Are Physical Therapeutics Important for Stroke Patients to Recover Their Cardiorespiratory Fitness?
Abstract
:1. Introduction
2. Materials and Methods
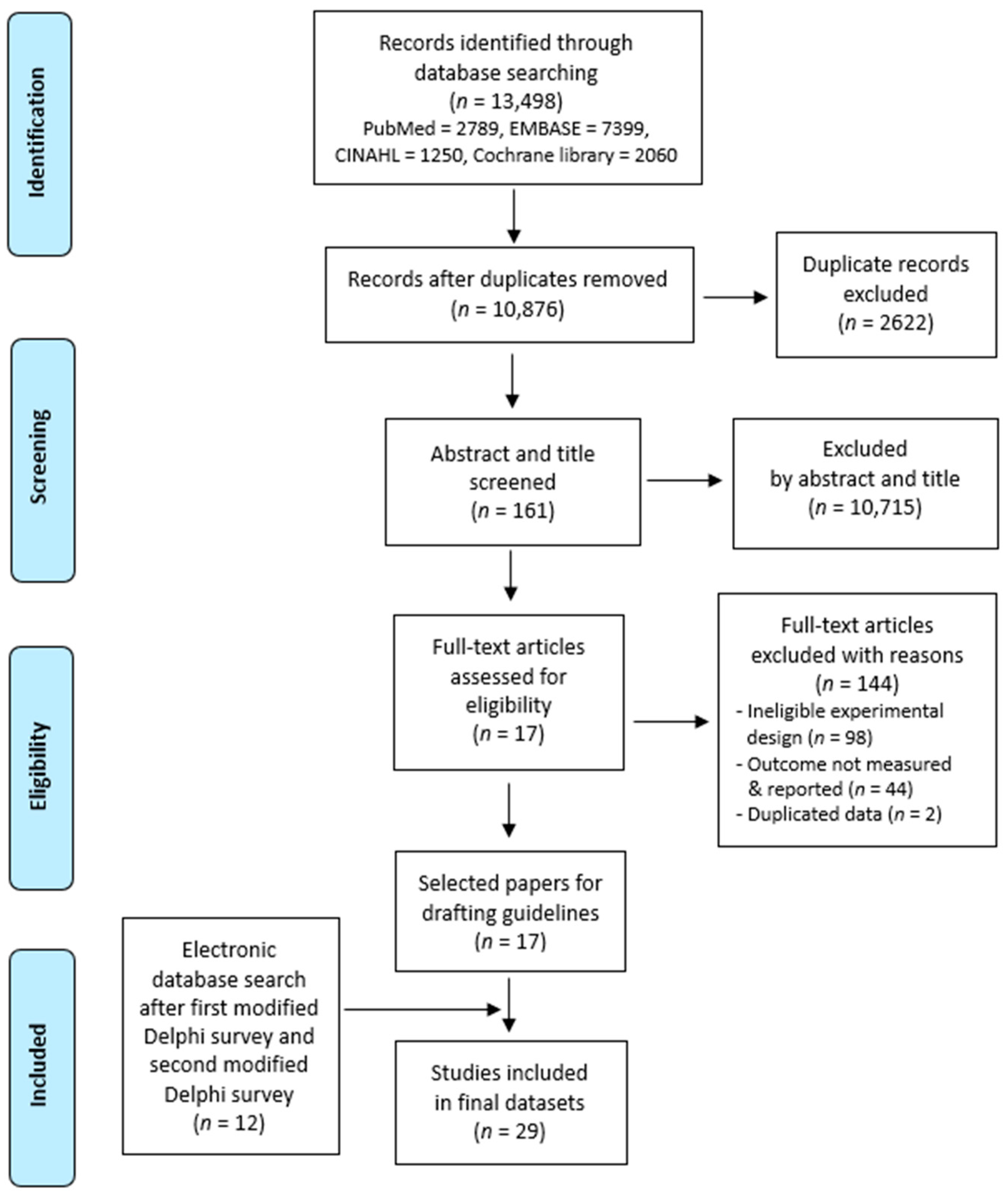
2.1. Literature Review and Study Selection
2.2. Modified Delphi Methodology
2.3. Principal Component Analysis
3. Results
3.1. Data Extraction Criteria
3.2. The Delphi Process
3.3. Deriving Final Evaluation Items
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Number | Intervention | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| 1 | Air stacking exercise | |||||
| 2 | Manually assisted cough | |||||
| 3 | Mechanical insufflator-exsufflator | |||||
| 4 | Noninvasive intermittent positive pressure ventilation | |||||
| 5 | Chest expansion resistance exercise | |||||
| 6 | Core exercise combined with abdominal breathing | |||||
| 7 | Diagonal pattern gymnastics motion with sitting | |||||
| 8 | Treadmill exercise | |||||
| 9 | High-intensity interval training (HIIT) | |||||
| 10 | Aquatic treadmill exercise | |||||
| 11 | Feedback controlled robotics assisted treadmill exercise | |||||
| 12 | Circuit aerobic exercise |
| Main Category | Number | Subcategory | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| Airway expansion and ventilation | 1 | Air stacking exercise or manual hyperinflation | |||||
| 2 | Manually assisted cough | ||||||
| 3 | Mechanical insufflator-exsufflator | ||||||
| 4 | Noninvasive intermittent positive pressure ventilation | ||||||
| 5 | Segmental breathing | ||||||
| 6 | Chest expansion exercise | ||||||
| 7 | Cervical and thoracic mobilization | ||||||
| 8 | Active assisted stretching exercise: four sections of the neck, upper thoracic, pectoralis major, and lateral chest | ||||||
| Strength training for respiratory rehabilitation | 9 | Core exercise combined with abdominal breathing | |||||
| 10 | Inspiratory muscle training (IMT) | ||||||
| Strength training for cardiac rehabilitation | 11 | Resistance training | |||||
| Cardiopulmonary endurance | 12 | L/E ergometer exercise | |||||
| 13 | Treadmill exercise | ||||||
| 14 | Aerobic exercise: principles of FITT | ||||||
| Education | 15 | Caregiver education (aerobic exercise and self-assisted coughing) |
References
- Imboden, M.T.; Harber, M.P.; Whaley, M.H.; Finch, W.H.; Bishop, D.L.; Kaminsky, L.A. Cardiorespiratory fitness and mortality in healthy men and women. J. Am. Coll. Cardiol. 2018, 72, 2283–2292. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.W.; Kim, S.H.; Kang, S.H.; Kim, H.J.; Yoon, C.H.; Youn, T.J.; Chae, I.H. Mortality reduction with physical activity in Patients with and without cardiovascular disease. Eur. Heart J. 2019, 40, 3547–3555. [Google Scholar] [CrossRef] [PubMed]
- Galloway, M.; Marsden, D.L.; Callister, R.; Erickson, K.I.; Nilsson, M.; English, C. What is the dose-response relationship between exercise and cardiorespiratory fitness after stroke? A systematic review. Phys. Ther. 2019, 99, 821–832. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Donnell, M.J.; Xavier, D.; Liu, L.; Zhang, H.; Chin, S.L.; Rao-Melacini, P.; Rangarajan, S.; Islam, S.; Pais, P.; McQueen, M.J.; et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): A case-control study. Lancet 2010, 376, 112–123. [Google Scholar] [CrossRef]
