Guidelines-Driven Educational Intervention Promotes Healthy Lifestyle Among Adolescents and Adults: A Serbian National Longitudinal Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. The National Diet and Physical Activity for Health Initiative (DiPAH)
2.2. Study Participants
2.3. Study Design
2.4. Educational Intervention
2.5. Statistical Analyses
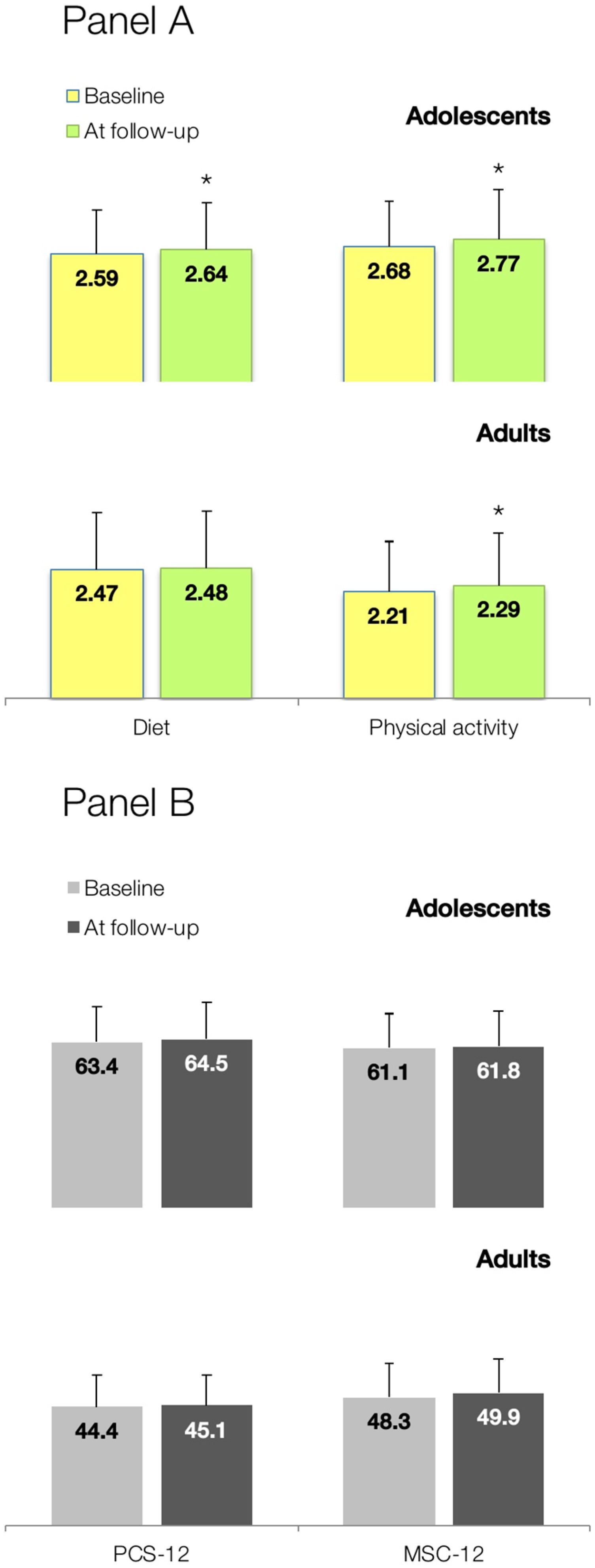
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization Regional Office for the Eastern Mediterranean. Health Education: Theoretical Concepts, Effective Strategies and Core Competencies: A Foundation Document to Guide Capacity Development of Health Educators; WHO Regional Office for the Eastern Mediterranean: Cairo, Egypt, 2012. [Google Scholar]
- Arena, R.; McNeil, A.; Sagner, M.; Hills, A. The current global state of key lifestyle characteristics: Health and economic implications. Prog. Cardiovasc. Dis. 2017, 59, 422–429. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Imamura, F.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Shi, P.; Powles, J.; Mozaffarian, D.; Global Burden of Diseases Nutrition and Chronic Diseases Expert Group (NutriCoDE). Dietary quality among men and women in 187 countries in 1990 and 2010: A systematic assessment. Lancet Glob. Health 2015, 3, e132–e142. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- GBD 2013 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef]
- Global Burden of Disease Study 2015. Global Burden of Disease Study 2015 (GBD 2015) Socio-Demographic Index (SDI) 1980–2015; Institute for Health Metrics and Evaluation: Seattle, WA, USA, 2016. [Google Scholar]
- World Health Organization. Global Status Report on Noncommunicable Diseases 2014; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- World Health Organization. Global Health Observatory (GHO) Data: Unhealthy Diet. Available online: https://www.who.int/gho/ncd/risk_factors/unhealthy_diet_text/en/ (accessed on 24 January 2019).
