A Six-Year Prospective Comparative Study of Wide and Standard Diameter Implants in the Maxillary and Mandibular Posterior Area
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Study Population
2.2. Surgical Methods
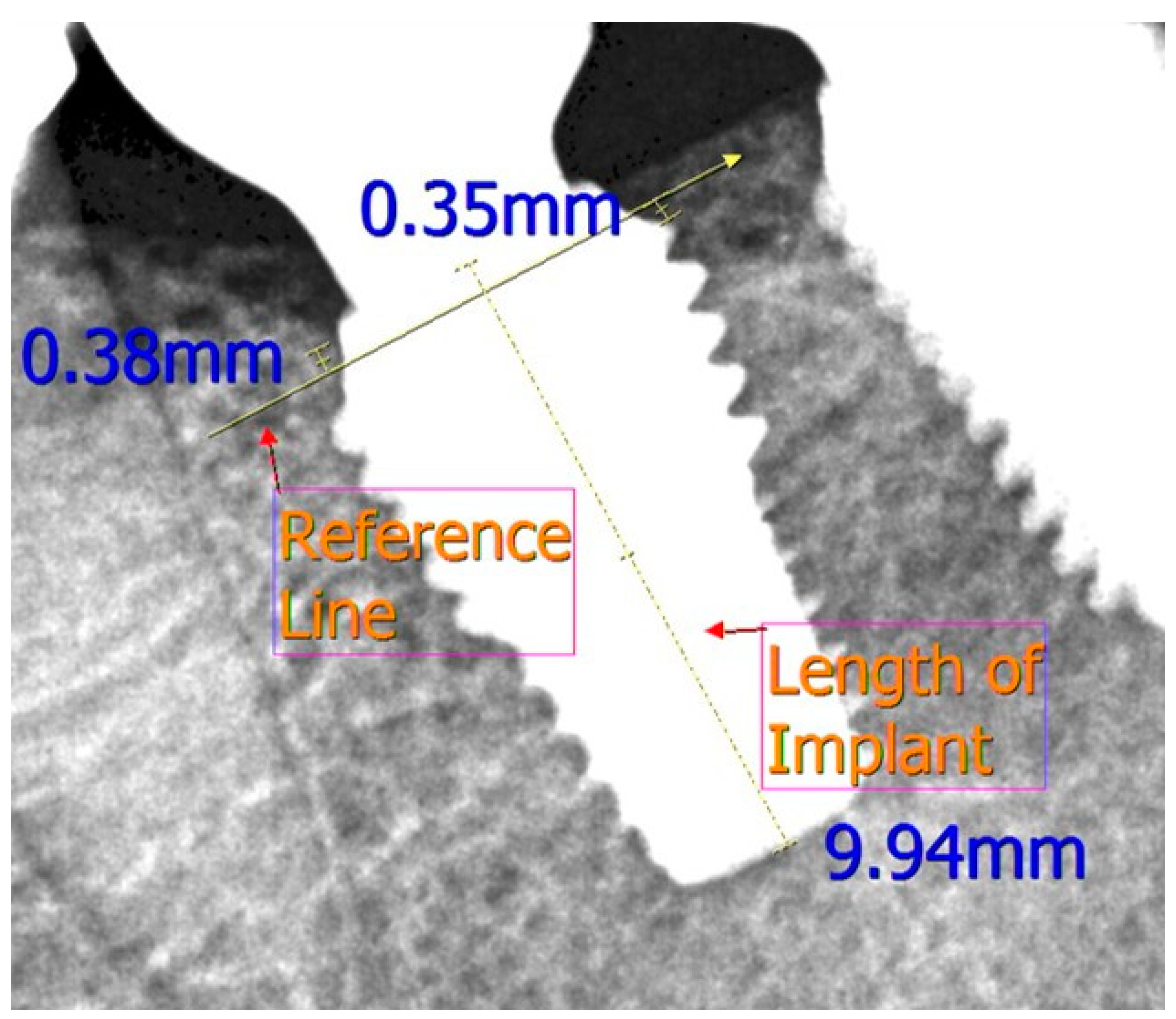
2.3. Measurement of Marginal Bone Levels and Implant Survival
2.4. Statistical Analyses
3. Results
3.1. Implant Survival Rates
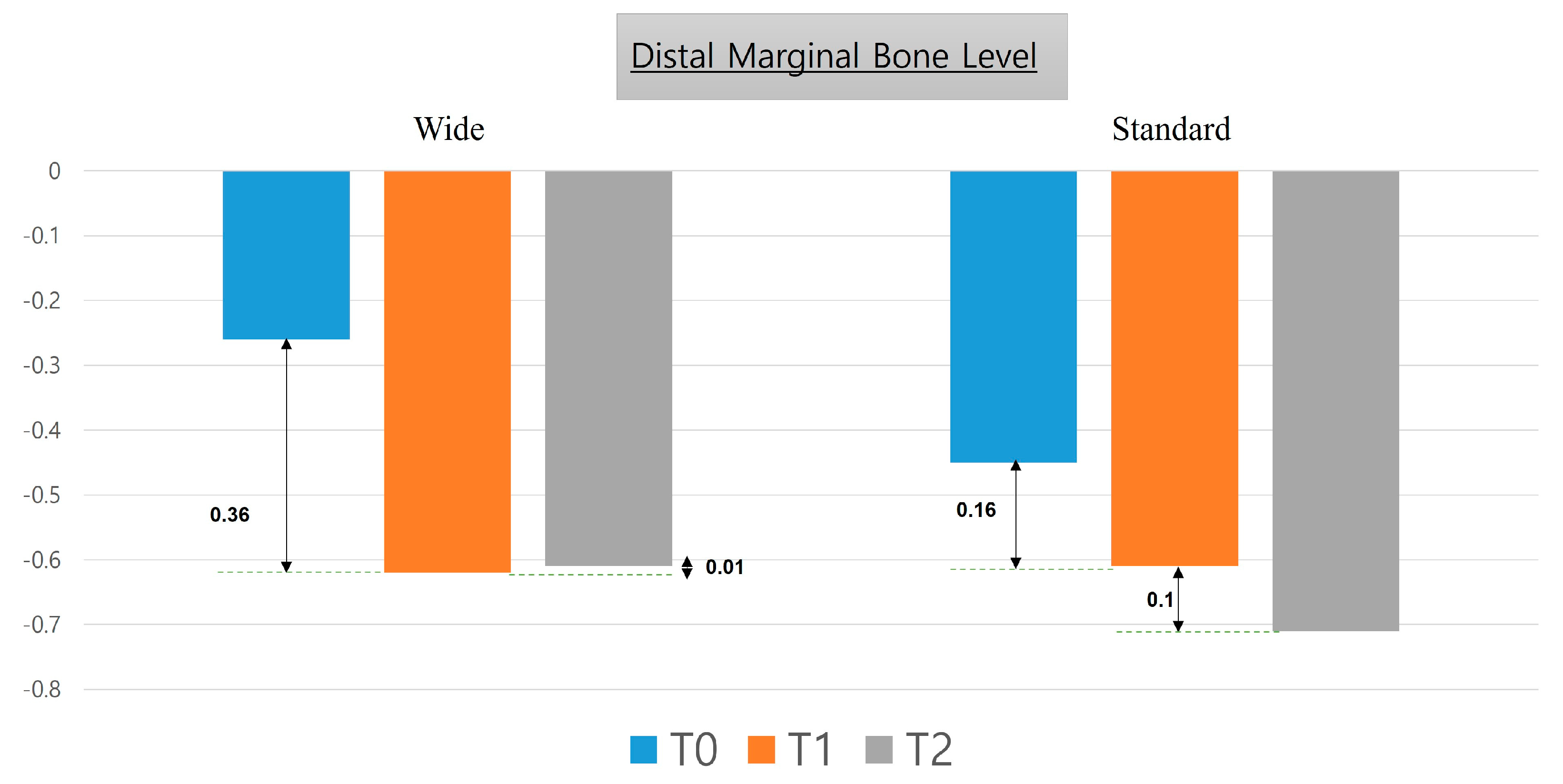
3.2. Marginal Bone Level
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Delle Donne, U.; Boni, W.; Corradini, G.; Tettamanti, L.; Tagliabue, A. Are Wide Diameter Implants Reliable for Jaws Rehabilitation? A Retrospective Study on 450 Implants. J. Biol. Regul. Homeost. Agents 2015, 29 (Suppl. 1), 34–38. [Google Scholar]
- Sohrabi, K.; Mushantat, A.; Esfandiari, S.; Feine, J. How successful are small-diameter implants? A literature review. Clin. Oral Implant. Res. 2012, 23, 515–525. [Google Scholar] [CrossRef] [PubMed]
- Davarpanah, M.; Martinez, H.; Kebir, M.; Etienne, D.; Tecucianu, J.F. Wide-diameter implants: New concepts. Int. J. Periodontics Restor. Dent. 2001, 21, 149–159. [Google Scholar]
- Nappo, A.; Rengo, C.; Pantaleo, G.; Spagnuolo, G.; Ferrari, M. Influence of Implant Dimensions and Position on Implant Stability: A Prospective Clinical Study in Maxilla Using Resonance Frequency Analysis. Appl. Sci. 2019, 9, 860. [Google Scholar] [CrossRef]
- Sivolella, S.; Guazzo, R.; Bressan, E.; Berengo, M.; Stellini, E. Platform switching on wide-diameter external hex implants: A finite element analysis. J. Clin. Exp. Dent. 2013, 5, e77–e82. [Google Scholar] [CrossRef] [PubMed]
- Langer, B.; Langer, L.; Herrmann, I.; Jorneus, L. The wide fixture: A solution for special bone situations and a rescue for the compromised implant. Part 1. Int. J. Oral Maxillofac. Implant. 1993, 8, 400–408. [Google Scholar]
- Checchi, V.; Felice, P.; Zucchelli, G.; Barausse, C.; Piattelli, M.; Pistilli, R.; Grandi, G.; Esposito, M. Wide diameter immediate post-extractive implants vs delayed placement of normal-diameter implants in preserved sockets in the molar region: 1-year post-loading outcome of a randomised controlled trial. Eur. J. Oral Implant. 2017, 10, 263–278. [Google Scholar]
