Age, Sex, and Maxillary Position Are Associated with Successful Microimplant-Assisted Rapid Palatal Expansion in Adults
Abstract
:1. Introduction
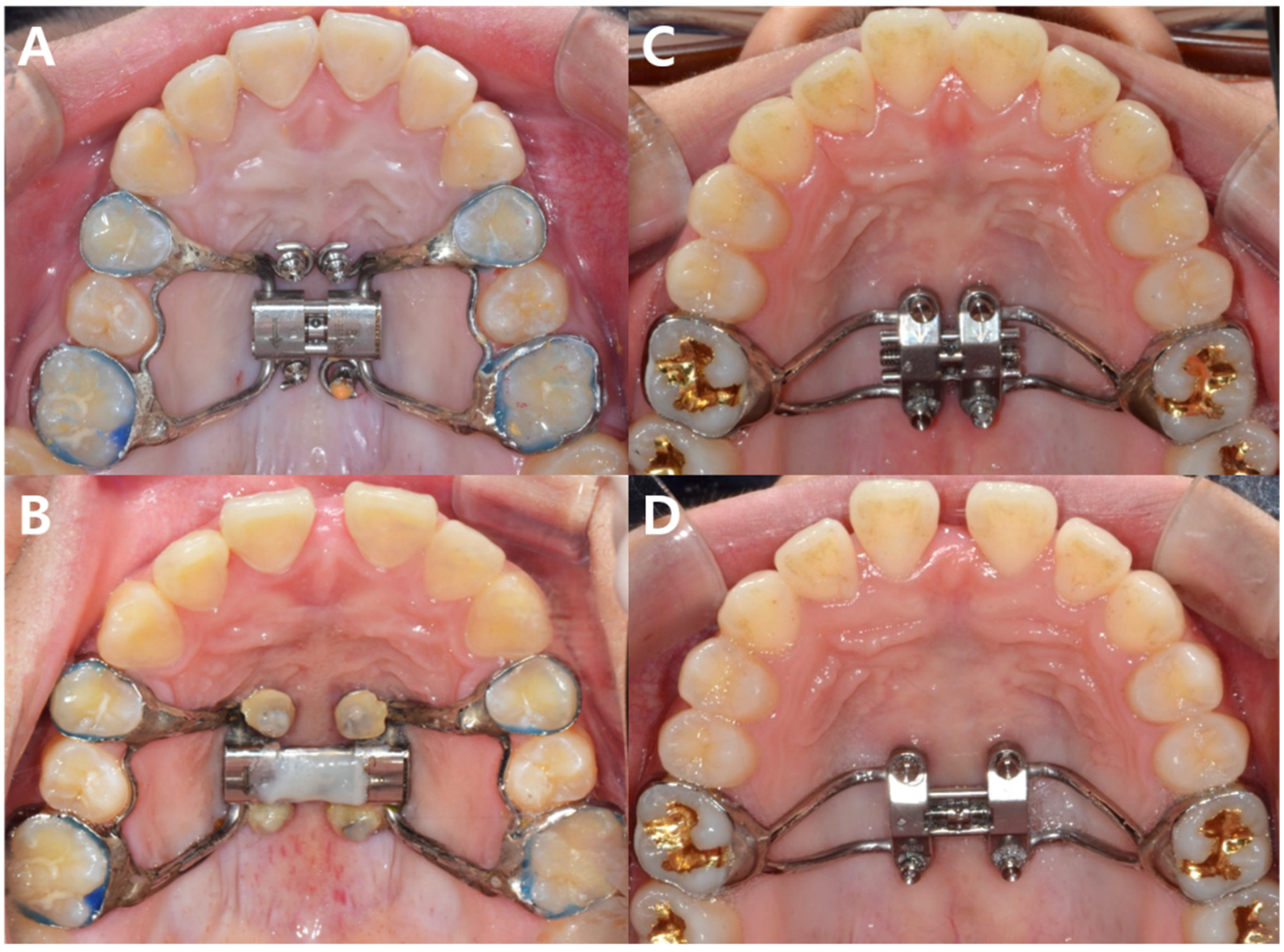
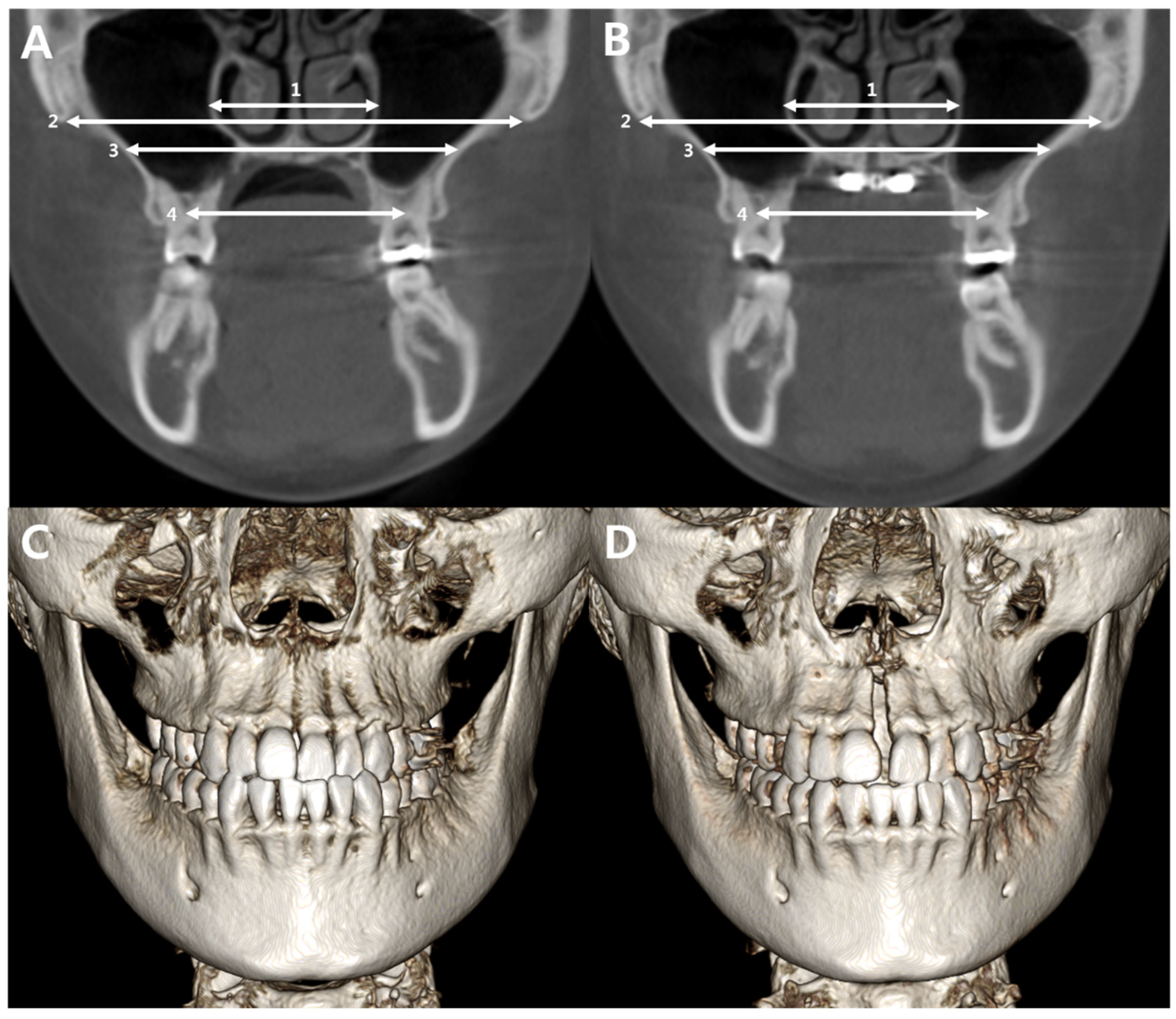
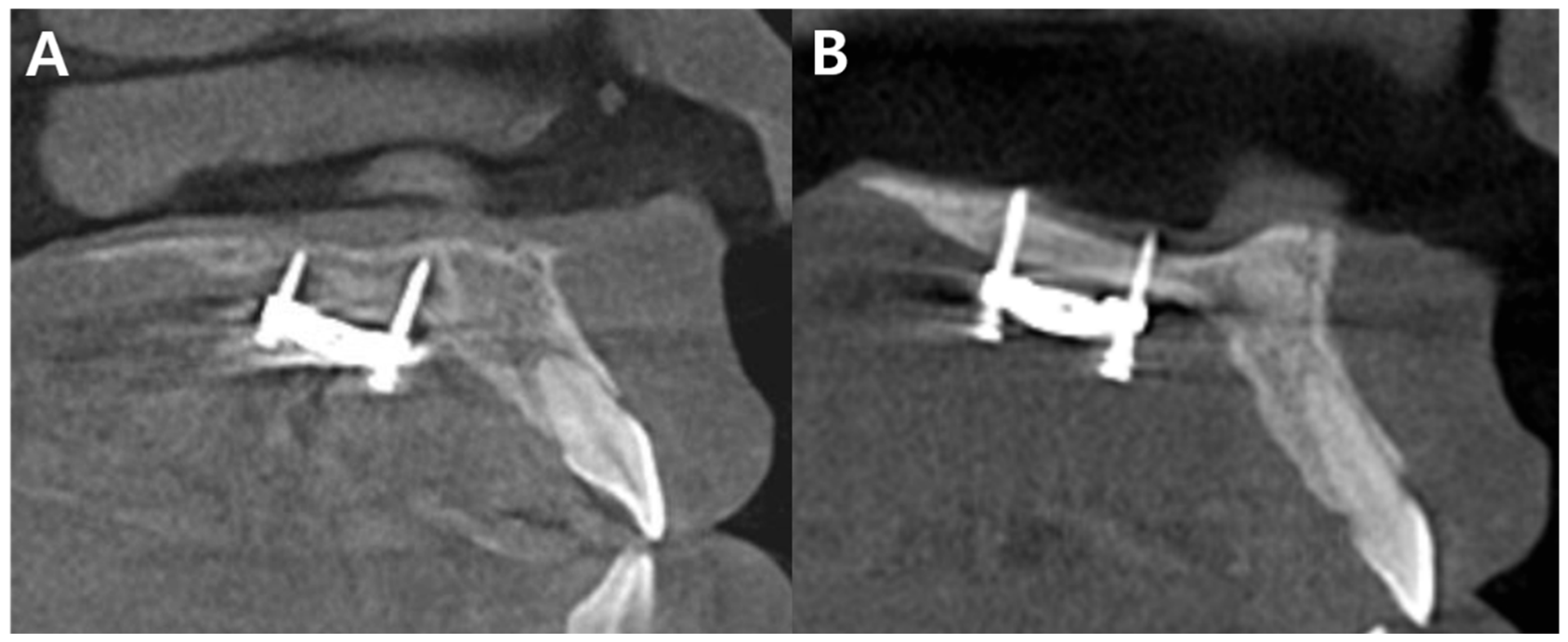
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Perillo, L.; Masucci, C.; Ferro, F.; Apicella, D.; Baccetti, T. Prevalence of orthodontic treatment need in southern Italian schoolchildren. Eur. J. Orthod. 2010, 32, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, T.; Arnlaugsson, S.; Karlsson, K.O.; Ragnarsson, B.; Arnarson, E.O.; Magnusson, T.E. Orthodontic treatment ex-perience and prevalence of malocclusion traits in an Icelandic adult population. Am. J. Orthod. Dentofac. Orthop. 2007, 131, e11–e18. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A. Maxillary transverse deficiency. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 567–570. [Google Scholar] [CrossRef]
- Ramires, T.; Maia, R.A.; Barone, J.R. Nasal cavity changes and the respiratory standard after maxillary expansion. Braz. J. Otorhinolaryngol. 2008, 74, 763–769. [Google Scholar] [CrossRef] [Green Version]
- Seif-Eldin, N.F.; Elkordy, S.A.; Fayed, M.S.; Elbeialy, A.R.; Eid, F.H. Transverse skeletal effects of rapid maxillary expansion in pre and post pubertal subjects: A systematic review. Open Access Maced. J. Med. Sci. 2019, 7, 467–477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lo Giudice, A.; Barbato, E.; Cosentino, L.; Ferraro, C.M.; Leonardi, R. Alveolar bone changes after rapid maxillary expansion with tooth-born appliances: A systematic review. Eur. J. Orthod. 