Preliminary Results of an Exercise Program After Laparoscopic Resective Colorectal Cancer Surgery in Non-Metastatic Adenocarcinoma: A Pilot Study of a Randomized Control Trial
Abstract
1. Introduction
2. Experimental Section
2.1. Study Population
2.2. Preoperative Workup and Surgical Techniques
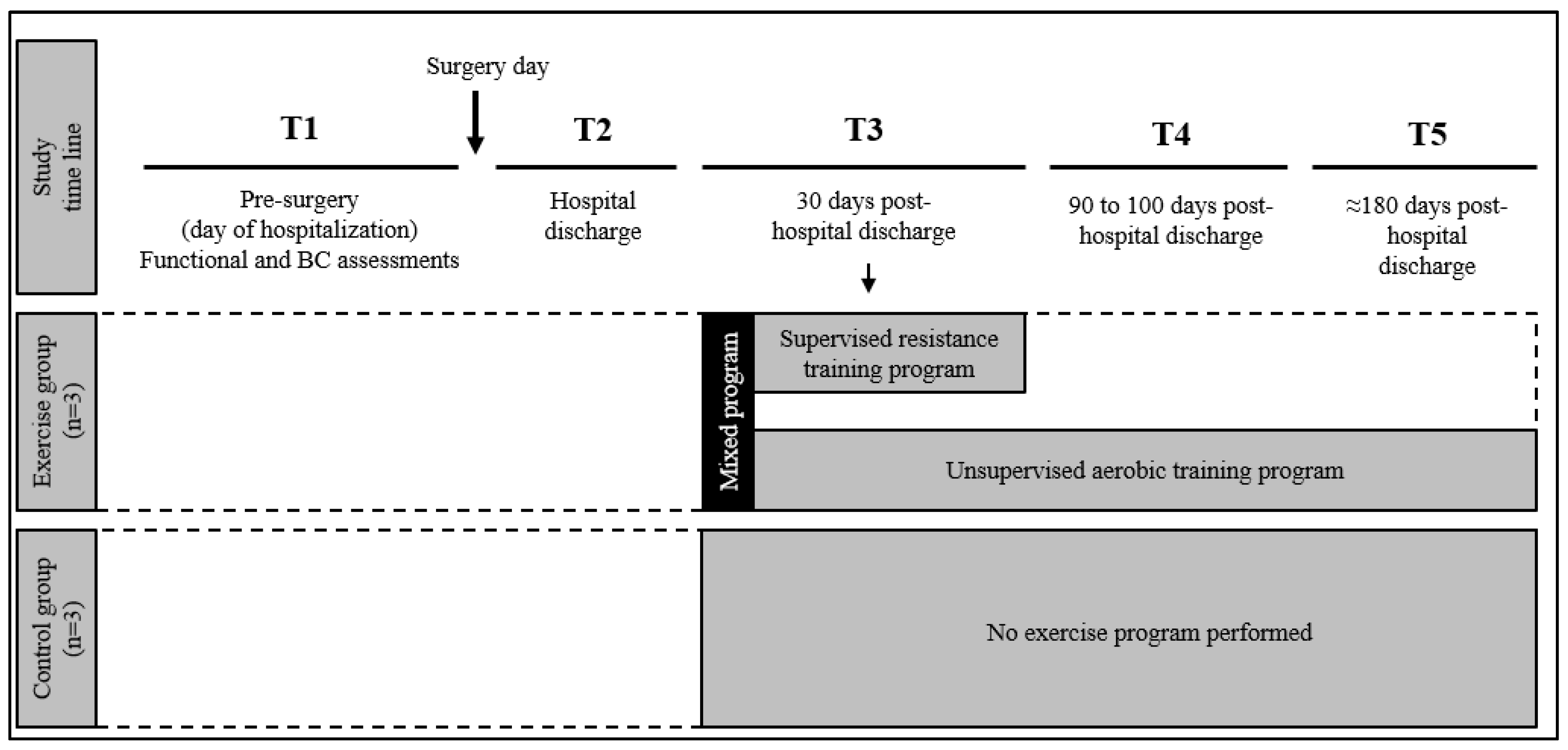
2.3. Study Design
2.4. Functional Assessment
2.4.1. Cardiovascular Fitness
2.4.2. Muscular Fitness
2.5. Body Composition Analysis
2.5.1. Anthropometry
