Handheld Ultrasound and Focused Cardiovascular Echography: Use and Information
Abstract
1. Introduction
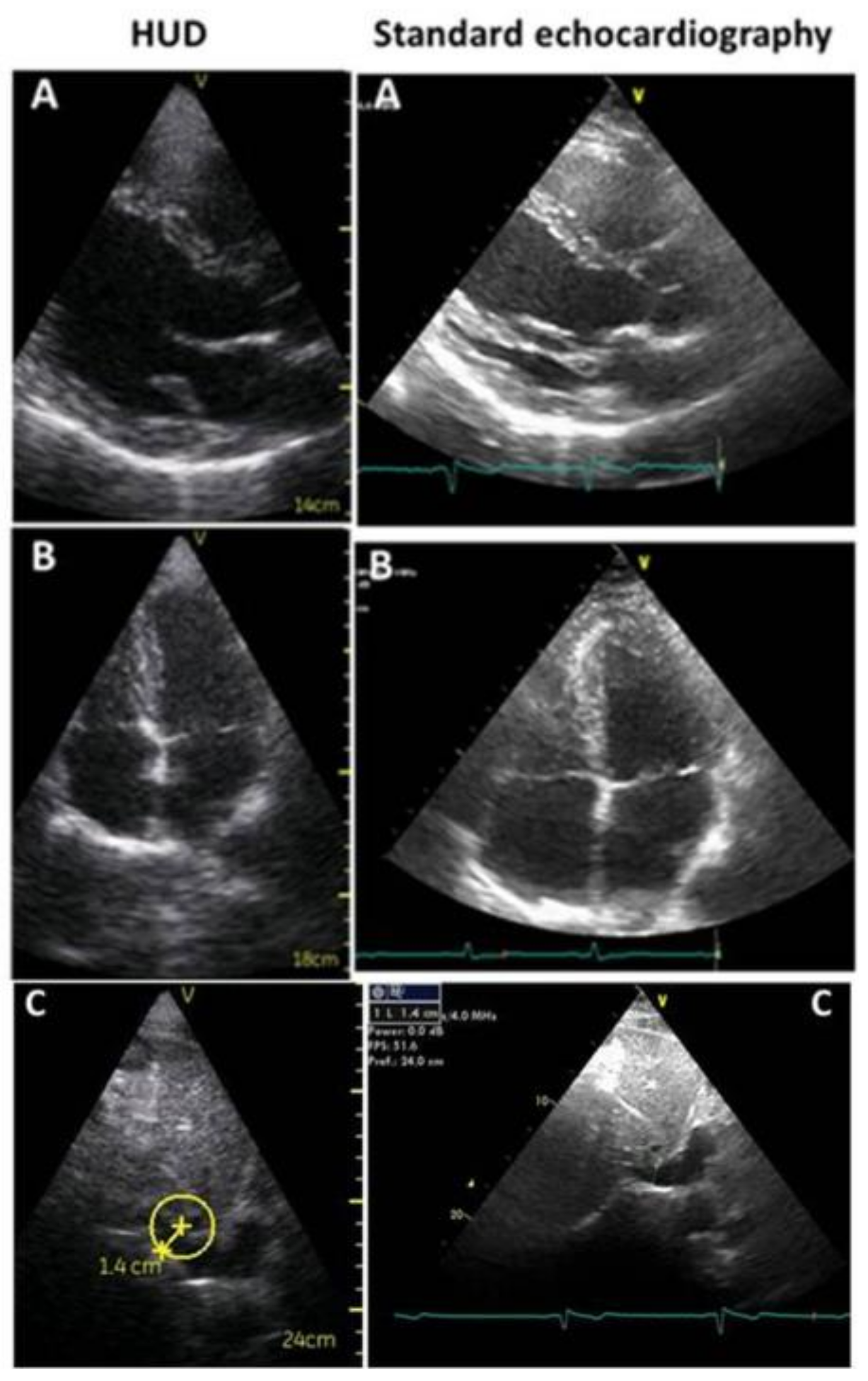
2. Differentiation of the Various Echocardiographic Equipment: From Standard, Comprehensive Transthoracic Echocardiography to Focused Cardiac Ultrasound
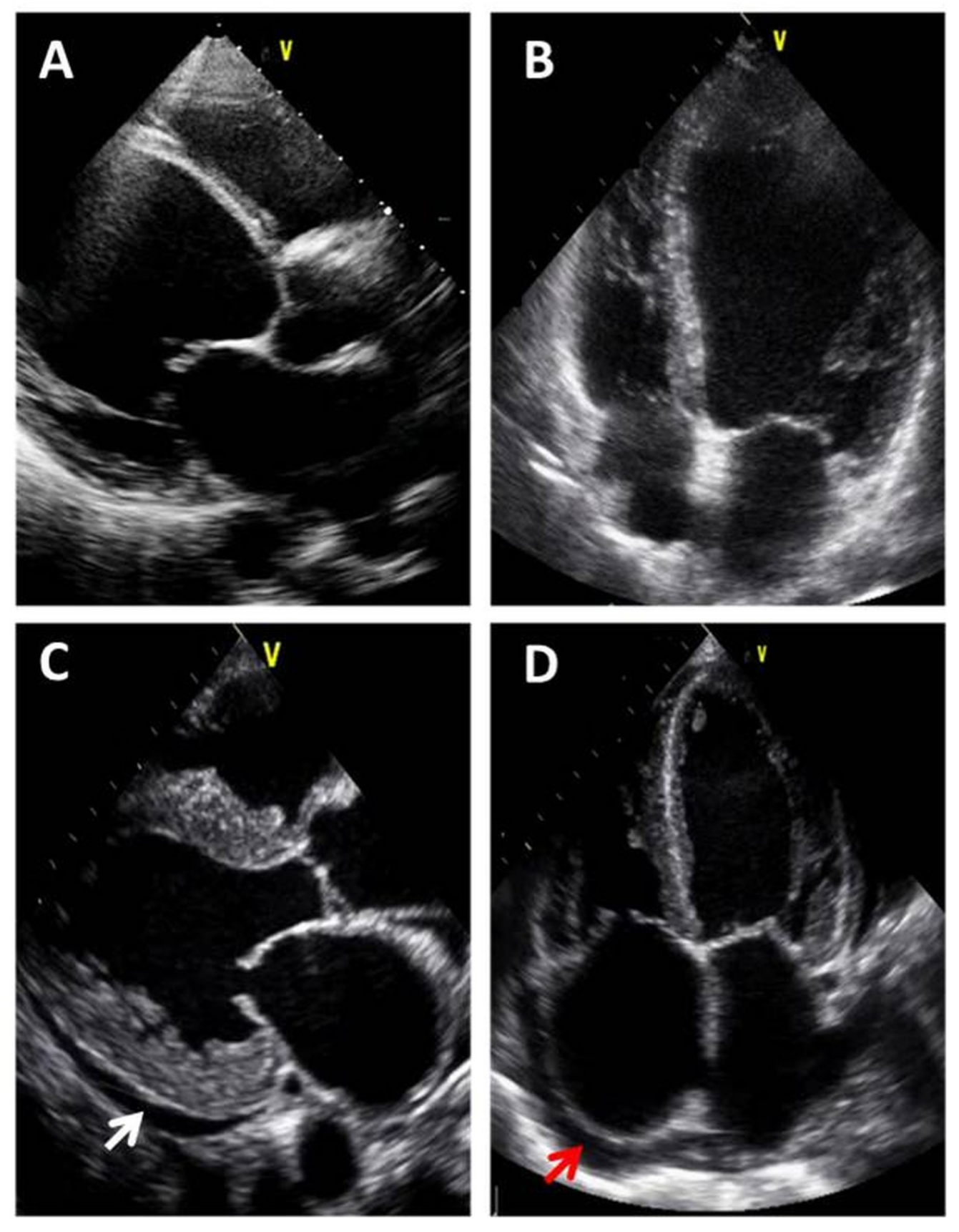
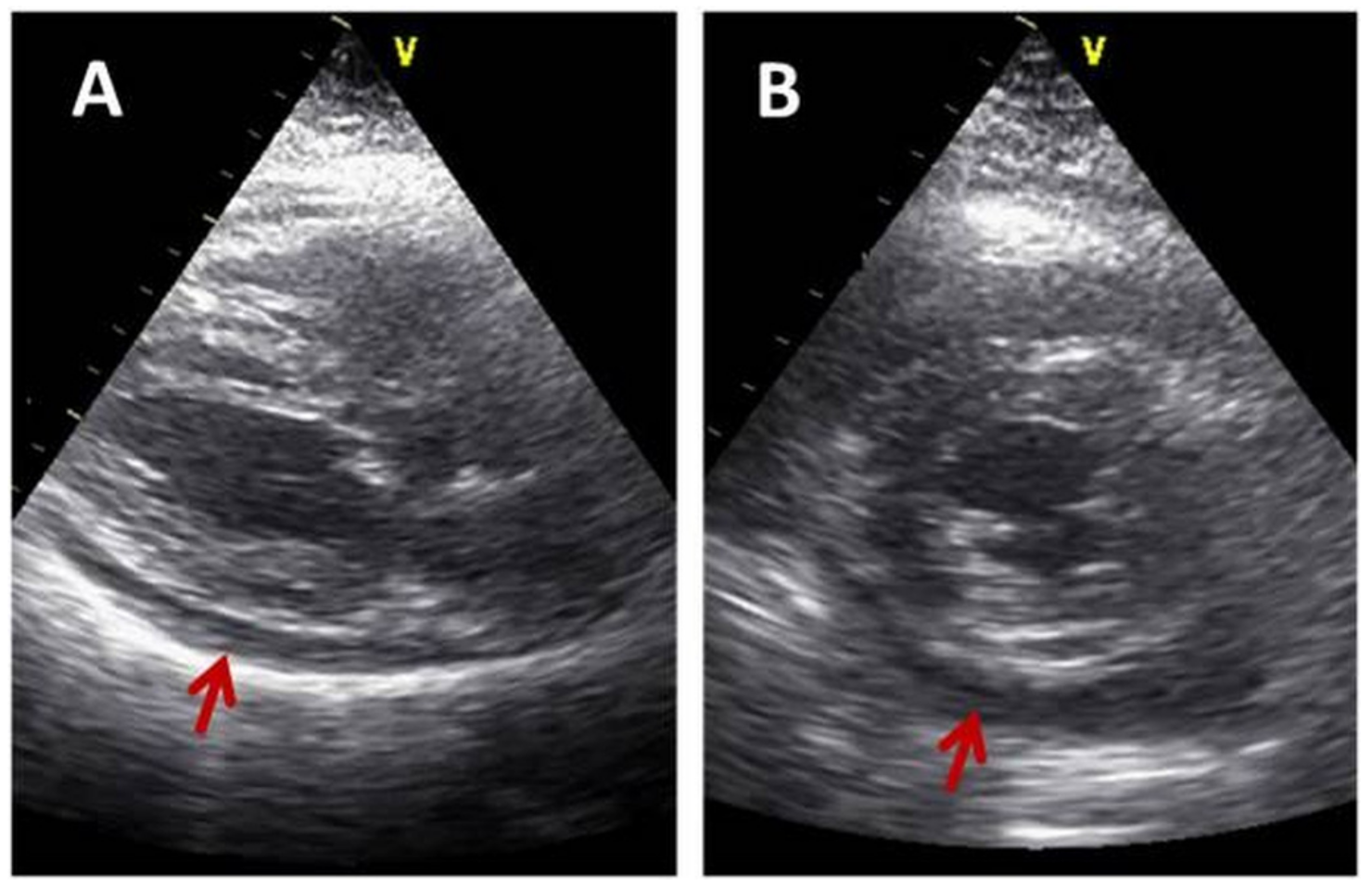
3. Focused-Echo in Various Clinical Scenarios: When to Use It
4. Specialties That Use HUDs and Training of Operators
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Mitchell, C.; Rahko, P.S.; Blauwet, L.A.; Canaday, B.; Finstuen, J.A.; Foster, M.C.; Horton, K.; Ogunyankin, K.O.; Palma, R.A.; Velazquez, E.J. Guidelines for Performing a Comprehensive Transthoracic Echocardiographic Examination in Adults: Recommendations from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2019, 32, 1–64. [Google Scholar] [CrossRef]
- Douglas, P.S.; Khandheria, B.J.; Stainback, R.F. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 appropriateness criteria for transthoracic and transesophageal echocardiography: A report of the American College of Cardiology Foundation Quality strategic directions committee appropriateness criteria working group, American Society of Echocardiography, American College of Emergency Physicians, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society for Cardiovascular Magnetic Resonance. Endorsed by the American College of Chest Physicians and the Society of Critical Care Medicine. J. Am. Soc. Echocardiogr. 2007, 20, 787–805. [Google Scholar] [CrossRef]
- Chamsi-Pasha, M.A.; Sengupta, P.P.; Zoghbi, W.A. Handheld Echocardiography. Circulation 2017, 136, 2178–2188. [Google Scholar] [CrossRef]
- Picard, M.H.; Adams, D.; Bierig, S.M.; Dent, J.M.; Douglas, P.S.; Gillam, L.D.; Keller, A.M.; Malenka, D.J.; Masoudi, F.A.; McCulloch, M.; et al. American Society of Echocardiography Recommendations for Quality Echocardiography Laboratory Operations. J. Am. Soc. Echocardiogr. 2011, 24, 1–10. [Google Scholar] [CrossRef]