- Lee, J.H.; Frias, V.; Lee, K.W.; Wright, R.F. Effect of implant size and shape on implant success rates: A literature review. J. Prosthet. Dent. 2005, 94, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Javed, F.; Romanos, G.E. Role of implant diameter on long-term survival of dental implants placed in posterior maxilla: A systematic review. Clin. Oral Investig. 2015, 19, 1–10. [Google Scholar] [CrossRef]
- Branemark, P.I.; Engstrand, P.; Ohrnell, L.O.; Grondahl, K.; Nilsson, P.; Hagberg, K.; Darle, C.; Lekholm, U. Branemark Novum: A new treatment concept for rehabilitation of the edentulous mandible. Preliminary results from a prospective clinical follow-up study. Clin. Implant. Dent. Relat Res. 1999, 1, 2–16. [Google Scholar] [CrossRef]
- Ibañez, C.; Catena, A.; Galindo-Moreno, P.; Noguerol, B.; Magán-Fernández, A.; Mesa, F. Relationship between Long-Term Marginal Bone Loss and Bone Quality, Implant Width, and Surface. Int. J. Oral Maxillofac. Implant. 2016, 31, 398–405. [Google Scholar] [CrossRef]
- Atieh, M.A.; Alsabeeha, N.H.; Duncan, W.J.; de Silva, R.K.; Cullinan, M.P.; Schwass, D.; Payne, A.G. Immediate single implant restorations in mandibular molar extraction sockets: A controlled clinical trial. Clin. Oral Implant. Res. 2013, 24, 484–496. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Xhanari, E.; Pisano, M.; Gatti, F.; Meloni, S.M. Molar replacement with 7 mm-wide diameter implants: To place the implant immediately or to wait 4 months after socket preservation? 1 year after loading results from a randomised controlled trial. Eur. J. Oral Implant. 2017, 10, 169–178. [Google Scholar]
- Tallarico, M.; Xhanari, E.; Pisano, M.; De Riu, G.; Tullio, A.; Meloni, S.M. Single post-extractive ultra-wide 7 mm-diameter implants versus implants placed in molar healed sites after socket preservation for molar replacement: 6-month post-loading results from a randomised controlled trial. Eur. J. Oral Implant. 2016, 9, 263–275. [Google Scholar]
- Ting, M.; Palermo, M.; Donatelli, D.P.; Gaughan, J.P.; Suzuki, J.B.; Jefferies, S.R. A meta-analysis on the effect of implant characteristics on the survival of the wide-diameter implant. Int. J. Implant. Dent. 2015, 1, 28. [Google Scholar] [CrossRef] [PubMed]
