Clinical Outcomes of Chemotherapeutic Molecules as Single and Multiple Agents in Advanced Non-Small-Cell Lung Carcinoma (NSCLC) Patients
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Monotherapy vs. Cisplatin/Carboplatin-Based Combination Chemotherapy
3.2. Comparison between Dual-Agent Chemotherapy
3.3. Doublet Chemotherapy vs. Triplet Chemotherapy
3.4. PD-1/PD-L1 Inhibitors Regimen vs. Chemotherapy-Only Regimen
3.5. EGFR TKI Regimens vs. Chemotherapy-Only Regimen
3.6. ALK TKI Regimens vs. Chemotherapy-Only Regimen
3.7. Treatment for Positive ROS1, BRAF and HER2 Mutations
4. Discussion
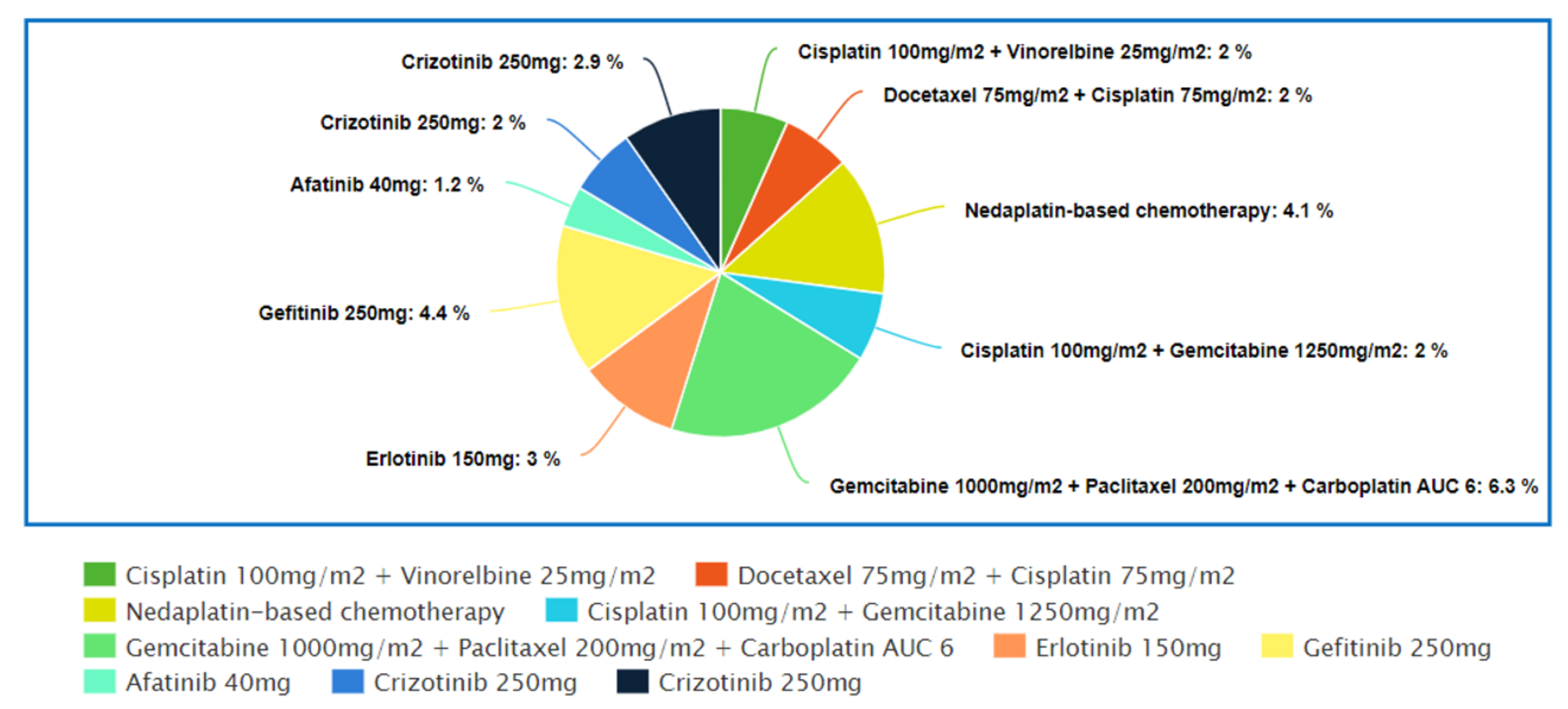
4.1. Top 10 Regimens with the Best “Complete Response” Rate
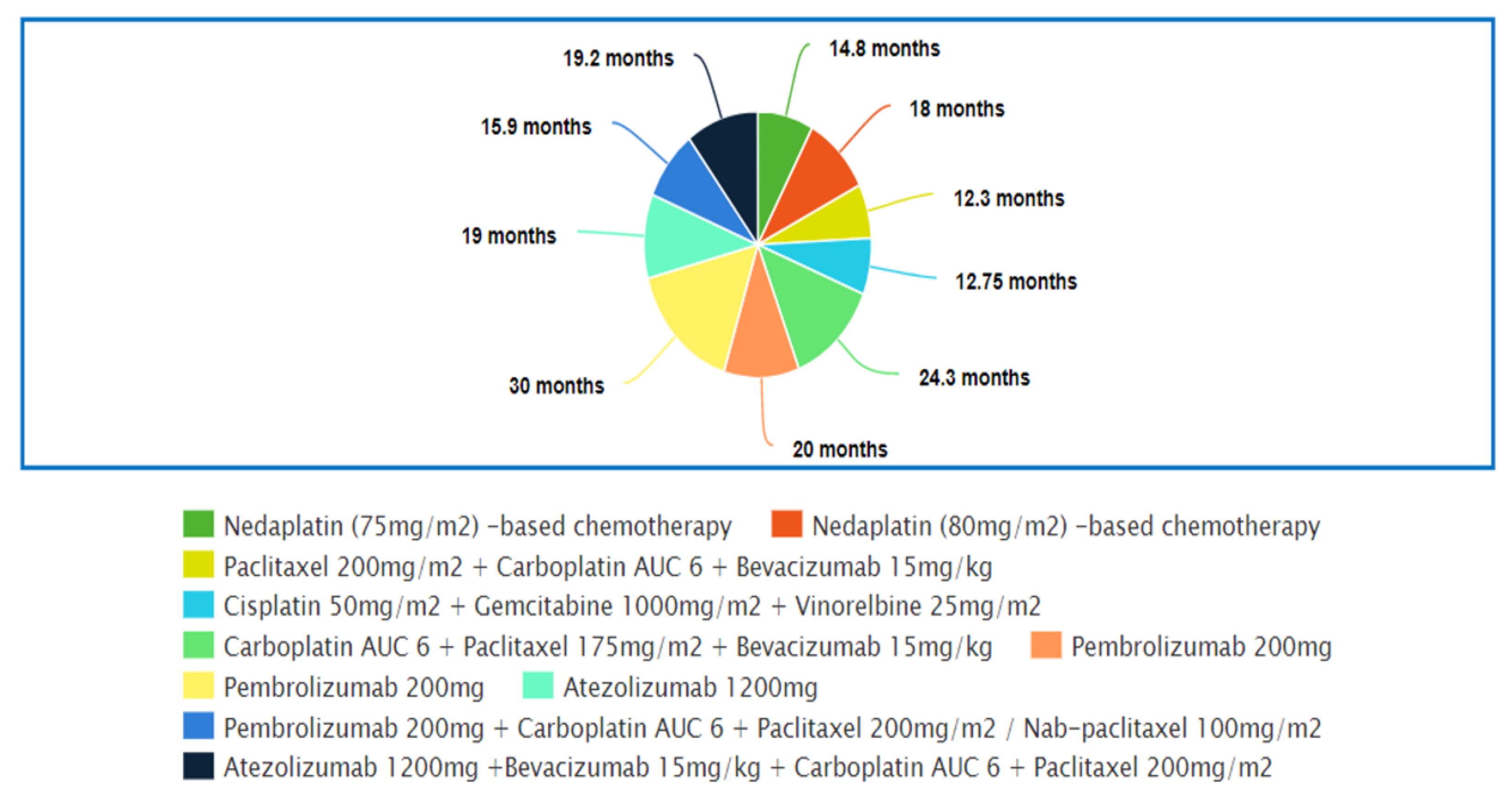
4.2. Top 10 Regimens with the Best Overall Survival
5. Limitation
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Fintelmann, F.J.; Bernheim, A.; Digumarthy, S.R.; Lennes, I.T.; Kalra, M.K.; Gilman, M.D.; Sharma, A.; Flores, E.; Muse, V.V.; Shepard, J.-A.O. The 10 Pillars of Lung Cancer Screening: Rationale and Logistics of a Lung Cancer Screening Program. Radiographics 2015, 35, 1893–1908. [Google Scholar] [CrossRef] [PubMed]
- Ries, L.A.; Harkins, D.; Krapcho, M.; Mariotto, A.; Miller, B.A.; Feuer, E.J.; Clegg, L.X.; Eisner, M.P.; Horner, M.J.; Howlader, N.; et al. SEER Cancer Statistics Review 1975–2017; National Cancer Institute: Bethesda, MD, USA, 2020. [Google Scholar]
- Molina, J.R.; Yang, P.; Cassivi, S.D.; Schild, S.E.; Adjei, A.A. Non-small cell lung cancer: Epidemiology, risk factors, treatment, and survivorship. Mayo Clin. Proc. 2008, 83, 584–594. [Google Scholar] [CrossRef]
- World Health Organization Classification of Tumours. In Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart; IARC Press: Lyon, France, 2004; 341p.
- Kosmidis, P. Chemotherapy in NSCLC: Historical review. Lung Cancer 2002, 38, 19–22. [Google Scholar] [CrossRef]
- Zhong, C.; Liu, H.; Jiang, L.; Zhang, W.; Yao, F. Chemotherapy Plus Best Supportive Care versus Best Supportive Care in Patients with Non-Small Cell Lung Cancer: A Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2013, 8, e58466. [Google Scholar] [CrossRef] [PubMed]
- Group NM-AC. Chemotherapy in addition to supportive care improves survival in advanced non-small-cell lung cancer: A systematic review and meta-analysis of individual patient data from 16 randomized controlled trials. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2008, 26, 4617–4625. [Google Scholar] [CrossRef] [PubMed]
- Spiro, S.G.; Rudd, R.M.; Souhami, R.L.; Brown, J.; Fairlamb, D.J.; Gower, N.H.; Maslove, L.; Milroy, R.; Napp, V.; Parmar, M.K.B.; et al. Chemotherapy versus supportive care in advanced non-small cell lung cancer: Improved survival without detriment to quality of life. Thorax 2004, 59, 828–836. [Google Scholar] [CrossRef]
- Chemotherapy in non-small cell lung cancer: A meta-analysis using updated data on individual patients from 52 randomised clinical trials. Non-small Cell Lung Cancer Collaborative Group. BMJ 1995, 311, 899–909.
