Abstract
Introduction: This study aimed to evaluate mandibular molar changes after distalization using Class III elastics and modified C-palatal plates (MCPPs) in the maxilla and to use CBCT to specifically analyze the third-molar position after long-term retention in adolescents. Methods: The sample consisted of 65 mandibular third molars from 35 subjects, divided into two groups. Twenty-six of the third molars were from fourteen adolescent patients with Class I bimaxillary protrusion (mean age, 12.8 years) who had undergone bilateral maxillary distalization using an MCPP and mandibular distalization with Class III elastics with non-extraction treatment. For the control group, 39 third molars from 21 Class I normal-occlusion subjects were used. In the treated group, CBCT images were taken before distalization (T1), after molar distalization (T2), and at a long-term observation point (6.1 ± 2.7 years) (T3). Repeated measures ANOVA and a post hoc test with Bonferroni correction were used to analyze significant differences in the positions at the three points in time. Results: There were 2.3 and 1.7 mm of distal movement at the crown of the mandibular first and second molars, with distal tipping of 5.2° and 5.3°, respectively, and 3.0° of distal tipping of the third molars. Comparing the treated group with the control group at T3, there was a significant change in the angulation of the third molars (p < 0.001). In the long-term, the third molars from the treated group showed a downward and buccal position after distalization. Conclusions: In the long term, the developing mandibular third molar buds had downward and buccal positional changes after total arch distalization. These findings suggest the need for clinicians to consider the possibility of the impaction of developing third molars after mandibular total arch distalization in adolescents.
1. Introduction
Bimaxillary dentoalveolar protrusion is characterized by the flaring of the anterior teeth and facial convexity. The retraction of anterior teeth after premolar extractions has been the standard orthodontic approach to reduce facial convexity [1,2].
Currently, however, temporary skeletal anchorage devices (TSADs) have become an important modality in orthodontics, reducing the need for extraction while allowing the distalization of the maxillary dentition [3,4,5].
A promising non-extraction treatment modality to consider for the correction of bimaxillary protrusion is molar distalization. To reduce bimaxillary protrusion, maxillary molar distalization should be performed concurrently with mandibular molar distalization.
Oh et al. [4] reported that with microimplant-aided sliding mechanics, crowding could be resolved while improving facial esthetics by retracting the lips with the distalization of the maxillary and mandibular posterior teeth without extraction. Chen et al. [6] demonstrated a novel technique to treat bimaxillary protrusion using miniscrews to extract only an impacted third molar without the extraction of the premolars.
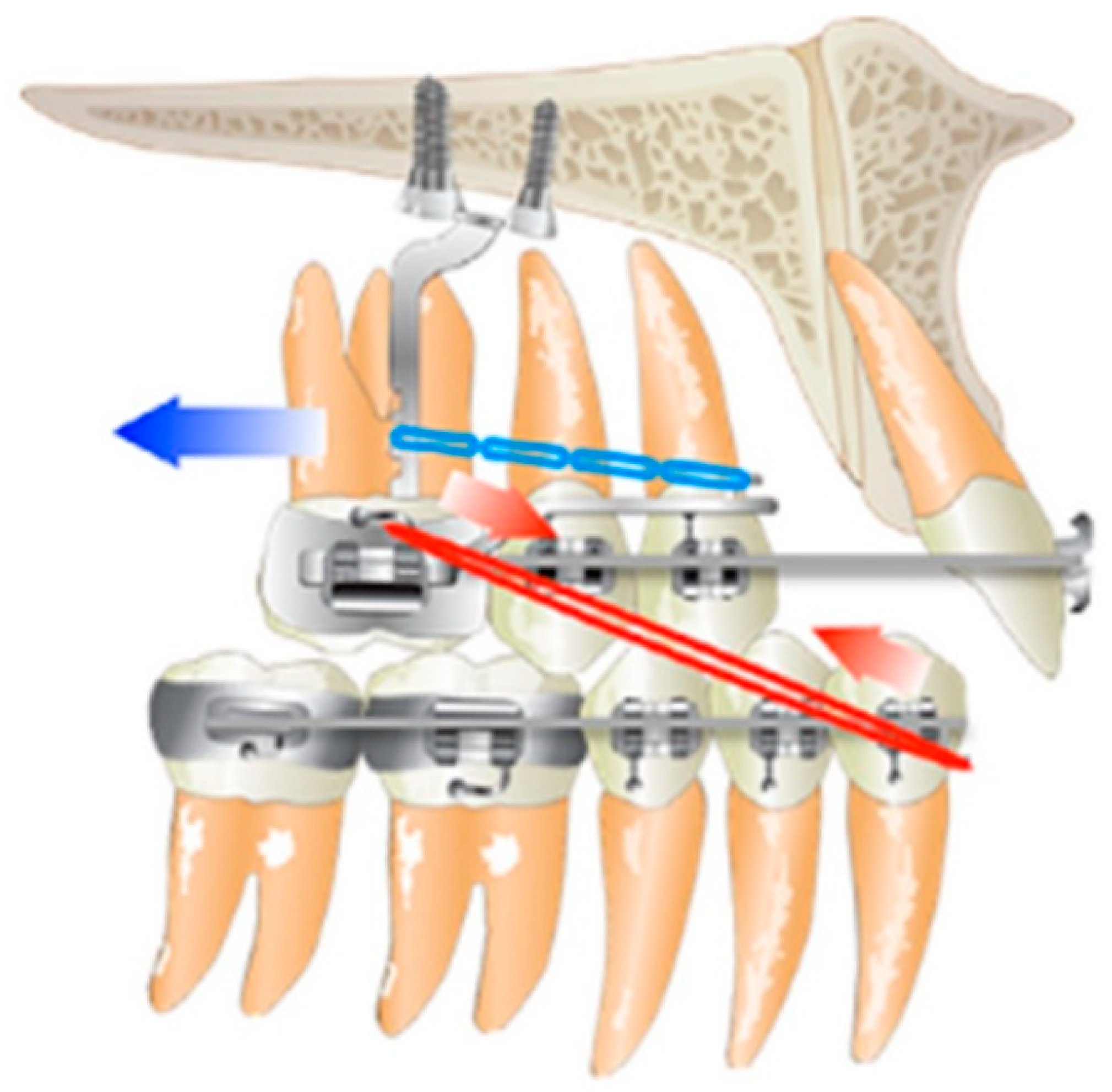
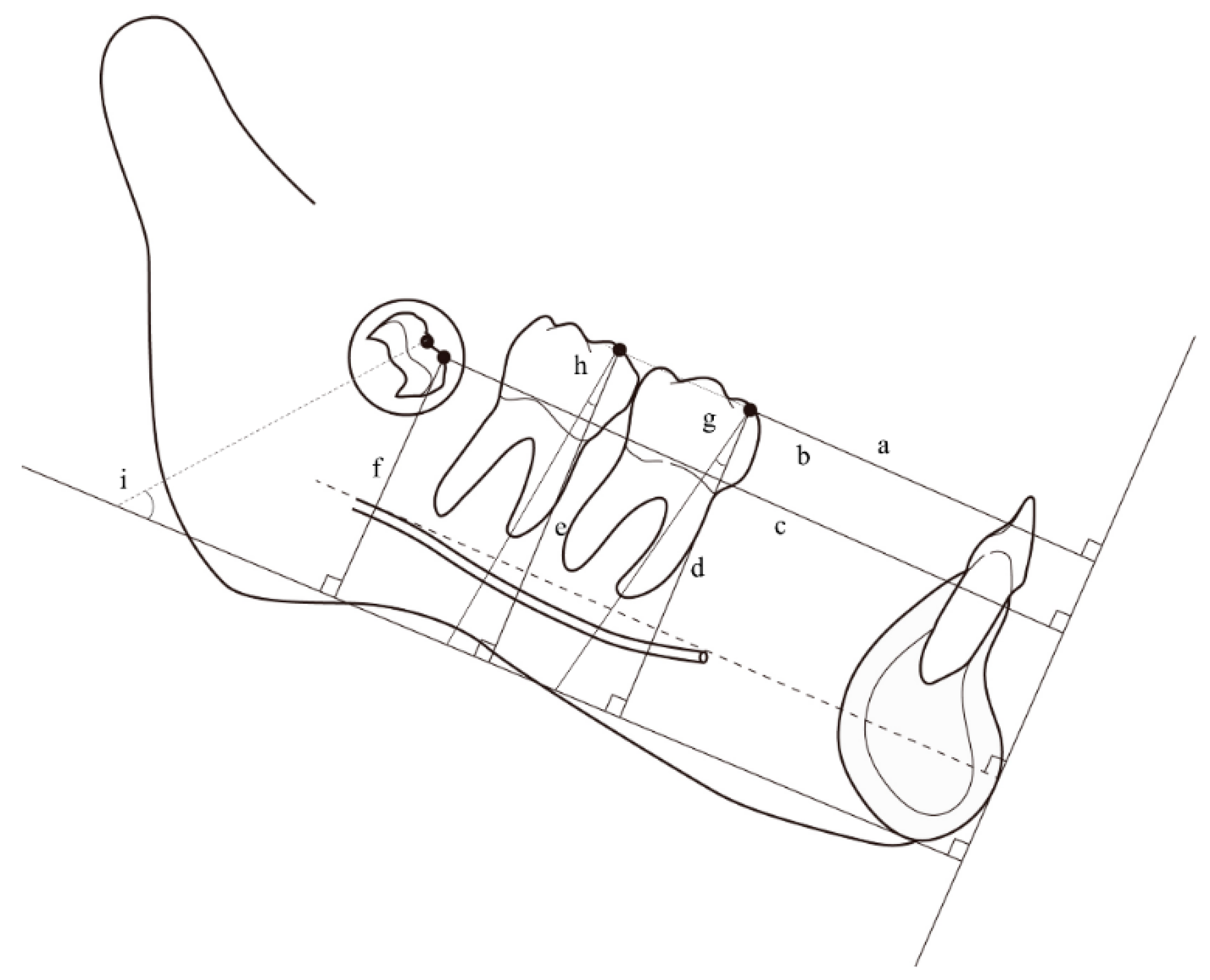