- Anner, R.; Better, H.; Chaushu, G. The clinical effectiveness of 6 mm diameter implants. J. Periodontol. 2005, 76, 1013–1015. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. A retrospective study on clinical and radiological outcomes of oral implants in patients followed up for a minimum of 20 years. Clin. Implant. Dent. Relat. Res. 2018, 20, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Anitua, E.; Fernandez-de-Retana, S.; Anitua, B.; Alkhraisat, M.H. Long-Term Retrospective Study of 3.0-mm-Diameter Implants Supporting Fixed Multiple Prostheses: Immediate Versus Delayed Implant Loading. Int. J. Oral Maxillofac. Implant. 2020, 35, 1229–1238. [Google Scholar] [CrossRef]
- Howe, M.S.; Keys, W.; Richards, D. Long-term (10-year) dental implant survival: A systematic review and sensitivity meta-analysis. J. Dent. 2019, 84, 9–21. [Google Scholar] [CrossRef]
- Park, Y.J.; Cho, S.A. Retrospective Chart Analysis on Survival Rate of Fixtures Installed at the Tuberosity Bone for Cases With Missing Unilateral Upper Molars: A Study of 7 Cases. J. Oral Maxillofac. Surg. 2010, 68, 1338–1344. [Google Scholar] [CrossRef]
- Shin, S.Y.; Shin, S.I.; Kye, S.B.; Hong, J.; Paeng, J.Y.; Chang, S.W.; Yang, S.M. The Effects of Defect Type and Depth, and Measurement Direction on the Implant Stability Quotient Value. J. Oral Implant. 2015, 41, 652–656. [Google Scholar] [CrossRef]
- Glauser, R.; Sennerby, L.; Meredith, N.; Ree, A.; Lundgren, A.; Gottlow, J.; Hammerle, C.H. Resonance frequency analysis of implants subjected to immediate or early functional occlusal loading. Successful vs. failing implants. Clin. Oral Implant. Res. 2004, 15, 428–434. [Google Scholar] [CrossRef]
- Attard, N.J.; Zarb, G.A. Implant prosthodontic management of partially edentulous patients missing posterior teeth: The Toronto experience. J. Prosthet. Dent. 2003, 89, 352–359. [Google Scholar] [CrossRef]
- Ku, J.-K.; Yi, Y.-J.; Yun, P.-Y.; Kim, Y.-K. Retrospective clinical study of ultrawide implants more than 6 mm in diameter. Maxillofac. Plast. Reconstr. Surg. 2016, 38, 30. [Google Scholar] [CrossRef] [PubMed]
- Santiago Junior, J.F.; Pellizzer, E.P.; Verri, F.R.; de Carvalho, P.S. Stress analysis in bone tissue around single implants with different diameters and veneering materials: A 3-D finite element study. Mater. Sci. Eng. C Mater. Biol. Appl. 2013, 33, 4700–4714. [Google Scholar] [CrossRef] [PubMed]