- Jaul, E.; Barron, J.; Rosenzweig, J.P.; Menczel, J. An overview of co-morbidities and the development of pressure ulcers among older adults. BMC Geriatr. 2018, 18, 305. [Google Scholar] [CrossRef]
- Billinger, S.A.; Kluding, P.M. Use of doppler ultrasound to assess femoral artery adaptations in the hemiparetic limb in people with stroke. Cerebrovasc. Dis. 2009, 27, 552–558. [Google Scholar] [CrossRef]
- MacKay-Lyons, M.J.; Macko, R.; Howlett, J. Cardiovascular fitness and adaptations to aerobic training after stroke. Physiother. Can. 2006, 58, 103–113. [Google Scholar] [CrossRef]
- Lee, J.; Stone, A.J. Combined aerobic and resistance training for cardiorespiratory fitness, muscle strength, and walking capacity after stroke: A systematic review and meta-analysis. J. Stroke Cereb. Dis. 2020, 29, 104498. [Google Scholar] [CrossRef] [Green Version]
- Saunders, D.H.; Sanderson, M.; Hayes, S.; Johnson, L.; Kramer, S.; Carter, D.D.; Jarvis, H.; Brazzelli, M.; Mead, G.E. Physical fitness training for stroke patients. Cochrane Database Syst. Rev. 2020, 3, CD003316. [Google Scholar] [CrossRef] [Green Version]
- Lanini, B.; Bianchi, R.; Romagnoli, I.; Coli, C.; Binazzi, B.; Gigliotti, F.; Pizzi, A.; Grippo, A.; Scano, G. Chest wall kinematics in patients with hemiplegia. Am. J. Respir. Crit. Care Med. 2003, 168, 109–113. [Google Scholar] [CrossRef]
- Berlowitz, D.J.; Wadsworth, B.; Ross, J. Respiratory problems and management in people with spinal cord injury. Breathe 2016, 12, 328–340. [Google Scholar] [CrossRef] [Green Version]
- Padkao, T.; Boonla, O. Relationships between respiratory muscle strength, chest wall expansion, and functional capacity in healthy nonsmokers. J. Exerc. Rehabil. 2020, 16, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Oyake, K.; Baba, Y.; Ito, N.; Suda, Y.; Murayama, J.; Mochida, A.; Kondo, K.; Otaka, Y.; Momose, K. Cardiorespiratory factors related to the increase in oxygen consumption during exercise in individuals with stroke. PLoS ONE 2019, 14, e0217453. [Google Scholar] [CrossRef]
- Girard, V.; Bellavance-Tremblay, H.; Gaudet-Drouin, G.; Lessard, G.; Dupont, M.; Gagnon, M.A.; Ngueleu, A.M.; Mandigout, S.; Batcho, C.S. Cardiorespiratory strain during stroke rehabilitation: Are patients trained enough? a systematic review. Ann. Phys. Rehabil. Med. 2021, 64, 101443. [Google Scholar] [CrossRef] [PubMed]
- Brooks, D.; Tang, A.; Sibley, K.M.; McIlroy, W.E. Profile of patients at admission into an inpatient stroke rehabilitation programme: Cardiorespiratory fitness and functional characteristics. Physiother. Can. 2008, 60, 171–179. [Google Scholar] [CrossRef] [Green Version]
- Ramas, J.; Courbon, A.; Roche, F.; Bethoux, F.; Calmels, P. Effect of training programs and exercise in adult stroke patients: Literature review. Ann. Readapt. Med. Phys. 2007, 50, 438–444. [Google Scholar] [CrossRef] [PubMed]
- Tang, A.; Sibley, K.M.; Thomas, S.G.; McIlroy, W.E.; Brooks, D. Maximal exercise test results in subacute stroke. Arch. Phys. Med. Rehabil. 2006, 87, 1100–1105. [Google Scholar] [CrossRef] [PubMed]
