Analysis of Alveolar Bone Morphology of the Maxillary Central and Lateral Incisors with Normal Occlusion
Abstract
1. Introduction
2. Experimental Section
2.1. Participants
2.2. Image Processing
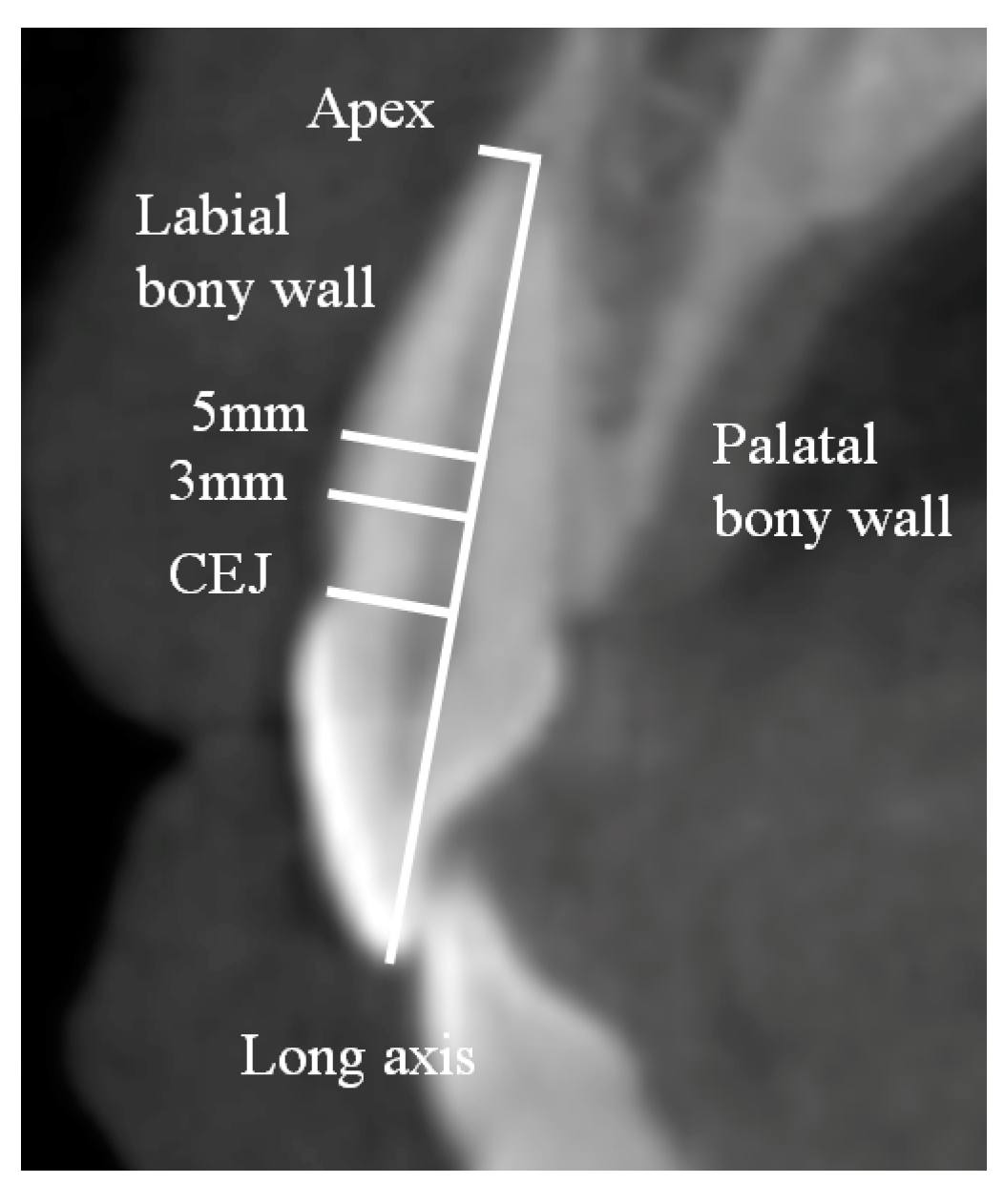
2.3. Measurements
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lee, J.E.; Lee, Y.J.; Jin, S.H.; Kim, Y.; Kook, Y.A.; Ko, Y.; Park, J.B. Topographic analysis of the mandibular symphysis in a normal occlusion population using cone-beam computed tomography. Exp. Ther. Med. 2015, 10, 2150–2156. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Rathee, S.; Agarwal, J.; Pachar, R.B. Measurement of Crestal Cortical Bone Thickness at Implant Site: A Cone Beam Computed Tomography Study. J. Contemp. Dent. Pract. 2017, 18, 785–789. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Skrypczak, A.; Weltman, R. Anterior maxilla alveolar ridge dimension and morphology measurement by cone beam computerized tomography (CBCT) for immediate implant treatment planning. BMC Oral Health 2015, 15, 65. [Google Scholar] [CrossRef] [PubMed]
- Braut, V.; Bornstein, M.M.; Belser, U.; Buser, D. Thickness of the anterior maxillary facial bone wall-a retrospective radiographic study using cone beam computed tomography. Int. J. Periodont. Restorative Dent. 2011, 31, 125–131. [Google Scholar] [PubMed]
- Dau, M.; Edalatpour, A.; Schulze, R.; Al-Nawas, B.; Alshihri, A.; Kammerer, P.W. Presurgical evaluation of bony implant sites using panoramic radiography and cone beam computed tomography-influence of medical education. Dentomaxillofac. Radiol. 2017, 46, 20160081. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.H.; Wang, H.L. Reliability of volumetric imaging software for cone-beam computed tomogram scans in the anterior maxilla. Implant Dent. 2013, 22, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Ko, Y.C.; Huang, H.L.; Shen, Y.W.; Cai, J.Y.; Fuh, L.J.; Hsu, J.T. Variations in crestal cortical bone thickness at dental implant sites in different regions of the jawbone. Clin. Implant Dent. Relat. Res. 2017, 19, 440–446. [Google Scholar] [CrossRef]
- Kook, Y.A.; Kim, G.; Kim, Y. Comparison of alveolar bone loss around incisors in normal occlusion samples and surgical skeletal class III patients. Angle Orthod. 2012, 82, 645–652. [Google Scholar] [CrossRef]