In other cases, miniplates, as well as miniscrews, were efficiently used for total mandibular arch distalization. Kook et al. [7] presented improved lip protrusion, and retroclination of the upper and lower incisors was achieved with non-extraction treatment using a modified C-palatal plate (MCPP) and intermaxillary elastics in a bimaxillary patient (Figure 1). Sugawara et al. [1] reported that the miniplate is a useful tool for moving mandibular molars distally to correct anterior crossbite or mandibular anterior crowding.
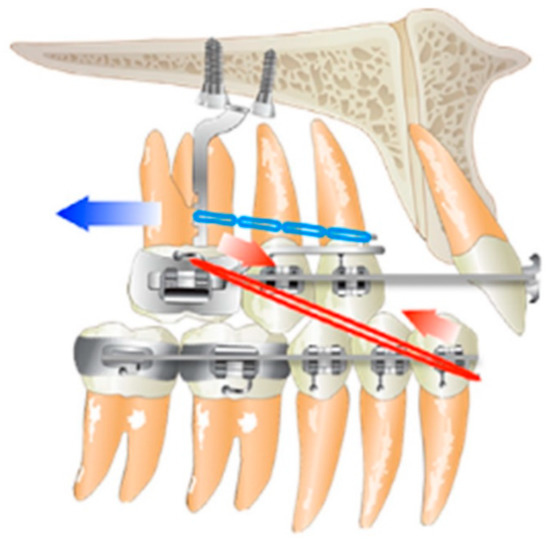
Figure 1.
Schematic drawing of Class III elastics and a maxillary MCPP for total arch distalization.
Further, Yeon et al. [8] evaluated the differences in treatment effects between arch distalization using buccal miniscrews and ramal plates in the mandibular dentition. They suggested that the ramal plates presented more molar distalization than could be achieved with buccal miniscrews.
Traditionally, Class III elastics have been used to correct protrusions of the mandibular dentition. This approach caused the distal tipping of molars, incisor uprighting, and anti-clockwise rotation of the occlusal plane, correcting lower-lip protrusion [9,10], but causing the extrusion and mesialization of the maxillary posterior teeth. To avoid this drawback, He et al. [11] successfully used the multiloop edgewise archwire technique and Class III elastics with mini-implants for a compromised treatment of Class III malocclusion.
During distalization, third molars, which are more likely to become impacted in general, should be the primary concern of clinicians. The eruption space of the third molar is affected by bone remodeling and orthodontic treatment. With the distalization of the maxillary third molars, the use of germectomy prior to applying a pendulum in growing patients has been proposed [12], because non-extraction treatment is significantly associated with increased third-molar impaction rates [13,14].
When Park et al. [15] evaluated the three-dimensional position of the maxillary molars during retention using cone-beam computed tomography (CBCT), they concluded that second molars can fully erupt and that the third molars in both the groups they studied presented a favorable position after distalization. Recently, Kang et al. [16] evaluated the long-term position of erupted third molars after maxillary total arch distalization using MCPPs in adolescents. They reported that maxillary third molars erupt spontaneously over time in spite of their position after distalization.
This is encouraging because prior to mandibular molar distalization, several studies recommended the extraction of the third molar [4,6,17,18]. To the best of our knowledge, no long-term evaluations of the positional changes of mandibular third molars have been reported. In addition, only a few studies have evaluated Class III effects in the mandible using maxillary TSADs as indirect anchorages.
Therefore, this study aimed to evaluate mandibular molar changes after distalization using Class III elastic and maxillary MCPPs as indirect anchorages and to use CBCT to specifically analyze the third-molar position after long-term retention in adolescents.
2. Materials and Methods
This retrospective study was approved by the Institutional Review Board at the Catholic University of Korea (IRB number KC21RISI0767).