- Razaak, M.; Martini, M.G.; Savino, K. A Study on Quality Assessment for Medical Ultrasound Video Compressed via HEVC. IEEE J. Biomed. Health Inform. 2014, 18, 1552–1559. [Google Scholar] [CrossRef]
- Martini, M.G.; Iacobelli, L.; Bergeron, C.; Hewage, C.T.; Panza, G.; Piri, E.; Vehkaperä, J.; Amon, P.; Mazzotti, M.; Savino, K.; et al. Real-time multimedia communications in medical emergency—The CONCERTO project solution. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; Volume 2015, pp. 7324–7327. [Google Scholar]
- Di Bello, V.; La Carruba, S.; Conte, L.; Fabiani, I.; Posteraro, A.; Antonini-Canterin, F.; Barletta, V.; Nicastro, I.; Mariotti, E.; Severino, S.; et al. Incremental value of pocket-sized echocardiography in addition to physical examination during inpatient cardiology evaluation: A multicenter Italian study (SIEC). Echocardiography 2015, 32, 1463–1470. [Google Scholar] [CrossRef]
- Cardim, N.; Dalen, H.; Voigt, J.U.; Ionescu, A.; Price, S.; Neskovic, A.N.; Edvardsen, T.; Galderisi, M.; Sicari, R.; Donal, E.; et al. The use of handheld ultrasound devices: A position statement of the European Association of Cardiovascular Imaging (2018 update). Eur. Heart J. Cardiovasc. Imaging 2019, 20, 245–252. [Google Scholar] [CrossRef]
- Spencer, K.T.; Kimura, B.J.; Korcarz, C.E.; Pellikka, P.A.; Rahko, P.S.; Siegel, R.J. Focused Cardiac Ultrasound: Recommendations from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2013, 26, 567–581. [Google Scholar] [CrossRef]
- Nesković, A.N.; Skinner, H.; Price, S.; Via, G.; De Hert, S.; Stankovic, I.; Galderisi, M.; Donal, E.; Muraru, D.; Sloth, E.; et al. Focus cardiac ultrasound core curriculum and core syllabus of the European Association of Cardiovascular Imaging. Eur. Hear. J. Cardiovasc. Imaging 2018, 19, 475–481. [Google Scholar] [CrossRef]