- Tian, Y.L.; Liu, F.; Sun, H.J.; Lv, P.; Cao, Y.M.; Yu, M.; Yue, Y. Alveolar bone thickness around maxillary central incisors of different inclination assessed with cone-beam computed tomography. Korean J. Orthod. 2015, 45, 245–252. [Google Scholar] [CrossRef]
- Gracco, A.; Lombardo, L.; Mancuso, G.; Gravina, V.; Siciliani, G. Upper incisor position and bony support in untreated patients as seen on CBCT. Angle Orthod. 2009, 79, 692–702. [Google Scholar] [CrossRef]
- Jin, S.H.; Park, J.B.; Kim, N.; Park, S.; Kim, K.J.; Kim, Y.; Kook, Y.A.; Ko, Y. The thickness of alveolar bone at the maxillary canine and premolar teeth in normal occlusion. J. Periodontal. Implant Sci. 2012, 42, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Park, J.B.; Lee, J.E.; Kim, K.; Yoo, J.T.; Kim, Y.; Kook, Y.A.; Ko, Y. The thickness of alveolar bone at the mandibular canine and premolar teeth in normal occlusion. J. Craniofac. Surg. 2014, 25, 1115–1119. [Google Scholar] [CrossRef] [PubMed]
- AlTarawneh, S.; AlHadidi, A.; Hamdan, A.A.; Shaqman, M.; Habib, E. Assessment of Bone Dimensions in the Anterior Maxilla: A Cone Beam Computed Tomography Study. J. Prosthodont. 2018, 27, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Farahamnd, A.; Sarlati, F.; Eslami, S.; Ghassemian, M.; Youssefi, N.; Jafarzadeh Esfahani, B. Evaluation of Impacting Factors on Facial Bone Thickness in the Anterior Maxillary Region. J. Craniofac. Surg. 2017, 28, 700–705. [Google Scholar] [CrossRef] [PubMed]
- Gluckman, H.; Pontes, C.C.; Du Toit, J. Radial plane tooth position and bone wall dimensions in the anterior maxilla: A CBCT classification for immediate implant placement. J. Prosthet. Dent. 2018, 120, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D.J.; Swenson, D.T.; Johnson, T.M. Buccal bone thickness adjacent to virtual dental implants following guided bone regeneration. J. Periodontol. 2019, 90, 595–607. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Zhou, T.; Zhou, N.; Man, Y. The thickness of labial bone affects the esthetics of immediate implant placement and provisionalization in the esthetic zone: A prospective cohort study. Clin. Implant Dent. Relat. Res. 2019, 21, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Gakonyo, J.; Mohamedali, A.J.; Mungure, E.K. Cone Beam Computed Tomography Assessment of the Buccal Bone Thickness in Anterior Maxillary Teeth: Relevance to Immediate Implant Placement. Int. J. Oral Maxillofac. Implants 2018, 33, 880–887. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Noh, K.; Al-Nawas, B.; Kwon, Y.D. A 10-Year Cone Beam Computerized Tomography Observation of the Buccal Bony Wall of an Immediately Placed Implant at the Anterior Maxilla: A Case Report. J. Oral Implantol. 2018, 44, 213–217. [Google Scholar] [CrossRef]