2018, 40, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.M.; Park, Y.C.; Lee, K.J.; Kim, K.H.; Choi, Y.J. Stability of dental, alveolar, and skeletal changes after minis-crew-assisted rapid palatal expansion. Korean J. Orthod. 2017, 47, 313–322. [Google Scholar] [CrossRef] [Green Version]
- Carlson, C.; Sung, J.; McComb, R.W.; Machado, A.W.; Moon, W. Microimplant-assisted rapid palatal expansion appliance to orthopedically correct transverse maxillary deficiency in an adult. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 716–728. [Google Scholar] [CrossRef]
- Choi, S.H.; Shi, K.K.; Cha, J.Y.; Park, Y.C.; Lee, K.J. Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. Angle Orthod. 2016, 86, 713–720. [Google Scholar] [CrossRef] [Green Version]
- Wehrbein, H.; Yildizhan, F. The mid-palatal suture in young adults. A radiological-histological investigation. Eur. J. Orthod. 2001, 23, 105–114. [Google Scholar] [CrossRef] [Green Version]
- Revelo, B.; Fishman, L.S. Maturational evaluation of ossification of the midpalatal suture. Am. J. Orthod. Dentofac. Orthop. 1994, 105, 288–292. [Google Scholar]
- Franchi, L.; Baccetti, T.; McNamara, J.A. Postpubertal assessment of treatment timing for maxillary expansion and protrac-tion therapy followed by fixed appliances. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 555–568. [Google Scholar]
- Baccetti, T.; Franchi, L.; Cameron, C.G.; McNamara, J.A. Treatment timing for rapid maxillary expansion. Angle Orthod. 2001, 71, 343–350. [Google Scholar] [PubMed]
- Angelieri, F.; Cevidanes, L.H.; Franchi, L.; Goncalves, J.R.; Benavides, E.; McNamara, J.A. Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 759–769. [Google Scholar]
