019 (COVID-19) pandemic on dental students: A nationwide study. J. Dent. Educ. 2021, 85, 494–503. [Google Scholar] [CrossRef]
- Keskin, G. Self-Report Measurement of Depression, Anxiety, and Stress Caused by COVID-19 Pandemic in Senior Undergraduate Dental Students. Pesqui. Bras. Odontopediatr. Clin. Integr. 2021, 21, 0243. [Google Scholar] [CrossRef]
- Khanagar, S.B.; Alfadley, A. Psychological Impact of the COVID-19 Pandemic on Dental Interns in Riyadh, Saudi Arabia: A Cross-sectional Survey. Int. J. Clin. Pediatr. Dent. 2021, 13, 508–512. [Google Scholar] [CrossRef]
- Abu Kwaik, A.; Saleh, R.; Danadneh, M.; Kateeb, E. Stress, Anxiety and Depression Among Dental Students in Times of Covid-19 Lockdown. Int. J. Dent. Oral Sci. 2021, 8, 1397–1401. [Google Scholar]
- Medeiros, R.A.; Vieira, D.L.; Silva, E.V.F.D.; Rezende, L.V.M.L.; Santos, R.W.D.; Tabata, L.F. Prevalence of symptoms of temporomandibular disorders, oral behaviors, anxiety, and depression in Dentistry students during the period of social isolation due to COVID-19. J. Appl. Oral Sci. 2020, 28, e20200445,0445. [Google Scholar] [CrossRef] [PubMed]
- Mekhemar, M.; Attia, S.; Dörfer, C.; Conrad, J. Dental Students in Germany throughout the COVID-19 Pandemic: A Psychological Assessment and Cross-Sectional Survey. Biology 2021, 10, 611. [Google Scholar] [CrossRef] [PubMed]
- Samsudin, A.D.; Jaafar, A.; Idaham, N.I.; Jali@yunos, M.H.M. The Effect of COVID-19 Pandemic on Psychological Wellness among Dental Students of a Malaysian Public University. Ulum Islamiyyah 2021, 87–97. [Google Scholar] [CrossRef]
- Shailaja, B.; Shetty, V.; Chaudhury, S.; Thyloth, M. Exploring cyberchondria and its associations in dental students amid COVID-19 infodemic. Ind. Psychiatry J. 2020, 29, 257–267. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, F.; Qian, G. Psychological impact of self-quarantine on malaysian dental students during COVID-19 pandemic. Med. J. Dr. D.Y. Patil Vidyapeeth 2021. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. Available online: https://www.sciencedirect.com/science/article/pii/S088915912030845X (accessed on 8 July 2021). [CrossRef]
- Salari, N.; Hosseinian-Far, A.; Jalali, R.; Vaisi-Raygani, A.; Rasoulpoor, S.; Mohammadi, M.; Rasoulpoor, S.; Khaledi-Paveh, B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Glob. Health 2020, 16, 57. [Google Scholar] [CrossRef]
- Wang, Z.-H.; Yang, H.-L.; Yang, Y.-Q.; Liu, D.; Li, Z.-H.; Zhang, X.-R.; Zhang, Y.-J.; Shen, D.; Chen, P.-L.; Song, W.-Q.; et al. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study. J. Affect. Disord. 2020, 275, 188–193. [Google Scholar] [CrossRef]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Drakos, A.; Zuo, Q.K.; Huang, E. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 301, 113863. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Wen, W.; Zhang, H.; Ni, J.; Jiang, J.; Cheng, Y.; Zhou, M.; Ye, L.; Feng, Z.; Ge, Z.; et al. Anxiety, depression, and stress prevalence among college students during the COVID-19 pandemic: A systematic review and meta-analysis. J. Am. Coll. Health 2021, 1–8. [Google Scholar] [CrossRef]
- Shah, S.M.A.; Mohammad, D.; Qureshi, M.F.H.; Abbas, M.Z.; Aleem, S. Prevalence, Psychological Responses and Associated Correlates of Depression, Anxiety and Stress in a Global Population, During the Coronavirus Disease (COVID-19) Pandemic. Community Ment. Health J. 2020, 57, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Uraz, A.; Tocak, Y.S.; Yozgatlıgil, C.; Cetiner, S.; Bal, B. Psychological well–being, health, and stress sources in turkish dental students. J. Dent. Educ. 2013, 77, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Ardoino, G.I.; Queirolo, E.I.; Barg, G.; Ciccariello, D.A.; Kordas, K. The Relationship Among Depression, Parenting Stress, and Partner Support in Low-Income Women From Montevideo, Uruguay. Health Care Women Int. 2013, 36, 392–408. [Google Scholar] [CrossRef]
- Seto, M.; Morimoto, K.; Maruyama, S. Effects of work-related factors and work-family conflict on depression among Japanese working women living with young children. Environ. Health Prev. Med. 2004, 9, 220–227. [Google Scholar] [CrossRef]
- Chirikov, I.; Soria, K.M.; Horgos, B.; Jones-White, D. Undergraduate and graduate students’ mental health during the COVID-19 pandemic. eScholarship 2020. [Google Scholar]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- Perry, S.; Burrow, M.F.; Leung, W.K.; Bridges, S.M. Simulation and curriculum design: A global survey in dental education. Aust. Dent. J. 2017, 62, 453–463. [Google Scholar] [CrossRef]
- Faisal, G.G.; Radeef, A.S. Stressors and Their Association with Symptoms of Depression, Anxiety and Stress in Dental Students. Makara J. Health Res. 2018, 22, 58–62. [Google Scholar] [CrossRef]
- Adolescent Mental Health. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (accessed on 2 September 2021).
