Ocular Decompression Retinopathy after Anterior Chamber Paracentesis for Neovascular Glaucoma
Abstract
:1. Introduction
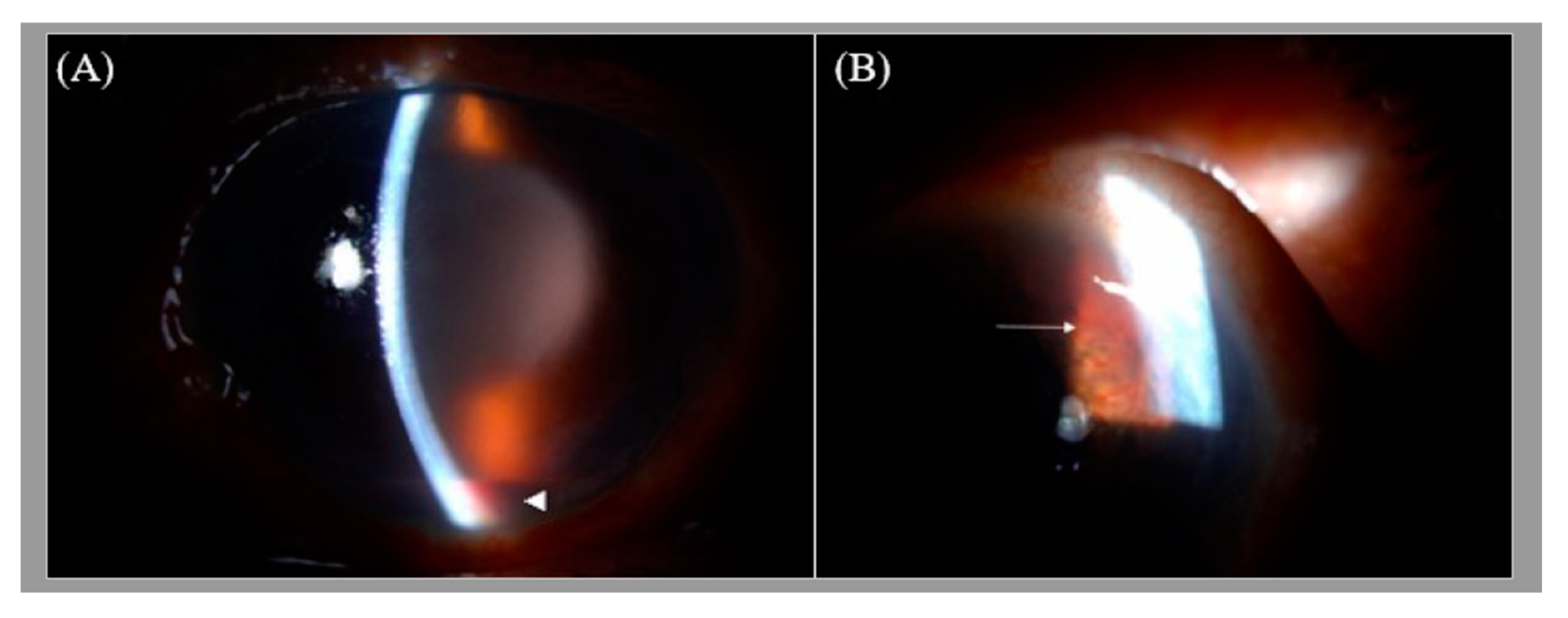
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Fechtner, R.D.; Minckler, D.; Weinreb, R.N.; Frangei, G.; Jampol, L.M. Complications of glaucoma surgery. Ocular decompression retinopathy. Arch. Ophthalmol. 1992, 110, 965–968. [Google Scholar] [CrossRef] [PubMed]
- Mukkamala, S.K.; Patel, A.; Dorairaj, S.; McGlynn, R.; Sidoti, P.A.; Weinreb, R.N.; Rusoff, J.; Rao, S.; Gentile, R.C. Ocular decompression retinopathy: A review. Surv. Ophthalmol. 2013, 58, 505–512. [Google Scholar] [CrossRef] [PubMed]
- Saricaoglu, M.S.; Kalayci, D.; Guven, D.; Karakurt, A.; Hasiripi, H. Decompression retinopathy and possible risk factors. Acta Ophthalmol. 2009, 87, 94–95. [Google Scholar] [CrossRef] [PubMed]
- Arévalo, J.F.; Mendoza, A.J.; Fernández, C.F.; Yépez, J.B.; Krivoy, D.; Millán, F.A. Decompression retinopathy after intraocular surgery. Arch. Soc. Esp. Oftalmol. 2007, 82, 629–634. [Google Scholar] [PubMed] [Green Version]
- Jamie, P.; David, F. Immediate manifestation of ocular decompression retinopathy following anterior chamber paracentesis. Case Rep. Ophthalmol. 2019, 10, 287–291. [Google Scholar]
- Sang, J.L.; Jung, J.L.; Shin, D.K. Multiple retinal hemorrhage following anterior chamber paracentesis in uveitic glaucoma. KJO 2006, 20, 128–130. [Google Scholar]
- Rao, S.K.; Greenberg, P.B.; Macintyre, R.B.L.; Ducharme, J.F. Ocular decompression retinopathy after anterior chamber paracentesis for uveitic glaucoma. Retina 2009, 29, 280–281. [Google Scholar] [CrossRef] [PubMed]
- Semra, K.; Defne, K.; Zeynep, D.; Ayten, B. Ocular decompression retinopathy following anterior chamber paracentesis in a patient with neovascular glaucoma associated with diabetic retinopathy. Research 2014, 1, 975. [Google Scholar]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, Y.-E.; Hsu, C.-R. Ocular Decompression Retinopathy after Anterior Chamber Paracentesis for Neovascular Glaucoma. Medicina 2021, 57, 1038. https://doi.org/10.3390/medicina57101038
Tsai Y-E, Hsu C-R. Ocular Decompression Retinopathy after Anterior Chamber Paracentesis for Neovascular Glaucoma. Medicina. 2021; 57(10):1038. https://doi.org/10.3390/medicina57101038
Chicago/Turabian StyleTsai, Yung-En, and Cherng-Ru Hsu. 2021. "Ocular Decompression Retinopathy after Anterior Chamber Paracentesis for Neovascular Glaucoma" Medicina 57, no. 10: 1038. https://doi.org/10.3390/medicina57101038
APA StyleTsai, Y.-E., & Hsu, C.-R. (2021). Ocular Decompression Retinopathy after Anterior Chamber Paracentesis for Neovascular Glaucoma. Medicina, 57(10), 1038. https://doi.org/10.3390/medicina57101038