- Valera-Jiménez, J.F.; Burgueño-Barris, G.; Gómez-González, S.; López-López, J.; Valmaseda-Castellón, E.; Fernández-Aguado, E. Finite element analysis of narrow dental implants. Dent. Mater. 2020, 36, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Gargallo Albiol, J.; Satorres-Nieto, M.; Puyuelo Capablo, J.L.; Sanchez Garces, M.A.; Pi Urgell, J.; Gay Escoda, C. Endosseous dental implant fractures: An analysis of 21 cases. Med. Oral Patol. Oral Cir. Bucal 2008, 13, E124–E128. [Google Scholar]
- Zurdo, J.; Romão, C.; Wennström, J.L. Survival and complication rates of implant-supported fixed partial dentures with cantilevers: A systematic review. Clin. Oral Implant. Res. 2009, 20 (Suppl. 4), 59–66. [Google Scholar] [CrossRef]
- Di Fiore, A.; Vigolo, P.; Sivolella, S.; Cavallin, F.; Katsoulis, J.; Monaco, C.; Stellini, E. Influence of Crown-to-Implant Ratio on Long-Term Marginal Bone Loss Around Short Implants. Int. J. Oral Maxillofac. Implant. 2019, 34, 19. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, J.; Lapinska, B.; Nissan, J.; Lukomska-Szymanska, M. Factors Influencing Marginal Bone Loss around Dental Implants: A Narrative Review. Coatings 2021, 11, 865. [Google Scholar] [CrossRef]
- Lee, D.-W.; Park, K.-H.; Moon, I.-S. The effects of off-axial loading on periimplant marginal bone loss in a single implant. J. Prosthet. Dent. 2014, 112, 501–507. [Google Scholar] [CrossRef]
- Degidi, M.; Piattelli, A. 7-year follow-up of 93 immediately loaded titanium dental implants. J. Oral Implant. 2005, 31, 25–31. [Google Scholar] [CrossRef]
- Krennmair, G.; Waldenberger, O. Clinical analysis of wide-diameter frialit-2 implants. Int. J. Oral Maxillofac. Implant. 2004, 19, 710–715. [Google Scholar]
- Rodriguez, X.; Mendez, V.; Vela, X.; Segala, M. Modified surgical protocol for placing implants in the pterygomaxillary region: Clinical and radiologic study of 454 implants. Int. J. Oral Maxillofac. Implant. 2012, 27, 1547–1553. [Google Scholar]
- Lambert, F.; Lecloux, G.; Rompen, E. One-step approach for implant placement and subantral bone regeneration using bovine hydroxyapatite: A 2- to 6-year follow-up study. Int. J. Oral Maxillofac. Implant. 2010, 25, 598–606. [Google Scholar]
- Ridell, A.; Grondahl, K.; Sennerby, L. Placement of Branemark implants in the maxillary tuber region: Anatomical considerations, surgical technique and long-term results. Clin. Oral Implant. Res. 2009, 20, 94–98. [Google Scholar] [CrossRef]