- Fukuda, S.; Shimada, K.; Kawasaki, T.; Fujimoto, H.; Maeda, K.; Inanami, H.; Yoshida, K.; Jissho, S.; Taguchi, H.; Yoshiyama, M.; et al. Pocket-Sized Transthoracic Echocardiography Device for the Measurement of Cardiac Chamber Size and Function. Circ. J. 2009, 73, 1092–1096. [Google Scholar] [CrossRef]
- Culp, B.C.; Mock, J.D.; Chiles, C.D.; Culp, W.C. The Pocket Echocardiograph: Validation and Feasibility. Echocardiography 2010, 27, 759–764. [Google Scholar] [CrossRef]
- Culp, B.C.; Mock, J.D.; Ball, T.R.; Chiles, C.D.; Culp, W.C., Jr. The Pocket Echocardiograph: A Pilot Study of Its Validation and Feasibility in Intubated Patients. Echocardiography 2011, 28, 371–377. [Google Scholar] [CrossRef]
- Kitada, R.; Fukuda, S.; Watanabe, H.; Oe, H.; Abe, Y.; Yoshiyama, M.; Song, J.M.; Sitges, M.; Shiota, T.; Ito, H.; et al. Diagnostic Accuracy and Cost-Effectiveness of a Pocket-Sized Transthoracic Echocardiographic Imaging Device. Clin. Cardiol. 2013, 36, 603–610. [Google Scholar] [CrossRef]
- Andersen, C.A.; Holden, S.; Vela, J.; Rathleff, M.S.; Jensen, M.B. Point-of-Care Ultrasound in General Practice: A Systematic Review. Ann. Fam. Med. 2019, 17, 61–69. [Google Scholar] [CrossRef]
- Giusca, S.; Jurcut, R.; Ticulescu, R.; Dumitru, D.; Vladaia, A.; Savu, O.; Voican, A.; Popescu, B.A.; Ginghina, C. Accuracy of handheld echocardiography for bedside diagnostic evaluation in a tertiary cardiology center: Comparison with standard echocardiography. Echocardiography 2011, 28, 136–141. [Google Scholar] [CrossRef]
- Mantella, L.E.; Colledanchise, K.; Bullen, M.; Hétu, M.F.; Day, A.G.; McLellan, C.S.; Johri, A.M. Handheld versus conventional vascular ultrasound for assessing carotid artery plaque. Int. J. Cardiol. 2019, 278, 295–299. [Google Scholar] [CrossRef]
- Mirabel, M.; Celermajer, D.; Beraud, A.-S.; Jouven, X.; Marijon, E.; Hagège, A.A. Pocket-sized focused cardiac ultrasound: Strengths and limitations. Arch. Cardiovasc. Dis. 2015, 108, 197–205. [Google Scholar] [CrossRef]