- Barroso-Panella, A.; Gargallo-Albiol, J.; Hernandez-Alfaro, F. Evaluation of Bone Stability and Esthetic Results After Immediate Implant Placement Using a Novel Synthetic Bone Substitute in the Anterior Zone: Results After 12 Months. Int. J. Periodont. Restorative Dent. 2018, 38, 235–243. [Google Scholar] [CrossRef]
- De Bruyckere, T.; Eeckhout, C.; Eghbali, A.; Younes, F.; Vandekerckhove, P.; Cleymaet, R.; Cosyn, J. A randomized controlled study comparing guided bone regeneration with connective tissue graft to re-establish convexity at the buccal aspect of single implants: A one-year CBCT analysis. J. Clin. Periodontol. 2018, 45, 1375–1387. [Google Scholar] [CrossRef] [PubMed]
- Song, W.K.; Kang, J.H.; Cha, J.K.; Lee, J.S.; Paik, J.W.; Jung, U.W.; Kim, B.H.; Choi, S.H. Biomimetic characteristics of mussel adhesive protein-loaded collagen membrane in guided bone regeneration of rabbit calvarial defects. J. Periodontal. Implant Sci. 2018, 48, 305–316. [Google Scholar] [CrossRef] [PubMed]
- Baumer, D.; Zuhr, O.; Rebele, S.; Hurzeler, M. Socket Shield Technique for immediate implant placement-clinical, radiographic and volumetric data after 5 years. Clin. Oral Implants Res. 2017, 28, 1450–1458. [Google Scholar] [CrossRef]
- Zhang, C.Y.; DeBaz, C.; Bhandal, G.; Alli, F.; Buencamino Francisco, M.C.; Thacker, H.L.; Palomo, J.M.; Palomo, L. Buccal Bone Thickness in the Esthetic Zone of Postmenopausal Women: A CBCT Analysis. Implant Dent. 2016, 25, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Ghassemian, M.; Nowzari, H.; Lajolo, C.; Verdugo, F.; Pirronti, T.; D’Addona, A. The thickness of facial alveolar bone overlying healthy maxillary anterior teeth. J. Periodontol. 2012, 83, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Januario, A.L.; Duarte, W.R.; Barriviera, M.; Mesti, J.C.; Araujo, M.G.; Lindhe, J. Dimension of the facial bone wall in the anterior maxilla: A cone-beam computed tomography study. Clin. Oral Implants Res. 2011, 22, 1168–1171. [Google Scholar] [CrossRef]