- Baxevanos, P.; Mountzios, G. Novel chemotherapy regimens for advanced lung cancer: Have we reached a plateau? Ann. Transl. Med. 2018, 6, 139. [Google Scholar] [CrossRef]
- Davies, M. New modalities of cancer treatment for NSCLC: Focus on immunotherapy. Cancer Manag. Res. 2014, 6, 63–75. [Google Scholar] [CrossRef][Green Version]
- Rébé, C.; Demontoux, L.; Pilot, T.; Ghiringhelli, F. Platinum Derivatives Effects on Anticancer Immune Response. Biomolecules 2019, 10, 13. [Google Scholar] [CrossRef]
- Hato, S.V.; Khong, A.; de Vries, J.; Lesterhuis, W.J. Molecular Pathways: The Immunogenic Effects of Platinum-Based Chemotherapeutics. Clin. Cancer Res. 2014, 20, 2831–2837. [Google Scholar] [CrossRef] [PubMed]
- Plunkett, W.; Huang, P.; Xu, Y.-Z.; Heinemann, V.; Grunewald, R.; Gandhi, V. Gemcitabine: Metabolism, mechanisms of action, and self-potentiation. Semin Oncol. 1995, 4, 3–10. [Google Scholar]
- Herbst, R.S.; Khuri, F.R. Mode of action of docetaxel—A basis for combination with novel anticancer agents. Cancer Treat. Rev. 2003, 29, 407–415. [Google Scholar] [CrossRef]
- Horwitz, S.B. Taxol (paclitaxel): Mechanisms of action. Ann. Oncol. 1994, 5 (Suppl. 6), S3–S6. [Google Scholar]
- Levêque, D.; Jehl, F. Clinical Pharmacokinetics of Vinorelbine. Clin. Pharmacokinet. 1996, 31, 184–197. [Google Scholar] [CrossRef]
- Adjei, A.A. Pharmacology and Mechanism of Action of Pemetrexed. Clin. Lung Cancer 2004, 5, S51–S55. [Google Scholar] [CrossRef]
- Kazazi-Hyseni, F.; Beijnen, J.H.; Schellens, J.H.M. Bevacizumab. Oncologist 2010, 15, 819–825. [Google Scholar] [CrossRef] [PubMed]
- Philips, G.K.; Atkins, M.B. Therapeutic uses of anti-PD-1 and anti-PD-L1 antibodies. Int. Immunol. 2014, 27, 39–46. [Google Scholar] [CrossRef]
- Rawluk, J.; Waller, C.F. Gefitinib. In Small Molecules in Oncology; Martens, U.M., Ed.; Springer International Publishing: Cham, Switzerland, 2018; pp. 235–246. [Google Scholar]
- Schettino, C.; Bareschino, M.A.; Ricci, V.; Ciardiello, F. Erlotinib: An EGF receptor tyrosine kinase inhibitor in non-small-cell lung cancer treatment. Expert Rev. Respir. Med. 2008, 2, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Malapelle, U.; Ricciuti, B.; Baglivo, S.; Pepe, F.; Pisapia, P.; Anastasi, P.; Tazza, M.; Sidoni, A.; Liberati, A.M.; Bellezza, G.; et al. Osimertinib. In Small Molecules in Oncology; Martens, U.M., Ed.; Springer International Publishing: Cham, Switzerland, 2018; pp. 257–276. [Google Scholar]
- Heigener, D.F.; Reck, M. Crizotinib. In Small Molecules in Oncology; Martens, U.M., Ed.; Springer: Berlin/Heidelberg, Germany, 2014; pp. 197–205. [Google Scholar]
- Wozniak, A.J.; Crowley, J.J.; Balcerzak, S.P.; Weiss, G.R.; Spiridonidis, C.H.; Baker, L.H.; Albain, K.S.; Kelly, K.; A Taylor, S.; Gandara, D.R.; et al. Randomized trial comparing cisplatin with cisplatin plus vinorelbine in the treatment of advanced non-small-cell lung cancer: A Southwest Oncology Group study. J. Clin. Oncol. 1998, 16, 2459–2465. [Google Scholar] [CrossRef]
- Le Chevalier, T.; Brisgand, D.; Douillard, J.Y.; Pujol, J.L.; Alberola, V.; Monnier, A.; Riviere, A.; Lianes, P.; Chomy, P.; Cigolari, S. Randomized study of vinorelbine and cisplatin versus vindesine and cisplatin versus vinorelbine alone in advanced non-small-cell lung cancer: Results of a European multicenter trial including 612 patients. J. Clin. Oncol. 1994, 12, 360–367. [Google Scholar] [CrossRef] [PubMed]
- Sandler, A.; Nemunaitis, J.; Denham, C.; Von Pawel, J.; Cormier, Y.; Gatzemeier, U.; Mattson, K.; Manegold, C.; Palmer, M.; Gregor, A.; et al. Phase III Trial of Gemcitabine Plus Cisplatin Versus Cisplatin Alone in Patients with Locally Advanced or Metastatic Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2000, 18, 122. [Google Scholar] [CrossRef] [PubMed]
- De Pierre, A.; Chastang, C.; Quoix, E.; Lebeau, B.; Blachon, F.; Paillot, N.; Lemarie, E.; Milleron, B.; Moro, D.; Clavier, J.; et al. Vinorelbine versus vinorelbine plus cisplatin in advanced non-small cell lung cancer: A randomized trial. Ann. Oncol. 1994, 5, 37–42. [Google Scholar] [CrossRef]
- Zukin, M.; Barrios, C.H.; Pereira, J.R.; Ribeiro, R.D.A.; de Mendonça Beato, C.A.; Nascimento, Y.N.D.; Murad, A.; Franke, F.A.; Precivale, M.; de Lima Araujo, L.H.; et al. Randomized Phase III Trial of Single-Agent Pemetrexed Versus Carboplatin and Pemetrexed in Patients with Advanced Non–Small-Cell Lung Cancer and Eastern Cooperative Oncology Group Performance Status of 2. J. Clin. Oncol. 2013, 31, 2849–2853. [Google Scholar] [CrossRef] [PubMed]
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]
- Shukuya, T.; Yamanaka, T.; Seto, T.; Daga, H.; Goto, K.; Saka, H.; Sugawara, S.; Takahashi, T.; Yokota, S.; Kaneda, H.; et al. Nedaplatin plus docetaxel versus cisplatin plus docetaxel for advanced or relapsed squamous cell carcinoma of the lung (WJOG5208L): A randomised, open-label, phase 3 trial. Lancet Oncol. 2015, 16, 1630–1638. [Google Scholar] [CrossRef]
- Shan, J.; Xiong, Y.; Wang, D.; Xu, M.; Yang, Y.I.; Gong, K.; Yang, Z.; Wang, G.E.; Yang, X. Nedaplatin-versus cisplatin-based chemotherapy in the survival time of patients with non-small cell lung cancer. Mol. Clin. Oncol. 2015, 3, 543–549. [Google Scholar] [CrossRef][Green Version]
- Schiller, J.H.; Harrington, D.; Belani, C.; Langer, C.; Sandler, A.; Krook, J.; Zhu, J.; Johnson, D.H. Comparison of Four Chemotherapy Regimens for Advanced Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2002, 346, 92–98. [Google Scholar] [CrossRef]
- Scagliotti, G.; Parikh, P.; Von Pawel, J.; Biesma, B.; Vansteenkiste, J.; Manegold, C.; Serwatowski, P.; Gatzemeier, U.; Digumarti, R.; Zukin, M.; et al. Phase III Study Comparing Cisplatin Plus Gemcitabine with Cisplatin Plus Pemetrexed in Chemotherapy-Naive Patients with Advanced-Stage Non–Small-Cell Lung Cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. 2008, 26, 3543–3551. [Google Scholar] [CrossRef]
- Grønberg, B.H.; Bremnes, R.M.; Fløtten, Ø.; Amundsen, T.; Brunsvig, P.F.; Hjelde, H.H.; Kaasa, S.; von Plessen, C.; Stornes, F.; Tollåli, T.; et al. Phase III Study by the Norwegian Lung Cancer Study Group: Pemetrexed Plus Carboplatin Compared with Gemcitabine Plus Carboplatin As First-Line Chemotherapy in Advanced Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2009, 27, 3217–3224. [Google Scholar] [CrossRef]
- Rodrigues-Pereira, J.; Kim, J.-H.; Magallanes, M.; Lee, D.H.; Wang, J.; Ganju, V.; Martínez-Barrera, L.; Barraclough, H.; van Kooten, M.; Orlando, M. A Randomized Phase 3 Trial Comparing Pemetrexed/Carboplatin and Docetaxel/Carboplatin as First-Line Treatment for Advanced, Nonsquamous Non-small Cell Lung Cancer. J. Thorac. Oncol. 2011, 6, 1907–1914. [Google Scholar] [CrossRef]
- Zatloukal, P.; Petruželka, L.; Zemanová, M.; Kolek, V.; Skřičková, J.; Pešek, M.; Fojtů, H.; Grygárková, I.; Sixtová, D.; Roubec, J.; et al. Gemcitabine plus cisplatin vs. gemcitabine plus carboplatin in stage IIIb and IV non-small cell lung cancer: A phase III randomized trial. Lung Cancer 2003, 41, 321–331. [Google Scholar] [CrossRef]
- Ohe, Y.; Ohashi, Y.; Kubota, K.; Tamura, T.; Nakagawa, K.; Negoro, S.; Nishiwaki, Y.; Saijo, N.; Ariyoshi, Y.; Fukuoka, M. Randomized phase III study of cisplatin plus irinotecan versus carboplatin plus paclitaxel, cisplatin plus gemcitabine, and cisplatin plus vinorelbine for advanced non-small-cell lung cancer: Four-Arm Cooperative Study in Japan. Ann. Oncol. 2007, 18, 317–323. [Google Scholar] [CrossRef]
- Kelly, K.; Crowley, J.; Bunn Jr, P.A.; Presant, C.A.; Grevstad, P.K.; Moinpour, C.M.; Ramsey, S.D.; Wozniak, A.J.; Weiss, G.R.; Moore, D.F.; et al. Randomized phase III trial of paclitaxel plus carboplatin versus vinorelbine plus cisplatin in the treatment of patients with advanced non–small-cell lung cancer: A Southwest Oncology Group trial. J. Clin. Oncol. 2001, 19, 3210–3218. [Google Scholar] [CrossRef]
- Scagliotti, G.; De Marinis, F.; Rinaldi, M.; Crinò, L.; Gridelli, C.; Ricci, S.; Matano, E.; Boni, C.; Marangolo, M.; Failla, G.; et al. Phase III Randomized Trial Comparing Three Platinum-Based Doublets in Advanced Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2002, 20, 4285–4291. [Google Scholar] [CrossRef] [PubMed]
- Fossella, F.; Pereira, J.R.; Von Pawel, J.; Pluzanska, A.; Gorbounova, V.; Kaukel, E.; Mattson, K.V.; Ramlau, R.; Szczęsna, A.; Fidias, P.; et al. Randomized, Multinational, Phase III Study of Docetaxel Plus Platinum Combinations Versus Vinorelbine Plus Cisplatin for Advanced Non–Small-Cell Lung Cancer: The TAX 326 Study Group. J. Clin. Oncol. 2003, 21, 3016–3024. [Google Scholar] [CrossRef]