- Razi, R.; Estrada, J.R.; Doll, J.; Spencer, K.T. Bedside Hand-Carried Ultrasound by Internal Medicine Residents Versus Traditional Clinical Assessment for the Identification of Systolic Dysfunction in Patients Admitted with Decompensated Heart Failure. J. Am. Soc. Echocardiogr. 2011, 24, 1319–1324. [Google Scholar] [CrossRef]
- Kono, Y.; Fukuda, S.; Shimada, K.; Oe, H.; Maeda, K.; Kawasaki, T.; Fujimoto, H.; Otsuka, K.; Kubo, T.; Jissho, S.; et al. Pocket-sized echo for evaluation of mitral and tricuspid regurgitation. JACC Cardiovasc. Imaging 2011, 4, 921. [Google Scholar] [CrossRef][Green Version]
- Cameli, M.; Mandoli, G.E.; Ambrosio, A.; Cerbai, E.; Coiro, S.; Emdin, M.; Marcucci, R.; Morrone, D.; Palazzuoli, A.; Savino, K.; et al. Arterial hypertension and atrial fibrillation: Standard and advanced echocardiography from diagnosis to prognostication. J. Cardiovasc. Med. 2018, 19, 51–61. [Google Scholar] [CrossRef]
- Beltrami, M.; Palazzuoli, A.; Padeletti, L.; Cerbai, E.; Coiro, S.; Emdin, M.; Marcucci, R.; Morrone, D.; Cameli, M.; Savino, K.; et al. The importance of integrated left atrial evalutation: From hypertension to heart failure with preserved ejection fraction. Int. J. Clin. Pract. 2018, 72, 130–150. [Google Scholar] [CrossRef]
- Abe, Y.; Ito, M.; Tanaka, C.; Ito, K.; Naruko, T.; Itoh, A.; Haze, K.; Muro, T.; Yoshiyama, M.; Yoshikawa, J. A Novel and Simple Method Using Pocket-Sized Echocardiography to Screen for Aortic Stenosis. J. Am. Soc. Echocardiogr. 2013, 26, 589–596. [Google Scholar] [CrossRef]
- Wiley, B.; Bibhu Mohanty, B. Handheld ultrasound and diagnosis of cardiovascular disease at the bedside. J. Am. Coll. Cardiol. 2014, 64, 229–230. [Google Scholar] [CrossRef]
- Moore, C.L.; Copel, J.A. Point-of-care ultrasonography. N. Engl. J. Med. 2011, 364, 749–757. [Google Scholar] [CrossRef]
- Lichtenstein, D.A. Lung ultrasound in the critically ill. Ann. Intensive Care 2014, 4, 1–12. [Google Scholar] [CrossRef]
- Peterson, D.; Arntfield, R.T. Critical Care Ultrasonography. Emerg. Med. Clin. N. Am. 2014, 32, 907–926. [Google Scholar] [CrossRef]