- Bulyalert, A.; Pimkhaokham, A. A novel classification of anterior alveolar arch forms and alveolar bone thickness: A cone-beam computed tomography study. Imaging Sci. Dent. 2018, 48, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Shelley, A.; Tinning, J.; Yates, J.; Horner, K. Potential neurovascular damage as a result of dental implant placement in the anterior maxilla. Br. Dent. J. 2019, 226, 657–661. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.Y.; Pan, W.L.; Wang, H.L. Facial Fenestration and Dehiscence Defects Associated with Immediate Implant Placement without Flap Elevation in Anterior Maxillary Ridge: A Preliminary Cone Beam Computed Tomography Study. Int. J. Oral Maxillofac. Implants 2018, 33, 1112–1118. [Google Scholar] [CrossRef]
- Nikiforidou, M.; Tsalikis, L.; Angelopoulos, C.; Menexes, G.; Vouros, I.; Konstantinides, A. Classification of periodontal biotypes with the use of CBCT. A cross-sectional study. Clin. Oral Investig. 2016, 20, 2061–2071. [Google Scholar] [CrossRef]
- Esfahanizadeh, N.; Daneshparvar, N.; Askarpour, F.; Akhoundi, N.; Panjnoush, M. Correlation between Bone and Soft Tissue Thickness in Maxillary Anterior Teeth. J. Dent. (Tehran). 2016, 13, 302–308. [Google Scholar]
- Pauwels, R.; Jacobs, R.; Singer, S.R.; Mupparapu, M. CBCT-based bone quality assessment: Are Hounsfield units applicable? Dentomaxillofac. Radiol. 2015, 44, 20140238. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, M.; Stefanelli, L.V.; Pacifici, A.; Pacifici, L.; Barbato, E. How accurate is CBCT in measuring bone density? A comparative CBCT-CT in vitro study. Clin. Implant Dent. Relat. Res. 2014, 16, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; An, X.; Jeong, S.M.; Choi, B.H. Accuracy of computer-guided implant placement in anterior regions. J. Prosthet. Dent. 2019, 121, 836–842. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Li, J.; Sinjab, K.; Mendonca, G.; Yu, H.; Wang, H.L. Accuracy of flapless immediate implant placement in anterior maxilla using computer-assisted versus freehand surgery: A cadaver study. Clin. Oral Implants Res. 2018, 29, 1186–1194. [Google Scholar] [CrossRef] [PubMed]
- Joshi, V.; Gupta, S. Immediate Implant Placement in Anterior Aesthetic Region and Assessment using Cone-Beam Computed Tomography Scan Technology. J. Int. Oral Health 2015, 7, 99–102. [Google Scholar] [PubMed]
- Chung, M.P.; Wang, I.C.; Chan, H.L.; Wang, H.L. Evaluation of Buccal Bone Concavity in the Esthetic Zone: A Cadaver Study. Implant. Dent. 2017, 26, 751–755. [Google Scholar] [CrossRef] [PubMed]