- Li, C.-H.; Liu, M.-Y.; Liu, W.; Li, D.-D.; Cai, L. Randomized control study of nedaplatin or cisplatin concomitant with other chemotherapy in the treatment of advanced non-small cell lung cancer. Asian Pac. J. Cancer Prev. 2014, 15, 731–736. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rosell, R.; Gatzemeier, U.; Betticher, D.C.; Keppler, U.; Macha, H.N.; Pirker, R.; Berthet, P.; Breau, J.L.; Lianes, P.; Nicholson, M.; et al. Phase III randomised trial comparing paclitaxel/carboplatin with paclitaxel/cisplatin in patients with advanced non-small-cell lung cancer: A cooperative multinational trial. Ann. Oncol. 2002, 13, 1539–1549. [Google Scholar] [CrossRef] [PubMed]
- Gridelli, C.; Gallo, C.; Shepherd, F.A.; Illiano, A.; Piantedosi, F.; Robbiati, S.F.; Manzione, L.; Barbera, S.; Frontini, L.; Veltri, E.; et al. Gemcitabine Plus Vinorelbine Compared with Cisplatin Plus Vinorelbine or Cisplatin Plus Gemcitabine for Advanced Non-Small-Cell Lung Cancer: A Phase III Trial of the Italian GEMVIN Investigators and the National Cancer Institute of Canada Clinical Trials Group. J. Clin. Oncol. 2003, 21, 3025–3034. [Google Scholar] [CrossRef]
- Georgoulias, V.; Papadakis, E.; Alexopoulos, A.; Tsiafaki, X.; Rapti, A.; Veslemes, M.; Palamidas, P.; Vlachonikolis, I. Platinum-based and non-platinum-based chemotherapy in advanced non-small-cell lung cancer: A randomised multicentre trial. Lancet 2001, 357, 1478–1484. [Google Scholar] [CrossRef]
- Park, C.-K.; Oh, I.-J.; Kim, K.-S.; Choi, Y.-D.; Jang, T.-W.; Kim, Y.-S.; Lee, K.-H.; Shin, K.-C.; Jung, C.Y.; Yang, S.-H.; et al. Randomized Phase III Study of Docetaxel Plus Cisplatin Versus Pemetrexed Plus Cisplatin as First-line Treatment of Nonsquamous Non–Small-cell Lung Cancer: A TRAIL Trial. Clin. Lung Cancer 2017, 18, e289–e296. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.-j.; Zhou, Q.; Liao, R.-q.; Huang, Y.-s.; Xu, C.-r.; Wang, Z.; Wang, B.-c.; Chen, H.-j.; Wu, Y.-l. Nedaplatin/gemcitabine versus carboplatin/gemcitabine in treatment of advanced non-small cell lung cancer: A randomized clinical trial. Chin. J. Cancer Res. 2012, 24, 97–102. [Google Scholar] [CrossRef][Green Version]
- Zhou, C.; Wu, Y.-L.; Chen, G.; Liu, X.; Zhu, Y.; Lu, S.; Feng, J.; He, J.; Han, B.; Wang, J.; et al. BEYOND: A Randomized, Double-Blind, Placebo-Controlled, Multicenter, Phase III Study of First-Line Carboplatin/Paclitaxel Plus Bevacizumab or Placebo in Chinese Patients with Advanced or Recurrent Nonsquamous Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2015, 33, 2197–2204. [Google Scholar] [CrossRef]
- Boni, C.; Tiseo, M.; Boni, L.; Baldini, E.; Recchia, F.; Barone, C.; Grossi, F.; Germano, D.; Matano, E.; Marini, G.; et al. Triplets versus doublets, with or without cisplatin, in the first-line treatment of stage IIIB–IV non-small cell lung cancer (NSCLC) patients: A multicenter randomised factorial trial (FAST). Br. J. Cancer 2012, 106, 658–665. [Google Scholar] [CrossRef]
- Paccagnella, A.; Oniga, F.; Bearz, A.; Favaretto, A.; Clerici, M.; Barbieri, F.; Riccardi, A.; Chella, A.; Tirelli, U.; Ceresoli, G.; et al. Adding Gemcitabine to Paclitaxel/Carboplatin Combination Increases Survival in Advanced Non–Small-Cell Lung Cancer: Results of a Phase II-III Study. J. Clin. Oncol. 2006, 24, 681–687. [Google Scholar] [CrossRef]
- Comella, P.; Frasci, G.; Panza, N.; Manzione, L.; De Cataldis, G.; Cioffi, R.; Maiorino, L.; Micillo, E.; Lorusso, V.; Di Rienzo, G.; et al. Randomized Trial Comparing Cisplatin, Gemcitabine, and Vinorelbine With Either Cisplatin and Gemcitabine or Cisplatin and Vinorelbine in Advanced Non–Small-Cell Lung Cancer: Interim Analysis of a Phase III Trial of the Southern Italy Cooperative Oncology Group. J. Clin. Oncol. 2000, 18, 1451–1457. [Google Scholar] [CrossRef] [PubMed]
- Sandler, A.; Gray, R.; Perry, M.C.; Brahmer, J.; Schiller, J.H.; Dowlati, A.; Lilenbaum, R.; Johnson, D.H. Paclitaxel–carboplatin alone or with bevacizumab for non–small-cell lung cancer. N. Engl. J. Med. 2006, 355, 2542–2550. [Google Scholar] [CrossRef]
- Alberola, V.; Camps, C.; Provencio, M.; Isla, D.; Rosell, R.; Vadell, C.; Bover, I.; Ruiz-Casado, A.; Azagra, P.; Jiménez, U.; et al. Cisplatin Plus Gemcitabine Versus a Cisplatin-Based Triplet Versus Nonplatinum Sequential Doublets in Advanced Non–Small-Cell Lung Cancer: A Spanish Lung Cancer Group Phase III Randomized Trial. J. Clin. Oncol. 2003, 21, 3207–3213. [Google Scholar] [CrossRef]
- Reck, M.; Von Pawel, J.; Zatloukal, P.; Ramlau, R.; Gorbounova, V.; Hirsh, V.; Leighl, N.; Mezger, J.; Archer, V.; Moore, N.; et al. Phase III Trial of Cisplatin Plus Gemcitabine with Either Placebo or Bevacizumab As First-Line Therapy for Nonsquamous Non–Small-Cell Lung Cancer: AVAiL. J. Clin. Oncol. 2009, 27, 1227–1234. [Google Scholar] [CrossRef]
- Reck, M.; von Pawel, J.; Zatloukal, P.; Ramlau, R.; Gorbounova, V.; Hirsh, V.; Leighl, N.; Mezger, J.; Archer, V.; Moore, N.; et al. Overall survival with cisplatin–gemcitabine and bevacizumab or placebo as first-line therapy for nonsquamous non-small-cell lung cancer: Results from a randomised phase III trial (AVAiL). Ann. Oncol. 2010, 21, 1804–1809. [Google Scholar] [CrossRef]
- Crinò, L.; Dansin, E.; Garrido, P.; Griesinger, F.; Laskin, J.; Pavlakis, N.; Stroiakovski, D.; Thatcher, N.; Tsai, C.-M.; Wu, Y.-L.; et al. Safety and efficacy of first-line bevacizumab-based therapy in advanced non-squamous non-small-cell lung cancer (SAiL, MO19390): A phase 4 study. Lancet Oncol. 2010, 11, 733–740. [Google Scholar] [CrossRef]
- Patel, J.D.; Socinski, M.A.; Garon, E.B.; Reynolds, C.H.; Spigel, D.R.; Olsen, M.R.; Hermann, R.C.; Jotte, R.M.; Beck, T.; Richards, D.A.; et al. PointBreak: A Randomized Phase III Study of Pemetrexed Plus Carboplatin and Bevacizumab Followed by Maintenance Pemetrexed and Bevacizumab Versus Paclitaxel Plus Carboplatin and Bevacizumab Followed by Maintenance Bevacizumab in Patients with Stage IIIB or IV Nonsquamous Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2013, 31, 4349–4357. [Google Scholar] [CrossRef] [PubMed]
- Mok, T.S.K.; Wu, Y.-L.; Kudaba, I.; Kowalski, D.M.; Cho, B.C.; Turna, H.Z.; Castro, G., Jr.; Srimuninnimit, V.; Laktionov, K.K.; Bondarenko, I.; et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): A randomised, open-label, controlled, phase 3 trial. Lancet 2019, 393, 1819–1830. [Google Scholar] [CrossRef]
- Reck, M.; Rodríguez-Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Pembrolizumab versus Chemotherapy for PD-L1–Positive Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2016, 375, 1823–1833. [Google Scholar] [CrossRef] [PubMed]
- Reck, M.; Rodríguez–Abreu, D.; Robinson, A.G.; Hui, R.; Csőszi, T.; Fülöp, A.; Gottfried, M.; Peled, N.; Tafreshi, A.; Cuffe, S.; et al. Updated Analysis of KEYNOTE-024: Pembrolizumab Versus Platinum-Based Chemotherapy for Advanced Non–Small-Cell Lung Cancer With PD-L1 Tumor Proportion Score of 50% or Greater. J. Clin. Oncol. 2019, 37, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, L.; Rodríguez-Abreu, D.; Gadgeel, S.; Esteban, E.; Felip, E.; De Angelis, F.; Domine, M.; Clingan, P.; Hochmair, M.J.; Powell, S.F.; et al. Pembrolizumab plus Chemotherapy in Metastatic Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 378, 2078–2092. [Google Scholar] [CrossRef]
- Gadgeel, S.; Rodríguez-Abreu, D.; Speranza, G.; Esteban, E.; Felip, E.; Dómine, M.; Hui, R.; Hochmair, M.J.; Clingan, P.; Powell, S.F.; et al. Updated Analysis From KEYNOTE-189: Pembrolizumab or Placebo Plus Pemetrexed and Platinum for Previously Untreated Metastatic Nonsquamous Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2020, 38, 1505–1517. [Google Scholar] [CrossRef] [PubMed]
- Carbone, D.P.; Reck, M.; Paz-Ares, L.; Creelan, B.; Horn, L.; Steins, M.; Felip, E.; van den Heuvel, M.M.; Ciuleanu, T.E.; Badin, F.; et al. First-Line Nivolumab in Stage IV or Recurrent Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2017, 376, 2415–2426. [Google Scholar] [CrossRef]
- Jotte, R.; Cappuzzo, F.; Vynnychenko, I.; Stroyakovskiy, D.; Rodríguez-Abreu, D.; Hussein, M.; Soo, R.; Conter, H.J.; Kozuki, T.; Huang, K.-C.; et al. Atezolizumab in Combination with Carboplatin and Nab-Paclitaxel in Advanced Squamous NSCLC (IMpower131): Results From a Randomized Phase III Trial. J. Thorac. Oncol. 2020, 15, 1351–1360. [Google Scholar] [CrossRef] [PubMed]