- Grunheid, T.; Larson, C.E.; Larson, B.E. Midpalatal suture density ratio: A novel predictor of skeletal response to rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 267–276. [Google Scholar]
- Oliveira, C.B.; Ayub, P.; Angelieri, F.; Murata, W.H.; Suzuki, S.S.; Ravelli, D.B.; Santos-Pinto, A. Evaluation of factors related to the success of miniscrew-assisted rapid palatal expansion. Angle Orthod. 2021, 91, 187–194. [Google Scholar]
- de Jesus, A.S.; de Oliveira, C.B.; Murata, W.H.; Suzuki, S.S.; dos Santos-Pinto, A. Would midpalatal suture characteristics help to predict the success rate of miniscrew-assisted rapid palatal expansion? Am. J. Orthod. Dentofac. Orthop. 2021, 160, 363–373. [Google Scholar]
- Shin, H.; Hwang, C.J.; Lee, K.J.; Choi, Y.J.; Han, S.S.; Yu, H.S. Predictors of midpalatal suture expansion by minis-crew-assisted rapid palatal expansion in young adults: A preliminary study. Korean J. Orthod. 2019, 49, 360–371. [Google Scholar]
- Koo, Y.J.; Choi, S.H.; Keum, B.T.; Yu, H.S.; Hwang, C.J.; Melsen, B.; Lee, K.J. Maxillomandibular arch width differences at estimated centers of resistance: Comparison between normal occlusion and skeletal Class III malocclusion. Korean J. Orthod. 2017, 47, 167–175. [Google Scholar]
- Franchi, L.; Baccetti, T.; McNamara, J.A. Mandibular growth as related to cervical vertebral maturation and body height. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 335–340. [Google Scholar]
- Korbmacher, H.; Schilling, A.; Puschel, K.; Amling, M.; Kahl-Nieke, B. Age-dependent three-dimensional microcomputed tomography analysis of the human midpalatal suture. J. Orofac. Orthop. 2007, 68, 364–376. [Google Scholar] [PubMed]