- World Health Organization. Global Strategy on Diet., Physical Activity and Health. Physical Inactivity: A Global Public Health Problem. Available online: https://www.who.int/dietphysicalactivity/factsheet_inactivity/en/ (accessed on 24 January 2019).
- The United States Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans; USDHHS: Washington, DC, USA, 2008.
- The World Health Organization. Global Recommendations on Physical Activity for Health; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Canadian Society for Exercise Physiology. Canadian Physical Activity Guidelines for Adults 18–64 Years; CSEP: Ottawa, ON, Canada, 2011. [Google Scholar]
- Canadian Society for Exercise Physiology. Canadian Physical Activity Guidelines for Older Adults 65 Years and Older; CSEP: Ottawa, ON, Canada, 2011. [Google Scholar]
- The United States Department of Health and Human Services. 2015–2020 Dietary Guidelines for Americans; USDHHS: Washington, DC, USA, 2015.
- Canadian Society for Exercise Physiology. Canadian 24-Hour Movement Guidelines for the Early Years; CSEP: Ottawa, ON, Canada, 2016. [Google Scholar]
- Canadian Society for Exercise Physiology. Canadian 24-Hour Movement Guidelines for Children and Youth (Ages 5–17 Years); CSEP: Ottawa, ON, Canada, 2016. [Google Scholar]
- Straker, L.M.; Howie, E.K.; Smith, K.L.; Fenner, A.A.; Kerr, D.A.; Olds, T.S.; Abbott, R.A.; Smith, A.J. The impact of Curtin University’s activity, food and attitudes program on physical activity, sedentary time and fruit, vegetable and junk food consumption among overweight and obese adolescents: A waitlist controlled trial. PLoS ONE 2014, 9, e111954. [Google Scholar] [CrossRef]
- Xu, F.; Ware, R.S.; Leslie, E.; Tse, L.A.; Wang, Z.; Li, J.; Wang, Y. Effectiveness of a randomized controlled lifestyle intervention to prevent obesity among Chinese primary school students: CLICK-Obesity Study. PLoS ONE 2015, 10, e0141421. [Google Scholar] [CrossRef] [PubMed]
- Sharma, B.; Kim, H.Y.; Nam, E.W. Effects of school-based health promotion intervention on health behaviors among school adolescents in North Lima and Callao, Peru. J. Lifestyle Med. 2018, 8, 60–71. [Google Scholar] [CrossRef]
- Atalla, M.; Pinto, A.J.; Mielke, G.I.; Baciuk, E.P.; Benatti, F.B.; Gualano, B. Tackling youth inactivity and sedentary behavior in an entire Latin America City. Front. Pediatr. 2018, 6, 298. [Google Scholar] [CrossRef] [PubMed]
- Morgan, P.J.; Collins, C.E.; Plotnikoff, R.C.; Callister, R.; Burrows, T.; Fletcher, R.; Okely, A.D.; Young, M.D.; Miller, A.; Lloyd, A.B.; et al. The ‘Healthy Dads, Healthy Kids’ community randomized controlled trial: A community-based healthy lifestyle program for fathers and their children. Prev. Med. 2014, 61, 90–99. [Google Scholar] [CrossRef]
- Walker, S.N.; Sechrist, K.R.; Pender, N.J. The Health-Promoting Lifestyle Profile II; University of Nebraska Medical Center: Omaha, NE, USA, 1995. [Google Scholar]
