Circulating Soluble Urokinase-Type Plasminogen Activator Receptor in Obstructive Sleep Apnoea
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
2.2. Sleep Studies
2.3. SuPAR Measurements
2.4. Statistical Analyses
3. Results
3.1. Patient Characteristics
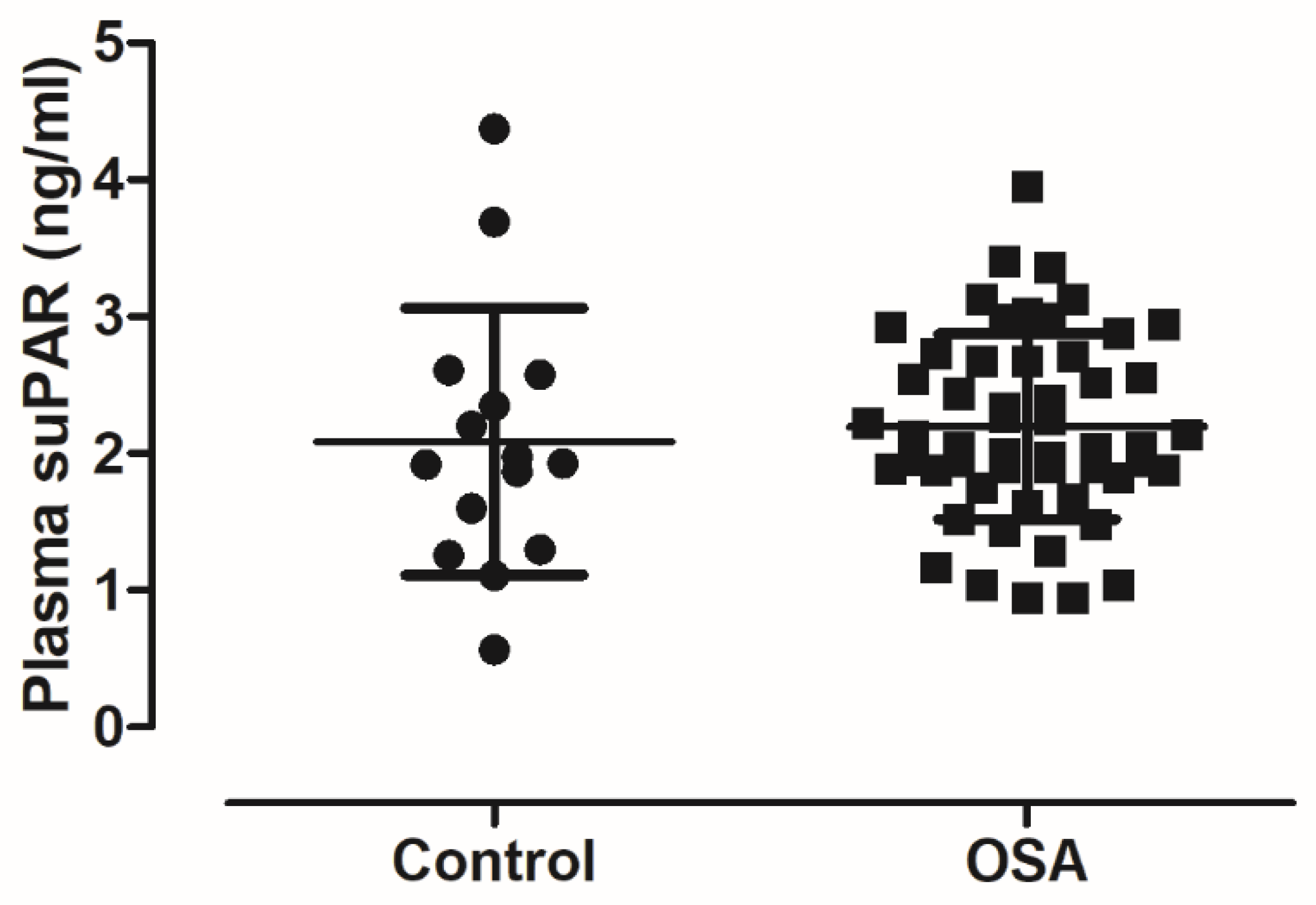
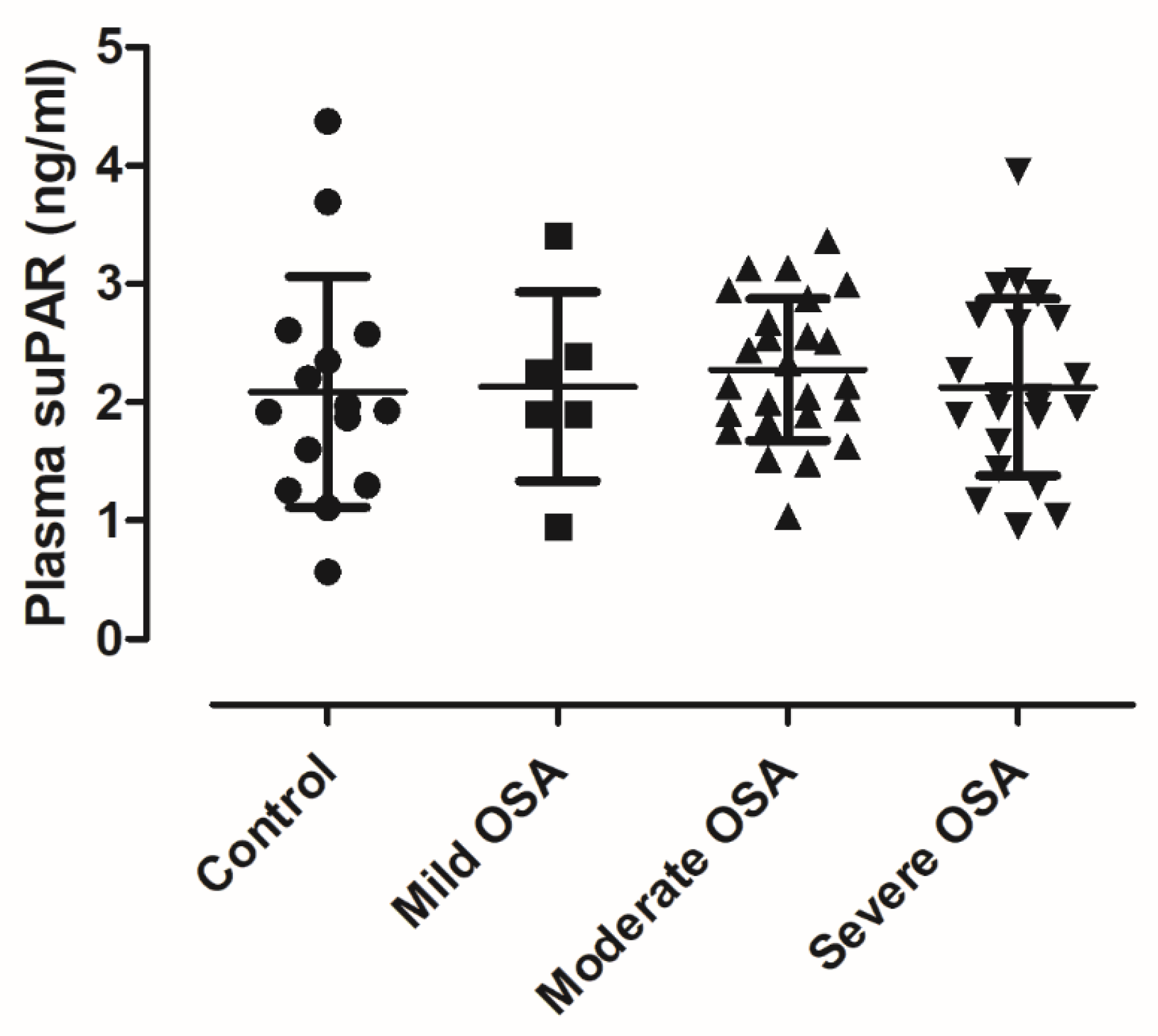
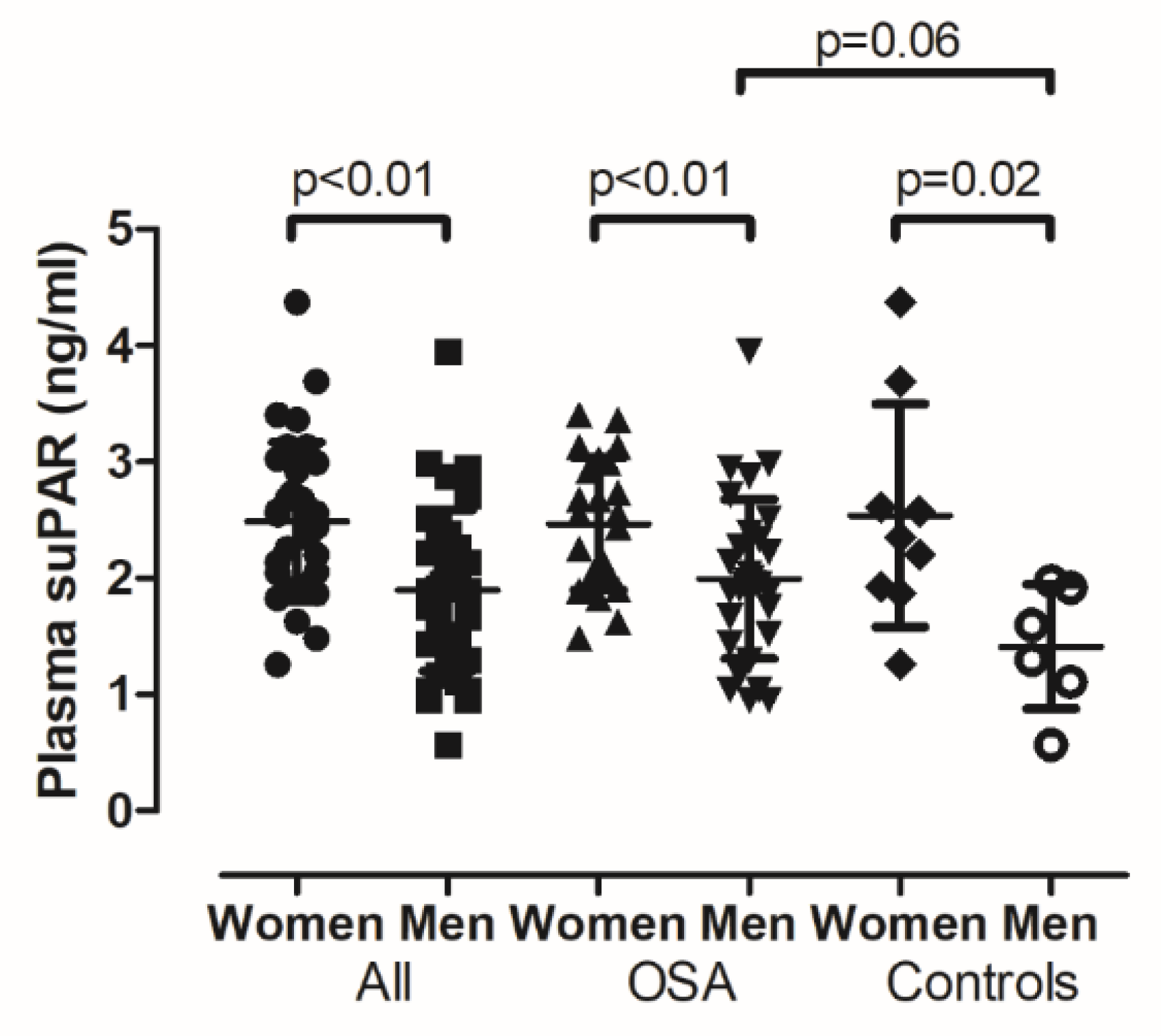
3.2. Circulating suPAR Results
3.3. Plasma suPAR Results in Control and OSA Participants without Hypertension or Diabetes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kent, B.D.; Ryan, S.; McNicholas, W.T. Obstructive sleep apnea and inflammation: Relationship to cardiovascular co-morbidity. Respir. Physiol. Neurobiol. 2011, 178, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Horvath, P.; Tarnoki, D.L.; Tarnoki, A.D.; Karlinger, K.; Lazar, Z.; Losonczy, G.; Kunos, L.; Bikov, A. Complement system activation in obstructive sleep apnea. J. Sleep Res. 2018, 27, e12674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kunos, L.; Horvath, P.; Kis, A.; Tarnoki, D.L.; Tarnoki, A.D.; Lazar, Z.; Bikov, A. Circulating Survivin Levels in Obstructive Sleep Apnoea. Lung 2018, 196, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Pako, J.; Kunos, L.; Meszaros, M.; Tarnoki, D.L.; Tarnoki, A.D.; Horvath, I.; Bikov, A. Decreased Levels of Anti-Aging Klotho in Obstructive Sleep Apnea. Rejuvenation Res. 2019. [Google Scholar] [CrossRef]
- Bagai, K.; Muldowney, J.A., 3rd; Song, Y.; Wang, L.; Bagai, J.; Artibee, K.J.; Vaughan, D.E.; Malow, B.A. Circadian variability of fibrinolytic markers and endothelial function in patients with obstructive sleep apnea. Sleep 2014, 37, 359–367. [Google Scholar] [CrossRef]
- Zakrzewski, M.; Zakrzewska, E.; Kicinski, P.; Przybylska-Kuc, S.; Dybala, A.; Myslinski, W.; Pastryk, J.; Tomaszewski, T.; Mosiewicz, J. Evaluation of Fibrinolytic Inhibitors: Alpha-2-Antiplasmin and Plasminogen Activator Inhibitor 1 in Patients with Obstructive Sleep Apnoea. PLoS ONE 2016, 11, e0166725. [Google Scholar] [CrossRef]