- Teixeira-Salmela, L.F.; Parreira, V.F.; Britto, R.R.; Brant, T.C.; Inácio, E.P.; Alcântara, T.O.; Carvalho, I.F. Respiratory pressures and thoracoabdominal motion in community-dwelling chronic stroke survivors. Arch. Phys. Med. Rehabil. 2005, 86, 1974–1978. [Google Scholar] [CrossRef]
- Tang, A.; Sibley, K.M.; Thomas, S.G.; Bayley, M.T.; Richardson, D.; McIlroy, W.E.; Brooks, D. Effects of an aerobic exercise program on aerobic capacity, spatiotemporal gait parameters, and functional capacity in subacute stroke. Neurorehabil. Neural Repair. 2009, 23, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Billinger, S.A.; Gajewski, B.J.; Guo, L.X.; Kluding, P.M. Single limb exercise induces femoral artery remodeling and improves blood flow in the hemiparetic leg poststroke. Stroke 2009, 40, 3086–3090. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stuart, M.; Benvenuti, F.; Macko, R.; Taviani, A.; Segenni, L.; Mayer, F.; Sorkin, J.D.; Stanhope, S.J.; Macellari, V.; Weinrich, M. Community-based adaptive physical activity program for chronic stroke: Feasibility, safety, and efficacy of the Empoli model. Neurorehabil. Neural Repair. 2009, 23, 726–734. [Google Scholar] [CrossRef]
- Tsuji, T.; Liu, M.; Hase, K.; Masakado, Y.; Takahashi, H.; Hara, Y.; Chino, N. Physical fitness in persons with hemiparetic stroke: Its structure and longitudinal changes during an inpatient rehabilitation programme. Clin. Rehabil. 2004, 18, 450–460. [Google Scholar] [CrossRef]
- Thomas, G.D.; Segal, S.S. Neural control of muscle blood flow during exercise. J. Appl. Physiol. 2004, 97, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Pérez-de la Cruz, S. Comparison between three therapeutic options for the treatment of balance and gait in stroke: A randomized controlled trial. Int. J. Environ. Res. Public Health 2021, 18, 426. [Google Scholar] [CrossRef]
- Jung, K.M.; Joo, M.C.; Jung, Y.J.; Jang, W.N. The effects of the three-dimensional active trunk training exercise on trunk control ability, trunk muscle strength, and balance ability in sub-acute stroke patients: A randomized controlled pilot study. Technol. Health Care 2021, 29, 213–222. [Google Scholar] [CrossRef]
- Alessandro, L.; Olmos, L.E.; Bonamico, L.; Muzio, D.M.; Ahumada, M.H.; Russo, M.J.; Allegri, R.F.; Gianella, M.G.; Campora, H.; Delorme, R.; et al. Multidisciplinary rehabilitation for adult patients with stroke. Medicina (B. Aires) 2020, 80, 54–68. [Google Scholar] [PubMed]
- Gustavsson, M.; Ytterberg, C.; Guidetti, S. Exploring future possibilities of using information and communication technology in multidisciplinary rehabilitation after stroke—A grounded theory study. Scand. J. Occup. Ther. 2020, 27, 223–230. [Google Scholar] [CrossRef]
- Pogrebnoy, D.; Dennett, A. Exercise programs delivered according to guidelines improve mobility in people with stroke: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2020, 101, 154–165. [Google Scholar] [CrossRef] [Green Version]