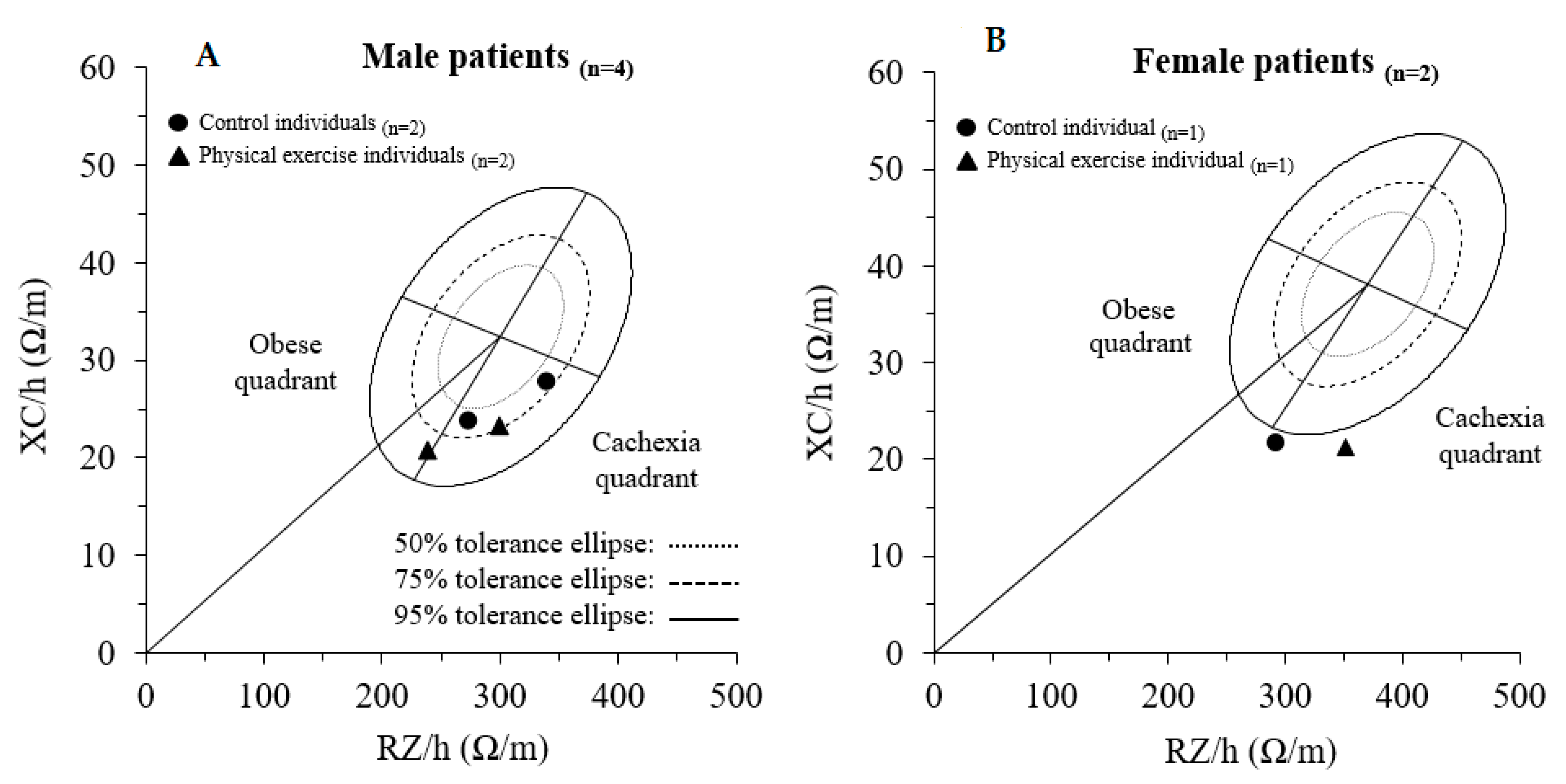
2.5.2. Whole-Body Bioimpedance Analysis (BIA) and Vector Analysis (BIVA)
2.6. Exercise Program
2.7. Statistical Analysis
3. Results
3.1. Functional Assessment
3.2. Body Composition Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- AIOM, AIRTUM. Fondazione AIOM, PASSI, PASSI D’Argento, SIAPEC-IAP Workinggroup. I Numeri del cancro in Italia 2019. Available online: https://www.epicentro.iss.it/tumori/pdf/NC2019-operatori-web.pdf (accessed on 4 November 2019).