- Byhahn, C.; Bingold, T.M.; Zwissler, B.; Maier, M.; Walcher, F. Prehospital ultrasound detects pericardial tamponade in a pregnant victim of stabbing assault. Resuscitation 2008, 76, 146–148. [Google Scholar] [CrossRef]
- Douglas, P.S.; Garcia, M.J.; Haines, D.E.; Lai, W.W.; Manning, W.J.; Patel, A.R.; Picard, M.H.; Polk, D.M.; Ragosta, M.; Ward, R.P.; et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/ SCCM/SCCT/SCMR 2011 Appropriate use criteria for echocardiography. J. Am. Soc. Echocardiogr. 2011, 24, 229–267. [Google Scholar] [CrossRef]
- Savino, K.; Bagliani, G.; Crusco, F.; Padeletti, M.; Lombardi, M. Electrocardiogram and Imaging: An Integrated Approach to Arrhythmogenic Cardiomyopathies. Card. Electrophysiol. Clin. 2018, 10, 413–429. [Google Scholar] [CrossRef]
- Olasveengen, T.M.; De Caen, A.R.; Mancini, M.E.; Maconochie, I.K.; Aickin, R.; Atkins, D.L.; Berg, R.A.; Bingham, R.M.; Brooks, S.C.; Castrén, M.; et al. 2017 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations Summary. Circulation 2017, 136, e424–e440. [Google Scholar] [CrossRef]
- Gundersen, G.H.; Norekval, T.M.; Haug, H.H.; Skjetne, K.; Kleinau, J.O.; Graven, T.; Dalen, H. Adding point of care ultrasound to assess volume status in heart failure patients in a nurse-led outpatient clinic. A randomised study. Heart 2016, 102, 29–34. [Google Scholar] [CrossRef]
- Panoulas, V.F.; Daigeler, A.L.; Malaweera, A.S.; Lota, A.S.; Baskaran, D.; Rahman, S.; Nihoyannopoulos, P. Pocket-size hand-held cardiac ultrasound as an adjunct to clinical examination in the hands of medical students and junior doctors. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 323–330. [Google Scholar] [CrossRef]
- Alexander, J.H.; Peterson, E.D.; Chen, A.Y.; Harding, T.M.; Adams, D.B.; Kisslo, J.A. Feasibility of point-of-care echocardiography by internal medicine house staff. Am. Hear. J. 2004, 147, 476–481. [Google Scholar] [CrossRef]