- Chinembiri, B.; Ming, Z.; Kai, S.; Xiu Fang, Z.; Wei, C. The fourier M2 robotic machine combined with occupational therapy on post-stroke upper limb function and independence-related quality of life: A randomized clinical trial. Top Stroke Rehabil. 2021, 28, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Chiaramonte, R.; Vecchio, M. Dysarthria and stroke. The effectiveness of speech rehabilitation. a systematic review and meta-analysis of the studies. Eur. J. Phys. Rehabil. Med. 2021, 57, 24–43. [Google Scholar] [CrossRef]
- Stockley, R.C.; Jarvis, K.; Boland, P.; Clegg, A.J. Systematic review and meta-analysis of the effectiveness of mental practice for the upper limb after stroke: Imagined or real benefit? Arch. Phys. Med. Rehabil. 2021, 102, 1011–1027. [Google Scholar] [CrossRef] [PubMed]
- Gomes-Neto, M.; Saquetto, M.B.; Silva, C.M.; Carvalho, V.O.; Ribeiro, N.; Conceição, C.S. Effects of respiratory muscle training on respiratory function, respiratory muscle strength, and exercise tolerance in patients poststroke: A systematic review with meta-analysis. Arch. Phys. Med. Rehabil. 2016, 97, 1994–2001. [Google Scholar] [CrossRef] [PubMed]
- Hegland, K.W.; Davenport, P.W.; Brandimore, A.E.; Singletary, F.F.; Troche, M.S. Rehabilitation of swallowing and cough functions following stroke: An expiratory muscle strength training trial. Arch. Phys. Med. Rehabil. 2016, 97, 1345–1351. [Google Scholar] [CrossRef]
- Menezes, K.K.P.; Nascimento, L.R.; Polese, J.C.; Ada, L.; Teixeira-Salmela, L.F. Effect of high-intensity home-based respiratory muscle training on strength of respiratory muscles following a stroke: A protocol for a randomized controlled trial. Braz. J. Phys. Ther. 2017, 21, 372–377. [Google Scholar] [CrossRef]
- Messaggi-Sartor, M.; Guillen-Solà, A.; Depolo, M.; Duarte, E.; Rodríguez, D.A.; Barrera, M.C.; Barreiro, E.; Escalada, F.; Orozco-Levi, M.; Marco, E. Inspiratory and expiratory muscle training in subacute stroke: A randomized clinical trial. Neurology 2015, 85, 564–572. [Google Scholar] [CrossRef] [PubMed]
- Modai, G.; Sharon, B.; Bar-Haim, S.; Hutzler, Y. Stair climbing test post-stroke: Feasibility, convergent validity and metabolic, cardiac, and respiratory responses. Top. Stroke Rehabil. 2015, 22, 281–288. [Google Scholar] [CrossRef]
- Parreiras de Menezes, K.K.; Nascimento, L.R.; Ada, L.; Avelino, P.R.; Polese, J.C.; Mota Alvarenga, M.T.; Barbosa, M.H.; Teixeira-Salmela, L.F. High-intensity respiratory muscle training improves strength and dyspnea poststroke: A double-blind randomized trial. Arch. Phys. Med. Rehabil. 2019, 100, 205–212. [Google Scholar] [CrossRef]
- Degeling, C.J.; Johnson, J.; Ward, M.; Wilson, A.; Gilbert, G. A Delphi survey and analysis of expert perspectives on one health in Australia. Ecohealth 2017, 14, 783–792. [Google Scholar] [CrossRef] [Green Version]
- Boulkedid, R.; Abdoul, H.; Loustau, M.; Sibony, O.; Alberti, C. Using and reporting the Delphi method for selecting healthcare quality indicators: A systematic review. PLoS ONE 2011, 6, e20476. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Shah, R.D.; Rasinski, K.A.; Alexander, G.C. The influence of surrogate decision makers on clinical decision making for critically Ill adults. J. Intensive Care Med. 2015, 30, 278–285. [Google Scholar] [CrossRef]