- AIRTUM Working Group. Italiancancerfigures, Report 2014: Prevalenza e guarigione da tumore in Italia. Prevalence and cure of cancer in Italy. EpidemiolPrev 2014, 38 (Suppl. 1), 1–144. [Google Scholar]
- Kang, C.Y.; Chaudhry, O.O.; Halabi, W.J.; Nguyen, V.; Carmichael, J.C.; Stamos, M.J.; Mills, S. Outcomes of laparoscopic colorectal surgery: Data from the Nationwide Inpatient Sample 2009. Am. J. Surg. 2012, 204, 952–957. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.; Coolsen, M.M.; Aahlin, E.K.; Harrison, E.M.; McNally, S.J.; DeJong, C.; Lassen, K.; Wigmore, S.J. Attitudes of patients and care providers to enhanced recovery after surgery programs after major abdominal surgery. J. Surg. Res. 2015, 193, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Carmichael, J.C.; Keller, D.S.; Baldini, G.; Bordeianou, L.; Weiss, E.; Lee, L.; Boutros, M.; McClane, J.; Feldman, L.S.; Steele, S.R. Clinical Practice Guidelines for Enhanced Recovery After Colon and Rectal Surgery From the American Society of Colon and Rectal Surgeons and Society of American Gastrointestinal and Endoscopic Surgeons. Dis. Colon Rectum 2017, 60, 761–784. [Google Scholar] [CrossRef]
- Thiele, R.H.; Rea, K.M.; Turrentine, F.E.; Friel, C.M.; Hassinger, T.E.; Goudreau, B.J.; Umapathi, B.A.; Kron, I.L.; Sawyer, R.G.; Hedrick, T.L.; et al. Standardization of Care: Impact of an Enhanced Recovery Protocol on Length of Stay, Complications, and Direct Costs after Colorectal Surgery. J. Am. Coll. Surg. 2015, 220, 430–443. [Google Scholar] [CrossRef]
- McTiernan, A.; Friedenreich, C.M.; Katzmarzyk, P.T.; Powell, K.E.; Macko, R.; Buchner, D.; Pescatello, L.S.; Bloodgood, B.; Tennant, B.; Vaux-Bjerke, A.; et al. 2018 PHYSICAL ACTIVITY GUIDELINES ADVISORY COMMITTEE. Physical Activity in Cancer Prevention and Survival: A Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1252–1261. [Google Scholar] [CrossRef]
- Arem, H.; Pfeiffer, R.M.; Engels, E.A.; Alfano, C.M.; Hollenbeck, A.; Park, Y.; Matthews, C.E. Pre- and post-diagnosis physical activity, television viewing, and mortality among patients with colorectal cancer in the National Institutes of Health-AARP Diet and Health Study. J. Clin. Oncol. 2015, 33, 180–188. [Google Scholar] [CrossRef]
- Van Zutphen, M.; Winkels, R.M.; Van Duijnhoven, F.J.B.; Van Harten-Gerritsen, S.A.; Kok, D.E.G.; Van Duijvendijk, P.; Van Halteren, H.K.; Hansson, B.M.E.; Kruyt, F.M.; Bilgen, E.J.S.; et al. An increase in physical activity after colorectal cancer surgery is associated with improved recovery of physical functioning: A prospective cohort study. BMC Cancer 2017, 17, 74. [Google Scholar] [CrossRef]
- van Putten, M.; Husson, O.; Mols, F.; Luyer, M.D.; van de Poll-Franse, L.V.; Ezendam, N.P. Correlates of physical activity among colorectal cancer survivors: Results from the longitudinal population-based profiles registry. Support Care Cancer 2016, 24, 573–583. [Google Scholar] [CrossRef]