- Robinson, G.V.; Pepperell, J.C.; Segal, H.C.; Davies, R.J.; Stradling, J.R. Circulating cardiovascular risk factors in obstructive sleep apnoea: Data from randomised controlled trials. Thorax 2004, 59, 777–782. [Google Scholar] [CrossRef] [Green Version]
- Steffanina, A.; Proietti, L.; Antonaglia, C.; Palange, P.; Angelici, E.; Canipari, R. The Plasminogen System and Transforming Growth Factor-beta in Subjects With Obstructive Sleep Apnea Syndrome: Effects of CPAP Treatment. Respir. Care 2015, 60, 1643–1651. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Ortega, A.; Manas, E.; Lopez-Reyes, R.; Selma, M.J.; Garcia-Sanchez, A.; Oscullo, G.; Jimenez, D.; Martinez-Garcia, M.A. Obstructive sleep apnoea and venous thromboembolism: Pathophysiological links and clinical implications. Eur. Respir. J. 2019, 53. [Google Scholar] [CrossRef]
- Kohler, M.; Stradling, J.R. Mechanisms of vascular damage in obstructive sleep apnea. Nat. Rev. Cardiol. 2010, 7, 677–685. [Google Scholar] [CrossRef]
- Enocsson, H.; Sjowall, C.; Wettero, J. Soluble urokinase plasminogen activator receptor—A valuable biomarker in systemic lupus erythematosus? Clin. Chim. Acta Int. J. Clin. Chem. 2015, 444, 234–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donadello, K.; Scolletta, S.; Covajes, C.; Vincent, J.L. suPAR as a prognostic biomarker in sepsis. BMC Med. 2012, 10, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thuno, M.; Macho, B.; Eugen-Olsen, J. suPAR: The molecular crystal ball. Dis. Markers 2009, 27, 157–172. [Google Scholar] [CrossRef] [PubMed]
- Nykjaer, A.; Moller, B.; Todd, R.F., 3rd; Christensen, T.; Andreasen, P.A.; Gliemann, J.; Petersen, C.M. Urokinase receptor. An activation antigen in human T lymphocytes. J. Immunol. (Baltim. Md. 1950) 1994, 152, 505–516. [Google Scholar]