- Yodthong, N.; Charoemratrote, C.; Leethanakul, C. Factors related to alveolar bone thickness during upper incisor retraction. Angle Orthod. 2013, 83, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Mandelaris, G.A.; Neiva, R.; Chambrone, L. Cone-Beam Computed Tomography and Interdisciplinary Dentofacial Therapy: An American Academy of Periodontology Best Evidence Review Focusing on Risk Assessment of the Dentoalveolar Bone Changes Influenced by Tooth Movement. J. Periodontol. 2017, 88, 960–977. [Google Scholar] [CrossRef]
| Parameter | Central Incisor | Lateral Incisor | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CEJ 3 mm | CEJ 5 mm | Root Apex | Root Tip-Apical Bone | Angulation | CEJ 3 mm | CEJ 5 mm | Root Apex | Root Tip-Apical Bone | Angulation | |
| Mean | 1.1 | 1.0 | 2.3 *,** | 10.4 | 12.4 | 1.2 | 1.0 | 2.2 #,## | 10.5 | 13.3 |
| Median | 1.2 | 1.0 | 2.3 | 9.6 | 12.1 | 1.1 | 1.0 | 2.1 | 10.3 | 13.1 |
| Maximum | 1.9 | 2.0 | 3.9 | 17.5 | 16.7 | 1.9 | 1.9 | 4.4 | 16.1 | 16.0 |
| Minimum | 0.3 | 0.1 | 0.8 | 7.5 | 8.0 | 0.3 | 0.4 | 0.6 | 5.5 | 10.7 |
| SD | 0.3 | 0.4 | 0.8 | 2.7 | 1.9 | 0.4 | 0.4 | 0.8 | 2.2 | 1.3 |
| Parameter | Central Incisor | Lateral Incisor | ||||
|---|---|---|---|---|---|---|
| CEJ 3 mm | CEJ 5 mm | Root apex | CEJ 3 mm | CEJ 5 mm | Root apex | |
| Mean | 1.9 | 2.7 * | 7.5 *,** | 1.5 | 2.2 # | 6.1 #,## |
| Median | 1.8 | 2.7 | 7.3 | 1.5 | 2.1 | 6.1 |
| Maximum | 3.6 | 4.4 | 11.2 | 3.1 | 3.9 | 11.1 |
| Minimum | 0.6 | 1.4 | 4.7 | 0.6 | 0.5 | 2.1 |
| SD | 0.6 | 0.7 | 1.7 | 0.5 | 0.7 | 1.7 |
| Tooth | Location | Thickness < 1 mm | 1 mm ≤ Thickness < 2 mm | Thickness ≥ 2 mm |
|---|---|---|---|---|
| Central incisor | CEJ 3 mm | 32.5 | 67.5 | 0.0 |
| CEJ 5 mm | 45.0 | 52.5 | 2.5 | |
| Root apex | 2.5 | 35.0 | 62.5 | |
| Lateral incisor | CEJ 3 mm | 32.5 | 67.5 | 0.0 |
| CEJ 5 mm | 47.5 | 52.5 | 0.0 | |
| Root apex | 2.5 | 42.5 | 55.0 |
| Tooth | Location | Thickness < 1 mm | 1 mm ≤ Thickness < 2 mm | Thickness ≥ 2 mm |
|---|---|---|---|---|
| Central incisor | CEJ 3 mm | 5.0 | 57.5 | 37.5 |
| CEJ 5 mm | 0.0 | 22.5 | 77.5 | |
| Root apex | 0.0 | 0.0 | 100.0 | |
| Lateral incisor | CEJ 3 mm | 10 | 75 | 15 |
| CEJ 5 mm | 2.5 | 32.5 | 65 | |
| Root apex | 0 | 0 | 100 |
| Tooth | Topology | Labial | Palatal | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CEJ 3 mm | CEJ 5 mm | Apex | Root Tip-Apical Bone | Angulation | CEJ 3 mm | CEJ 5 mm | Apex | ||
| Central incisor | Right | 1.1 ± 0.4 | 1.0 ± 0.4 | 2.3 ± 0.8 | 10.5 ± 2.3 | 12.4 ± 1.7 | 2.0 ± 0.7 | 2.7 ± 0.8 | 7.5 ± 1.8 |