- Segal, R.; Zwaal, C.; Green, E.; Tomasone, J.R.; Loblaw, A.; Petrella, T. Exercise for People with Cancer Guideline Development Group. Exercise for people with cancer: A clinical practice guideline. Curr. Oncol. 2017, 24, 40–46. [Google Scholar] [CrossRef]
- Shallwani, S.M.; King, J.; Thomas, R.; Thevenot, O.; De Angelis, G.; Aburub, A.S.; Brosseau, L. Methodological quality of clinical practice guidelines with physical activity recommendations for people diagnosed with cancer: A systematic critical appraisal using the AGREE II tool. PLoS ONE 2019, 14, e0214846. [Google Scholar] [CrossRef]
- Ringressi, M.N.; Boni, L.; Freschi, G.; Scaringi, S.; Indennitate, G.; Bartolini, I.; Bechi, P.; Taddei, A. Comparing laparoscopic surgery with open surgery for long-term outcomes in patients with stage I to III colon cancer. Surg. Oncol. 2018, 27, 115–122. [Google Scholar] [CrossRef]
- Labianca, R.; Nordlinger, B.; Beretta, G.D.; Mosconi, S.; Mandalà, M.; Cervantes, A.; Arnold, D.; ESMO Guidelines Working Group. ESMO Guidelines Working Group Early colon cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2013, 24 (Suppl. 6), vi64–vi72. [Google Scholar] [CrossRef] [PubMed]
- Moriello, C.; Mayo, N.E.; Feldman, L.; Carli, F. Validating the Six-Minute Walk Test as a Measure of Recovery After Elective Colon Resection Surgery. Arch. Phys. Med. Rehabil. 2008, 89, 1083–1089. [Google Scholar] [CrossRef] [PubMed]
- Arney, B.E.; Glover, R.; Fusco, A.; Cortis, C.; De Koning, J.J.; Van Erp, T.; Jaime, S.; Mikat, R.P.; Porcari, J.P.; Foster, C. Comparison of RPE (Rating of Perceived Exertion) Scales for Session RPE. Int. J. Sports Physiol. Perform. 2019, 14, 994–996. [Google Scholar] [CrossRef]
- Mayorga-Vega, D.; Merino-Marban, R.; Viciana, J. Criterion-Related Validity of Sit-and-Reach Tests for Estimating Hamstring and Lumbar Extensibility: A Meta-Analysis. J. Sports Sci. Med. 2014, 13, 1–14. [Google Scholar] [PubMed]
- Gomes, P.R.L.; Junior, I.F.F.; Da Silva, C.B.; Gomes, I.C.; Rocha, A.P.R.; Salgado, A.S.I.; Carmo, E.M.D. Short-term changes in handgrip strength, body composition, and lymphedema induced by breast cancer surgery. Rev. Bras. Ginecol. Obs. RBGO Gynecol. Obstet. 2014, 36, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; Garber, C.E.; Ortiz, M.; Shankar, V.; Goldberg, G.L.; Nevadunsky, N.S. Feasibility of a physical activity intervention for obese, socioculturally diverse endometrial cancer survivors. Gynecol. Oncol. 2016, 142, 304–310. [Google Scholar] [CrossRef]
- Stewart, A.; Marfell-Jones, J.M.; Olds, T.; De Ridder, H. International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: Wellington, New Zealand, 2011; pp. 1–126. [Google Scholar]
- Yanovski, S.Z.; Hubbard, V.S.; Heymsfield, S.B.; Lukaski, H.C. Bioelectrical impedance analysis in body composition measurement: National institutes of health technology assessment conference statement. Am. J. Clin. Nutr. 1996, 64, 524S–532S. [Google Scholar]