- Chavakis, T.; Willuweit, A.K.; Lupu, F.; Preissner, K.T.; Kanse, S.M. Release of soluble urokinase receptor from vascular cells. Thromb. Haemost. 2001, 86, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Eugen-Olsen, J. suPAR—A future risk marker in bacteremia. J. Intern. Med. 2011, 270, 29–31. [Google Scholar] [CrossRef]
- Masucci, M.T.; Pedersen, N.; Blasi, F. A soluble, ligand binding mutant of the human urokinase plasminogen activator receptor. J. Biol. Chem. 1991, 266, 8655–8658. [Google Scholar]
- Eapen, D.J.; Manocha, P.; Ghasemzadeh, N.; Patel, R.S.; Al Kassem, H.; Hammadah, M.; Veledar, E.; Le, N.A.; Pielak, T.; Thorball, C.W.; et al. Soluble urokinase plasminogen activator receptor level is an independent predictor of the presence and severity of coronary artery disease and of future adverse events. J. Am. Heart Assoc. 2014, 3, e001118. [Google Scholar] [CrossRef] [Green Version]
- Diederichsen, M.Z.; Diederichsen, S.Z.; Mickley, H.; Steffensen, F.H.; Lambrechtsen, J.; Sand, N.P.R.; Christensen, K.L.; Olsen, M.H.; Diederichsen, A.; Gronhoj, M.H. Prognostic value of suPAR and hs-CRP on cardiovascular disease. Atherosclerosis 2018, 271, 245–251. [Google Scholar] [CrossRef]
- Lyngbaek, S.; Sehestedt, T.; Marott, J.L.; Hansen, T.W.; Olsen, M.H.; Andersen, O.; Linneberg, A.; Madsbad, S.; Haugaard, S.B.; Eugen-Olsen, J.; et al. CRP and suPAR are differently related to anthropometry and subclinical organ damage. Int. J. Cardiol. 2013, 167, 781–785. [Google Scholar] [CrossRef]
- Cancello, R.; Rouault, C.; Guilhem, G.; Bedel, J.F.; Poitou, C.; Di Blasio, A.M.; Basdevant, A.; Tordjman, J.; Clement, K. Urokinase plasminogen activator receptor in adipose tissue macrophages of morbidly obese subjects. Obes. Facts 2011, 4, 17–25. [Google Scholar] [CrossRef] [PubMed]