- Melsen, B. Palatal growth studied on human autopsy material. A histologic microradiographic study. Am. J. Orthod. 1975, 68, 42–54. [Google Scholar] [PubMed]
- Cantarella, D.; Dominguez-Mompell, R.; Moschik, C.; Sfogliano, L.; Elkenawy, I.; Pan, H.C.; Mallya, S.M.; Moon, W. Zy-gomaticomaxillary modifications in the horizontal plane induced by micro-implant-supported skeletal expander, analyzed with CBCT images. Prog. Orthod. 2018, 19, 41. [Google Scholar]
- Knaup, B.; Yildizhan, F.; Wehrbein, H. Age-related changes in the midpalatal suture. A histomorphometric study. J. Orofac. Orthop. 2004, 65, 467–474. [Google Scholar] [PubMed]
- Jimenez-Valdivia, L.M.; Malpartida-Carrillo, V.; Rodriguez-Cardenas, Y.A.; Dias-Da Silveira, H.L.; Arriola-Guillen, L.E. Midpalatal suture maturation stage assessment in adolescents and young adults using cone-beam computed tomography. Prog. Orthod. 2019, 20, 38. [Google Scholar] [PubMed]
- Hartono, N.; Soegiharto, B.M.; Widayati, R. The difference of stress distribution of maxillary expansion using rapid maxillary expander (RME) and maxillary skeletal expander (MSE)—A finite element analysis. Prog. Orthod. 2018, 19, 33. [Google Scholar]
- Lee, H.K.; Bayome, M.; Ahn, C.S.; Kim, S.H.; Kim, K.B.; Mo, S.S.; Kook, Y.A. Stress distribution and displacement by different bone-borne palatal expanders with micro-implants: A three-dimensional finite-element analysis. Eur. J. Orthod. 2014, 36, 531–540. [Google Scholar]
- Yoon, S.; Lee, D.Y.; Jung, S.K. Influence of changing various parameters in miniscrew-assisted rapid palatal expansion: A three-dimensional finite element analysis. Korean J. Orthod. 2019, 49, 150–160. [Google Scholar]