- Piccoli, A.; Rossi, B.; Pillon, L.; Bucciante, G. A new method for monitoring body fluid variation by bioimpedance analysis: The RXc graph. Kidney Int. 1994, 46, 534–539. [Google Scholar] [CrossRef]
- Piccoli, A. Whole Body—Single Frequency Bioimpedance. Pathophysiol. Ren. Dis. 2005, 149, 150–161. [Google Scholar]
- Schmitz, K.H.; Courneya, K.S.; Matthews, C.; Demark-Wahnefried, W.; Galvão, D.A.; Pinto, B.M.; Irwin, M.L.; Wolin, K.Y.; Segal, R.J.; Lucia, A.; et al. on behalf of the American College of Sports Medicine. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med. Sci. Sports Exerc. 2010, 42, 1409–1426. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.S.; Matthews, C.E.; Ligibel, J.A.; Gerber, L.H.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: Abingdon, UK, 1988. [Google Scholar]
- Piccoli, A.; Pastori, G. BIVA Software; Department of Medical and Surgical Sciences, University of Padova: Padova, Italy, 2002. [Google Scholar]
- Saragat, B.; Buffa, R.; Mereu, E.; De Rui, M.; Coin, A.; Sergi, G.; Marini, E. Specific bioelectrical impedance vector reference values for assessing body composition in the Italian elderly. Exp. Gerontol. 2014, 50, 52–56. [Google Scholar] [CrossRef]
- Cabilan, C.; Hines, S. The short-term impact of colorectal cancer treatment on physical activity, functional status and quality of life. JBI Database Syst. Rev. Implement. Rep. 2017, 15, 517–566. [Google Scholar] [CrossRef]
- Devin, J.L.; Sax, A.T.; Hughes, G.I.; Jenkins, D.G.; Aitken, J.F.; Chambers, S.K.; Dunn, J.C.; Bolam, K.A.; Skinner, T.L. The influence of high-intensity compared with moderate-intensity exercise training on cardiorespiratory fitness and body composition in colorectal cancer survivors: A randomised controlled trial. J. Cancer Surviv. 2016, 10, 467–479. [Google Scholar] [CrossRef]
- Sellar, C.M.; Bell, G.J.; Haennel, R.G.; Au, H.-J.; Chua, N.; Courneya, K.S. Feasibility and efficacy of a 12-week supervised exercise intervention for colorectal cancer survivors. Appl. Physiol. Nutr. Metab. 2014, 39, 715–723. [Google Scholar] [CrossRef]
- Pinto, B.M.; Papandonatos, G.D.; Goldstein, M.G.; Marcus, B.H.; Farrell, N. Home-based physical activity intervention for colorectal cancer survivors. Psycho Oncol. 2013, 22, 54–64. [Google Scholar] [CrossRef]
- Min, J.-H.; Ahn, K.-Y.; Park, H.; Cho, W.; Jung, H.J.; Kim, N.K.; Jeon, J.Y. The Effect of Post-operative Exercise in Colorectal Cancer Patients: A Pilot Randomized Controlled Trial (RCT) Study. Asian Oncol. Nurs. 2017, 17, 29. [Google Scholar] [CrossRef]
- Awasthi, R.; Minnella, E.M.; Ferreira, V.; Ramanakumar, A.V.; Scheede-Bergdahl, C.; Carli, F. Supervised exercise training with multimodal pre-habilitation leads to earlier functional recovery following colorectal cancer resection. Acta Anaesthesiol. Scand. 2019, 63, 461–467. [Google Scholar] [CrossRef]