The study sample comprised 65 third molars from 35 subjects, divided into two groups. The treatment group included 26 third molars from 14 adolescent patients with Class I bimaxillary protrusion (mean age, 12.8 years), who underwent bilateral maxillary distalization with a modified C-palatal plate (MCPP) and mandibular distalization with Class III elastics at the Department of Orthodontics, Seoul St. Mary’s Hospital, The Catholic University of Korea, between January 2009 and December 2013. CBCT images were scanned at pre- and post-molar-distalization (mean duration, 15.8 months) for evaluation during pre- and post-treatment. Long-term data (mean period, 6.1 years) were extracted from the CBCT images. In addition, there were 21 Class I subjects in the control group with 39 mandibular third molars, of which CBCT images were been taken for purposes other than this research, such as for periodontic treatment or due to pathologic disease (Table 1).

Table 1.
Baseline characteristics of subjects in the treated and control groups.
The inclusion criteria of the treated group for this study were: (1) age range of 12 to 14 years, (2) Class I molar with bimaxillary protrusion, (3) unilateral or bilateral development of mandibular third molars, and (4) retention period of more than 4 years. For the comparison with the third-molar position at retention (T3) in treated group, control group included 21 participants with normal occlusion, (1) mean age 21.3 ± 1.6 years, (2) Class I occlusion with a normal overbite and overjet range of 1 to 3 mm, (3) crowding ≤ 2 mm, (4) no asymmetry or crossbite, and (5) the presence of third molars.
An i-CAT computed tomography scanner (Imaging Science International, Hatfield, PA, USA), which had 120 kVp, 47.7 mA, a standard voxel size of 0.4 mm, and a 200 × 400-mm field of view, was used for all patients. An MCPP was used to distalize the maxillary dentition, while Class III elastics were applied to distalize the mandibular dentition.
2.1. CBCT Reference Planes and Measurements
The CBCT imaging results were converted to the Digital Imaging and Communications in Medicine (DICOM) format. These DICOM data were three-dimensionally reconstructed using InVivo software (version 5.3; Anatomage, San Jose, CA, USA) before analyzing. The orientation and measurements were performed by single examiner (K.J).
Repeated measurements were calculated to analyze the intraclass correlation coefficient (ICC). The ICC values showed intrarater reliability ranging from 0.92 to 0.95. In addition, 10 cases were measured by another examiner (JHK) to assess the interexaminer reliability using the ICC test; and the results showed 0.99 of good inter-rater reliability. Landmarks were additionally digitized; the mesiobuccal (MB) and distobuccal (DB) cusps and the distance from the MB cusp of mandibular molar to the horizontal, frontal, and sagittal planes were measured.
As X-axis, the horizontal plane was defined as the plane passing through the menton and parallel to a plane extending through the right and left mental foramen and pogonion.
As Y-axis, the sagittal plane was defined as the plane perpendicular to the horizontal plane at the menton and passing through the B point.
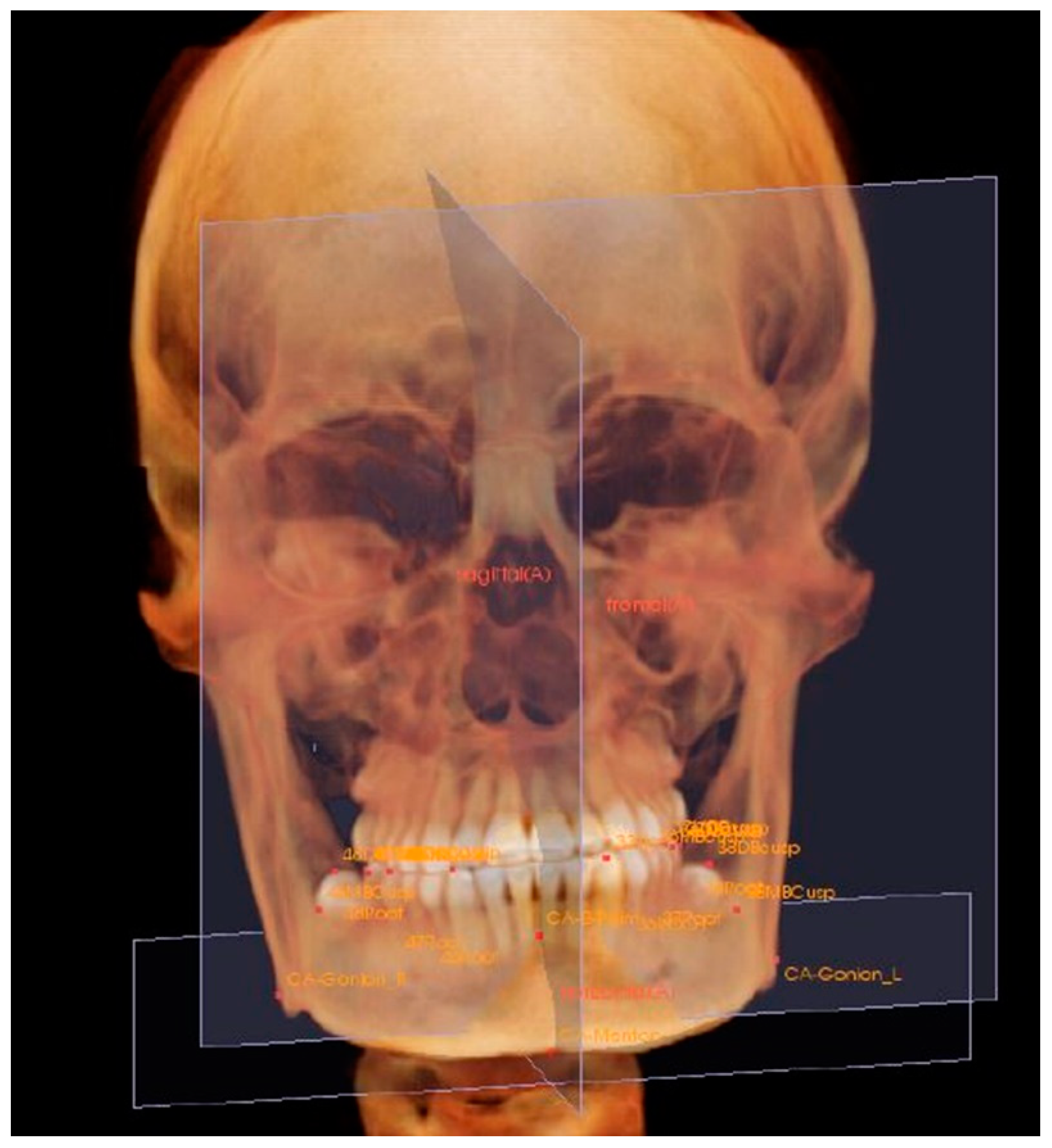
As Z-axis, the frontal plane was defined as the plane perpendicular to both planes and passing through the pogonion (Figure 2).