- Herbst, R.S.; Giaccone, G.; De Marinis, F.; Reinmuth, N.; Vergnenegre, A.; Barrios, C.H.; Morise, M.; Felip, E.; Andric, Z.; Geater, S.; et al. Atezolizumab for First-Line Treatment of PD-L1–Selected Patients with NSCLC. N. Engl. J. Med. 2020, 383, 1328–1339. [Google Scholar] [CrossRef]
- Paz-Ares, L.; Luft, A.; Vicente, D.; Tafreshi, A.; Gümüş, M.; Mazières, J.; Hermes, B.; Çay Şenler, F.; Csőszi, T.; Fülöp, A.; et al. Pembrolizumab plus Chemotherapy for Squamous Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 379, 2040–2051. [Google Scholar] [CrossRef]
- Socinski, M.A.; Jotte, R.M.; Cappuzzo, F.; Orlandi, F.; Stroyakovskiy, D.; Nogami, N.; Rodríguez-Abreu, D.; Moro-Sibilot, D.; Thomas, C.A.; Barlesi, F.; et al. Atezolizumab for First-Line Treatment of Metastatic Nonsquamous NSCLC. N. Engl. J. Med. 2018, 378, 2288–2301. [Google Scholar] [CrossRef]
- Herbst, R.S.; Prager, D.; Hermann, R.; Fehrenbacher, L.; Johnson, B.E.; Sandler, A.; Kris, M.; Tran, H.T.; Klein, P.; Li, X.; et al. TRIBUTE: A Phase III Trial of Erlotinib Hydrochloride (OSI-774) Combined with Carboplatin and Paclitaxel Chemotherapy in Advanced Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2005, 23, 5892–5899. [Google Scholar] [CrossRef] [PubMed]
- Herbst, R.S.; Giaccone, G.; Schiller, J.H.; Natale, R.B.; Miller, V.; Manegold, C.; Scagliotti, G.; Rosell, R.; Oliff, I.; Reeves, J.A.; et al. Gefitinib in Combination with Paclitaxel and Carboplatin in Advanced Non–Small-Cell Lung Cancer: A Phase III Trial—INTACT 2. J. Clin. Oncol. 2004, 22, 785–794. [Google Scholar] [CrossRef]
- Rosell, R.; Carcereny, E.; Gervais, R.; Vergnenegre, A.; Massuti, B.; Felip, E.; Palmero, R.; Garcia-Gomez, R.; Pallares, C.; Sanchez, J.M.; et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012, 13, 239–246. [Google Scholar] [CrossRef]
- Maemondo, M.; Inoue, A.; Kobayashi, K.; Sugawara, S.; Oizumi, S.; Isobe, H.; Gemma, A.; Harada, M.; Yoshizawa, H.; Kinoshita, I.; et al. Gefitinib or Chemotherapy for Non–Small-Cell Lung Cancer with Mutated EGFR. N. Engl. J. Med. 2010, 362, 2380–2388. [Google Scholar] [CrossRef]
- Wu, Y.-L.; Zhou, C.; Hu, C.-P.; Feng, J.; Lu, S.; Huang, Y.; Li, W.; Hou, M.; Shi, J.H.; Lee, K.Y.; et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): An open-label, randomised phase 3 trial. Lancet Oncol. 2014, 15, 213–222. [Google Scholar] [CrossRef]
- Yang, J.C.-H.; Wu, Y.; Schuler, M.; Sebastian, M.; Popat, S.; Yamamoto, N.; Zhou, C.; Hu, C.-P.; O’Byrne, K.; Feng, J.; et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): Analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol. 2015, 16, 141–151. [Google Scholar] [CrossRef]
- Sequist, L.V.; Yang, J.C.-H.; Yamamoto, N.; Obyrne, K.; Hirsh, V.; Mok, T.; Geater, S.L.; Orlov, S.; Tsai, C.-M.; Boyer, M.; et al. Phase III Study of Afatinib or Cisplatin Plus Pemetrexed in Patients with Metastatic Lung Adenocarcinoma With EGFR Mutations. J. Clin. Oncol. 2013, 31, 3327–3334. [Google Scholar] [CrossRef] [PubMed]
- Ramalingam, S.; Reungwetwattana, T.; Chewaskulyong, B.; Dechaphunkul, A.; Lee, K.; Imamura, F.; Nogami, N.; Ohe, Y.; Cheng, Y.; Cho, B.; et al. Osimertinib vs standard of care (SoC) EGFR-TKI as first-line therapy in patients (pts) with EGFRm advanced NSCLC: FLAURA. Ann. Oncol. 2017, 28, v635. [Google Scholar] [CrossRef]
- Ramalingam, S.S.; Gray, J.E.; Ohe, Y.; Cho, B.C.; Vansteenkiste, J.; Zhou, C.; Reungwetwattana, T.; Cheng, Y.; Chewaskulyong, B.; Shah, R.; et al. Osimertinib vs comparator EGFR-TKI as first-line treatment for EGFRm advanced NSCLC (FLAURA): Final overall survival analysis. Ann. Oncol. 2019, 30, v914–v915. [Google Scholar] [CrossRef]
- Mitsudomi, T.; Morita, S.; Yatabe, Y.; Negoro, S.; Okamoto, I.; Tsurutani, J.; Seto, T.; Satouchi, M.; Tada, H.; Hirashima, T.; et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): An open label, randomised phase 3 trial. Lancet Oncol. 2010, 11, 121–128. [Google Scholar] [CrossRef]
- Yoshioka, H.; Mitsudomi, T.; Morita, S.; Yatabe, Y.; Negoro, S.; Okamoto, I.; Seto, T.; Satouchi, M.; Tada, H.; Hirashima, T.; et al. Final overall survival results of WJTOG 3405, a randomized phase 3 trial comparing gefitinib (G) with cisplatin plus docetaxel (CD) as the first-line treatment for patients with non-small cell lung cancer (NSCLC) harboring mutations of the epidermal growth factor receptor (EGFR). J. Clin. Oncol. 2014, 32, 8117. [Google Scholar] [CrossRef]
- Wu, Y.-L.; Lu, S.; Lu, Y.; Zhou, J.; Shi, Y.-K.; Sriuranpong, V.; Ho, J.; Ong, C.K.; Tsai, C.-M.; Chung, C.-H.; et al. Results of PROFILE 1029, a Phase III Comparison of First-Line Crizotinib versus Chemotherapy in East Asian Patients with ALK-Positive Advanced Non–Small Cell Lung Cancer. J. Thorac. Oncol. 2018, 13, 1539–1548. [Google Scholar] [CrossRef]
- Solomon, B.J.; Mok, T.; Kim, D.-W.; Wu, Y.-L.; Nakagawa, K.; Mekhail, T.; Felip, E.; Cappuzzo, F.; Paolini, J.; Usari, T.; et al. First-Line Crizotinib versus Chemotherapy in ALK-Positive Lung Cancer. N. Engl. J. Med. 2014, 371, 2167–2177. [Google Scholar] [CrossRef]
- Solomon, B.J.; Kim, D.-W.; Wu, Y.-L.; Nakagawa, K.; Mekhail, T.; Felip, E.; Cappuzzo, F.; Paolini, J.; Usari, T.; Tang, Y.; et al. Final Overall Survival Analysis from a Study Comparing First-Line Crizotinib Versus Chemotherapy in ALK-Mutation-Positive Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2018, 36, 2251–2258. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.; Camidge, D.R.; Shaw, A.T.; Gadgeel, S.; Ahn, J.S.; Kim, D.-W.; Coudert, B.; Pérol, M.; Dziadziuszko, R.; Rosell, R.; et al. Alectinib versus Crizotinib in Untreated ALK-Positive Non–Small-Cell Lung Cancer. N. Engl. J. Med. 2017, 377, 829–838. [Google Scholar] [CrossRef]
- Shaw, A.T.; Bauer, T.M.; De Marinis, F.; Felip, E.; Goto, Y.; Liu, G.; Mazieres, J.; Kim, D.-W.; Mok, T.; Polli, A.; et al. First-Line Lorlatinib or Crizotinib in Advanced ALK-Positive Lung Cancer. N. Engl. J. Med. 2020, 383, 2018–2029. [Google Scholar] [CrossRef]
- Shaw, A.; Riely, G.; Bang, Y.-J.; Kim, D.-W.; Camidge, D.; Solomon, B.; Varella-Garcia, M.; Iafrate, A.; Shapiro, G.; Usari, T.; et al. Crizotinib in ROS1-rearranged advanced non-small-cell lung cancer (NSCLC): Updated results, including overall survival, from PROFILE 1001. Ann. Oncol. 2019, 30, 1121–1126. [Google Scholar] [CrossRef]
- Moro-Sibilot, D.; Cozic, N.; Pérol, M.; Mazières, J.; Otto, J.; Souquet, P.; Bahleda, R.; Wislez, M.; Zalcman, G.; Guibert, S.; et al. Crizotinib in c-MET- or ROS1-positive NSCLC: Results of the AcSé phase II trial. Ann. Oncol. 2019, 30, 1985–1991. [Google Scholar] [CrossRef]
- Planchard, D.; Kim, T.M.; Mazieres, J.; Quoix, E.; Riely, G.; Barlesi, F.; Souquet, P.-J.; Smit, E.F.; Groen, H.J.M.; Kelly, R.J.; et al. Dabrafenib in patients with BRAFV600E-positive advanced non-small-cell lung cancer: A single-arm, multicentre, open-label, phase 2 trial. Lancet Oncol. 2016, 17, 642–650. [Google Scholar] [CrossRef]
- Mazieres, J.; Cropet, C.; Montané, L.; Barlesi, F.; Souquet, P.; Quantin, X.; Dubos-Arvis, C.; Otto, J.; Favier, L.; Avrillon, V.; et al. Vemurafenib in non-small-cell lung cancer patients with BRAFV600 and BRAFnonV600 mutations. Ann. Oncol. 2020, 31, 289–294. [Google Scholar] [CrossRef]
- Planchard, D.; Besse, B.; Groen, H.J.; Souquet, P.-J.; Quoix, E.; Baik, C.S.; Barlesi, F.; Kim, T.M.; Mazieres, J.; Novello, S.; et al. Dabrafenib plus trametinib in patients with previously treated BRAFV600E-mutant metastatic non-small cell lung cancer: An open-label, multicentre phase 2 trial. Lancet Oncol. 2016, 17, 984–993. [Google Scholar] [CrossRef]
- Planchard, D.; Besse, B.; Kim, T.M.; Quoix, E.A.; Souquet, P.J.; Mazieres, J.; Barlesi, F.; Groen, H.J.; Smit, E.F.; Baik, C.S.; et al. Updated survival of patients (pts) with previously treated BRAF V600E–mutant advanced non-small cell lung cancer (NSCLC) who received dabrafenib (D) or D + trametinib (T) in the phase II BRF113928 study. J. Clin. Oncol. 2017, 35, 9075. [Google Scholar] [CrossRef]
- Gao, G.; Li, X.; Wang, Q.; Zhang, Y.; Chen, J.; Shu, Y.; Hu, Y.; Fan, Y.; Fang, J.; Chen, G.; et al. Single-arm, phase II study of pyrotinib in advanced non-small cell lung cancer (NSCLC) patients with HER2 exon 20 mutation. J. Clin. Oncol. 2019, 37, 9089. [Google Scholar] [CrossRef]
- Smit, E.F.; Nakagawa, K.; Nagasaka, M.; Felip, E.; Goto, Y.; Li, B.T.; Pacheco, J.M.; Murakami, H.; Barlesi, F.; Saltos, A.N.; et al. Trastuzumab deruxtecan (T-DXd; DS-8201) in patients with HER2-mutated metastatic non-small cell lung cancer (NSCLC): Interim results of DESTINY-Lung01. J. Clin. Oncol. 2020, 38, 9504. [Google Scholar] [CrossRef]