- Tigelaar, D.E.H.; Dolmans, D.H.J.M.; Wolfhagen, I.H.A.P.; van der Vleuten, C.P.M. The development and validation of a framework for teaching competencies in higher education. Higher Educ. 2004, 48, 253–268. [Google Scholar] [CrossRef]
- Murry, J.W.J.; Hammons, J.O. Delphi: A versatile methodology for conducting qualitative research. Rev. High. Educ. 1995, 18, 423–436. [Google Scholar] [CrossRef]
- Balady, G.J.; Williams, M.A.; Ades, P.A.; Bittner, V.; Comoss, P.; Foody, J.M.; Franklin, B.; Sanderson, B.; Southard, D. Core components of cardiac rehabilitation/ secondary prevention programs: 2007 update. Circulation 2007, 115, 2675–2682. [Google Scholar] [CrossRef] [PubMed]
- Spruit, M.A.; Singh, S.J.; Garvey, C.; ZuWallack, R.; Nici, L.; Rochester, C.; Hill, K.; Holland, A.E.; Lareau, S.C.; Man, W.D.; et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2013, 188, e13–e64. [Google Scholar] [CrossRef]
- Billinger, S.A.; Boyne, P.; Coughenour, E.; Dunning, K.; Mattlage, A. Does aerobic exercise and the FITT principle fit into stroke recovery? Curr. Neurol. Neurosci. Rep. 2015, 15, 519. [Google Scholar] [CrossRef]
- Ofori, E.K.; Frimpong, E.; Ademiluyi, A.; Olawale, O.A. Ergometer cycling improves the ambulatory function and cardiovascular fitness of stroke patient-a randomized controlled trial. J. Phys. Ther. Sci. 2019, 31, 211–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jang, S.H.; Bang, H.S. Effect of thoracic and cervical joint mobilization on pulmonary function in stroke patients. J. Phys. Sci. 2016, 28, 257–260. [Google Scholar] [CrossRef] [Green Version]
- Rattes, C.; Campos, S.L.; Morais, C.; Gonçalves, T.; Sayão, L.B.; Galindo-Filho, V.C.; Parreira, V.; Aliverti, A.; Dornelas de Andrade, A. Respiratory muscles stretching acutely increases expansion in hemiparetic chest wall. Respir. Physiol. Neurobiol. 2018, 254, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.E.; Lee, H.J.; Kim, M.K.; Lee, W.H. The improvement in respiratory function by inspiratory muscle training is due to structural muscle changes in patients with stroke: A randomized controlled pilot trial. Top. Stroke Rehabil. 2018, 25, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.B.; Kim, M.K.; Jeong, J.R.; Lee, W.H. Reliability of an electronic inspiratory loading device for assessing pulmonary function in post-stroke patients. Med. Sci. Monit. 2016, 22, 191–196. [Google Scholar] [CrossRef] [Green Version]
- Lund, C.; Dalgas, U.; Grønborg, T.K.; Andersen, H.; Severinsen, K.; Riemenschneider, M.; Overgaard, K. Balance and walking performance are improved after resistance and aerobic training in persons with chronic stroke. Disabil. Rehabil. 2018, 40, 2408–2415. [Google Scholar] [CrossRef]
- Pierson, L.M.; Herbert, W.G.; Norton, H.J.; Kiebzak, G.M.; Griffith, P.; Fedor, J.M.; Ramp, W.K.; Cook, J.W. Effects of combined aerobic and resistance training versus aerobic training alone in cardiac rehabilitation. J. Cardiopulm. Rehabil. 2001, 21, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Bibi, K.W.; Niederpruem, M.G. ACSM’s Certification Review, 4th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2010. [Google Scholar]