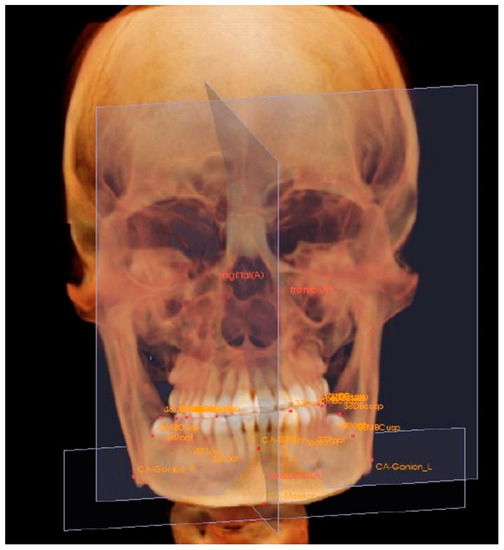
Figure 2.
Reorientation of X, Y, and Z reference planes using landmarks: menton; gonion; B point; pogonion; mental foramen. The horizontal plane (X-axis) was the plane passing the menton and parallel to a plane extending through the right and left mental foramen and pogonion. The sagittal plane (Y-axis) was perpendicular to the horizontal plane at the menton and passed through the B point. The frontal plane (Z-axis) was perpendicular to both planes and passed through the pogonion.
The distances from the MB cusps of mandibular first, second, and third molars to horizontal, sagittal, and frontal planes were measured. The distances from the frontal plane to each MB cusp of the lower posterior teeth were measured parallel to reference line from pogonion to the superior point of mental foramen.
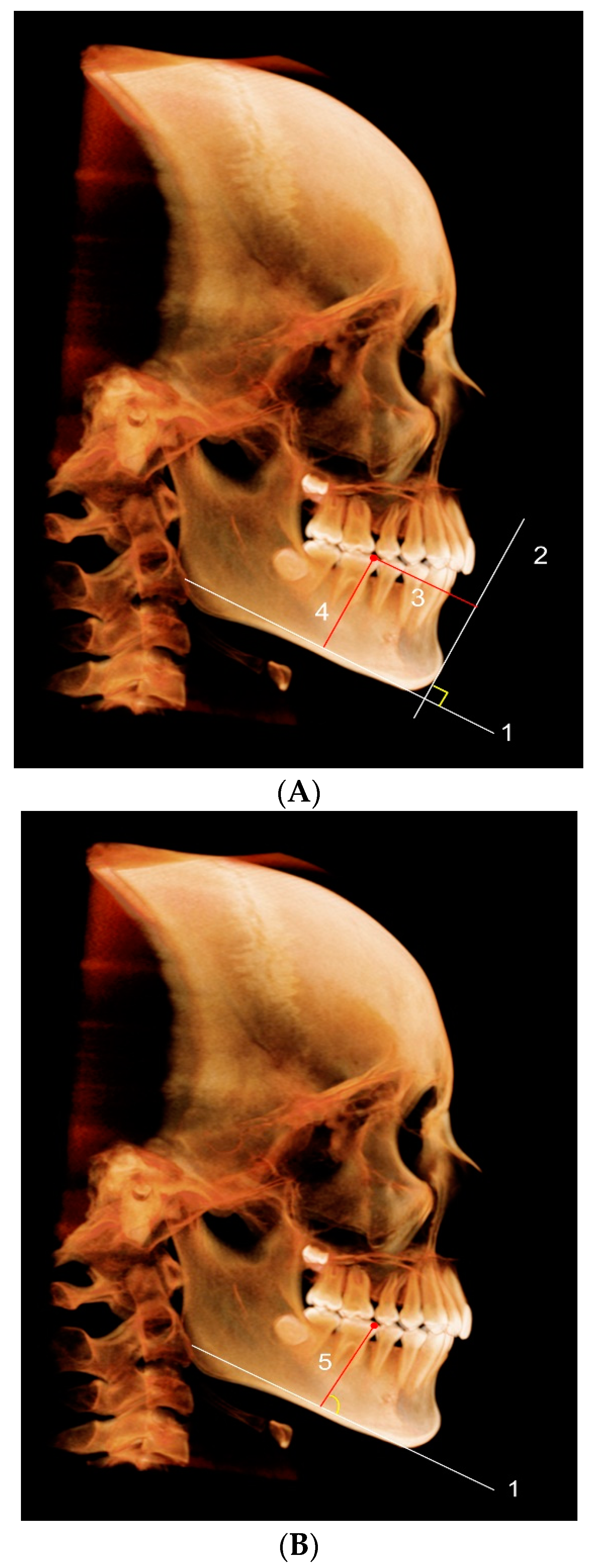
The positional changes on each plane were assessed by the distance differences pre- and post- distalization, and after long-term retention (Figure 3A).
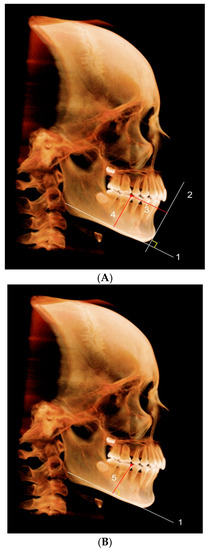
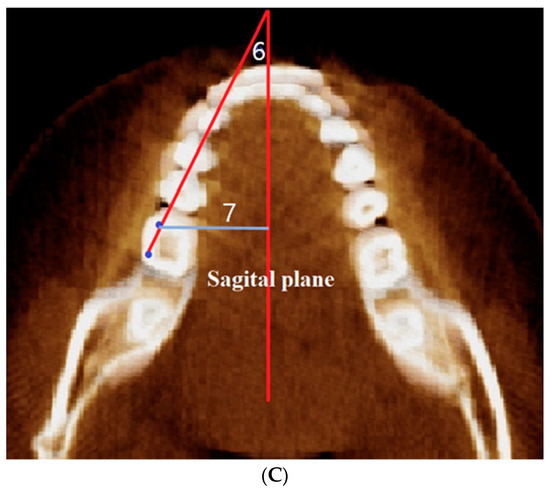
Figure 3.
(A) Position of the mandibular right first molar: (1) Horizontal plane; (2); frontal plane; (3) the distance from the mesiobuccal cusp to the frontal plane (Z); (4) the distance from the mesiobuccal cusp to the horizontal plane (X). (B) Angulation of the mandibular first molar: (5) The angle between the long axis of the first molar (mesiobuccal cusp-mesial root tip) and the horizontal plane (X). (C) Rotation of the mandibular first molar: (6) The angle between the crown axis of the first molar (mesiobuccal cusp-distobuccal cusp) and sagittal (Y) plane projected on the horizontal (X) plane; (7) the distance from the mesiobuccal cusp to the sagittal (Y) plane.
The angles between the horizontal plane and long axis of first and second molars, which were set as line from the MB cusp to the tip of mesial root, were calculated. The angulation of third molar was defined as the line from midpoint of the crown to that of developing root. The angulation changes of the posterior teeth were analyzed (Figure 3B).