- Peppard, P.E.; Young, T.; Barnet, J.H.; Palta, M.; Hagen, E.W.; Hla, K.M. Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol. 2013, 177, 1006–1014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- von Kanel, R.; Malan, N.T.; Hamer, M.; Lambert, G.W.; Schlaich, M.; Reimann, M.; Malan, L. Three-year changes of prothrombotic factors in a cohort of South Africans with a high clinical suspicion of obstructive sleep apnea. Thromb. Haemost. 2016, 115, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Berry, R.B.; Budhiraja, R.; Gottlieb, D.J.; Gozal, D.; Iber, C.; Kapur, V.K.; Marcus, C.L.; Mehra, R.; Parthasarathy, S.; Quan, S.F.; et al. Rules for scoring respiratory events in sleep: Update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J. Clin. Sleep Med. Off. Publ. Am. Acad. Sleep Med. 2012, 8, 597–619. [Google Scholar] [CrossRef] [Green Version]
- Bocskei, R.M.; Benczur, B.; Losonczy, G.; Illyes, M.; Cziraki, A.; Muller, V.; Bohacs, A.; Bikov, A. Soluble Urokinase-Type Plasminogen Activator Receptor and Arterial Stiffness in Patients with COPD. Lung 2019, 197, 189–197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baran, M.; Mollers, L.N.; Andersson, S.; Jonsson, I.M.; Ekwall, A.K.; Bjersing, J.; Tarkowski, A.; Bokarewa, M. Survivin is an essential mediator of arthritis interacting with urokinase signalling. J. Cell. Mol. Med. 2009, 13, 3797–3808. [Google Scholar] [CrossRef] [Green Version]
- Stavaras, C.; Pastaka, C.; Papala, M.; Gravas, S.; Tzortzis, V.; Melekos, M.; Seitanidis, G.; Gourgoulianis, K.I. Sexual function in pre- and post-menopausal women with obstructive sleep apnea syndrome. Int. J. Impot. Res. 2012, 24, 228–233. [Google Scholar] [CrossRef]
- Lund, L.R.; Ellis, V.; Ronne, E.; Pyke, C.; Dano, K. Transcriptional and post-transcriptional regulation of the receptor for urokinase-type plasminogen activator by cytokines and tumour promoters in the human lung carcinoma cell line A549. Biochem. J. 1995, 310, 345–352. [Google Scholar] [CrossRef]
