Health Behavior Change and Complementary Medicine Use: National Health Interview Survey 2012
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Measures
2.3. Statistical Analysis
2.4. Ethics
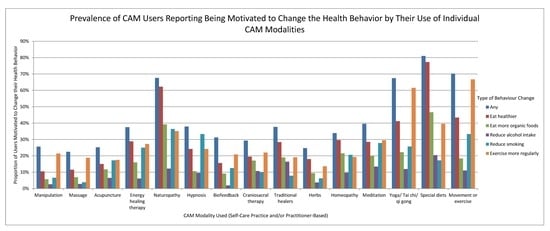
3. Results
3.1. Prevalence of Health Behavior Changes
3.2. Characteristics of CAM Users Motivated to Change Health Behaviors
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ford, E.S.; Bergmann, M.M.; Boeing, H.; Li, C.; Capewell, S. Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Prev. Med. 2012, 55, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Elley, C.R.; Kerse, N.; Arroll, B.; Robinson, E. Effectiveness of counselling patients on physical activity in general practice: Cluster randomised controlled trial. BMJ 2003, 326, 793. [Google Scholar] [CrossRef] [PubMed]
- Butler, C.C.; Simpson, S.A.; Hood, K.; Cohen, D.; Pickles, T.; Spanou, C.; McCambridge, J.; Moore, L.; Randell, E.; Fasihul, A.M.; et al. Training practitioners to deliver opportunistic multiple behaviour change counselling in primary care: A cluster randomised trial. BMJ 2013, 346, f1191. [Google Scholar] [CrossRef] [PubMed]
- Neuner-Jehle, S.; Schmid, M.; Grüninger, U. The Health Coaching programme: A new patient-centred and visually supported approach for health behaviour change in primary care. BMC Fam. Pract. 2013, 14, 100. [Google Scholar] [CrossRef] [PubMed]
- Dwamena, F.; Holmes-Rovner, M.; Gaulden, C.M.; Jorgenson, S.; Sadigh, G.; Sikorskii, A.; Lewin, S.; Smith, R.C.; Coffey, J.; Olomu, A. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst. Rev. 2012, 12, CD003267. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- McEwan, D.; Harden, S.M.; Zumbo, B.D.; Sylvester, B.D.; Kaulius, M.; Ruissen, G.R.; Dowd, A.J.; Beauchamp, M.R. The effectiveness of multi-component goal setting interventions for changing physical activity behaviour: A systematic review and meta-analysis. Health Psychol. Rev. 2016, 10, 67–88. [Google Scholar] [CrossRef] [PubMed]
- Epton, T.; Currie, S.; Armitage, C.J. Unique effects of setting goals on behavior change: Systematic review and meta-analysis. J. Consult. Clin. Psychol. 2017, 85, 1182–1198. [Google Scholar] [CrossRef]
- Michie, S.; West, R.; Sheals, K.; Godinho, C.A. Evaluating the effectiveness of behavior change techniques in health-related behavior: A scoping review of methods used. Transl. Behav. Med. 2018, 8, 212–224. [Google Scholar] [CrossRef]
- National Center for Complementary and Integrative Health. Complementary, Alternative, or Integrative Health: What’s in a Name? Available online: https://nccih.nih.gov/health/integrative-health (accessed on 31 January 2017).