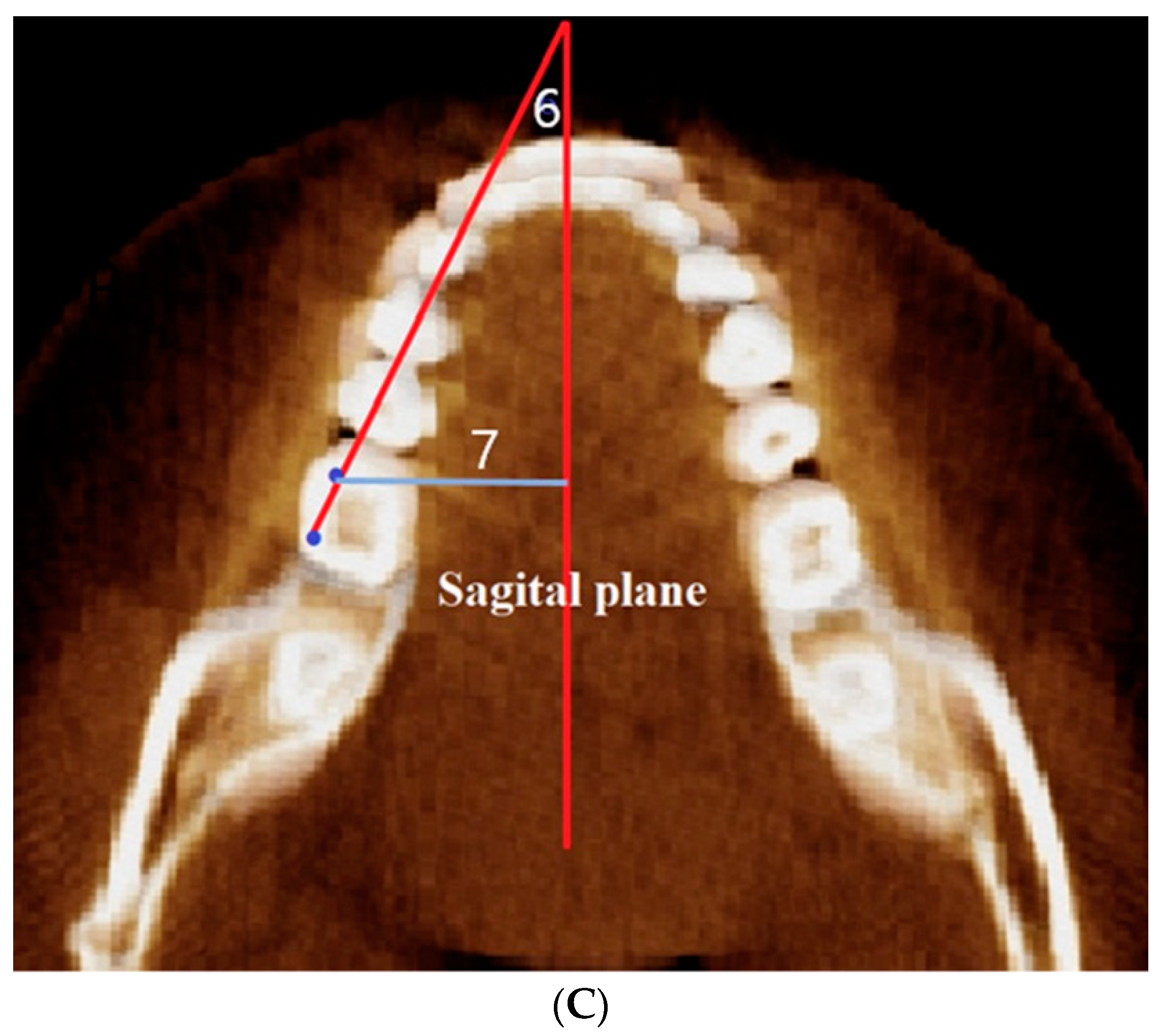
The angles were analyzed between sagittal plane projected on horizontal plane and the crown axis of molars, a line tangential to the MB and DB cusps. The change in rotation of maxillary molars was also measured (Figure 3C and Figure 4).
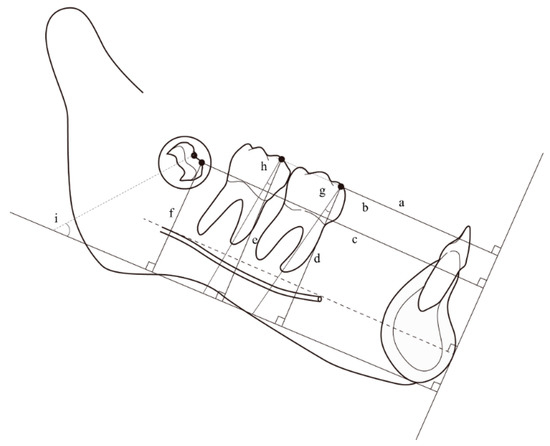
Figure 4.
Schematic illustration of the measurements. (a–c) Distance between the MB cusp of each tooth and the frontal plane; (d–f) distance between the MB cusp of each tooth and the horizontal plane; (g–i) angulation of each tooth to the horizontal plane. The first and second molar axis were defined as extending through the MB cusp and apex of the mesial root. The third molar axis was defined and extended through the midpoint of the crown and the mesial and distal endpoint of the developing root.
2.2. Statistical Analysis
With IBM SPSS software, version 26.0 (SPSS Inc., Chicago, IL, USA), post hoc repeated-measures ANOVA (RMANOVA) analysis with Bonferroni corrections was used to evaluate the significance between pre-treatment with post-treatment (P1), between pretreatment and after retention (P2), and between post-treatment and after retention (P3). RMANOVA was used to compare variables between (T3) and the control group for analysis. Differences with probabilities of less than 5% (p < 0.05) were considered statistically significant.
3. Results
Table 2 shows the measurements of each posterior tooth’s angulation, rotation, position, and width at predistalization, postdistalization, and postretention in the treatment group.

Table 2.
Measurements of predistalization, postdistalization and long-term retention treated group.