- Ware, J.E.; Kosinski, M.; Keller, S.D. A 12-item, short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med. Care 1996, 3, 220–223. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Keller, S.D. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales, 2nd ed.; The Health Institute: Boston, MA, USA, 1995. [Google Scholar]
- Chafjiri, R.T.; Shirinkam, F.; Karimi, H. Investigating the effect of education on health-promoting lifestyle among the elderly of Ramsar in 2017. J. Fam. Med. Prim. Care 2018, 7, 612–617. [Google Scholar] [CrossRef]
- Shayesteh, H.; Mirzaei, A.; Sayehmiri, K.; Qorbani, M.; Mansourian, M. Effect of education intervention on lifestyle of patients with hypertension among the rural population of Lorestan Province. J. Lifestyle Med. 2016, 6, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Safabakhsh, L.; Jahantigh, M.; Nosratzehi, S.; Navabi, S. The effect of health promoting programs on patient’s life style after coronary artery bypass graft-hospitalized in Shiraz hospitals. Glob. J. Health Sci. 2015, 8, 154–159. [Google Scholar] [CrossRef] [PubMed]
- McElligott, D.; Capitulo, K.L.; Morris, D.L.; Click, E.R. The effect of a holistic program on health-promoting behaviors in hospital registered nurses. J. Holist. Nurs. 2010, 28, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Wilson, H.K.; Scult, M.; Wilcher, M.; Chudnofsky, R.; Malloy, L.; Drewel, E.; Riklin, E.; Saul, S.; Fricchione, G.L.; Benson, H.; et al. Teacher-led relaxation response curriculum in an urban high school: Impact on student behavioral health and classroom environment. Adv. Mind Body Med. 2015, 29, 6–14. [Google Scholar] [PubMed]
- Sallis, J.F. Age-related decline in physical activity: A synthesis of human and animal studies. Med. Sci. Sports Exerc. 2000, 32, 1598–1600. [Google Scholar] [CrossRef]
- Nacar, M.; Baykan, Z.; Cetinkaya, F.; Arslantas, D.; Ozer, A.; Coskun, O.; Bati, H.; Karaoglu, N.; Elmali, F.; Yilmaze, G. Health promoting lifestyle behaviour in medical students: A multicentre study from Turkey. Asian Pac. J. Cancer Prev. 2014, 15, 8969–8974. [Google Scholar] [CrossRef]
- Pearson, N.; Biddle, S.J.; Gorely, T. Family correlates of fruit and vegetable consumption in children and adolescents: A systematic review. Public Health Nutr. 2009, 12, 267–283. [Google Scholar] [CrossRef]
- Kim, S.Y.; Sim, S.; Park, B.; Kong, I.G.; Kim, J.H.; Choi, H.G. Dietary habits are associated with school performance in adolescents. Medicine 2016, 95, e3096. [Google Scholar] [CrossRef]
- Hardcastle, S.J.; Hancox, J.; Hattar, A.; Maxwell-Smith, C.; Thøgersen-Ntoumani, C.; Hagger, M.S. Motivating the unmotivated: How can health behavior be changed in those unwilling to change? Front. Psychol. 2015, 6, 835. [Google Scholar] [CrossRef] [PubMed]
- Kurnat-Thoma, E.; El-Banna, M.; Oakcrum, M.; Tyroler, J. Nurses’ health promoting lifestyle behaviors in a community hospital. Appl. Nurs. Res. 2017, 35, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Burkow-Heikkinen, L. Non-invasive physiological monitoring of exercise and fitness. Neurol. Res. 2011, 33, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Tulle, E. Physical activity and sedentary behaviour: A vital politics of old age? In Physical Activity and Sport in Later Life; Global Culture and Sport Series; Tulle, E., Phoenix, C., Eds.; Palgrave Macmillan: London, UK, 2016. [Google Scholar]