- Kaptchuk, T. The Web That Has No Weaver: Understanding Chinese Medicine; Contemporary Books Inc.: Chicago, IL, USA, 2000. [Google Scholar]
- Luberto, C.M.; Chad-Friedman, E.; Dossett, M.L.; Perez, G.K.; Park, E.R. Characteristics of adult smokers presenting to a mind-body medicine clinic. J. Health Psychol. 2018, 23, 860–870. [Google Scholar] [CrossRef]
- Harris, P.E.; Cooper, K.L.; Relton, C.; Thomas, K.J. Prevalence of complementary and alternative medicine (CAM) use by the general population: A systematic review and update. Int J. Clin. Pract. 2012, 66, 924–939. [Google Scholar] [CrossRef] [PubMed]
- Rhee, T.G.; Pawloski, P.A.; Parsons, H.M. Health-related quality of life among US adults with cancer: Potential roles of complementary and alternative medicine for health promotion and well-being. Psychooncology 2019, 28, 896–902. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.A.; West, A.N.; Weeks, W.B.; Sirovich, B.E. Health behaviors and utilization among users of complementary and alternative medicine for treatment versus health promotion. Health Serv. Res. 2011, 46, 1402–1416. [Google Scholar] [CrossRef] [PubMed]
- Nahin, R.L.; Dahlhamer, J.M.; Taylor, B.L.; Barnes, P.M.; Stussman, B.J.; Simile, C.M.; Blackman, M.R.; Chesney, M.A.; Jackson, M.; Miller, H.; et al. Health behaviors and risk factors in those who use complementary and alternative medicine. BMC Public Health 2007, 7, 217. [Google Scholar] [CrossRef] [PubMed]
- Hawk, C.; Ndetan, H.; Evans, M.W., Jr. Potential role of complementary and alternative health care providers in chronic disease prevention and health promotion: An analysis of National Health Interview Survey data. Prev. Med. 2012, 54, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Foley, H.; Steel, A. Patient perceptions of clinical care in complementary medicine: A systematic review of the consultation experience. Patient Educ. Couns. 2016, 100, 212–223. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.; Paterson, C.; Wye, L.; Chapman, R.; Robinson, J.; Norton, R.; Bertschlinger, R. Lifestyle and self-care advice within traditional acupuncture consultations: A qualitative observational study nested in a co-operative inquiry. J. Altern. Complement. Med. 2011, 17, 519–529. [Google Scholar] [CrossRef]
- Clarke, T.C.; Black, L.I.; Stussman, B.J.; Barnes, P.M.; Nahin, R.L. Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl. Health Stat. Rep. 2015, 79, 1–16. [Google Scholar]
- 2012 National Health Interview Survey (NHIS) Public Use Data Release: NHIS Survey Description. Available online: ftp://ftp.cdc.gov/pub/health_statistics/nchs/dataset_documentation/NHIS/2012/srvydesc.pdf (accessed on 13 October 2016).
- Sarris, J.; Wardle, J. Clinical Naturopathy: An Evidence-Based Guide to Practice; Churchill Livingstone/Elsevier Health Sciences: Sydney, Australian, 2010. [Google Scholar]
- Paterson, C.; Britten, N. Acupuncture as a complex intervention: A holistic model. J. Altern. Complement. Med. 2004, 10, 791–801. [Google Scholar] [CrossRef]
- Bishop, F.L.; Lewith, G.T. A qualitative exploration of how patients conceptualise their acupuncturists: Technicians, caring professionals, and wise healers. Complement. Ther. Med. 2016, 27, 74–81. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. The “what” and “why” of goal pursuits: Human needs and the self-determination of behavior. Psychol. Inq. 2000, 11, 227–268. [Google Scholar] [CrossRef]