- Shetty, S.; Idell, S. A urokinase receptor mRNA binding protein from rabbit lung fibroblasts and mesothelial cells. Am. J. Physiol. 1998, 274, L871–L882. [Google Scholar] [CrossRef]
- Sorensen, M.H.; Gerke, O.; Eugen-Olsen, J.; Munkholm, H.; Lambrechtsen, J.; Sand, N.P.; Mickley, H.; Rasmussen, L.M.; Olsen, M.H.; Diederichsen, A. Soluble urokinase plasminogen activator receptor is in contrast to high-sensitive C-reactive-protein associated with coronary artery calcifications in healthy middle-aged subjects. Atherosclerosis 2014, 237, 60–66. [Google Scholar] [CrossRef]
- Guan, Y.M.; Carlberg, M.; Bruse, C.; Carlstrom, K.; Bergqvist, A. Effects of hormones on uPA, PAI-1 and suPAR from cultured endometrial and ovarian endometriotic stromal cells. Acta Obstet. Gynecol. Scand. 2002, 81, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.M.; Davidson, T.M.; Ancoli-Israel, S. Gender differences in obstructive sleep apnea and treatment implications. Sleep Med. Rev. 2008, 12, 481–496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsai, M.S.; Lee, L.A.; Tsai, Y.T.; Yang, Y.H.; Liu, C.Y.; Lin, M.H.; Hsu, C.M.; Chen, C.K.; Li, H.Y. Sleep apnea and risk of vertigo: A nationwide population-based cohort study. Laryngoscope 2018, 128, 763–768. [Google Scholar] [CrossRef] [PubMed]
- Andersen, O.; Eugen-Olsen, J.; Kofoed, K.; Iversen, J.; Haugaard, S.B. Soluble urokinase plasminogen activator receptor is a marker of dysmetabolism in HIV-infected patients receiving highly active antiretroviral therapy. J. Med Virol. 2008, 80, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Eugen-Olsen, J.; Andersen, O.; Linneberg, A.; Ladelund, S.; Hansen, T.W.; Langkilde, A.; Petersen, J.; Pielak, T.; Moller, L.N.; Jeppesen, J.; et al. Circulating soluble urokinase plasminogen activator receptor predicts cancer, cardiovascular disease, diabetes and mortality in the general population. J. Intern. Med. 2010, 268, 296–308. [Google Scholar] [CrossRef] [PubMed]