- Socinski, M.; Cornelissen, R.; Garassino, M.; Clarke, J.; Tchekmedyian, N.; Molina, J.; Goldman, J.; Bhat, G.; Lebel, F.; Le, X. LBA60 ZENITH20, a multinational, multi-cohort phase II study of poziotinib in NSCLC patients with EGFR or HER2 exon 20 insertion mutations. Ann. Oncol. 2020, 31, S1188. [Google Scholar] [CrossRef]
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–655. [Google Scholar] [CrossRef]
- Zubrod, C.G.; Schneiderman, M.; Frei, E.; Brindley, C.; Gold, G.L.; Shnider, B.; Oviedo, R.; Gorman, J.; Jones, R.; Jonsson, U.; et al. Appraisal of methods for the study of chemotherapy of cancer in man: Comparative therapeutic trial of nitrogen mustard and triethylene thiophosphoramide. J. Chronic Dis. 1960, 11, 7–33. [Google Scholar] [CrossRef]
- Buccheri, G.; Ferrigno, D.; Tamburini, M. Karnofsky and ECOG performance status scoring in lung cancer: A prospective, longitudinal study of 536 patients from a single institution. Eur. J. Cancer 1996, 32, 1135–1141. [Google Scholar] [CrossRef]
- Sok, M.; Zavrl, M.; Greif, B.; Srpčič, M. Objective assessment of WHO/ECOG performance status. Support. Care Cancer 2019, 27, 3793–3798. [Google Scholar] [CrossRef]
- Calvert, A.H.; Newell, D.R.; Gumbrell, L.A.; O’Reilly, S.; Burnell, M.; Boxall, F.E.; Siddik, Z.H.; Judson, I.R.; Gore, M.E.; Wiltshaw, E. Carboplatin dosage: Prospective evaluation of a simple formula based on renal function. J. Clin. Oncol. 1989, 7, 1748–1756. [Google Scholar] [CrossRef]
- Julka, P.K.; Doval, D.C.; Gupta, S.; Rath, G.K. Response assessment in solid tumours: A comparison of WHO, SWOG and RECIST guidelines. Br. J. Radiol. 2008, 81, 444–449. [Google Scholar] [CrossRef]
- Jang, G.-S.; Kim, M.-J.; Ha, H.-I.; Kim, J.H.; Kim, H.S.; Ju, S.B.; Zang, D.Y. Comparison of RECIST version 1.0 and 1.1 in assessment of tumor response by computed tomography in advanced gastric cancer. Chin. J. Cancer Res. 2013, 25, 689–694. [Google Scholar] [CrossRef]
- McKee, A.E.; Farrell, A.T.; Pazdur, R.; Woodcock, J. The Role of the U.S. Food and Drug Administration Review Process: Clinical Trial Endpoints in Oncology. Oncologist 2010, 15, 13–18. [Google Scholar] [CrossRef]
- Ardizzoni, A.; Boni, L.; Tiseo, M.; Fossella, F.V.; Schiller, J.H.; Paesmans, M.; Radosavljevic, D.; Paccagnella, A.; Zatloukal, P.; Mazzanti, P.; et al. Cisplatin- Versus Carboplatin-Based Chemotherapy in First-Line Treatment of Advanced Non-Small-Cell Lung Cancer: An Individual Patient Data Meta-analysis. J. Natl. Cancer Inst. 2007, 99, 847–857. [Google Scholar] [CrossRef]
- Hotta, K.; Matsuo, K.; Ueoka, H.; Kiura, K.; Tabata, M.; Tanimoto, M. Meta-Analysis of Randomized Clinical Trials Comparing Cisplatin to Carboplatin in Patients with Advanced Non–Small-Cell Lung Cancer. J. Clin. Oncol. 2004, 22, 3852–3859. [Google Scholar] [CrossRef]
- Sanborn, R.E. Cisplatin versus carboplatin in NSCLC: Is there one “best” answer? Curr. Treat. Options Oncol. 2008, 9, 326–342. [Google Scholar] [CrossRef]
- Rajeswaran, A.; Trojan, A.; Burnand, B.; Giannelli, M. Efficacy and side effects of cisplatin- and carboplatin-based doublet chemotherapeutic regimens versus non-platinum-based doublet chemotherapeutic regimens as first line treatment of metastatic non-small cell lung carcinoma: A systematic review of randomized controlled trials. Lung Cancer 2008, 59, 1–11. [Google Scholar] [CrossRef]
- D’Addario, G.; Pintilie, M.; Leighl, N.B.; Feld, R.; Cerny, T.; Shepherd, F.A. Platinum-Based Versus Non-Platinum-Based Chemotherapy in Advanced Non-Small-Cell Lung Cancer: A Meta-Analysis of the Published Literature. J. Clin. Oncol. 2005, 23, 2926–2936. [Google Scholar] [CrossRef]
- Liu, Y.; Yu, S.; Liu, S.; Cao, H.; Ma, R.; Wu, J.; Feng, J. Comparison of nedaplatin-based versus cisplatin-based chemotherapy for advanced non-small cell lung cancer among East Asian populations: A meta-analysis. Sci. Rep. 2015, 5, 10516. [Google Scholar] [CrossRef]
- Scagliotti, G.; Brodowicz, T.; Shepherd, F.A.; Zielinski, C.; Vansteenkiste, J.; Manegold, C.; Simms, L.; Fossella, F.; Sugarman, K.; Belani, C. Treatment-by-Histology Interaction Analyses in Three Phase III Trials Show Superiority of Pemetrexed in Nonsquamous Non-small Cell Lung Cancer. J. Thorac. Oncol. 2011, 6, 64–70. [Google Scholar] [CrossRef]
- Treat, J.; Scagliotti, G.V.; Peng, G.; Monberg, M.J.; Obasaju, C.K.; Socinski, M.A. Comparison of pemetrexed plus cisplatin with other first-line doublets in advanced non-small cell lung cancer (NSCLC): A combined analysis of three phase 3 trials. Lung Cancer 2012, 76, 222–227. [Google Scholar] [CrossRef]
- Shaw, A.T.; Yeap, B.Y.; Solomon, B.J.; Riely, G.J.; Iafrate, A.J.; Shapiro, G.; Costa, D.B.; Butaney, M.; Ou, S.I.; Maki, R.G.; et al. Impact of crizotinib on survival in patients with advanced, ALK-positive NSCLC compared with historical controls. J. Clin. Oncol. 2011, 29, 7507. [Google Scholar] [CrossRef]
- Oh, I.-J.; Kim, K.-S.; Kim, Y.-C.; Ban, H.-J.; Kwon, Y.-S.; Kim, Y.-I.; Lim, S.-C.; Chung, W.-K.; Nam, T.-K.; Song, J.-Y.; et al. A phase III concurrent chemoradiotherapy trial with cisplatin and paclitaxel or docetaxel or gemcitabine in unresectable non-small cell lung cancer: KASLC 0401. Cancer Chemother. Pharmacol. 2013, 72, 1247–1254. [Google Scholar] [CrossRef]
- Berghmans, T.; Lafitte, J.-J.; Scherpereel, A.; Paesmans, M.; LeComte, J.; Marco, V.G.; Meert, A.-P.; Leclercq, N.; Sculier, J.-P. An ELCWP phase III trial comparing ifosfamide and cisplatin regimens in advanced NSCLC. Anticancer Res. 2013, 33, 5477–5482. [Google Scholar]
- Lee, C.K.; Davies, L.; Wu, Y.-L.; Mitsudomi, T.; Inoue, A.; Rosell, R.; Zhou, C.; Nakagawa, K.; Thongprasert, S.; Fukuoka, M.; et al. Gefitinib or Erlotinib vs. Chemotherapy for EGFR Mutation-Positive Lung Cancer: Individual Patient Data Meta-Analysis of Overall Survival. J. Natl. Cancer Inst. 2017, 109, djw279. [Google Scholar] [CrossRef]
- Sutandyo, N.; Hanafi, A.; Jayusman, M. Comparison of Effectiveness of Gefitinib, Erlotinib, and Afatinib in Advanced Non-small Cell Lung Cancer Patients with EGFR Mutation Positive in Indonesian Population. Zhongguo Fei Ai Za Zhi 2019, 22, 562–567. [Google Scholar]
- Krawczyk, P.; Kowalski, D.; Ramlau, R.; Kalinka, E.; Winiarczyk, K.; Stencel, K.; Powrózek, T.; Reszka, K.; Wojas-Krawczyk, K.; Bryl, M.; et al. Comparison of the effectiveness of erlotinib, gefitinib, and afatinib for treatment of non-small cell lung cancer in patients with common and rare EGFR gene mutations. Oncol. Lett. 2017, 13, 4433–4444. [Google Scholar] [CrossRef]
- Zhao, S.; Gao, F.; Zhang, Y.; Zhang, Z.; Zhang, L. Bevacizumab in combination with different platinum-based doublets in the first-line treatment for advanced nonsquamous non-small-cell lung cancer: A network meta-analysis. Int. J. Cancer 2018, 142, 1676–1688. [Google Scholar] [CrossRef]
- Zhou, Y.; Chen, C.; Zhang, X.; Fu, S.; Xue, C.; Ma, Y.; Fang, W.; Yang, Y.; Hou, X.; Huang, Y.; et al. Immune-checkpoint inhibitor plus chemotherapy versus conventional chemotherapy for first-line treatment in advanced non-small cell lung carcinoma: A systematic review and meta-analysis. J. Immunother. Cancer 2018, 6, 155. [Google Scholar] [CrossRef]
- You, W.; Liu, M.; Miao, J.-D.; Liao, Y.-Q.; Song, Y.-B.; Cai, D.-K.; Gao, Y.; Peng, H. A Network Meta-analysis Comparing the Efficacy and Safety of Anti-PD-1 with Anti-PD-L1 in Non-small Cell Lung Cancer. J. Cancer 2018, 9, 1200–1206. [Google Scholar] [CrossRef]
- Kim, R.; Keam, B.; Hahn, S.; Ock, C.-Y.; Kim, M.; Kim, T.M.; Kim, D.-W.; Heo, D.S. First-line Pembrolizumab Versus Pembrolizumab Plus Chemotherapy Versus Chemotherapy Alone in Non–small-cell Lung Cancer: A Systematic Review and Network Meta-analysis. Clin. Lung Cancer 2019, 20, 331–338.e4. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. FDA Approves Nivolumab Plus Ipilimumab for First-Line mNSCLC (PD-L1 Tumor Expression ≥ 1%); FDA: Silver Spring, MD, USA, 2020. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-nivolumab-plus-ipilimumab-first-line-mnsclc-pd-l1-tumor-expression-1 (accessed on 4 November 2021).
- U.S. Food and Drug Administration. FDA Grants Accelerated Approval to Tepotinib for Metastatic Non-Small Cell Lung Cancer; FDA: Silver Spring, MD, USA, 2021. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-tepotinib-metastatic-non-small-cell-lung-cancer (accessed on 4 November 2021).
- U.S. Food and Drug Administration. FDA Grants Accelerated Approval to Capmatinib for Metastatic Non-Small Cell Lung Cancer; FDA: Silver Spring, MD, USA, 2020. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-capmatinib-metastatic-non-small-cell-lung-cancer (accessed on 4 November 2021).