- Holmström, I.; Röing, M. The relation between patient-centeredness and patient empowerment: A discussion on concepts. Patient Educ. Couns. 2010, 79, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.; Lauche, R.; Moebus, S.; Michalsen, A.; Langhorst, J.; Dobos, G.; Paul, A. Predictors of health behavior change after an integrative medicine inpatient program. Int. J. Behav. Med. 2014, 21, 775–783. [Google Scholar] [CrossRef] [PubMed]
- Daubenmier, J.J.; Weidner, G.; Sumner, M.D.; Mendell, N.; Merritt-Worden, T.; Studley, J.; Ornish, D. The contribution of changes in diet, exercise, and stress management to changes in coronary risk in women and men in the multisite cardiac lifestyle intervention program. Ann. Behav. Med. 2007, 33, 57–68. [Google Scholar] [CrossRef] [PubMed]
- Furnham, A.; Vincent, C.; Wood, R. The health beliefs and behaviors of three groups of complementary medicine and a general practice group of patients. J. Altern. Complement. Med. 1995, 1, 347–359. [Google Scholar] [CrossRef] [PubMed]
- Karlik, J.B.; Ladas, E.J.; Ndao, D.H.; Cheng, B.; Bao, Y.; Kelly, K.M. Associations between healthy lifestyle behaviors and complementary and alternative medicine use: Integrated wellness. J. Natl. Cancer Inst. Monogr. 2014, 2014, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Chung, V.C.H.; Ma, P.H.X.; Lau, C.H.; Wong, S.Y.S.; Yeoh, E.K.; Griffiths, S.M. Views on traditional Chinese medicine amongst Chinese population: A systematic review of qualitative and quantitative studies. Health Expect. 2014, 17, 622–636. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Amireault, S.; Godin, G.; Vézina-Im, L.-A. Determinants of physical activity maintenance: A systematic review and meta-analyses. Health Psychol. Rev. 2013, 7, 55–91. [Google Scholar] [CrossRef]
- Cheng, C.; Cheung, M.W.L.; Lo, B.C.Y. Relationship of health locus of control with specific health behaviours and global health appraisal: A meta-analysis and effects of moderators. Health Psychol. Rev. 2016, 10, 460–477. [Google Scholar] [CrossRef]
- Lauche, R.; Cramer, H.; Moebus, S.; Paul, A.; Michalsen, A.; Langhorst, J.; Dobos, G. Results of a 2-week inpatient stay at the department for internal and integrative medicine: An observational study. Evid. Based Complement. Altern. Med. 2012, 2012, 875874. [Google Scholar] [CrossRef][Green Version]
- Bryan, S.; Pinto Zipp, G.; Parasher, R. The effects of yoga on psychosocial variables and exercise adherence: A randomized, controlled pilot study. Altern. Ther. Health Med. 2012, 18, 50–59. [Google Scholar]
- Pullen, C.; Walker, S.N.; Fiandt, K. Determinants of health-promoting lifestyle behaviors in rural older women. Fam. Community Health 2001, 24, 49–72. [Google Scholar] [CrossRef]
- Brunello, G.; Fort, M.; Schneeweis, N.; Winter-Ebmer, R. The causal effect of education on health: What is the role of health behaviors? Health Econ. 2016, 25, 314–336. [Google Scholar] [CrossRef]
- Rosenstock, I.M. Why people use health services. Milbank Mem. Fund Q. 1966, 44, 94–127. [Google Scholar] [CrossRef]
- Williams-Piehota, P.A.; Sirois, F.M.; Bann, C.M.; Isenberg, K.B.; Walsh, E.G. Agents of change: How do complementary and alternative medicine providers play a role in health behavior change? Altern. Ther. Health Med. 2011, 17, 22–30. [Google Scholar]