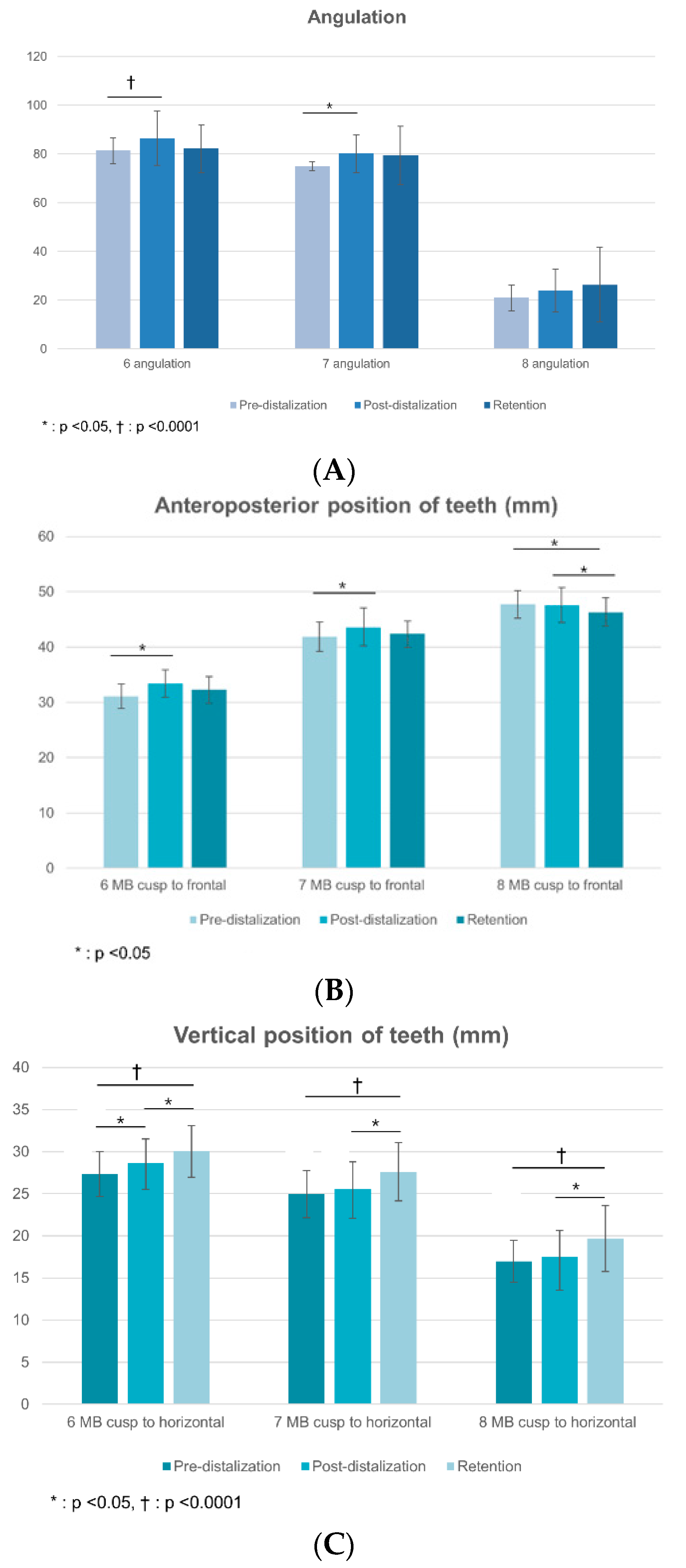
The mandibular first and second molars showed significant distal movement, of 2.3 and 1.7 mm (p < 0.05), with distal crown tipping of 5.2° and 5.3° and extrusion of 1.3 and 0.6 mm, respectively, after total arch distalization. Notably, there were no significant changes in the distal tipping of the third molars (Figure 5).
Figure 5.
Bar graphs of angulation and frontal and horizontal positional changes at predistalization, postdistalization, and long-term retention in the treated group. (A) Angulation. (B) Frontal positional change. (C) Horizontal positional change.
The mandibular first and second molars moved insignificantly mesially by 1.1 and 1.3 mm during the retention period. The first molars showed mesial tipping of 4.5° (p = 0.001) (Table 3).

Table 3.
Changes in post-distalization and long-term retention of the treated group.
Comparing the treated group with the control group post-retention, there were no significant differences in the positions of the first and second molars in either group. However, a significant difference was observed in the angulations of the third molars between the treated and control groups, which were 26.3° and 71.4°, respectively (p < 0.001) (Table 4).

Table 4.
Comparison of the measurements among long-term retention and the control group.
Regarding the vertical positions of the third molars, the treatment group showed a more downward position than the control group; the respective values were 19.7 mm and 22.7 mm, respectively (p = 0.002). Furthermore, regarding the evaluation of the transverse position, the treated group had a more buccal position than the control group; the respective values were 39.0 mm versus 35.1 mm (p = 0.001).
Regarding the mandibular intercanine width, the treated group presented a significant increase compared to the control group, of 28.0 mm versus 26.9 mm (p < 0.05).
4. Discussion
Total arch distalization of the mandible in Class I bimaxillary protrusion cases can cause posterior crowding, which, in turn, can change the positions of developing third molars in adolescents [7]. Until now, there were no studies using CBCT to analyze the positional changes of molars after the distalization of mandibular dentition. In this study, mandibular third-molar positions were evaluated in Class III patients treated with elastics and maxillary MCPPs for total arch distalization.
The mandibular first molars of the treated group in our study showed 2.3 mm of distalization, with distal crown tipping of 5.2° and extrusion of 1.3 mm, in patients distalized using Class III elastics. Nakamura et al. [19] demonstrated 3.0-mm distal movement with 6.2° distal tipping with TSADs. Furthermore, Yu et al. [20] reported 3.2-mm distal movement and 4.6° distal tipping with a ramal plate. Our results showed less distal movement compared to the results in other reports because we used Class III elastics instead of TSADs in the mandible.
After post-distalization, the samples in this study consisted of adolescents aged 14.4 ± 1.3 with cervical vertebral maturation stages (CVMSs) of CS3 and CS4 (Table 1). Gu et al. [21] found that the peak increase in mandibular length occurs during this stage. Another report showed that continued accelerated craniofacial growth can be anticipated in the CS4 stage [22]. Interestingly, the treated group and the control group had the same CVMSs, of CS5 and CS6, post-retention, as seen in Table 1.
Orthodontic appliances that produce posterior movement of the mandibular dentition, either through the tipping of individual teeth or through the translation of the dentition, may restrict the space for second and third molars, which can cause impaction of third molars [23,24,25,26].
It is known that the third molars to show mesioangular and unfavorable positions in the long-term. Kinzinger et al. [12] evaluated the treatment outcomes of maxillary third molars during distalization by modified pendulum. The tooth buds of the third molars acted as a fulcra, causing the second molars to tip approximately 8° to the palatal plane after 2.6-mm distalization. In addition, Kang et al. [27] demonstrated this effect by using the three-dimensional finite element method. The presence or absence of third-molar follicles did not significantly affect the movement of the first molars in their study.
Several studies reported that premolar extraction treatment might produce posterior space and reduce the potential of third-molar impaction [28,29]. Regarding the vertical and horizontal positions in our case, the lower third molars in the treatment group showed a more downward and mesial position compared to those in the control group. Accordingly, the potential for third-molar impaction could be high. On the other hand, Kang et al. [16] reported that third molars moved distally and downward or distally and upward after maxillary molar distalization. However, they also demonstrated that maxillary third molars show spontaneous eruption over time, despite their position after distalization.
