Follicle-Targeted Delivery of Betamethasone and Minoxidil Co-Entrapped in Polymeric and Lipid Nanoparticles for Topical Alopecia Areata Treatment
Abstract
:1. Introduction
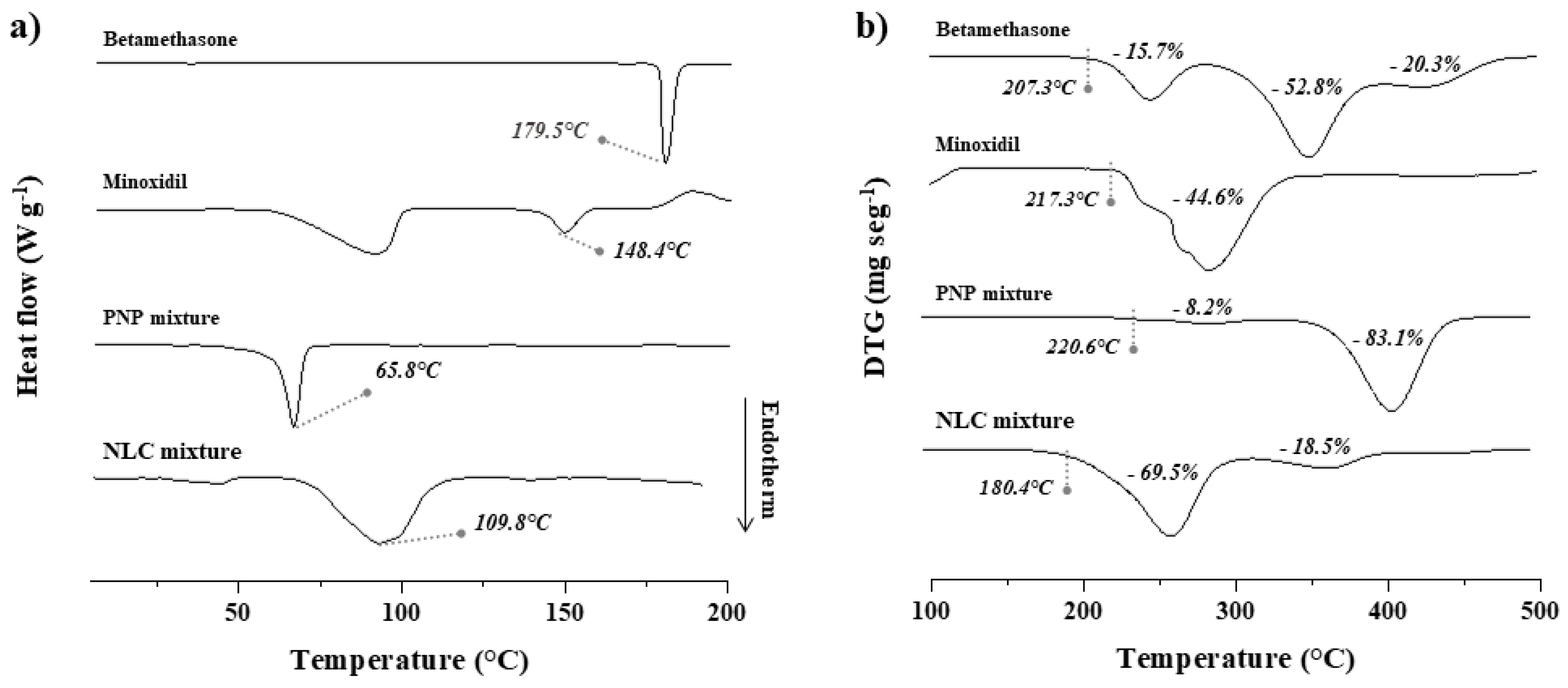
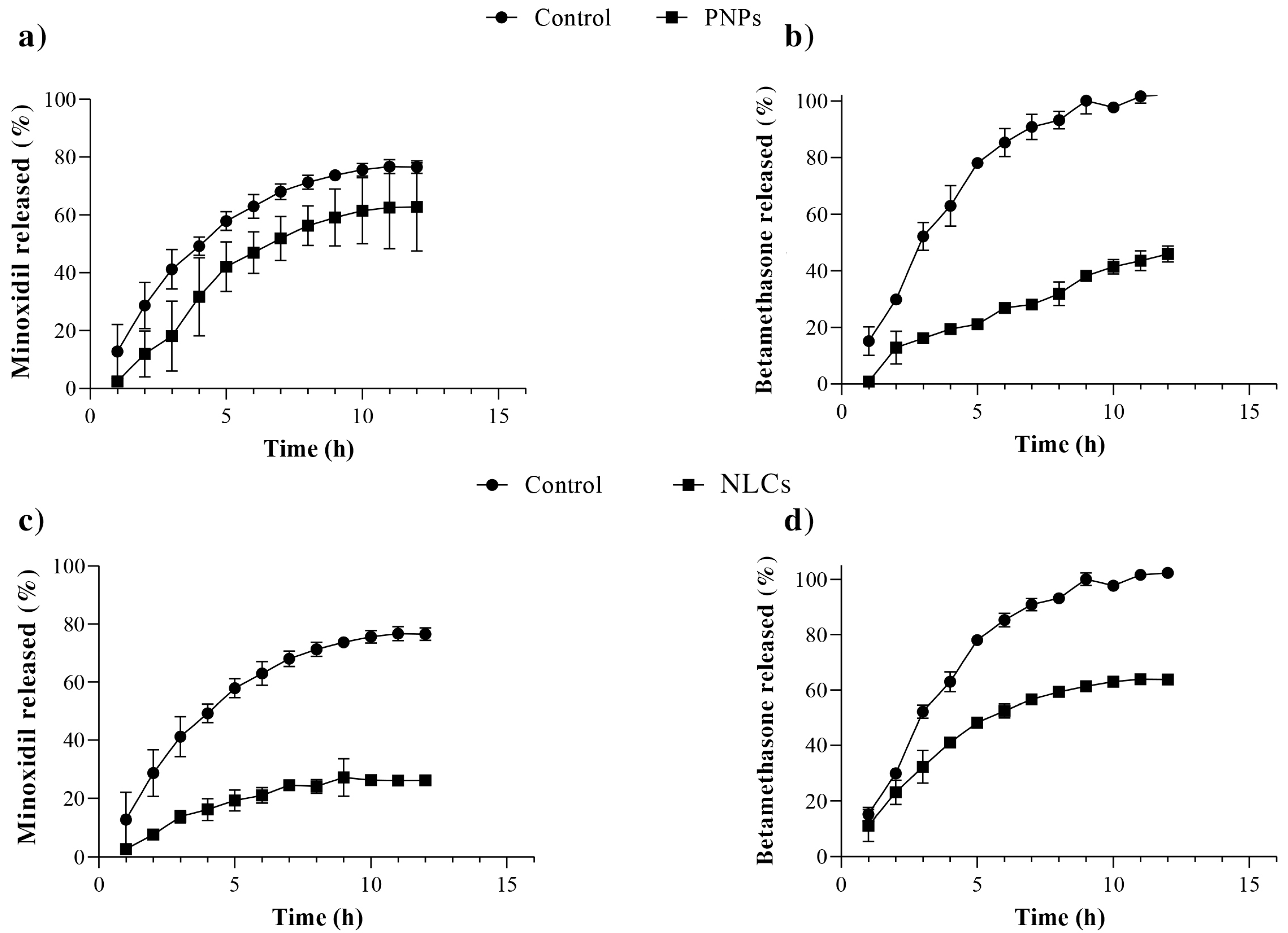
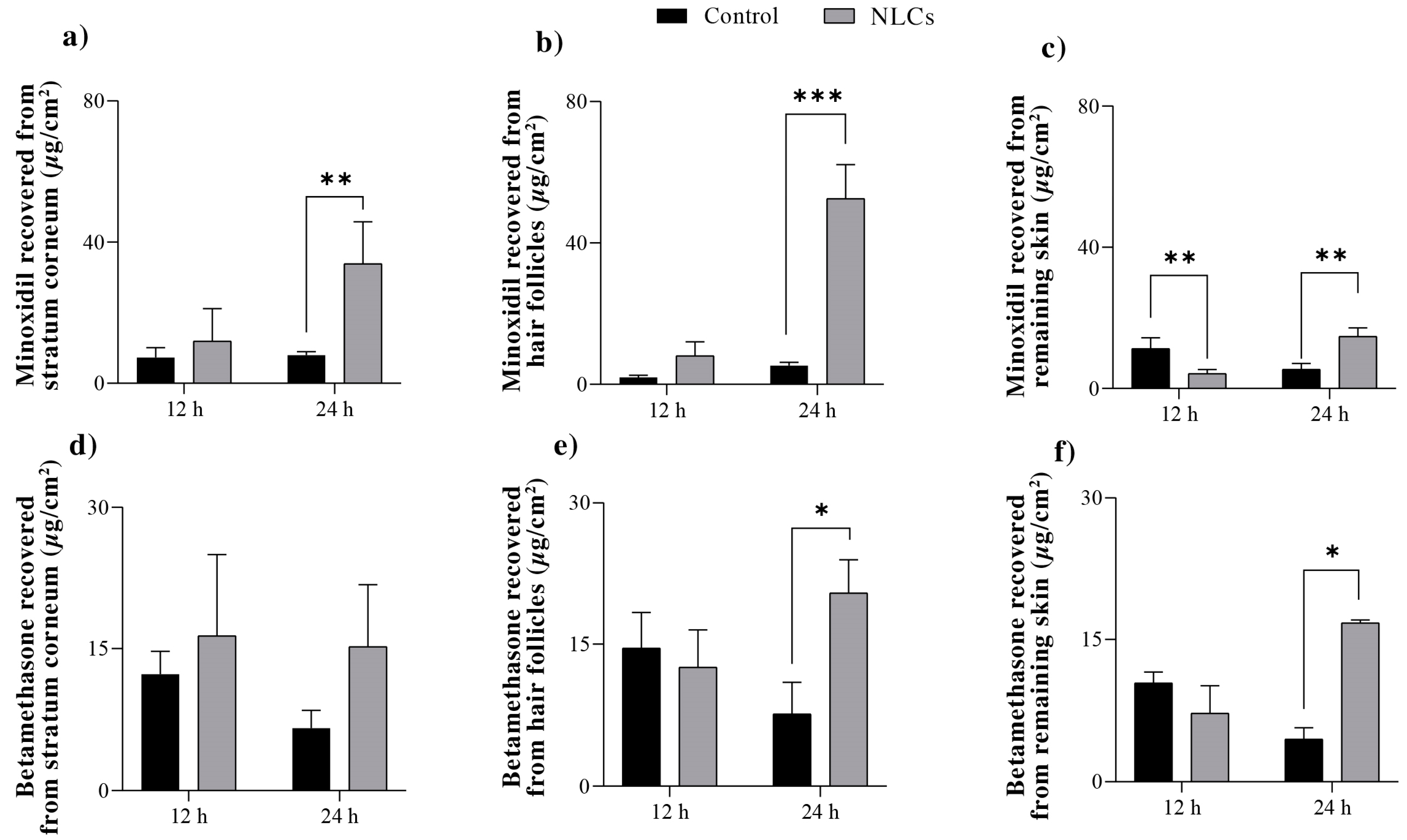
2. Results and Discussion
2.1. Development and Characterization of the Nanoparticles
2.2. In Vitro Drug Release
2.3. Skin Permeation Studies
3. Material and Methods
3.1. Material
3.2. Skin
3.3. Development of the PNPs
3.4. Development of the NLCs
3.5. Characterization of the Nanoparticles
3.5.1. Hydrodynamic Diameter and Zeta Potential
3.5.2. Entrapment Efficiency