- Douma, J.G.; Volkers, K.M.; Engels, G.; Sonneveld, M.H.; Goossens, R.H.M.; Scherder, E.J.A. Setting-related influences on physical inactivity of older adults in residential care settings: A review. BMC Geriatr. 2017, 17, 97. [Google Scholar] [CrossRef] [PubMed]
- Harada, C.N.; Natelson Love, M.C.; Triebel, K.L. Normal cognitive aging. Clin. Geriatr. Med. 2013, 29, 737–752. [Google Scholar] [CrossRef] [PubMed]
- Tucker, J.S.; Klein, D.J.; Elliott, M.N. Social control of health behaviors: A comparison of young, middle-aged, and older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 2004, 59, 147–150. [Google Scholar] [CrossRef]
- Leroux, J.S.; Moore, S.; Richard, L.; Gauvin, L. Physical inactivity mediates the association between the perceived exercising behavior of social network members and obesity: A cross-sectional study. PLoS ONE 2012, 7, e46558. [Google Scholar] [CrossRef] [PubMed]
- United Nations Economic Commission for Europe Population Unit: The Active Aging Pilot Studies for Serbia and Turkey. Available online: https://bit.ly/1cQmpcZ (accessed on 22 December 2017).
- National Research Council (US) Committee on Aging Frontiers in Social Psychology, Personality, and Adult Developmental Psychology. 3. Motivation and Behavioral Change. In When I’m 64; Carstensen, L.L., Hartel, C.R., Eds.; National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Ministry of Health of the Republic of Serbia, AmCham. Possible Directions of Increasing Efficiency pf Healthcare System in The Republic of Serbia; Ernst & Young Global Limited: London, UK, 2015. [Google Scholar]
- Mikkelsen, B.E.; Bloch, P.; Reinbach, H.C.; Buch-Andersen, T.; Lawaetz Winkler, L.; Toft, U.; Glümer, C.; Jensen, B.B.; Aagaard-Hansen, J. Project SoL-a community-based, multi-component health promotion intervention to improve healthy eating and physical activity practices among Danish families with young children part 2: Evaluation. Int. J. Environ. Res. Public Health 2018, 15, 1513. [Google Scholar] [CrossRef]
- Viner, R.; Macfarlane, A. Health promotion. Br. Med. J. 2005, 330, 527–529. [Google Scholar] [CrossRef]
| Adolescents | p | Adults | p | |||
|---|---|---|---|---|---|---|
| Baseline (n = 3278) | At Follow Up (n = 3105) | Baseline (n = 544) | At Follow Up (n = 515) | |||
| Choose a diet low in fat, saturate fat, and cholesterol | 7.7 | 9.2 | 0.03 | 35.6 | 41.8 | 0.04 |
| Limit use of sugars and food containing sugar (sweets) | 16.7 | 16.9 | 0.83 | 40.8 | 46.3 | 0.07 |
| Eat 6–11 servings of bread, cereal, rice, and pasta each day | 10.1 | 11.0 | 0.24 | 19.6 | 22.9 | 0.19 |
| Eat 2–4 servings of fruit each day | 34.7 | 33.9 | 0.50 | 42.6 | 43.6 | 0.74 |
| Eat 3–5 servings of vegetables each day | 20.1 | 23.1 | 0.00 | 39.9 | 40.5 | 0.84 |
| Eat 2–3 servings of milk, yogurt, or cheese each day | 34.1 | 34.9 | 0.50 | 46.7 | 46.8 | 0.97 |