| Left | 1.1 ± 0.3 | 1.0 ± 0.4 | 2.3 ± 0.8 | 10.3 ± 2.7 | 12.4 ± 2.1 | 1.8 ± 0.5 | 2.6 ± 0.7 | 7.5 ± 1.7 | |
| p-value | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | |
| Lateral incisor | Right | 1.3 ± 0.3 | 1.1 ± 0.4 | 2.1 ± 0.7 | 10.2 ± 2.1 | 13.8 ± 1.2 | 1.7 ± 0.5 | 2.4 ± 0.7 | 6.1 ± 1.5 |
| Left | 1.0 ± 0.4 * | 1.0 ± 0.4 | 2.2 ± 0.8 | 10.9 ± 2.3 | 12.8 ± 1.2 | 1.4 ± 0.4 * | 2.1 ± 0.7 | 6.0 ± 1.9 | |
| p-value | 0.000 | >0.05 | >0.05 | >0.05 | 0.007 | 0.019 | 0.094 | 0.838 | |
| Tooth | Gender | Labial | Palatal | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CEJ 3 mm | CEJ 5 mm | Apex | Root Tip-Apical Bone | Angulation | CEJ 3 mm | CEJ 5 mm | Apex | ||
| Central incisor | Male | 1.3 ± 0.3 | 1.1 ± 0.4 | 2.5 ± 0.9 | 10.7 ± 3.1 | 12.7 ± 2.2 | 2.1 ± 0.7 | 2.8 ± 0.8 | 7.8 ± 1.4 |
| Female | 1.0 ± 0.3 * | 0.9 ± 0.4 * | 2.2 ± 0.6 | 10.2 ± 2.4 | 12.2 ± 1.62 | 1.7 ± 0.5 | 2.5 ± 0.7 | 7.2 ± 1.9 | |
| p-value | 0.000 | 0.045 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | |
| Lateral incisor | Male | 1.4 ± 0.4 | 1.2 ± 0.3 | 2.4 ± 0.9 | 10.8 ± 2.6 | 13.4 ± 21.4 | 1.6 ± 0.5 | 2.2 ± 0.6 | 7.0 ± 1.4 |
| Female | 1.0 ± 0.3 * | 0.9 ± 0.3 * | 2.0 ± 0.6 | 10.3 ± 1.9 | 13.2 ± 1.2 | 1.5 ± 0.4 | 2.2 ± 0.8 | 5.3 ± 1.6 * | |
| p-value | 0.002 | 0.001 | >0.05 | >0.05 | >0.05 | >0.05 | >0.05 | 0.002 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.-E.; Jung, C.Y.; Kim, Y.; Kook, Y.-A.; Ko, Y.; Park, J.-B. Analysis of Alveolar Bone Morphology of the Maxillary Central and Lateral Incisors with Normal Occlusion. Medicina 2019, 55, 565. https://doi.org/10.3390/medicina55090565
Lee J-E, Jung CY, Kim Y, Kook Y-A, Ko Y, Park J-B. Analysis of Alveolar Bone Morphology of the Maxillary Central and Lateral Incisors with Normal Occlusion. Medicina. 2019; 55(9):565. https://doi.org/10.3390/medicina55090565
Chicago/Turabian StyleLee, Ji-Eun, Chang Yoon Jung, Yoonji Kim, Yoon-Ah Kook, Youngkyung Ko, and Jun-Beom Park. 2019. "Analysis of Alveolar Bone Morphology of the Maxillary Central and Lateral Incisors with Normal Occlusion" Medicina 55, no. 9: 565. https://doi.org/10.3390/medicina55090565
APA StyleLee, J.-E., Jung, C. Y., Kim, Y., Kook, Y.-A., Ko, Y., & Park, J.-B. (2019). Analysis of Alveolar Bone Morphology of the Maxillary Central and Lateral Incisors with Normal Occlusion. Medicina, 55(9), 565. https://doi.org/10.3390/medicina55090565