| Top Therapy | n | Any Health Behavior Change | Eat Healthier | Eat More Organic Foods | Reduce Alcohol Intake 1 | Reduce Smoking 2 | Exercise More Regularly |
|---|---|---|---|---|---|---|---|
| Special diets | 898 | 81.0% | 77.3% | 46.6% | 20.4% | 17.2% | 39.6% |
| Movement or exercise therapies | 593 | 70.2% | 43.4% | 18.4% | 11.0% | 33.3% | 66.7% |
| Naturopathy | 74 | 67.6% | 62.2% | 39.2% | 12.2% | 36.4% | 35.1% |
| Yoga/Tai chi/qi gong | 2698 | 67.4% | 41.2% | 22.2% | 11.9% | 25.7% | 61.5% |
| Meditation | 1338 | 39.6% | 28.5% | 20.0% | 13.4% | 27.8% | 29.5% |
| Hypnosis | 66 | 37.9% | 24.2% | 10.6% | 9.6% | 33.3% | 24.2% |
| Traditional healers | 115 | 37.7% | 28.4% | 19.0% | 16.4% | 7.8% | 19.1% |
| Energy healing therapy | 80 | 37.5% | 28.8% | 16.0% | 6.1% | 25.0% | 27.2% |
| Homeopathy | 504 | 33.9% | 29.6% | 21.5% | 9.7% | 20.6% | 19.3% |
| Biofeedback | 77 | 31.2% | 15.6% | 9.1% | 1.9% | 12.5% | 20.8% |
| Craniosacral therapy | 41 | 29.3% | 19.5% | 17.1% | 10.7% | 10.0% | 22.0% |
| Chiropractic or osteopathic manipulation | 2710 | 25.6% | 10.5% | 5.7% | 2.6% | 6.6% | 21.4% |
| Acupuncture | 418 | 25.2% | 15.0% | 11.7% | 6.5% | 17.2% | 17.5% |
| Herbs | 5373 | 24.7% | 18.0% | 9.4% | 3.7% | 6.2% | 13.6% |
| Massage | 2005 | 22.5% | 11.5% | 6.9% | 2.8% | 3.8% | 18.8% |
| Characteristic | Not Motivated to Change Health Behavior | Motivated to Change at Least One Health Behavior | |||
|---|---|---|---|---|---|
| n | % | n | % | p | |
| Age (years) | <0.001 * | ||||
| 18–29 | 814 | 43.8% | 1042 | 56.2% | |
| 30-39 | 934 | 50.6% | 910 | 49.4% | |
| 40-49 | 1052 | 55.5% | 842 | 44.5% | |
| 50–64 | 1666 | 56.0% | 1312 | 44.0% | |
| 65 plus | 1107 | 67.9% | 523 | 32.1% | |
| Gender | <0.001 * | ||||
| Male | 2548 | 61.0% | 1627 | 39.0% | |
| Female | 3024 | 50.2% | 3002 | 49.8% | |
| Marital status | <0.001 * | ||||
| Not in relationship | 1820 | 50.0% | 1823 | 50.0% | |
| In relationship | 3752 | 57.2% | 2806 | 42.8% | |
| Ethnicity | <0.001 * | ||||
| White | 4473 | 56.6% | 3425 | 43.4% | |
| Hispanic | 473 | 49.0% | 493 | 51.0% | |
| Black | 318 | 45.8% | 376 | 54.2% | |
| Asian | 280 | 49.4% | 287 | 50.6% | |
| Other | 29 | 37.8% | 48 | 62.2% | |
| Region | 0.003 * | ||||
| West | 1520 | 52.2% | 1393 | 47.8% | |
| Northeast | 980 | 56.5% | 755 | 43.5% | |
| Midwest | 1476 | 56.6% | 1133 | 43.4% | |
| South | 1597 | 54.2% | 1348 | 45.8% | |
| Education | <0.001 * | ||||
| Less than high school | 386 | 61.2% | 245 | 38.8% | |
| High school | 2390 | 57.5% | 1768 | 42.5% | |
| College or higher | 2780 | 51.7% | 2595 | 48.3% | |
| Health insurance coverage | <0.001 * | ||||
| Uninsured | 568 | 46.1% | 664 | 53.9% | |
| At least public health insurance | 792 | 58.6% | 558 | 41.4% | |
| Private health insurance | 4122 | 55.4% | 3321 | 44.6% | |
| Body Mass Index (kg/m2) | <0.001 * | ||||
| < 18.5 | 93 | 51.3% | 88 | 48.7% | |
| 18.5–25 | 1950 | 50.7% | 1893 | 49.3% | |
| 25–30 | 1935 | 56.5% | 1488 | 43.5% | |
| >30 | 1594 | 57.9% | 1159 | 42.1% | |
| Subjective health status | <0.001 * | ||||
| Very good or excellent | 3477 | 52.3% | 3173 | 47.7% | |
| Good | 1460 | 58.4% | 1038 | 41.6% | |
| Fair or poor | 634 | 60.3% | 417 | 39.7% | |
| Number of chronic conditions | 0.001 * | ||||