With regard to the positional changes of third molars after distalization, significant tipping, of 8.9°, was observed in the treated group. To reduce this distinct tipping of second molars during molar distalization, a surgical extraction of the third molar bud was recommended due to fulcrum action [12]. Unfortunately, the study had a limited evaluation immediately after distalization with a few patients in the germectomy group and only used two-dimensional images.
In our study, stable structures were applied in the mandible to evaluate the positional changes in the three stages (pre- and post-distalization and retention). Oh et al. [30] evaluated mandibular and dentoalveolar changes using functional appliances based on the mandibular reference plane with Björk’s structural method on a two-dimensional cephalometric radiograph, while we used CBCT images to analyze a three-dimensional determination of stable structures in the mandible, as seen in Figure 4. Adams et al. [31] showed that three-dimensional evaluations are more precise and accurate than the two-dimensional approach. Nguyen et al. [32] demonstrated that the anterior contour of bony chin at pogonion showed no remodeling, while Chen et al. [33] showed that as a stable structure in the mandible, the mental foramen can be used for regional superimposition in the three-dimensional mandibular evaluation of growing patients. In our study with CBCT images, we used a reference line from the pogonion to the superior point of the mental foramen as stable structures to evaluate the anterioposterior movement of the lower posterior teeth.
Regarding maxillary third molars, the distalization of posterior teeth can occur in adolescents who have retained third molars [27]. Molar distalization has no significant impact on the normal eruption of maxillary third molars, which suggests that surgical removal may not be required prior to distalizing maxillary molars in adolescents with developing third molars [16,34].
Additionally, Chen et al. [35] reported that the increased posterior available space in the mandible was mainly due to bony resorption on the anterior border of the ramus in growing patients. They also found that the average available spaces increased by 1.2 mm in females under the age of 16 and by 1.5 mm in males under the age of 17 per side, annually. Our study found that the mandibular third molars showed a downward and buccal position after distalization in the long-term compared with the control group. This means that clinically, there is a possibility that third molars could be impacted after distalizing mandibular dentition in adolescents.
In addition, periodontal stability is one of the important factors in patients undergoing orthodontic treatment with skeletal anchorage, such as MCPP. Several clinical indicators of oral hygiene and periodontal status are monitored. For example, the plaque index, bleeding on probing, and other biomarkers can be used to assess the periodontal status of orthodontic patients [36,37]. To prevent the loosening of skeletal anchorage as in implant failure, it is recommended to use chlorhexidine-based mouthwash [38]. For long-term success, periodontal care is required throughout orthodontic treatment and in the maintenance phase.
One limitation of our study was that the control group comprised adult patients whose CBCT data were obtained for purposes other than this research, such as for periodontic treatment or due to pathologic disease; the longitudinal sample was limited for ethical reasons. Therefore, the positional changes of their third molars could not be evaluated at each treatment stage, as was possible with the treated group. Furthermore, since the control group in this study had a small number of subjects, the evaluation of third molar angulation is needed in a larger sample with a broad age range. In the future, a study is needed to evaluate longitudinal positions in adolescents to demonstrate the treatment effect after distalization using TSADs in the mandible.
5. Conclusions
We evaluated mandibular molar changes after molar distalization and used CBCT to specifically analyze the third-molar position after long-term retention in adolescents.
- The first and second molars exhibited distal movements of 2.3 and 1.7 mm, respectively, with distal crown tipping after distalization. There were no significant changes in the angulations of the third molars.
- The treated group showed a downward and buccal position of the third molars after distalization in the long-term compared to the control group.
These findings suggest that clinicians should consider the possibility of impacted third molars after mandibular distalization in adolescents.
Author Contributions
Conceptualization, N.-K.L. and J.H.P.; data curation, H.-R.H. and J.H.K.; formal analysis, J.K.; investigation, J.H.K. and J.K.; methodology, J.H.P.; software, M.B.; supervision, Y.-A.K.; validation, S.-S.M.; visualization, M.B.; writing—original draft, H.-R.H. and N.-K.L.; Writing—review and editing, S.-S.M. and Y.-A.K. All authors have read and agreed to the published version of the manuscript.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board at the Catholic University of Korea (IRB number KC21RISI0767).
Informed Consent Statement
Written informed consent was obtained from the patient for publication of this short report and any accompanying images.
Data Availability Statement
The authors declare that the materials are available.
Acknowledgments
The authors would like to express their gratitude to Jiyoung Oh (Resident, Department of Orthodontics, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea) for her invaluable contribution to this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sugawara, J.; Daimaruya, T.; Umemori, M.; Nagasaka, H.; Takahashi, I.; Kawamura, H.; Mitani, H. Distal movement of mandibular molars in adult patients with the skeletal anchorage system. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Kook, Y.-A.; Park, J.H.; Bayome, M.; Sa’Aed, N.L. Correction of severe bimaxillary protrusion with first premolar extractions and total arch distalization with palatal anchorage plates. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 310–320. [Google Scholar] [CrossRef] [PubMed]
- Kook, Y.-A.; Bayome, M.; Trang, V.T.T.; Kim, H.-J.; Park, J.H.; Kim, K.B.; Behrents, R.G. Treatment effects of a modified palatal anchorage plate for distalization evaluated with cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Oh, Y.-H.; Park, H.-S.; Kwon, T.-G. Treatment effects of microimplant-aided sliding mechanics on distal retraction of posterior teeth. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 470–481. [Google Scholar] [CrossRef]
- Baccetti, T.; Franchi, L.; Stahl, F. Comparison of 2 comprehensive Class II treatment protocols including the bonded Herbst and headgear appliances: A double-blind study of consecutively treated patients at puberty. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 698.e1–698.e10, discussion 698–699. [Google Scholar] [CrossRef]
- Chen, G.; Teng, F.; Xu, T.-M. Distalization of the maxillary and mandibular dentitions with miniscrew anchorage in a patient with moderate Class I bimaxillary dentoalveolar protrusion. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 401–410. [Google Scholar] [CrossRef]