- Valeron, J.F.; Valeron, P.F. Long-term results in placement of screw-type implants in the pterygomaxillary-pyramidal region. Int. J. Oral Maxillofac. Implant. 2007, 22, 195–200. [Google Scholar]
- Ivanoff, C.J.; Grondahl, K.; Sennerby, L.; Bergstrom, C.; Lekholm, U. Influence of variations in implant diameters: A 3- to 5-year retrospective clinical report. Int. J. Oral Maxillofac. Implant. 1999, 14, 173–180. [Google Scholar] [CrossRef]
- Atieh, M.A.; Alsabeeha, N.H.M.; Faggion Jr, C.M.; Duncan, W.J. The Frequency of Peri-Implant Diseases: A Systematic Review and Meta-Analysis. J. Periodontol. 2013, 84, 1586–1598. [Google Scholar] [CrossRef]
- Rinke, S.; Ohl, S.; Ziebolz, D.; Lange, K.; Eickholz, P. Prevalence of periimplant disease in partially edentulous patients: A practice-based cross-sectional study. Clin. Oral Implant. Res. 2011, 22, 826–833. [Google Scholar] [CrossRef]
- Smith, D.E.; Zarb, G.A. Criteria for success of osseointegrated endosseous implants. J. Prosthet. Dent. 1989, 62, 567–572. [Google Scholar] [CrossRef]
- Zarb, G.A.; Albrektsson, T. Consensus report: Towards optimized treatment outcomes for dental implants. J. Prosthet. Dent. 1998, 80, 641. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; León-Cano, A.; Ortega-Oller, I.; Monje, A.; Suárez, F.; ÓValle, F.; Spinato, S.; Catena, A. Prosthetic Abutment Height is a Key Factor in Peri-implant Marginal Bone Loss. J. Dent. Res. 2014, 93 (Suppl. 7), 12. [Google Scholar] [CrossRef] [PubMed]



| Implants | Wide n = 40 | Standard n = 40 | |
|---|---|---|---|
| Anatomical location | Maxilla | 22 | 19 |
| Mandible | 18 | 21 | |
| Sex | Male | 29 | 20 |
| Female | 7 | 16 | |
| Age (years) | Mean | 52.83 | 54.27 |
| Immediately placed after extraction | Yes | 8 | 4 |
| No | 32 | 36 | |
| Bone graft (Bio-Oss) | Yes | 10 | 17 |
| No | 30 | 23 | |
| Surgical Technique | One-Stage | 14 | 11 |
| Two-Stage | 26 | 29 | |
| Sinus Floor Elevation | Yes | 4 | 4 |
| Implant Length | 7 mm | 2 | 2 |
| 8.5 mm | 3 | 13 | |
| 10 mm | 26 | 18 | |
| 11 mm | 9 | 7 |
| Group | Total Implants | Lost To Follow-Up | Implants Lost | Implants Survived | Survival Rate (%) | Failure Rate (%) | Fisher’s Exact Test |
|---|---|---|---|---|---|---|---|
| Wide | 40 | 3 | 1 | 36 | 97.29 | 2.70 | p-value > 0.05 |