- U.S. Food and Drug Administration. FDA Approves Entrectinib for NTRK Solid Tumors and ROS-1 NSCLC; FDA: Silver Spring, MD, USA, 2019. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-entrectinib-ntrk-solid-tumors-and-ros-1-nsclc (accessed on 4 November 2021).
| PS ** | Median Age | Regimen | Patients(n) | Objective Response (CR + PR)/SD/PD; ORR (%) * | Median OS/MST *** | Study |
|---|---|---|---|---|---|---|
| 0–1 | 63 | Cisplatin monotherapy vs. Cisplatin + Vinorelbine | 415 | 25 (0/25)/72/112; 12% vs. 54 (4/50)/97/55; 26% (p = 0.0002) | 8 m vs. 6 m (p = 0.0018) | 1998, Wozniak et al. [26] |
| WHO PS 0–2 | 59 vs. 59 vs. 60 | Vinorelbine + Cisplatin (NVB-P) vs. Vindesine + Cisplatin (VDS-P) vs. Vinorelbine monotherapy (NVB) | 612 | 57 (NR)/NR/NR; 30% vs.35 (NR)/NR/NR; 19% vs.28 (NR)/NR/NR; 14% NVB-P vs. VDS-P (X2, p = 0.02) NVB-P vs. NVB (X2, p < 0.001) | 40 w vs. 32 w vs. 31 w NVB-P vs. VDS-P (p = 0.4) NVB-P vs. NVB (p = 0.1) | 1994, Le Chevalier et al. [27] |
| KPS 70–100 | 62 vs. 63 | Gemcitabine + Cisplatin vs. Cisplatin monotherapy | 522 | 79 (3/76)/97/38; 30.4% vs. 29 (1/28)/111/86; 11.1% (p < 0.0001) | 9.1 m vs. 7.6 m (log-rank test, p = 0.004) | 2000, Sandler et al. [28] |
| WHO PS 0–2 | 58.8 vs. 59.2 | Vinorelbine monotherapy vs. Vinorelbine + Cisplatin | 240 | 18 (1/17)28/58; 16% vs. 50 (2/48)/35/19; 43% (p = 0.0001) | 32 w vs. 33 w (log-rank test p = 0.48) | 1994, Depierre et al. [29] |
| ECOG PS 2 | 65 vs. 65 | Pemetrexed monotherapy vs. Pemetrexed + Carboplatin | 217 | 7; s10.5% vs. 19; 24% (p = 0.32) | 5.3 (95% CI, 4.1–6.5 m) vs. 9.3 m (95% CI, 7.4–11.2 m) (HR, 0.62; 95% CI, 0.46–0.83, p = 0.001) | 2013, Zukin et al. [30] |
| PS ** | Median Age | Regimen | Patients (n) | Objective Response (CR+PR)/SD/PD; ORR (%) * | Median OS/MST *** | Study |
|---|---|---|---|---|---|---|
| ECOG PS 0–2 | 63 | Cisplatin + Paclitaxel vs. Cisplatin + Gemcitabine vs. Cisplatin + Docetaxel vs. Carboplatin + Paclitaxel | 1155 | (<1% + 21%)/18%/49%; 21% vs. 22% (1% + 21%)/18%/40%; 22% vs. (<1% + 17%)/25%/42%; 17% vs. (<1% + 16%)/23%/49%; 17% | 7.8 m (95% CI, 7.0–8.9 m) vs. 8.1 m (95% CI, 7.2–9.4 m) vs. 7.4 m (95% CI, 6.6–8.8 m) vs. 8.1 m (95% CI, 7.0–9.5 m) | 2002, Schiller et al. [34] |
| ECOG PS 0–1 | 61.1 vs. 61.0 | Cisplatin + Pemetrexed vs. Cisplatin + Gemcitabine | 1725 | 30.6% vs. 28.2% | 10.3 m vs. 10.3 m (HR = 0.94, 95% CI, 0.84–1.05) | 2008, Scagliotti et al. [35] |
| WHO PS 0–2 | 64 vs. 66 | Pemetrexed +Carboplatin vs. Gemcitabine + Carboplatin | 446 | NR | 7.3 m vs. 7.0 m (p = 0.63) | 2009, Grønberg et al. [36] |
| ECOG PS 0–2 | 60.1 vs. 58.9 | Pemetrexed +Carboplatin vs. Docetaxel + Carboplatin | 260 | 34% vs. 22.9% (OR = 1.68 (95% CI: 0.91–3.10), p = 0.095) | HR = 0.93 (95% CI: 0.66–1.32), p = 0.698 | 2011, Rodrigues-Pereira et al. [37] |
| KPS 70–100 | 63 vs. 62 | Gemcitabine + Cisplatin vs. Gemcitabine + Carboplatin | 176 | 36 (5 + 31)/29/16; 41.4% (95% CI: 31.0–51.7%) vs. 26 (5 + 21)/39/21; 29.2% (95% CI: 19.8–38.7%) (p = 0.09) | 8.75 m (95% CI: 6.7–10.5 m) vs. 8 m (95% CI: 6.9–11.4 m) (p = 0.9024) | 2003, Zatloukal et al. [38] |
| ECOG PS 0–1 | 62 vs. 63 vs. 61 vs. 61 | Cisplatin + Irinotecan (IP) vs. Paclitaxel + Carboplatin (TC) vs. Cisplatin + Gemcitabine (GP) vs. Cisplatin + Vinorelbine (NP) | 602 | 31% vs. 32.4% (p = 0.801 *) vs. 30.1% (p = 0.868 *) vs. 33.1% (p = 0.706 *) * Compared with IP by the x2 test. | 13.9 m vs. 12.3 m vs. 14.0 m vs. 11.4 m | 2007, Ohe et al. [39] |
| PS 0–1 | 61 vs. 62 | Cisplatin + Vinorelbine vs. Paclitaxel + Carboplatin | 408 | 56 (0 + 56)/53/56; 28% vs. 52 (2 + 50)/67/53; 25% (p = NS) | 8.1 m (95% CI, 6.7–9.6 m) vs. 8.6 m (95% CI, 7.2–10.7 m) (p = 0.87) | 2001, Kelly et al. [40] |
| ECOG PS 0–2 | 63 vs.62 vs.63 | Gemcitabine + Cisplatin (GC) vs. Paclitaxel + Carboplatin (PCb) vs. Vinorelbine + Cisplatin (VC) | 607 | 62 (0 + 62)/81/36; 30% (95% CI 24–37%) vs. 64 (1 + 63)/75/37; 32% (95% CI 25–38%) vs. 61 (1 + 60)/62/34; 30% (95% CI 24–36%) (GC vs. VC, p = 0.982) (PCb vs. VC, p = 0.747) | 9.8 m (95% CI, 8.6–11.2 m) vs. 10.0 m (95% CI, 9.0–12.5 m) vs. 9.5 m (95% CI, 8.3–11.0 m) * No differences between experimental arm and reference arm (VC) | 2002, Scagliotti et al. [41] |
| KPS 70–100 | 61 vs. 59 vs. 61 | Docetaxel + Cisplatin (DC) vs. Docetaxel + Carboplatin (DCb) vs. Vinorelbine + Cisplatin (VC) | 1218 patients | 129 (8 + 121)/176/72; 31.6% (95% CI 27.1–36.4%) vs. 97 (5 + 92)/188/88; 23.9% (95% CI 19.8–28.3%) vs. 99 (8 + 91)/170/86; 24.5% (95% CI 20.4–29.0%) DC vs. VC (p = 0.029) DCb vs. VC (p = 0.870) | DC vs. VC = 11.3 m vs. 10.1 m (HR = 1.183 (97.2% CI, 0.989–1.416)) * Not statistically significant DCb vs. VC = 9.4 m vs. 9.9 m (HR = 1.048 (97.2% CI, 0.877–1.253)) * Not statistically significant | 2003, Fossella et al. [42] |
| ECOG PS 0–1 | 64 vs. 65 | Nedaplatin + Docetaxel vs. Cisplatin + Docetaxel | 355 | 96 (3 + 93)/50/NR); 56% vs. 89 (1 + 88)/47/NR); 53% (two-sided Fisher’s exact test, p = 0.66) | 13.6 m (95% CI 11–15.6 m) vs. 11.4 m (95% CI 10.2–12.2 m) (HR 0.81, 95% CI 0.65–1.02; one-sided stratified log-rank, p = 0.037) | 2015, Shukuya et al. [32] |
| NR | NR | Nedaplatin + Gemcitabine/Paclitaxel/Navelbine/Docetaxel/Cyclophosphamide + Doxorubicin vs. Cisplatin + Gemcitabine/Paclitaxel/Navelbine/Docetaxel/Cyclophosphamide + Doxorubicin | 392 | NR | 20 m (95% CI 17.0–23.0 m) vs. 15 m (95% CI 13.4–16.6 m) (p = 0.022) | 2015, Shan et al. [33] |
| NR | 56.28 vs. 55.01 | Nedaplatin Group (NDP + Pemetrexed/Docetaxel/Gemcitabine/Vinorelbine/Paclitaxel) vs. Cisplatin Group (DDP + Pemetrexed/Docetaxel/Gemcitabine/Vinorelbine/Paclitaxel) | 619 | 143 (12 + 131)/137/14; 48.6% vs. 114 (10 + 104)/176/35; 35.1% (p < 0.01) | (14.783 ± 1.092) m vs. (13.502 ± 2.327) m (p < 0.01) | 2014, Li et al. [43] |
| ECOG 0–2 | 58 vs. 58 | Paclitaxel + Cisplatin vs. Paclitaxel + Carboplatin | 618 | 80 (2 + 78)/123/58; 28% (95% CI 23–34%) vs. 70 (4 + 66)/112/80; 25% (95% CI 20–31%) * Paclitaxel/Carboplatin is statistically non-inferior compared to paclitaxel/cisplatin | 9.8 m (95% CI 8.2–11 m) vs. 8.2 m (95% CI 7.4–9.6 m) (p = 0.019) | 2002, Rosell et al. [44] |
| ECOG 0–2 | 62 | Cisplatin based regimen (Cisplatin + Gemcitabine/Vinorelbine) vs. Gemcitabine + Vinorelbine | 503 | 30% vs. 25% (p = 0.30) | 38 w vs. 32 w (HR = 1.15; 90% CI 0.96–1.37; one-sided, p = 0.08) | 2003, Gridelli et al. [45] |
| WHO PS 0–2 | 61 vs. 62 | Cisplatin + Docetaxel vs. Gemcitabine + Docetaxel | 441 | 71 (3 + 68)/71/53; 34.6% (95%CI 28.1–41.1%) vs. 67 (2 + 65)/67/58; 33.3% (95%CI 26.8–39.9%) * No statistically significant difference in both ORRs | 10 m (95%CI 0.5–37.5 m) vs. 9.5 m (95% CI 1–36 m) (p = 0.980) | 2001, Georgoulias et al. [46] |
| ECOG PS 0–2 | 63.0 vs. 63.6 | Pemetrexed + Cisplatin vs. Docetaxel + Cisplatin | 156 | 24;35.2% vs. 24;37.5% * No statistically significant difference | 11.7 m (95% CI, 8.6–14.8 m) vs. 13.3 m (95% CI, 8.1–18.5 m) (p > 0.5) | 2017, Park et al. [47] |
| ECOG 0–2 | 56.8 vs. 57.5 | Nedaplatin + Gemcitabine vs. Carboplatin + Gemcitabine | 49 | 9 (0 + 9)/13/2; 37.5% vs. 6 (0 + 6)/15/4; 24% (p = 0.305) | 17.5 m (95% CI 10.8–24.2 m) vs. 17 m (95% CI 12.1–21.9 m) (p = 0.961) | 2012, Yang et al. [48] |
| PS ** | Median Age | Regimen | Patients (n) | Objective Response (CR+PR)/SD/PD; ORR (%) * | Median OS/MST *** | Study |
|---|---|---|---|---|---|---|