- Kang, D.; Park, J.; Jeong, I.; Eun, S.D. Comparing the effects of multicomponent exercise with or without power training on the cardiorespiratory fitness, physical function, and muscular strength of patients with stroke: A randomized controlled trial. J. Sports Med. Phys. Fitness 2021. [Google Scholar] [CrossRef]
- Luo, L.; Meng, H.; Wang, Z.; Zhu, S.; Yuan, S.; Wang, Y.; Wang, Q. Effect of high-intensity exercise on cardiorespiratory fitness in stroke survivors: A systematic review and meta-analysis. Ann. Phys. Rehabil. Med. 2020, 63, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Sutbeyaz, S.; Koseoglu, F.; Inan, L.; Coskun, O. Respiratory muscle training improves cardiopulmonary function and exercise tolerance in subjects with subacute stroke: A randomized controlled trial. Clin. Rehabil. 2010, 24, 240–250. [Google Scholar] [CrossRef]
| User Group | Field of Health Research | |
|---|---|---|
| Stroke | Cardiac rehabilitation | Exercise |
| Cerebrum | Respiratory therapy | Heart |
| Brain | Patient outcome assessment | Rehabilitation |
| Cardiorespiratory fitness | ||
| User Group | Field of Health Research | |
|---|---|---|
| Stroke patient | Cardiorespiratory fitness | Exercise |
| Cerebrovascular disease | Respiratory care | Heart rehabilitation |
| Brain | Breathing | Breathing exercise |
| Lung function test | Outcome assessment | |
| Checklist | Respiratory tract parameters | |
| Participants | Adult stroke patients aged > 18 years |
| Intervention | A single intervention (single intervention group) or a combination of two or more interventions (combination group) |
| Comparisons | Groups receiving no interventions for cardiorespiratory physiotherapy or those receiving typical physiotherapy without interventions |
| Outcomes | A single variable or two or more variables containing exercise interventions related to physiotherapy of cardiac and respiratory functions |
| Study design | Observational descriptive study, case-series, observational analytical study, consensus document, editorial, cross-sectional study, case-control study, cohort study, systematic literature reviews, systematic review, meta-analysis, randomized controlled trial (RCT), quasi-experimental design |
| Domain | No | Intervention Item | Mean | SD | CVR | Q1 | Median | Q3 | Stability | Convergence | Consensus |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Airway expansion and ventilation | 1 | Air stacking exercise or manual hyperinflation | 4.56 | 0.53 | 1.00 | 4.00 | 5.00 | 5.00 | 0.12 | 0.50 | 0.80 |
| 2 | Manually assisted cough | 4.89 | 0.33 | 1.00 | 5.00 | 5.00 | 5.00 | 0.07 | 0.00 | 1.00 | |
| 3 | Mechanical insufflator-exsufflator | 4.67 | 0.50 | 1.00 | 4.00 | 5.00 | 5.00 | 0.11 | 0.50 | 0.80 | |
| 4 | Noninvasive intermittent positive pressure ventilation | 4.56 | 0.53 | 1.00 | 4.00 | 5.00 | 5.00 | 0.12 | 0.50 | 0.80 | |
| 5 | Segmental breathing | 4.56 | 0.53 | 1.00 | 4.00 | 5.00 | 5.00 | 0.12 | 0.50 | 0.80 | |