- Gillis, C.; Li, C.; Lee, L.; Awasthi, R.; Augustin, B.; Gamsa, A.; Liberman, A.S.; Stein, B.; Charlebois, P.; Feldman, L.S.; et al. Prehabilitation versus rehabilitation: A randomized control trial in patients undergoing colorectal resection for cancer. Anesthesiology 2014, 121, 937–947. [Google Scholar] [CrossRef] [PubMed]
- ACSM. ACSM’s Resource Manual for Guidelines for Exercise Testing and Prescription, 10th ed.; Riebe, D., Ehrman, J.K., Liguori, G., Magal, M., Eds.; Wolters Kluwer: Philadelphia, PA, USA, 2018. [Google Scholar]
- Moore, F.D.; Boyden, C.M. Body cell mass and limits of hydration of the fat-free body: Their relation to estimated skeletal weight*. Ann. New York Acad. Sci. 2006, 110, 62–71. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, I.C.R.; Aredes, M.A.; Chaves, G.V. Applicability of the direct parameters of bioelectrical impedance in assessing nutritional status and surgical complications of women with gynecological cancer. Eur. J. Clin. Nutr. 2017, 71, 1278–1284. [Google Scholar] [CrossRef] [PubMed]
- Buffa, R.; Saragat, B.; Cabras, S.; Rinaldi, A.C.; Marini, E. Accuracy of Specific BIVA for the Assessment of Body Composition in the United States Population. PLoS ONE 2013, 8, e58533. [Google Scholar] [CrossRef] [PubMed]
- Marini, E.; Sergi, G.; Succa, V.; Saragat, B.; Sarti, S.; Coin, A.; Manzato, E.; Buffa, R. Efficacy of specific bioelectrical impedance vector analysis (BIVA) for assessing body composition in the elderly. J. Nutr. Health Aging. 2013, 17, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Marini, E.; Buffa, R.; Saragat, B.; Coin, A.; Toffanello, E.D.; Berton, L.; Manzato, E.; Sergi, G. The potential of classic and specific bioelectrical impedance vector analysis for the assessment of sarcopenia and sarcopenic obesity. Clin. Interv. Aging 2012, 7, 585–591. [Google Scholar] [CrossRef] [PubMed]

| Sit and Reach (cm) | 30˝ Chair Test (rep.) | Handgrip Dx. (kg) | Handgrip Sx. (kg) | 6-MWD (m) | CR10 (a. u) | Rest HR (bpm) | HR Max (bpm) | Rest SBP (mmHg) | Rest DBP (mmHg) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Exercise Group | ||||||||||
| T1pre-surgery | −15.3 ± 9.2 | 11.3 ± 4.5 | 29.0 ± 4.6 | 30.7 ± 6.8 | 463.3 ± 102.6 | 4.3 ± 2.5 | 91.3 ± 4.9 | 107.3 ± 1.5 | 118.3 ± 17.6 | 73.3 ± 10.4 |
| T2post-surgery | −17.3 ± 11.0 | 10.0 ± 5.6 | 26.3 ± 6.7 | 26.3 ± 6.7 | 418.3 ± 107.5 | 4.7 ± 3.1 | 89.3 ± 5.1 | 106.7 ± 2.9 | 106.7 ± 5.8 | 66.7 ± 2.9 |
| T3post-exercise | −14.0 ± 7.8 | 12.7 ± 5.0 § (0.27) | 29.3 ± 4.6 | 29.0 ± 6.1 | 476.7 ± 121.0 | 5.0 ± 3.0 | 91.7 ± 4.2 | 108.0 ± 11.8 | 110.0 ± 5.0 | 71.7 ± 2.9 |
| T43-months | −12.0 ± 6.0 | 13.0 ± 6.1 (0.31) | 27.0 ± 7.8 | 30.7 ± 4.2 | 478.3 ± 101.0 § (0.32) | 5.0 ± 4.0 | 89.3 ± 6.0 | 107.0 ± 10.8 | 118.3 ± 7.6 | 73.3 ± 2.9 |