| ECOG 0–2 | 63 | Gemcitabine + Cisplatin (GP) vs. Gemcitabine + Vinorelbine (GN) vs. Gemcitabine + Ifosfamide + Cisplatin (GIP) vs. Gemcitabine + Ifosfemide + Vinorelbine (GIN) | 433 | Platinum based vs. Non-platinum based: 66 (4 + 62)/77/29; 31% (95% CI 25–37%) vs. 52 (4 + 48)/71/39; 24% (95% CI 19–30%) (OR = 0.72, 95% CI 0.47–1.10, p = 0.124) Doublet vs. Triplet therapy: 61 (4 + 57)/69/34;29% (95% CI 23–35%) vs. 57 (4 + 57)/79/34;28% (95% CI 21–33%) (OR = 0.86, 95% CI 0.56–1.32, p = 0.487) | Platinum based vs. Non-platinum based: 11.3 m (95% CI 9.8–12.7 m) vs. 9.7 m (95% CI 8.7–10.8 m) (HR = 1.23, 95% CI 1.01–1.49, p = 0.044) Doublet vs. Triplet therapy: 10.4 m (95% CI 9.4–12.2 m) vs. 10.3 m (95% CI 9.2–11.8 m) (HR = 1.03, 95% CI 0.85–1.25, p = 0.781) | 2012, Boni et al. [50] |
| WHO PS 0–2 | 62 | Paclitaxel + Carboplatin vs. Gemcitabine + Paclitaxel + Carboplatin | 324 | 30 (0 + 30)/48/72; 20% vs. 69 (10 + 59)/43/46; 43.6% (p ≤ 0.0001) | 8.3 m vs. 10.8 m (p = 0.044, HR = 1.31, 95% CI 1.02–1.68) | 2006, Paccagnella et al. [51] |
| ECOG PS 0–1 | 62 | Cisplatin + Gemcitabine + Vinorelbine (PGV) vs. Cisplatin + Gemcitabine (PG) vs. Cisplatin + Vinorelbine (PV) | 180 | 28 (2 + 26)/17/15; 47% (95% CI 34–60%) vs. 15 (0 + 15)/15/30; 25% (95% CI 15–38%) vs. 18 (0 + 18)/22/20; 30% (95% CI 19–43%) | 51 w vs. 42 w vs. 35 w PGV vs. PV: HR = 0.35 (95% CI 0.16 to 0.77, p < 0.0058) | 2000, Pasquale et al. [52] |
| ECOG PS 0–1 | NR | Paclitaxel + Carboplatin + Bevacizumab vs. Paclitaxel + Carboplatin | 878 | 59; 15% vs. 133; 35% (p < 0.001) | 12.3 m vs. 10.3 m (HR = 0.79, 95% CI 0.67–0.92, p = 0.003) | 2006, Sandler et al. [53] |
| ECOG 0–2 | 59 vs. 59 vs. 60 | Cisplatin + Gemcitabine (CG) vs. Cisplatin + Gemcitabine + Vinorelbine (CGV) vs. Sequential doublet of Gemcitabine + Vinorelbine followed by Vinorelbine + Ifosfamide (GV-VI) | 570 | 77 (4 + 73)/40/38; 42% vs. 77 (3 + 74)/35/38; 41% vs. 50 (2 + 48)/62/43; 27% (CG vs. CGV, p = 0.4) (CG vs. GV-VI, p = 0.003) CGV vs. GV-VI, p = 0.001) | 9.3 m (95% CI 8.1–10.5 m) vs. 8.2 m (95% CI 7–9.4 m) vs. 8.1 m (95% CI 6.9–9.2 m) (Not statistically significant) | 2003, Alberola et al. [54] |
| ECOG 0–1 | 59 vs. 57 vs. 59 | Placebo + Cisplatin + Gemcitabine (CG) vs. Bevacizumab 7.5 mg/kg + Cisplatin + Gemcitabine (CGB7.5) vs. Bevacizumab 15 mg/kg + Cisplatin + Gemcitabine (CGB15) | 1043 | 20.1% vs. 34.1% vs. 30.4% (CG vs. CGB7.5, p < 0.0001) (CG vs. CGB15, p = 0.0023) | With post-study therapy: 13.1 m vs. 13.6 m vs. 13.4 m (CG vs. CGB7.5 = HR 0.93, 95% CI 0.78–1.11, p = 0.420) (CG vs. CGB15 = HR 1.03, 95% CI 0.86–1.23, p = 0.76) Without poststudy therapy: CG vs. CGB (7.5 + 15) 7.3 m vs. 8.7 m (HR 0.84, p = 0.20) | 2009, Reck et al. [55] |
| 2010, Reck et al. [56] | ||||||
| ECOG 0–1 | 57 vs. 56 | Carboplatin + Paclitaxel + Bevacizumab vs. Carboplatin + Paclitaxel + Placebo | 276 | 74 (0 + 74)/55/2; 54% (95% CI 46–63%) vs. 35 (0 + 35)/83/10; 26% (95% CI 19–35%) (p < 0.001) | 24.3 m vs. 17.7 m (HR 0.68; 95% CI 0.50–0.93, p = 0.0154) | 2015, Zhou et al. [49] |
| ECOG 0–2 | 58.8 | Bevacizumab + standard-of-care first-line chemotherapy: Carboplatin doublet vs. Cisplatin doublet vs. Non-platinum doublets vs. Monotherapy vs. Triplet and quadruplet chemotherapy regimen | 2212 | Post-baseline disease assessment (2036 patients): 1049 (65 + 984)/756/NR; 51% | Overall population: Median OS 14.6 m (95% CI 13.8–15.3 m 14.3 m (95% CI 13.2–15.6 m) vs. 14.7 m (95% CI 13.7–16.0 m) vs. 8.1 m (95% CI 5.7–13.0 m) vs. 9.4 m (95% CI 5.3–14.7 m) vs. 13.8 m (95% CI 4.4–21.7 m) | 2010, Crinò, et al. [57] |
| ECOG PS 0–1 | 64.6 vs. 64.9 | Pemetrexed + Carboplatin + Bevacizumab vs. Paclitaxel + Carboplatin + Bevacizumab | 939 | 34.1% vs. 33.0% | 12.6 m vs. 13.4 m (HR = 1.00, 95% CI 0.86–1.16, p = 0.949) | 2013, Patel et al. [58] |
| PS ** | Median Age | Regimen | Patients (n) | Objective Response (CR + PR)/SD/PD; ORR (%) * | Median OS/MST *** | Study |
|---|---|---|---|---|---|---|
| ECOG 0–1 | 63 | Pembrolizumab vs. Carboplatin + Paclitaxel/Pemetrexed | 1275 | NR | TPS 50% or greater: 20 m (95% CI 15.4–24.9 m) vs. 12.2 m (95% CI 10.4–14.2 m) (HR 0.69, 95% CI 0.56–0.85, p = 0.003) TPS 20% or greater: 17.7 m (95% CI 15.3–22.1 m) vs. 13.0 m (95% CI 11.6–15.3 m) (HR 0.77, 95% CI 0.64–0.92, p = 0.002) TPS 1% or greater: 16.7 m (95% CI 13.9–19.7 m) vs. 12.1 m (95% CI 11.3–13.3 m) (HR 0.81, 95% CI 0.73–0.93, p = 0.0018 | 2019, Mok et al. [59] |
| ECOG 0–1 | 64.5 vs. 66.0 | Pembrolizumab vs. Platinum-based regimen (Carboplastin + Pemetrexed, Cisplatin + Pemetrexed, Carboplastin + Gemcitabine, Cisplatin + Gemcitabine, Carbolastin + Paclitaxel) | 305 | 44.8% (95% CI 36.8–53.0%) vs. 27.8% (95% CI 20.8–35.7%) | Median OS not met. HR 0.60, 95% CI 0.41–0.89, p = 0.005 | 2016, Reck et al. [60] |
| NR | 30 m (95% CI 18.3–NR) vs. 14.2 m (95% CI 9.8–19.0 m) (HR 0.63, 95% CI 0.47–0.86, p = 0.002) | 2019, Reck et al. [61] | ||||
| ECOG 0–1 | 65 vs. 63.5 | Cisplatin/Carboplatin + Pemetrexed + Pembrolizumab vs. Cisplatin/Carboplatin + Pemetrexed + Placebo | 616 | 47.6% (95% CI 42.6–52.5%) vs. 18.9% (95% CI 13.8–25.0%) (p < 0.001) | Immature result vs. 11.3 m (95% CI 8.7–15.1%) (HR 0.49, 95% CI 0.38–0.64, p ≤ 0.001) | 2018, Gandhi et al. [62] |
| 197 (4 + 193)/150/37; 48% (95% CI 43.1–53.0%) vs. 40 (1 + 39)/105/36; 19.4% (95% CI 14.2–25.5%) | Median study follow-up = 23.1 m 22 m (95% CI 19.5–25.2 m) vs. 10.7 m (95% CI 8.7–13.6 m) (HR 0.56, 95% CI 0.45–0.70 | 2020, Gadgeel et al. [63] | ||||
| ECOG 0–1 | 63 vs. 65 | Nivolumab vs. Platinum doublet chemotherapy (Pemetrexed + Carboplatin, Pemetrexed + Cisplatin, Gemcitabine + Carboplatin, Gemcitabine + Cisplatin, Paclitaxel + Carboplatin) | 541 | 55 (4 + 51)/81/58; 26% (95% CI 20–33%) vs. 71 (1 + 70)/100/21; 33% (95% CI 27–40%) (OR 0.70, 95% CI 0.46–1.06) | 14.4 m (95% CI 11.7–17.4 m) vs. 13.2 m (95% CI 10.7–17.1 m) (HR 1.02, 95% CI 0.80–1.30 | 2017, Carbone et al. [64] |
| ECOG 0–1 | 66 vs. 65 vs. 65 | Atezolizumab + Carboplatin + Paclitaxel (ACP) vs. Atezolizumab + Carboplatin + Nab-paclitaxel (ACnP) vs. Carboplatin + nab-paclitaxel (CnP) | 1021 | ACnP vs. CnP: 170 (8 + 162)/107/25; 49.7% (95% CI 44.3–55.1%) vs. 139 (5 + 134)/120/48; 41.0% (95% CI 35.7–46.5%) | ACnP vs. CnP: 14.2 m (95% CI 12.3–16.8 m) vs. 13.5 m (95% CI 12.2–15.1 m) (HR 0.88, 95% CI 0.73–1.05, p = 0.1581) | 2020, Jotte et al. [65] |
| ECOG 0–1 | 64 vs. 65 | Atezolizumab vs. Cisplatin/Carboplatin + Pemetrexed/Gemcitabine | 572 | High PD-L1 expression: 38.3% (95% CI 29.1–48.2%) vs. 28.6% (95% CI 19.9–38.6%) High or intermediate PF-L1 expression: 30.7% (95% CI 23.8–38.3%) vs. 32.1% (95% CI 25.0–39.9%) Any PD-L1 expression: 29.2% (95% Ci 24.0–35.0%) vs. 31.8% (95% CI 26.3–37.6%) | High PD-L1 expression: 20.2 m vs. 13.1 m (HR 0.59, 95% CI 0.40–0.89, p = 0.01) High or intermediate PF-L1 expression: 18.2 m vs. 14.9 m (HR 0.72, 95% CI 0.52–0.99, p = 0.044) Any PD-L1 expression: 17.5 m vs. 14.1 m (HR 0.83, 95% CI 0.65–1.07) | 2020, Giaccone et al. [66] |
| ECOG 0–1 | 65 | Pembrolizumab + Carboplatin + Paclitaxel/Nab-paclitaxel vs. Placebo + Carboplatin + Paclitaxel/Nab-paclitaxel | 559 | 161; 57.9% (95% CI 51.9–63.8%) vs. 108; 38.4% (95% CI 32.7–44.4%) | 15.9 m (95% CI 13.2-NR) vs. 11.3 m (95% CI 9.5–14.8 m) (HR 0.64, 95% CI 0.49–0.85, p < 0.001) | 2018, Paz-Ares et al. [67] |
| ECOG 0–1 | 63 vs. 63 | Atezolizumab + Bevacizumab + Carboplatin + Paclitaxel (ABCP) vs. Bevacizumab + Carboplatin + Paclitaxel (BCP) | 1202 | 224 (13 + 211)/77/18; 63.5% (95% CI 58.2–68.5%) vs. 159 (4 + 155)/115/27; 48.0% (95% CI 42.5–53.6%) | 19.2 m vs. 14.7 m (HR 0.78, 95% CI 0.64–0.96, p = 0.02) | 2018, Socinski et al. [68] |