- Mazzotti, D.R.; Keenan, B.T.; Lim, D.C.; Gottlieb, D.J.; Kim, J.; Pack, A.I. Symptom Subtypes of Obstructive Sleep Apnea Predict Incidence of Cardiovascular Outcomes. Am. J. Respir. Crit. Care Med. 2019, 200, 493–506. [Google Scholar] [CrossRef] [PubMed]
- Chiu, H.Y.; Chen, P.Y.; Chuang, L.P.; Chen, N.H.; Tu, Y.K.; Hsieh, Y.J.; Wang, Y.C.; Guilleminault, C. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth sleepiness scale in detecting obstructive sleep apnea: A bivariate meta-analysis. Sleep Med. Rev. 2017, 36, 57–70. [Google Scholar] [CrossRef]
| Control (n = 15) | OSA (n = 53) | Total (n = 68) | p | |
|---|---|---|---|---|
| Age (years) | 48/31–62/ | 59/49–64/ | 54.6/44–64/ | 0.08 |
| Male (n, %) | 6, 40% | 30, 57% | 36, 53% | 0.26 |
| BMI (kg/m2) | 24.6±4.58 | 32.37±5.66 | 30.66±6.31 | <0.01 |
| Hypertension (%) | 33 | 70 | 62 | 0.01 |
| Diabetes (%) | 0 | 13 | 10 | 0.14 |
| Dyslipidaemia (%) | 27 | 53 | 47 | 0.07 |
| Cardiovascular disease (%) | 13 | 11 | 12 | 0.83 |
| Cardiac arrhythmia (%) | 13 | 26 | 24 | 0.29 |
| Smokers (%) | 20 | 23 | 22 | 0.83 |
| Subjects taking anticoagulants (%) | 0 | 11 | 10 | 0.32 |
| Subjects taking antithrombotic drugs (%) | 13 | 11 | 12 | 1.00 |
| SBP (mmHg) | 120/118–131/ | 138/130–150/ | 132/120–140/ | <0.01 |
| DBP (mmHg) | 70/70–75/ | 85/76–90/ | 80/70–90/ | <0.01 |
| Creatinine (mmol/L) | 77.5/66.3–83.5/ | 66/61–79/ | 70.0/62.0–82.5/ | 0.17 |
| GFR (mL/min/1.73m2) | 82.26±15.17 | 88.37±17.91 | 86.75±17.3 | 0.26 |
| CRP (mg/L) | 2.34/0.92–3.95/ | 3.0/1.36–4.65/ | 3.0/1.33–4.48/ | 0.23 |
| Glucose (mmol/L) | 4.65/4.1–5.3/ | 5.2/4.8–6.1/ | 5.1/4.7–5.7/ | 0.05 |
| Cholesterol (mmol/L) | 5.91±1.04 | 5.33±1.13 | 5.46±1.13 | 0.08 |
| HDL-C (mmol/L) | 1.84/1.58–2.34/ | 1.28/1.06–1.62/ | 1.36/1.17–1.82/ | <0.01 |