| T56-months | −9.9 ± 5.5 § (0.33) | 14.1 ± 5.1 § (0.42) | 29.5 ± 4.1 | 28.3 ± 6.0 | 472.3 ± 105.1 § (0.28) | 5.6 ± 1.7 | 89.0 ± 8.0 | 108.2 ± 2.4 | 109.3 ± 12.9 | 70.2 ± 5.0 |
| Control Group | ||||||||||
| T1pre-surgery | −8.0 ± 8.9 | 15.0 ± 5.2 | 32.7 ± 18.2 | 33.7 ± 11.7 | 543.3 ± 102.1 | 4.7 ± 2.5 | 94.3 ± 14.6 | 120.7 ± 10.6 | 131.7 ± 7.6 | 76.7 ± 7.6 |
| T2post-surgery | −7.7 ± 7.2 | 11.7 ± 4.0 | 30.7 ± 15.0 | 30.7 ± 15.0 | 470.0 ± 87.2 | 3.3 ± 1.5 | 90.7 ± 21.1 | 108.7 ± 17.7 | 120.0 ± 18.0 | 66.7 ± 15.3 |
| T3post-exercise | −9.3 ± 5.9 | 14.0 ± 5.2 | 33.3 ± 14.5 | 30.7 ± 15.0 | 502.0 ± 88.9 | 2.8 ± 1.4 | 92.3 ± 18.6 | 108.0 ± 9.6 | 128.3 ± 5.8 | 73.3 ± 2.9 |
| T43-months | −9.3 ± 11.2 | 15.3 ± 6.8 | 32.3 ± 13.6 | 31.3 ± 14.5 | 506.7 ± 107.9 | 3.7 ± 1.5 | 84.3 ± 25.0 | 102.7 ± 10.8 | 128.3 ± 5.8 | 73.3 ± 2.9 |
| T56-months | −11.0 ± 9.5 | 15.3 ± 5.9 | 33.3 ± 14.5 | 31.7 ± 14.2 | 510.0 ± 87.2 | 3.7 ± 1.5 | 89.3 ± 18.3 | 109.7 ± 5.5 | 121.7 ± 7.6 | 75.7 ± 2.9 |
| Weight (kg) | BMI (kg/m2) | Waist Circ. (cm) | Hip Circ. (cm) | Biceps Circ. (cm) | ∑4 Skinfold (mm) | FM (%) | FFM (kg) | |
|---|---|---|---|---|---|---|---|---|
| Exercise Group | ||||||||
| T1pre-surgery | 83.6 ± 19.6 | 30.1 ± 7.3 | 103.2 ± 18.5 | 109.0 ± 17.3 | 31.5 ± 4.5 | 129.1 ± 8.1 | 30.8 ± 10.6 | 54.7 ± 8.5 |
| T2post-surgery | 80.0 ± 18.6 * (0.11) | 28.8 ± 6.9 * (0.10) | 101.7 ± 18.1 | 106.7 ± 16.9 * (0.08) | 30.7 ± 4.5 | 128.1 ± 10.1 | 30.3 ± 9.9 | 52.3 ± 8.5 *(0.16) |
| T3post-exercise | 81.3 ± 17.8 | 29.3 ± 6.7 | 102.2 ± 17.5 | 105.7 ± 17.0 | 30.4 ± 4.1 | 127.3 ± 8.8 | 29.9 ± 9.9 | 53.7 ± 8.0 |
| T43-months | 81.7 ± 17.8 | 29.5 ± 6.8 | 101.2 ± 18.0 | 102.7 ± 13.1 | 30.5 ± 4.5 | 127.1 ± 4.7 | 29.8 ± 10.4 | 53.8 ± 7.8 |
| T56-months | 82.0 ± 18.6 | 29.6 ± 7.1 | 100.4 ± 17.2 | 104.9 ± 16.1 | 30.5 ± 4.3 | 125.5 ± 2.8 | 29.5 ± 9.8 | 54.2 ± 6.0 |
| Control Group | ||||||||
| T1pre-surgery | 71.3 ± 15.2 | 24.3 ± 2.7 | 88.0 ± 13.9 | 101.3 ± 6.0 | 27.7 ± 2.1 | 117.3 ± 20.1 | 25.2 ± 5.1 | 54.3 ± 13.0 |
| T2post-surgery | 68.6 ± 15.4 * (0.10) | 23.4 ± 3.0 * (0.02) | 86.7 ± 14.5 | 99.7 ± 8.0 | 26.5 ± 3.0 | 117.6 ± 19.8 | 25.3 ± 2.8 | 52.5 ± 13.0 |
| T3post-exercise | 70.5 ± 15.5 § (0.07) | 24.1 ± 2.9 § (0.13) | 87.5 ± 13.9 | 100.7 ± 6.7 | 27.0 ± 3.5 | 117.1 ± 17.4 | 25.1 ± 4.3 | 54.3 ± 13.8 |
| T43-months | 70.8 ± 15.2 § (0.15) | 24.8 ± 2.8 § (0.27) | 88.5 ± 15.0 | 99.3 ± 5.0 | 27.2 ± 2.5 | 119.3 ± 16.1 | 26.1 ± 4.0 | 54.1 ± 12.9 |
| T56-months | 71.4 ± 13.1 | 24.4 ± 1.8 | 86.5 ± 12.1 | 99.0 ± 5.0 | 27.7 ± 2.6 | 115.3 ± 13.3 | 27.7 ± 4.8 | 54.2 ± 12.5 |
| RZ (Ω) | XC (Ω) | PA (°) | TBW (L) | TBW (%) | ECW (%) | ICW (%) | BCM (kg) | RMR (kcal) | |
|---|---|---|---|---|---|---|---|---|---|
| Exercise Group | |||||||||
| T1pre-surgery | 502.3 ± 53.5 | 40.7 ± 5.5 | 4.6 ± 0.4 | 41.1 ± 5.9 | 49.7 ± 7.5 | 53.1 ± 2.5 | 46.9 ± 2.5 | 25.2±5.1 | 1480.8 ± 149.1 |