| PS ** | Median Age | Regimen | Patients (n) | Objective Response (CR + PR)/SD/PD; ORR (%) * | Median OS/MST *** | Study |
|---|---|---|---|---|---|---|
| ECOG 0–1 | 63 | Erlotinib + Chemotherapy (Carboplatin + Paclitaxel) vs. Placebo + Chemotherapy (Carboplatin + Paclitaxel) | 1079 | 21.5% vs. 19.3% (p = 0.36) | 10.6 m vs. 10.5 m (HR 0.995, 95% CI 0.86–1.16, p = 0.95) | 2005, Herbst et al. [69] |
| WHO 0–2 | 62 vs. 61 vs. 63 | Chemotherapy (Paclitaxel + Carboplatin) + 500 mg/d Gefitinib vs. Chemotherapy + 250 mg/d Gefitinib vs. Chemotherapy + Placebo | 1037 | CR rate; ORR: 0.6%; 30% vs. 2.6%; 30.4% vs. 1.2%; 28.7% (No statistically significant difference) | 8.7 m vs. 9.8 m vs. 9.9 m (p = 0.6385) | 2004, Herbst et al. [70] |
| ECOG 0–2 | NR | Erlotinib vs. Chemotherapy (Cisplatin/Carboplatin + Docetaxel/Gemcitabine) | 173 | 49 (2 + 47); 64% vs. 13 (0 + 13); 18% (OR 7.5, 95% CI 3.6–15.6, p < 0.0001) | 19.3 m (95% CI 14.7–26.8 m) vs. 19.5 m (95% CI 16.1 m–NR) (HR 1.04, 95% CI 0.65–1.68, p = 0.87) | 2012, Rosell et al. [71] |
| ECOG 0–2 | 63.9 vs. 62.6 | Gefitinib vs. Carboplatin + Paclitaxel | 230 | 73.7% vs. 30.7% (p < 0.001) | 30.5 m vs. 23.6 m (p = 0.31) | 2010, Maemondo et al. [72] |
| ECOG 0–1 | 58 | Afatinib vs. Gemcitabine + Cisplatin | 364 | 162; 66.9% vs. 28; 23% (OR 7.28, 95% CI 4.36–12.18, p < 0.0001) | NR | 2014, Wu et al. [73] |
| 23.1 m (95% CI 20.4–27.3 m) vs. 23.5 m (95% CI 18.0–25.6 m) (HR 0.93, 95% CI 0.72–1.22, p = 0.61 | 2015, Yang et al. [74] | |||||
| ECOG 0–1 | 61.5 vs. 61.0 | Afatinib vs. Cisplatin + Pemetrexed | 345 | 56% vs. 23% (p = 0.001) | NR | 2013, Sequist et al. [75] |
| 28.2 m (95% CI 24.6–33.6 m) vs. 28.2 m (95% CI 20.7–33.2 m) (HR 0.88, 95% CI 0.66–1.17, p = 0.39) | 2015, Yang et al. [74] | |||||
| WHO PS 0–1 | NR | Osimertinib vs. Gefitinib/Erlotinib | 556 | 80% (95% CI 75–85%) vs. 76% (95% CI 70–81%) | NR | 2017, Ramalingam et al. [76] |
| 38.6 m (95% CI 34.5–41.8 m) vs. 31.8 m (95% CI 26.6–36.0 m) (HR 0.799, 95% CI 0.641–0.997, p = 0.0462) | 2019, Ramalingam et al. [77] | |||||
| WHO PS 0–1 | 64 | Gefitinib vs. Cisplatin + Docetaxel | 106 | 36; 62.1% vs. 19; 32.2% (p < 0.0001) | NR | 2010, Mitsudomi et al. [78] |
| 34.9 m (95% CI 26.1–39.5 m) vs. 37.3 m (95% CI 31.2–45.5 m) (HR 1.252, 95% CI 0.883–1.775, p < 0.2070) | 2014, Yoshioka et al. [79] |
| PS ** | Median Age | Regimen | Patients (n) | Objective Response (CR + PR)/SD/PD; ORR (%) * | Median OS/MST *** | Study |
|---|---|---|---|---|---|---|
| ECOG PS 0–2 | 52 vs. 54 | Crizotinib vs. Chemotherapy (Pemetrexed + Cisplatin/Carboplatin) | 343 | 128 (3 + 125)/29/8; 74% (95% CI 67–81%) vs. 77 (2 + 75)/63/21; 45% (95% CI 37–53%) (p < 0.001) | HR 0.82 (95% CI 0.54–1.26, p = 0.36) (Immature results) | 2014, Solomon et al. [81] |
| NR (95% CI 45.8 m–NR) vs. 47.5 m (95% CI 32.2–NR) (HR 0.760, 95% CI 0.548–1.053, p = 0.0978) | 2018, Solomon et al. [82] | |||||
| ECOG PS 0–2 | 48 vs. 50 | Crizotinib vs. Pemetrexed + Cisplatin/Carboplatin | 207 | 91 (3 + 88); 87.5% (95% CI 79.6–93.2%) vs. 47 (0 + 47); 45.6% (95% CI 35.8–55.7%) (p < 0.001) | 28.5 m (95% CI 26.4 m–NR) vs. 27.7 m (95% CI 23.9 m–NR) (HR 0.897, 95% CI 0.556–1.445, p = 0.327) | 2018, Wu et al. [80] |
| ECOG PS 0–2 | 53.8 vs. 56.3 | Crizotinib vs. Alectinib | 303 | 114 (2 + 112)/24/NR; 75.5% (95% CI 67.8–82.1%) vs. 126 (6 + 120)/9/NR; 82.9% (95% CI 76.0–88.5%) (p = 0.09) | HR = 0.76, 95% CI 0.48–1.20, p = 0.24 | 2017, Peters et al. [83] |
| ECOG PS 0–2 | 59.1 vs. 55.6 | Lorlatinib vs. Crizotinib | 296 | 113 (4 + 109)/19/10; 76% (95% CI 68–83%) vs. 85 (0 + 85)/41/7; 58% (95% CI 49–66%) (OR 2.25, 95% CI 1.35–3.89) | HR = 0.72, 95% CI 0.41–1.25 | 2020, Shaw et al. [84] |
| PS ** | Median Age | Regimen | Patients (n) | Objective Response (CR+PR)/SD/PD; ORR (%) * | Median OS/MST *** | Study |
|---|---|---|---|---|---|---|
| ECOG 0–2 | 62 | Crizotinib | 93 | ROS1 translocation cohort: 17; 47.2% | ROS translocation cohort: 17.2 m (95% CI 6.8–32.8 m) | 2019, Moro-Sibilot et al. [86] |
| ECOG 0–1 | NR | Crizotinib | 53 | 38 (6 + 32)/10/3; 72% (95% CI 58–83%) | 51.4 m (95% CI 29.3 m–NR) | 2019, Shaw et al. [85] |
| ECOG 0–2 | 66 | Dabrafenib | 84 | ≥second-line patients: 21(NR)/13/23; 33% (95% CI 23–45%) | 12.7 m (95% CI 7.3–16.9 m) | 2016, Planchard et al. [87] |
| ECOG 0–2 | BRAFV600 = 68 BRAFNon-V600 = 65 | Vemurafenib | 118 | BRAFV600: 43; 44.8% BRAFNon-V600: No tumor response observed | BRAFV600: 10 m (95% CI 6.8–15.7 m) BRAFNon-V600: 5.2 m (95% CI 2.8–18.7 m) | 2020, Mazieres et al. [88] |
| ECOG 0–2 | 64 | Debrafenib + Trametinib | 59 | 36 (0 + 36)/4/8; 63.2% (95% CI 49.3–75.6%) | NR | 2016, Planchard et al. [89] |
| 18.2 m (95% CI 14.3 m–NR) | 2017, Planchard et al. [90] | |||||
| NR | 57 | Pyrotinib | 60 | 31.7% | NR | 2019, Gao et al. [91] |
| NR | 42 | Trastuzumab deruxtecan | 42 | 41.9% | NR | 2020, Smit et al. [92] |
| NR | 60 | Poziotinib | 90 | 27.8% | NR | 2020, Socinski et al. [93] |
| Score | Definition |
|---|---|
| 0 | Fully active without any restrictions to daily activities. |
| 1 | Able to ambulate and carry out light works only. |
| 2 | Able to ambulate >50% of waking hours and perform self-care. |
| 3 | Confined to bed/chair >50% of waking hours and limited self-care. |
| 4 | Total confinement to bed/chair and unable to perform any self-care. |
| Drug | Dosage as Monotherapy | Dosage in Combination Therapy |
|---|---|---|
| Cisplatin | 100 mg/m2 | 50–120 mg/m2 |
| Carboplatin * | NR | AUC 5 or 6 mg/(mL × min) |
| Nedaplatin | NR | 80–100 mg/m2 |
| Gemcitabine | NR | 1000–1250 mg/m2 |
| Docetaxel | 75 mg/m2 | 60–100 mg/m2 |
| Paclitaxel | NR | 135–225 mg/m2 |
| Vinorelbine | 30 mg/m2 | 25 or 30 mg/m2 |
| Pemetrexed | 500 mg/m2 | 500 mg/m2 |
| Bevacizumab | NR | 15 or 7.5 mg/kg |
| Pembrolizumab | 200 mg | 200 mg |
| Atezolizumab | 1200 mg | 1200 mg |
| Gefitinib | 250 mg | 250 or 500 mg |
| Erlotinib | 150 mg | 150 mg |
| Afatinib | 40 mg | NR |
| Osimertinib | 80 mg | NR |
| Crizotinib | 250 mg | NR |
| Types of Regimen | Median Cycles of Treatment Administered/Median Duration of Treatment |
|---|---|
| Platinum-based doublet 1 | 4 cycles |
| Platinum-based triplet 2 | 5–7 cycles |
| PD-1/PD-L1 inhibitors 3 | 8–10 cycles |
| EGFR TK inhibitors 4 | 3–13 m |
| Crizotinib | 10.7–15.6 m |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwan, T.Y.; Chowdhury, E.H. Clinical Outcomes of Chemotherapeutic Molecules as Single and Multiple Agents in Advanced Non-Small-Cell Lung Carcinoma (NSCLC) Patients. Medicina 2021, 57, 1252. https://doi.org/10.3390/medicina57111252
Kwan TY, Chowdhury EH. Clinical Outcomes of Chemotherapeutic Molecules as Single and Multiple Agents in Advanced Non-Small-Cell Lung Carcinoma (NSCLC) Patients. Medicina. 2021; 57(11):1252. https://doi.org/10.3390/medicina57111252
Chicago/Turabian StyleKwan, Ting Yoon, and Ezharul Hoque Chowdhury. 2021. "Clinical Outcomes of Chemotherapeutic Molecules as Single and Multiple Agents in Advanced Non-Small-Cell Lung Carcinoma (NSCLC) Patients" Medicina 57, no. 11: 1252. https://doi.org/10.3390/medicina57111252
APA StyleKwan, T. Y., & Chowdhury, E. H. (2021). Clinical Outcomes of Chemotherapeutic Molecules as Single and Multiple Agents in Advanced Non-Small-Cell Lung Carcinoma (NSCLC) Patients. Medicina, 57(11), 1252. https://doi.org/10.3390/medicina57111252