- Kobal, S.L.; Trento, L.; Baharami, S.; Tolstrup, K.; Naqvi, T.Z.; Cercek, B.; Neuman, Y.; Mirocha, J.; Kar, S.; Forrester, J.S.; et al. Comparison of Effectiveness of Hand-Carried Ultrasound to Bedside Cardiovascular Physical Examination. Am. J. Cardiol. 2005, 96, 1002–1006. [Google Scholar] [CrossRef]
- Evangelista, A.; Galuppo, V.; Mendez, J.; Evangelista, L.; Arpal, L.; Rubio, C.; Vergara, M.; Liceran, M.; López, F.; Sales, C.; et al. Handheld cardiac ultrasound screening performed by family doctors with remote expert support interpretation. Heart 2016, 102, 376–382. [Google Scholar] [CrossRef]
- Ryan, T.; Berlacher, K.; Lindner, J.R.; Mankad, S.V.; Rose, G.A.; Wang, A. COCATS 4 task force 5: Training in echocardiography: Endorsed by the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2015, 28, 615–627. [Google Scholar] [CrossRef]
Standard Echocardiography | Focused Echo | |
|---|---|---|
| Equipment | Stationary, top level technology | Handheld ultrasound devices |
| Echo purpose | All heart diseases study | Few clinical questions |
| Echo goal | Accurate study | Differential diagnosis |
| US sections | All recommended | Few |
| Execution time | >30 min | Few minutes |
| Diagnosis | In election | Rapid |
| Operator training | Accurate/long | Rapid/25–50 exams |
| Clinical Suspect | FoCUS Goals |
|---|---|
| Congestive heart failure | Left atrium and ventricle dimension, LV EF, significant valvular regurgitation, IVC dimension and collapse, pulmonary congestion |
| Cardiomyopathies | Left ventricular hypertrophy, dilated cardiomyopathies |
| Atrial fibrillation | Left atrial dimensions, left ventricular function |
| Stable coronary artery disease | Wall motion abnormalities, ejection fraction |
| Valvular stenosis | Thickness and calcification leaflet, reduced leaflets mobility, turbulent transvalvular flow at color-Doppler |
| Valvular regurgitation | Extent regurgitation jet at color-Doppler |
| Pericarditis | Pericardial effusion presence, size and distribution |
| Clinical Scenarios | POCUS Goal | Rule-In/Rule-Out Diseases |