| Standard | 40 | 1 | 2 | 37 | 94.87 | 5.13 |
| MBL | n | Mean ± SD | Median | Range | n | Mean ± SD | Median | Range | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Implant placement | Mesial | 40 | −0.14 ± 0.34 | −0.93 | −2.55 to 0 | 40 | −0.12 ± 0.58 | 0 | −1.01 to 1.24 | 0.8248 |
| Distal | −0.26 ± 0.49 | −1.05 | −2.25 to 0 | −0.45 ± 0.33 | −0.6 | −1.46 to 0 | 0.9436 | |||
| Mean | −0.2 ± 0.52 | −0.99 | −2.23 to −0.44 | −0.28 ± 0.35 | −0.175 | −1.235 to 0.35 | 0.5382 | |||
| 1 Year | Mesial | 39 | −0.48 ± 0.81 | −0.54 | −2.12 to 1.22 | 38 | −0.44 ± 0.44 | −0.425 | −1.3 to 0.55 | 0.8018 |
| Distal | −0.62 ± 0.63 | −0.62 | −2.79 to 0.87 | −0.61 ± 0.45 | −0.585 | −1.9 to 0.45 | 0.9764 | |||
| Mean | −0.55 ± 0.62 | −0.64 | −1.83 to 1.03 | −0.52 ± 0.37 | −0.5925 | −1.2 to 0.375 | 0.8606 | |||
| 6 Years | Mesial | 36 | −0.49 ± 1.02 | −0.4 | −2.9 to 1 | 37 | −0.61 ± 0.65 | −0.54 | −3.07 to 0.38 | 0.5507 |
| Distal | −0.61 ± 1.06 | −0.35 | −3.39 to 1.43 | −0.71 ± 0.69 | −0.75 | −2.98 to 0.4 | 0.6191 | |||
| Mean | −0.55 ± 1 | −0.35 | −3.11 to 1.09 | −0.66 ±0.63 | −0.66 | −3.02 to 0.28 | 0.5667 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wadhwa, P.; Kim, S.-K.; Kim, H.-J.; Lim, H.-K.; Jia, Q.; Jiang, H.-B.; Lee, E.-S. A Six-Year Prospective Comparative Study of Wide and Standard Diameter Implants in the Maxillary and Mandibular Posterior Area. Medicina 2021, 57, 1009. https://doi.org/10.3390/medicina57101009
Wadhwa P, Kim S-K, Kim H-J, Lim H-K, Jia Q, Jiang H-B, Lee E-S. A Six-Year Prospective Comparative Study of Wide and Standard Diameter Implants in the Maxillary and Mandibular Posterior Area. Medicina. 2021; 57(10):1009. https://doi.org/10.3390/medicina57101009
Chicago/Turabian StyleWadhwa, Puneet, Seung-Kook Kim, Hyun-Jin Kim, Ho-Kyung Lim, Qi Jia, Heng-Bo Jiang, and Eui-Seok Lee. 2021. "A Six-Year Prospective Comparative Study of Wide and Standard Diameter Implants in the Maxillary and Mandibular Posterior Area" Medicina 57, no. 10: 1009. https://doi.org/10.3390/medicina57101009
APA StyleWadhwa, P., Kim, S.-K., Kim, H.-J., Lim, H.-K., Jia, Q., Jiang, H.-B., & Lee, E.-S. (2021). A Six-Year Prospective Comparative Study of Wide and Standard Diameter Implants in the Maxillary and Mandibular Posterior Area. Medicina, 57(10), 1009. https://doi.org/10.3390/medicina57101009