| 6 | Chest expansion resistance exercise | 4.78 | 0.44 | 1.00 | 4.50 | 5.00 | 5.00 | 0.09 | 0.25 | 0.90 | |
| 7 | Cervical and thoracic mobilization | 4.78 | 0.44 | 1.00 | 4.50 | 5.00 | 5.00 | 0.09 | 0.25 | 0.90 | |
| 8 | Active assisted stretching exercise | 4.44 | 0.73 | 0.78 | 4.00 | 5.00 | 5.00 | 0.16 | 0.50 | 0.80 | |
| Strength training for respiratory rehabilitation | 9 | Core exercise combined with abdominal breathing | 4.56 | 0.53 | 1.00 | 4.00 | 5.00 | 5.00 | 0.12 | 0.50 | 0.80 |
| 10 | Inspiratory muscle training | 4.44 | 0.73 | 1.00 | 4.00 | 4.00 | 5.00 | 0.12 | 0.50 | 0.75 | |
| Strength training for cardiac rehabilitation | 11 | Resistance training | 4.44 | 0.73 | 0.78 | 4.00 | 5.00 | 5.00 | 0.16 | 0.50 | 0.80 |
| Cardiopulmonary endurance | 12 | L/E ergometer exercise | 4.67 | 0.50 | 1.00 | 4.00 | 5.00 | 5.00 | 0.11 | 0.50 | 0.80 |
| 13 | Treadmill exercise | 4.78 | 0.44 | 1.00 | 4.50 | 5.00 | 5.00 | 0.09 | 0.25 | 0.90 | |
| 14 | Aerobic exercise: principles of FITT | 4.89 | 0.33 | 1.00 | 5.00 | 5.00 | 5.00 | 0.07 | 0.00 | 1.00 | |
| Education | 15 | Caregiver education (Aerobic exercise and self-assisted coughing) | 4.89 | 0.33 | 1.00 | 5.00 | 5.00 | 5.00 | 0.07 | 0.00 | 1.00 |
| Intervention | Average | 4.66 | 0.23 | 0.97 | 4.30 | 4.93 | 5.00 | 0.11 | 0.35 | 0.86 | |
| Domain | No | Final Items |
|---|---|---|
| Airway expansion and ventilation | 1 | Air stacking exercise or manual hyperinflation |
| 2 | Manually assisted cough | |
| 3 | Mechanical insufflator-exsufflator | |
| 4 | Noninvasive intermittent positive pressure ventilation | |
| 5 | Segmental breathing | |
| 6 | Chest expansion exercise | |
| 7 | Cervical and thoracic mobilization | |
| 8 | Active assisted stretching exercise: four sections of neck, upper thoracic, pectoralis major, lateral chest | |
| Strength training for respiratory rehabilitation | 9 | Core exercise combined with abdominal breathing |
| 10 | Inspiratory muscle training | |
| Strength exercises for cardiac rehabilitation | 11 | Resistance training |
| Cardiopulmonary endurance | 12 | L/E ergometer exercise |
| 13 | Treadmill exercise | |
| 14 | Aerobic exercise: principles of FITT | |
| Education | 15 | Patient and protector education (aerobic exercise and self-assisted coughing) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, K.-B.; Cho, S.-H. Are Physical Therapeutics Important for Stroke Patients to Recover Their Cardiorespiratory Fitness? Medicina 2021, 57, 1182. https://doi.org/10.3390/medicina57111182
Choi K-B, Cho S-H. Are Physical Therapeutics Important for Stroke Patients to Recover Their Cardiorespiratory Fitness? Medicina. 2021; 57(11):1182. https://doi.org/10.3390/medicina57111182
Chicago/Turabian StyleChoi, Ki-Bok, and Sung-Hyoun Cho. 2021. "Are Physical Therapeutics Important for Stroke Patients to Recover Their Cardiorespiratory Fitness?" Medicina 57, no. 11: 1182. https://doi.org/10.3390/medicina57111182
APA StyleChoi, K.-B., & Cho, S.-H. (2021). Are Physical Therapeutics Important for Stroke Patients to Recover Their Cardiorespiratory Fitness? Medicina, 57(11), 1182. https://doi.org/10.3390/medicina57111182