| Eat only 2–3 servings from the protein group each day | 26.6 | 26.1 | 0.65 | 47.6 | 42.1 | 0.07 |
| Read labels to identify nutrients, fats, sodium content in packaged food | 12.2 | 14.2 | 0.02 | 42.0 | 40.0 | 0.51 |
| Eat breakfast | 78.2 | 73.8 | 0.00 | 87.3 | 83.0 | 0.05 |
| Adolescents | p | Adults | p | |||
|---|---|---|---|---|---|---|
| Baseline (n = 3278) | At Follow Up (n = 3105) | Baseline (n = 544) | At Follow Up (n = 515) | |||
| Follow a planned exercise program | 44.8 | 41.2 | 0.00 | 27.2 | 31.4 | 0.13 |
| Exercise vigorously for 20 or more minutes at least three times a week | 43.5 | 47.3 | 0.00 | 43.7 | 43.4 | 0.92 |
| Take part in light to moderate physical activity | 39.4 | 42.5 | 0.01 | 55.9 | 57.7 | 0.56 |
| Take part in leisure-time (recreational) physical activities | 29.1 | 31.4 | 0.05 | 30.8 | 36.8 | 0.04 |
| Do stretching exercises at least 3 times per week | 40.9 | 43.4 | 0.04 | 28.6 | 35.5 | 0.02 |
| Get exercise during usual daily activities | 72.9 | 69.3 | 0.00 | 63.3 | 58.8 | 0.13 |
| Check my pulse rate when exercising | 7.2 | 7.4 | 0.76 | 17.2 | 22.3 | 0.04 |
| Reach my target heart rate when exercising | 11.6 | 14.6 | 0.00 | 19.0 | 22.3 | 0.18 |
| Adolescents (n = 3278) | Adults (n = 544) | |||||||
|---|---|---|---|---|---|---|---|---|
| β | 95% CI | SE | p | β | 95% CI | SE | p | |
| Diet | ||||||||
| Age | −0.026 | −0.030 to −0.022 | 0.002 | <0.001 | 0.003 | 0.001 to 0.004 | 0.001 | <0.001 |
| Gender | −0.007 | −0.030 to −0.017 | 0.012 | 0.579 | 0.027 | −0.029 to 0.083 | 0.028 | 0.341 |
| Physical activity | ||||||||
| Age | −0.030 | −0.035 to −0.025 | 0.003 | <0.001 | 0.004 | 0.002 to 0.006 | 0.001 | <0.001 |
| Gender | −0.079 | −0.109 to −0.050 | 0.015 | <0.001 | −0.082 | −0.164 to 0.001 | 0.042 | 0.053 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Đorđić, V.; Božić, P.; Milanović, I.; Radisavljević, S.; Batez, M.; Jorga, J.; Ostojić, S.M. Guidelines-Driven Educational Intervention Promotes Healthy Lifestyle Among Adolescents and Adults: A Serbian National Longitudinal Study. Medicina 2019, 55, 39. https://doi.org/10.3390/medicina55020039
Đorđić V, Božić P, Milanović I, Radisavljević S, Batez M, Jorga J, Ostojić SM. Guidelines-Driven Educational Intervention Promotes Healthy Lifestyle Among Adolescents and Adults: A Serbian National Longitudinal Study. Medicina. 2019; 55(2):39. https://doi.org/10.3390/medicina55020039
Chicago/Turabian StyleĐorđić, Višnja, Predrag Božić, Ivana Milanović, Snežana Radisavljević, Maja Batez, Jagoda Jorga, and Sergej M. Ostojić. 2019. "Guidelines-Driven Educational Intervention Promotes Healthy Lifestyle Among Adolescents and Adults: A Serbian National Longitudinal Study" Medicina 55, no. 2: 39. https://doi.org/10.3390/medicina55020039
APA StyleĐorđić, V., Božić, P., Milanović, I., Radisavljević, S., Batez, M., Jorga, J., & Ostojić, S. M. (2019). Guidelines-Driven Educational Intervention Promotes Healthy Lifestyle Among Adolescents and Adults: A Serbian National Longitudinal Study. Medicina, 55(2), 39. https://doi.org/10.3390/medicina55020039