| T2post-surgery | 539.7 ± 69.2 | 41.0 ± 5.6 | 4.3 ± 0.4 *(0.42) | 39.2 ± 6.0 * (0.18) | 48.6 ± 6.4 | 54.8 ± 2.3 * (0.40) | 45.2 ± 2.3 * (0.40) | 23.2±4.9 * (0.23) | 1421.5 ± 141.3 * (0.23) |
| T3post-exercise | 513.7 ± 42.7 | 38.7 ± 2.3 | 4.3 ± 0.4 | 40.3 ± 5.5 | 49.8 ± 7.9 | 55.0 ± 2.7 | 45.0 ± 2.7 | 23.7±5.1 * | 1437.1 ± 148.8 |
| T43-months | 515.3 ± 36.6 | 40.7 ± 1.2 | 4.5 ± 0.2 | 39.4 ± 5.8 | 53.3 ± 3.3 | 53.7 ± 1.3 | 46.3 ± 1.3 § (0.32) | 24.2±4.2 § (0.31) | 1451.5 ± 121.8 § (0.18) |
| T56-months | 515.0 ± 48.0 | 40.3 ± 5.0 | 4.5 ± 0.2 | 40.1 ± 4.2 | 49.4 ± 6.9 | 53.7 ± 1.1 | 46.3 ± 1.1 § (0.33) | 24.5±2.9 § (0.33) | 1461.2 ± 84.0 § (0.26) |
| Control Group | |||||||||
| T1pre-surgery | 501.0 ± 68.4 | 37.0 ± 3.0 | 4.3 ± 0.8 | 41.4 ± 9.5 | 58.1 ± 2.6 | 55.5 ± 5.2 | 44.5 ± 5.2 | 24.0 ± 8.4 | 1446.0 ± 244.2 |
| T2post-surgery | 522.3 ± 93.9 | 36.7 ± 6.1 | 4.1 ± 1.0 * (0.13) | 40.2 ± 9.7 | 58.5 ± 1.4 | 57.1 ± 6.7 | 42.9 ± 6.7 * (0.17) | 22.4 ± 9.1 * (0.11) | 1399.6 ± 262.4 |
| T3post-exercise | 486.3 ± 87.3 § (0.22) | 35.0 ± 3.0 | 4.2 ± 0.9 | 42.3 ± 10.4 | 59.8 ± 2.0 | 57.1 ± 5.9 | 42.9 ± 5.9 | 22.7 ± 9.2 | 1419.0 ± 267.5 |
| T43-months | 475.3 ± 85.5 § (0.29) | 32.7 ± 3.2 | 4.2 ± 0.7 | 43.2 ± 10.4 § (0.11) | 59.2 ± 2.1 | 57.5 ± 4.8 | 42.5 ± 4.8 | 22.7 ± 7.8 | 1409.2 ± 226.0 |
| T56-months | 491.0 ± 70.1 | 36.3 ± 0.6 | 4.3 ± 0.7 | 42.9 ± 9.6 | 59.1 ± 2.9 | 57.4 ± 4.6 | 42.6 ± 4.6 | 23.1 ± 8.1 | 1419.4 ± 235.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mascherini, G.; Ringressi, M.N.; Castizo-Olier, J.; Badicu, G.; Irurtia, A.; Stefani, L.; Galanti, G.; Taddei, A. Preliminary Results of an Exercise Program After Laparoscopic Resective Colorectal Cancer Surgery in Non-Metastatic Adenocarcinoma: A Pilot Study of a Randomized Control Trial. Medicina 2020, 56, 78. https://doi.org/10.3390/medicina56020078
Mascherini G, Ringressi MN, Castizo-Olier J, Badicu G, Irurtia A, Stefani L, Galanti G, Taddei A. Preliminary Results of an Exercise Program After Laparoscopic Resective Colorectal Cancer Surgery in Non-Metastatic Adenocarcinoma: A Pilot Study of a Randomized Control Trial. Medicina. 2020; 56(2):78. https://doi.org/10.3390/medicina56020078
Chicago/Turabian StyleMascherini, Gabriele, Maria Novella Ringressi, Jorge Castizo-Olier, Georgian Badicu, Alfredo Irurtia, Laura Stefani, Giorgio Galanti, and Antonio Taddei. 2020. "Preliminary Results of an Exercise Program After Laparoscopic Resective Colorectal Cancer Surgery in Non-Metastatic Adenocarcinoma: A Pilot Study of a Randomized Control Trial" Medicina 56, no. 2: 78. https://doi.org/10.3390/medicina56020078
APA StyleMascherini, G., Ringressi, M. N., Castizo-Olier, J., Badicu, G., Irurtia, A., Stefani, L., Galanti, G., & Taddei, A. (2020). Preliminary Results of an Exercise Program After Laparoscopic Resective Colorectal Cancer Surgery in Non-Metastatic Adenocarcinoma: A Pilot Study of a Randomized Control Trial. Medicina, 56(2), 78. https://doi.org/10.3390/medicina56020078