|---|---|---|
| Acute respiratory failure | No lung sliding sign (lung movement absence), Anechoic space between visceral and parietal pleura, Lines B—comets | Pneumotorax Pleural effusion Pulmonary congestion |
| Shock | Chambers size and shape, LV EF, IVC size and collapsibility, pericardial effusion, pulmonary congestion | Cardiogenic shock |
| Cardiac tamponade | Pericardial fluid size and distribution Guide to pericardiocentesis | Massive pericardial effusion |
| Acute chest pain | LV wall motion abnormalities, LV EF, RV size and function, Ascending aorta dimensions and morphology, aortic regurgitation, pericardial effusion | Acute coronary syndrome Pulmonary embolism Aortic dissection Pericarditis |
| Arrhythmic cardiac arrest | Left ventricular hypertrophy, LV dilatation, LV dysfunction, RV dilatation and dysfunction | Hypertrophic cardiomyopathy Dilated cardiomyopathy Arrhythmogenic right ventricular cardiomyopathy |
| Cardiopulmonary resuscitation | Massive pericardial effusion, RV dilatation, RV severe dysfunction, LV severe dysfunction, LV very small dimension (empty ventricle) | Cardiac tamponade Massive pulmonary embolism Severe congestive heart failure Hypovolemia |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Savino, K.; Ambrosio, G. Handheld Ultrasound and Focused Cardiovascular Echography: Use and Information. Medicina 2019, 55, 423. https://doi.org/10.3390/medicina55080423
Savino K, Ambrosio G. Handheld Ultrasound and Focused Cardiovascular Echography: Use and Information. Medicina. 2019; 55(8):423. https://doi.org/10.3390/medicina55080423
Chicago/Turabian StyleSavino, Ketty, and Giuseppe Ambrosio. 2019. "Handheld Ultrasound and Focused Cardiovascular Echography: Use and Information" Medicina 55, no. 8: 423. https://doi.org/10.3390/medicina55080423
APA StyleSavino, K., & Ambrosio, G. (2019). Handheld Ultrasound and Focused Cardiovascular Echography: Use and Information. Medicina, 55(8), 423. https://doi.org/10.3390/medicina55080423