| LDL-C (mmol/L) | 3.41±0.89 | 3.16±1.02 | 3.22±0.99 | 0.39 |
| Triglyceride (mmol/L) | 1.23/0.94–1.32/ | 1.33/1.07–1.97/ | 1.28/1.04–1.92/ | 0.10 |
| Lipoprotein (a) (mmol/L) | 0.2/0.0–0.4/ | 0.17/0.10–0.49/ | 0.18/0.07–0.44/ | 0.56 |
| AHI (1/h) | 1.6/1.0–2.4/ | 27.5/18.55–42.75/ | 21.89/8.9–40.63/ | <0.01 |
| ODI (1/h) | 0.9/0.4–1.7/ | 23.2/14.1–38.95/ | 19.65/6.2–32/ | <0.01 |
| SPT (min) | 395.19±36.1 | 439.93±72.82 | 427.81±67.62 | 0.04 |
| TST (min) | 398/319–409.5/ | 428/384.5–452/ | 410.5/363.25–440.75/ | <0.01 |
| TST90% (%) | 0.0/0.0–0.1/ | 6/1.7–12.5/ | 3.85/0.4–11.6/ | <0.01 |
| Minimal oxygen saturation (%) | 91/88.25–92.75/ | 82.5/76.8–85/ | 83/77.8–88/ | <0.01 |
| ESS | 5.0/2.75–7.0/ | 7/5–10/ | 6/4–8/ 6.6±3.68 | 0.05 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bocskei, R.M.; Meszaros, M.; Tarnoki, A.D.; Tarnoki, D.L.; Kunos, L.; Lazar, Z.; Bikov, A. Circulating Soluble Urokinase-Type Plasminogen Activator Receptor in Obstructive Sleep Apnoea. Medicina 2020, 56, 77. https://doi.org/10.3390/medicina56020077
Bocskei RM, Meszaros M, Tarnoki AD, Tarnoki DL, Kunos L, Lazar Z, Bikov A. Circulating Soluble Urokinase-Type Plasminogen Activator Receptor in Obstructive Sleep Apnoea. Medicina. 2020; 56(2):77. https://doi.org/10.3390/medicina56020077
Chicago/Turabian StyleBocskei, Renata Marietta, Martina Meszaros, Adam Domonkos Tarnoki, David Laszlo Tarnoki, Laszlo Kunos, Zsofia Lazar, and Andras Bikov. 2020. "Circulating Soluble Urokinase-Type Plasminogen Activator Receptor in Obstructive Sleep Apnoea" Medicina 56, no. 2: 77. https://doi.org/10.3390/medicina56020077
APA StyleBocskei, R. M., Meszaros, M., Tarnoki, A. D., Tarnoki, D. L., Kunos, L., Lazar, Z., & Bikov, A. (2020). Circulating Soluble Urokinase-Type Plasminogen Activator Receptor in Obstructive Sleep Apnoea. Medicina, 56(2), 77. https://doi.org/10.3390/medicina56020077