- Kook, Y.-A.; Park, J.H.; Kim, Y.; Ahn, C.S.; Bayome, M. Sagittal correction of adolescent patients with modified palatal anchorage plate appliances. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 674–684. [Google Scholar] [CrossRef][Green Version]
- Yeon, B.M.; Lee, N.K.; Park, J.H.; Kim, J.M.; Kim, S.H.; Kook, Y.A. Comparison of treatment effects after total mandibular arch distalization with miniscrews vs. ramal plates in Class III patients. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 529–536. [Google Scholar] [CrossRef]
- León-Salazar, V.; Janson, G.; de Freitas, M.R.; de Almeida, R.R.; León-Salazar, R. Nonextraction treatment of a skeletal Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 736–745. [Google Scholar] [CrossRef]
- Lin, J.; Gu, Y. Preliminary investigation of nonsurgical treatment of severe skeletal Class III malocclusion in the permanent dentition. Angle Orthod. 2003, 73, 401–410. [Google Scholar]
- He, S.; Gao, J.; Wamalwa, P.; Wang, Y.; Zou, S.; Chen, S. Camouflage treatment of skeletal Class III malocclusion with multiloop edgewise archwire and modified Class III elastics by maxillary mini-implant anchorage. Angle Orthod. 2013, 83, 630–640. [Google Scholar] [CrossRef] [PubMed]
- Kinzinger, G.S.M.; Fritz, U.B.; Sander, F.G.; Diedrich, P.R. Efficiency of a pendulum appliance for molar distalization related to second and third molar eruption stage. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 8–23. [Google Scholar] [CrossRef] [PubMed]
- Ricketts, R.M. A Principle of Arcial Growth of the Mandible. Angle Orthod. 1972, 42, 368–386. [Google Scholar] [PubMed]
- Kaplan, R.G. Some Factors Related to Mandibular Third Molar Impaction. Angle Orthod. 1975, 45, 153–158. [Google Scholar] [PubMed]
- Park, J.H.; Kim, Y.; Park, J.H.; Lee, N.K.; Kim, S.H.; Kook, Y.A. Long-term evaluation of maxillary molar position after distalization with and without second molar eruption. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 853–861. [Google Scholar] [CrossRef]
- Kang, H.; Lee, N.K.; Kim, J.; Park, J.H.; Kim, Y.; Kook, Y.A. Factors associated with the maxillary third molar position after total arch distalization using a modified C-palatal plate in adolescents. Orthod. Craniofac. Res. 2021, 24 (Suppl. 1), 31–38. [Google Scholar] [CrossRef] [PubMed]
- Kook, Y.A.; Park, J.H.; Bayome, M.; Kim, S.; Han, E.; Kim, C.H. Distalization of the mandibular dentition with a ramal plate for skeletal Class III malocclusion correction. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 364–377. [Google Scholar] [CrossRef]
- Tai, K.; Park, J.H.; Tatamiya, M.; Kojima, Y. Distal movement of the mandibular dentition with temporary skeletal anchorage devices to correct a Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 715–725. [Google Scholar] [CrossRef]
- Nakamura, M.; Kawanabe, N.; Kataoka, T.; Murakami, T.; Yamashiro, T.; Kamioka, H. Comparative evaluation of treatment outcomes between temporary anchorage devices and Class III elastics in Class III malocclusions. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1116–1124. [Google Scholar] [CrossRef]
- Yu, J.; Park, J.H.; Bayome, M.; Kim, S.; Kook, Y.-A.; Kim, Y.; Kim, C.-H. Treatment effects of mandibular total arch distalization using a ramal plate. Korean J. Orthod. 2016, 46, 212–221. [Google Scholar] [CrossRef]
- Gu, Y.; McNamara, J.A., Jr. Mandibular growth changes and cervical vertebral maturation: A cephalometric implant study. Angle Orthod. 2007, 77, 947–953. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A.; Franchi, L. The cervical vertebral maturation method: A user’s guide. Angle Orthod. 2018, 88, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E.; Andreasen, G. Third molars: A review. Am. J. Orthod. 1983, 83, 131–137. [Google Scholar] [CrossRef]
- Vaden, J.L.; Kiser, H.E. Straight talk about extraction and nonextraction: A differential diagnostic decision. Am. J. Orthod. Dentofac. Orthop. 1996, 109, 445–452. [Google Scholar] [CrossRef]
- Richardson, M.E. The etiology and prediction of mandibular third molar impaction. Angle Orthod. 1977, 47, 165–172. [Google Scholar] [PubMed]
- Kim, S.J.; Choi, T.H.; Baik, H.S.; Park, Y.C.; Lee, K.J. Mandibular posterior anatomic limit for molar distalization. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 190–197. [Google Scholar] [CrossRef]
- Kang, J.M.; Park, J.H.; Bayome, M.; Oh, M.; Park, C.O.; Kook, Y.A.; Mo, S.S. A three-dimensional finite element analysis of molar distalization with a palatal plate, pendulum, and headgear according to molar eruption stage. Korean J. Orthod. 2016, 46, 290–300. [Google Scholar] [CrossRef]
- Richardson, M.E.; Richardson, A. Lower third molar development subsequent to second molar extraction. Am. J. Orthod. Dentofac. Orthop. 1993, 104, 566–574. [Google Scholar] [CrossRef]
- Behbehani, F.; Artun, J.; Thalib, L. Prediction of mandibular third-molar impaction in adolescent orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 47–55. [Google Scholar] [CrossRef]
- Oh, E.; Ahn, S.J.; Sonnesen, L. Evaluation of growth changes induced by functional appliances in children with Class II malocclusion: Superimposition of lateral cephalograms on stable structures. Korean J. Orthod. 2020, 50, 170–180. [Google Scholar] [CrossRef]
- Adams, G.L.; Gansky, S.A.; Miller, A.J.; Harrell, W.E., Jr.; Hatcher, D.C. Comparison between traditional 2-dimensional cephalometry and a 3-dimensional approach on human dry skulls. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 397–409. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.; Cevidanes, L.; Franchi, L.; Ruellas, A.; Jackson, T. Three-dimensional mandibular regional superimposition in growing patients. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Al Awadi, M.; Chambers, D.W.; Lagravère-Vich, M.O.; Xu, T.; Oh, H. The three-dimensional stable mandibular landmarks in patients between the ages of 12.5 and 17.1 years. BMC Oral. Health 2020, 20, 153. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-J.; Kook, Y.-A.; Park, J.H.; Park, J.; Bayome, M.; Vaid, N.R.; Kim, Y. Short-term cone-beam computed tomography evaluation of maxillary third molar changes after total arch distalization in adolescents. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 191–197. [Google Scholar] [CrossRef]
- Chen, L.L.; Xu, T.M.; Jiang, J.H.; Zhang, X.Z.; Lin, J.X. Longitudinal changes in mandibular arch posterior space in adolescents with normal occlusion. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 187–193. [Google Scholar] [CrossRef]
- Tecco, S.; Grusovin, M.G.; Sciara, S.; Bova, F.; Pantaleo, G.; Capparé, P. The association between three attitude-related indexes of oral hygiene and secondary implant failures: A retrospective longitudinal study. Int. J. Dent. Hyg. 2018, 16, 372–379. [Google Scholar] [CrossRef]
- Sioustis, I.A.; Martu, M.A.; Aminov, L.; Pavel, M.; Cianga, P.; Kappenberg-Nitescu, D.C.; Luchian, I.; Solomon, S.M.; Martu, S. Salivary Metalloproteinase-8 and Metalloproteinase-9 Evaluation in Patients Undergoing Fixed Orthodontic Treatment before and after Periodontal Therapy. Int. J. Environ. Res. Public Health 2021, 18, 1583. [Google Scholar] [CrossRef]
- Polizzi, E.; Tetè, G.; Bova, F.; Pantaleo, G.; Gastaldi, G.; Capparè, P.; Gherlone, E. Antibacterial Properties and Side Effects of Chlorhexidine-Based Mouthwashes. A Prospective, Randomized Clinical Study. J. Osseointegr. 2019, 12, 2–7. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).