| 0 | 2744 | 50.4% | 2705 | 49.6% | |
| 1 | 1504 | 57.2% | 1127 | 42.8% | |
| 2 | 783 | 63.9% | 443 | 36.1% | |
| 3 | 318 | 62.4% | 192 | 37.6% | |
| 4 or more | 201 | 61.2% | 128 | 38.8% | |
| Characteristic | Category | OR | Lower CI | Upper CI | p |
|---|---|---|---|---|---|
| Age (years) | 65 plus | Reference | |||
| 50–64 | 1.599 | 1.383 | 1.850 | <0.001 * | |
| 40–49 | 1.457 | 1.236 | 1.717 | <0.001 * | |
| 30–39 | 1.662 | 1.404 | 1.966 | <0.001 * | |
| 18–29 | 2.127 | 1.794 | 2.522 | <0.001 * | |
| Gender | Male | Reference | |||
| Female | 1.612 | 1.479 | 1.757 | <0.001 * | |
| Marital status | In relationship | Reference | |||
| Not in relationship | 1.237 | 1.132 | 1.353 | <0.001 * | |
| Ethnicity | White | Reference | |||
| Hispanic | 1.273 | 1.097 | 1.477 | 0.001 * | |
| Black | 1.447 | 1.225 | 1.710 | <0.001 * | |
| Asian | 1.154 | 0.962 | 1.385 | 0.122 | |
| Other | 1.909 | 1.174 | 3.103 | 0.009 | |
| Region | Midwest | Reference | |||
| Northeast | 0.967 | 0.850 | 1.099 | 0.603 | |
| West | 1.132 | 1.011 | 1.267 | 0.032 | |
| South | 1.041 | 0.931 | 1.163 | 0.484 | |
| Education | Less than high school | Reference | |||
| High school | 1.197 | 0.994 | 1.441 | 0.058 | |
| College or higher | 1.527 | 1.265 | 1.844 | <0.001 * | |
| Health insurance coverage | Private health insurance | Reference | |||
| At least public health insurance | 1.194 | 1.041 | 1.369 | 0.011 | |
| Uninsured | 1.382 | 1.211 | 1.576 | <0.001 * | |
| Body mass index (kg/m2) | >30 | Reference | |||
| 25–30 | 1.120 | 1.003 | 1.250 | 0.044 | |
| 18.5–25 | 1.009 | 0.734 | 1.387 | 0.958 | |
| <18.5 | 1.109 | 0.995 | 1.236 | 0.062 | |
| Self-rated health status | Fair or poor | Reference | |||
| Good | 1.169 | 0.997 | 1.370 | 0.054 | |
| Very good or excellent | 1.024 | 0.870 | 1.205 | 0.777 | |
| Number of chronic conditions | 0 | Reference | |||
| 1 | 0.897 | 0.809 | 0.995 | 0.040 | |
| 2 | 0.795 | 0.686 | 0.921 | 0.002 * | |
| 3 | 0.912 | 0.737 | 1.129 | 0.398 | |
| 4 or more | 1.162 | 0.894 | 1.510 | 0.261 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bishop, F.L.; Lauche, R.; Cramer, H.; Pinto, J.W.; Leung, B.; Hall, H.; Leach, M.; Chung, V.C.; Sundberg, T.; Zhang, Y.; et al. Health Behavior Change and Complementary Medicine Use: National Health Interview Survey 2012. Medicina 2019, 55, 632. https://doi.org/10.3390/medicina55100632
Bishop FL, Lauche R, Cramer H, Pinto JW, Leung B, Hall H, Leach M, Chung VC, Sundberg T, Zhang Y, et al. Health Behavior Change and Complementary Medicine Use: National Health Interview Survey 2012. Medicina. 2019; 55(10):632. https://doi.org/10.3390/medicina55100632
Chicago/Turabian StyleBishop, Felicity L, Romy Lauche, Holger Cramer, Jonquil W Pinto, Brenda Leung, Helen Hall, Matthew Leach, Vincent CH Chung, Tobias Sundberg, Yan Zhang, and et al. 2019. "Health Behavior Change and Complementary Medicine Use: National Health Interview Survey 2012" Medicina 55, no. 10: 632. https://doi.org/10.3390/medicina55100632
APA StyleBishop, F. L., Lauche, R., Cramer, H., Pinto, J. W., Leung, B., Hall, H., Leach, M., Chung, V. C., Sundberg, T., Zhang, Y., Steel, A., Ward, L., Sibbritt, D., & Adams, J. (2019). Health Behavior Change and Complementary Medicine Use: National Health Interview Survey 2012. Medicina, 55(10), 632. https://doi.org/10.3390/medicina55100632