- Oh, H.; Park, J.; Lagravere-Vich, M.O. Comparison of traditional RPE with two types of micro-implant assisted RPE: CBCT study. Semin. Orthod. 2019, 25, 60–68. [Google Scholar]
- Pauwels, R.; Jacobs, R.; Singer, S.R.; Mupparapu, M. CBCT-based bone quality assessment: Are Hounsfield units applicable? Dentomaxillofac. Radiol. 2015, 44, 20140238. [Google Scholar]
| Variables | Total | Sex Differences | ||
|---|---|---|---|---|
| Male (n = 27) | Female (n = 26) | p-Value | ||
| MEAN ± SD | MEAN ± SD | MEAN ± SD | ||
| Age (year) | 25.7 ± 8.7 | 24.6 ± 6.1 | 27 ± 11.1 | 0.343 |
| SNA (°) | 80.5 ± 4.0 | 80.3 ± 4.0 | 80.5 ± 4.2 | 0.798 |
| SNB (°) | 79.8 ± 4.1 | 79.6 ± 4.8 | 79.8 ± 3.6 | 0.893 |
| ANB (°) | 0.7 ± 3.3 | 0.6 ± 3.8 | 0.8 ± 3.0 | 0.870 |
| A-N perp (mm) | −0.2 ± 3.6 | −0.5 ± 4.0 | −0.2 ± 3.2 | 0.815 |
| SN-MP (°) | 34 ± 5.6 | 32.8 ± 5.9 | 35.4 ± 5 | 0.095 |
| Overbite (mm) | 0.6 ± 2 | 1.1 ± 2 | 0.2 ± 1.9 | 0.092 |
| Overjet (mm) | 2.1 ± 2.5 | 1.9 ± 2.7 | 2.4 ± 2.3 | 0.458 |
| Rickett’s LFH (mm) | 48.2 ± 4.4 | 48.5 ± 4.7 | 48.1 ± 4.3 | 0.778 |
| Variables | T1 | T2 | p-Value |
|---|---|---|---|
| SNA (°) | 81.2 ± 3.8 | 82.5 ± 3.6 | <0.001 |
| SNB (°) | 80.9 ± 3.6 | 80.8 ± 3.7 | 0.725 |
| ANB (°) | 0.3 ± 3.2 | 1.6 ± 2.8 | 0.001 |
| A-N perp (mm) | 0.6 ± 3.4 | 1.1 ± 3.2 | <0.001 |
| SN-MP (°) | 34.3 ± 4.7 | 35.6 ± 4.7 | 0.001 |
| Overbite (mm) | 0.3 ± 2.0 | −0.5 ± 1.8 | 0.009 |
| Overjet (mm) | 1.6 ± 2.3 | 2.1 ± 2.4 | 0.091 |
| Rickett’s LFH (mm) | 48.4 ± 4.2 | 49.6 ± 4.2 | 0.002 |
| SNA (°) | 81.2 ± 3.8 | 82.5 ± 3.6 | <0.001 |
| F Group | S Group | p-Value | ||
|---|---|---|---|---|
| (n = 15) | (n = 41) | |||
| Sex | Male | 13 | 16 | 0.002 |
| Female | 2 | 25 | ||