- Haroon, Z.; Azad, A.A.; Sharif, M.; Aslam, A.; Arshad, K.; Rafiq, S. COVID-19 Era: Challenges and Solutions in Dental Education. J. Coll. Physicians Surg. Pak. 2020, 30, 129–131. [Google Scholar] [CrossRef]


| (COVID [tiab] OR COVID-19[tiab] OR coronavirus[tiab] OR SARS-CoV-2[tiab] OR “Coronavirus”[Mesh] OR “severe acute respiratory syndrome coronavirus 2”[Supplementary Concept] OR “COVID-19”[Supplementary Concept] OR “Coronavirus Infections/epidemiology”[Mesh] OR “Coronavirus Infections/prevention and control”[Mesh] OR “Coronavirus Infections/psychology”[Mesh] OR “Coronavirus Infections/statistics and numerical data”[Mesh]) AND (“Depression”[Mesh] OR “Depressive Disorder”[Mesh] OR “depression”[tiab] OR “depressive”[tiab] OR “Depression/statistics and numerical data”[Mesh]) AND (“Students, Dental”[Mesh] OR “dental students”[tiab] OR “dentistry students”[tiab] OR “dental undergraduates”[tiab] OR “dentistry undergraduates”[tiab] OR “university students” [tiab]) |
| Author (Publication Year) | Country | Mean Age (SD) | % Females (n) | Sample Size (n) | Response Rate (%) | Sampling Method | Depression Assessment | Diagnostic Criteria | Prevalence | Quality Assessment * | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| % | n | ||||||||||
| Babadi et al. (2021) [47] | Iran | 22.9 (3.3) | 53.28% (122) | 229 | 54.5% | Convenience sampling | DASS-21 | ≥10 | 28.8% | 66 | 7 |
| Chakraborty et al. (2020) [48] | India | 24 (3) | 81.55% (137) | 168 | NR | Convenience sampling | PHQ-9 | ≥10 | 53.5% | 90 | 6 |
| Chi el al. (2021) [49] | USA | NR | 52.58% (51) | 97 | 35.5% | Convenience sampling | PHQ-9 | ≥10 | 14.4% | 14 | 6 |
| Gaș et al. (2021) [50] | Turkey | 21.31 (1.9) | 64.66% (452) | 699 | 95.1% | Random sampling | DASS-21 | ≥10 | 27.2% | 190 | 9 |
| Hakami et al. (2021) [51] | Saudi Arabia | 21.76 (1.9) | 54.82% (381) | 695 | NR | Cluster sampling | DASS-21 | ≥10 | 60.7% | 422 | 8 |
| Keskin et al. (2021) [52] | Turkey | NR | 60.23% (156) | 259 | NR | Convenience sampling | DASS-42 | ≥10 | 75.3% | 195 | 5 |
| Khanagar & Alfadley (2020) [53] | Saudi Arabia | 25.1 (NR) | 64.55% (71) | 110 | 68.7% | Convenience sampling | DASS-21 | ≥10 | 10.9% | 12 | 7 |
| Kwaik et al. (2021) [54] | Palestine | NR | 81.19% (354) | 436 | 55.18% | NR | DASS-21 | ≥10 | 69.9% | 305 | 8 |
| Medeiros et al. (2020) [55] | Brazil | 21.46 (2.37) | 76.99% (87) | 113 | 51.36% | NR | HADS | ≥8 | 38.9% | 44 | 6 |
| Mekhemar et al. (2021) [56] | Germany | NR | 73.46% (155) | 211 | NR | Convenience sampling | DASS-21 | ≥6 | 26.5% | 77 | 5 |
| Samsudin et al. (2021) [57] | Malaysia | NR | 79.43% (139) | 175 | 94.6% | Convenience sampling | DASS-21 | ≥10 | 24% | 42 | 6 |
| Shailaja et al. (2021) [58] | India | 22.63 (2.88) | 82.00% (246) | 300 | NR | NR | DASS-21 | ≥10 | 20% | 60 | 7 |
| Siddiqui & Qian (2021) [59] | Malaysia | 22.45 (NR) | 79.24% (519) | 655 | 20% | Convenience sampling | DASS-21 | ≥10 | 33.6% | 220 | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santabárbara, J.; Ozamiz-Etxebarria, N.; Idoiaga, N.; Olaya, B.; Bueno-Novitol, J. Meta-Analysis of Prevalence of Depression in Dental Students during COVID-19 Pandemic. Medicina 2021, 57, 1278. https://doi.org/10.3390/medicina57111278
Santabárbara J, Ozamiz-Etxebarria N, Idoiaga N, Olaya B, Bueno-Novitol J. Meta-Analysis of Prevalence of Depression in Dental Students during COVID-19 Pandemic. Medicina. 2021; 57(11):1278. https://doi.org/10.3390/medicina57111278
Chicago/Turabian StyleSantabárbara, Javier, Naiara Ozamiz-Etxebarria, Nahia Idoiaga, Beatriz Olaya, and Juan Bueno-Novitol. 2021. "Meta-Analysis of Prevalence of Depression in Dental Students during COVID-19 Pandemic" Medicina 57, no. 11: 1278. https://doi.org/10.3390/medicina57111278
APA StyleSantabárbara, J., Ozamiz-Etxebarria, N., Idoiaga, N., Olaya, B., & Bueno-Novitol, J. (2021). Meta-Analysis of Prevalence of Depression in Dental Students during COVID-19 Pandemic. Medicina, 57(11), 1278. https://doi.org/10.3390/medicina57111278