| Appliance type | Hyrax | 3 | 7 | 0.999 |
| MSE | 12 | 34 | ||
| Fixation | Monocortical | 6 | 10 | 0.483 |
| Bicortical | 6 | 20 |
| Independent Variable | B | Odds Ratio | p-Value |
|---|---|---|---|
| Age | −0.140 | 0.869 | 0.019 |
| Sex * | −3.804 | 0.022 | 0.002 |
| A-N perp | 0.464 | 1.591 | 0.015 |
| Rickett’s LFH | 0.234 | 1.264 | 0.084 |
| MPSD_T1 | ZMSD_T1 | SN-MP | ANB | A-Nperp | Age | |
|---|---|---|---|---|---|---|
| Nasal_change | −0.322 | −0.192 | 0.382 * | 0.006 | −0.011 | −0.161 |
| Zygo_change | −0.371 * | −0.192 | −0.002 | −0.139 | 0.004 | −0.211 |
| Palatal_change | −0.027 | −0.038 | 0.350 * | −0.085 | −0.217 | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.-H.; Gil, B.G.; Kim, Y.-J.; Lee, D.-Y. Age, Sex, and Maxillary Position Are Associated with Successful Microimplant-Assisted Rapid Palatal Expansion in Adults. Appl. Sci. 2022, 12, 7324. https://doi.org/10.3390/app12147324
Choi J-H, Gil BG, Kim Y-J, Lee D-Y. Age, Sex, and Maxillary Position Are Associated with Successful Microimplant-Assisted Rapid Palatal Expansion in Adults. Applied Sciences. 2022; 12(14):7324. https://doi.org/10.3390/app12147324
Chicago/Turabian StyleChoi, Jae-Hong, Byung Gyu Gil, Yoon-Ji Kim, and Dong-Yul Lee. 2022. "Age, Sex, and Maxillary Position Are Associated with Successful Microimplant-Assisted Rapid Palatal Expansion in Adults" Applied Sciences 12, no. 14: 7324. https://doi.org/10.3390/app12147324
APA StyleChoi, J.-H., Gil, B. G., Kim, Y.-J., & Lee, D.-Y. (2022). Age, Sex, and Maxillary Position Are Associated with Successful Microimplant-Assisted Rapid Palatal Expansion in Adults. Applied Sciences, 12(14), 7324. https://doi.org/10.3390/app12147324