3.5.3. Thermal Analyses
3.6. In Vitro Drug Release
3.7. Skin Permeation Studies
3.8. Minoxidil and Betamethasone Quantification
3.9. Data Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Strazzulla, L.C.; Wang, E.H.C.; Avila, L.; Lo Sicco, K.; Brinster, N.; Christiano, A.M.; Shapiro, J. Alopecia areata: Disease characteristics, clinical evaluation, and new perspectives on pathogenesis. J. Am. Acad. Dermatol. 2018, 78, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.H.; Gwillim, E.; Patel, K.R.; Hua, T.; Rastogi, S.; Ibler, E.; Silverberg, J.I. Epidemiology of alopecia areata, ophiasis, totalis, and universalis: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2020, 82, 675–682. [Google Scholar] [CrossRef] [PubMed]
- Cranwell, W.C.; Lai, V.W.; Photiou, L.; Meah, N.; Wall, D.; Rathnayake, D.; Joseph, S.; Chitreddy, V.; Gunatheesan, S.; Sindhu, K.; et al. Treatment of alopecia areata: An Australian expert consensus statement. Australas. J. Dermatol. 2019, 60, 163–170. [Google Scholar] [CrossRef]
- Freire, P.C.B.; Riera, R.; Martimbianco, A.L.C.; Petri, V.; Atallah, A.N. Minoxidil for patchy alopecia areata: Systematic review and meta-analysis. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 1792–1799. [Google Scholar] [CrossRef] [PubMed]
- Kiszewski, A.E.; Bevilaqua, M.; De Abreu, L.B. Mesalazine in the Treatment of Extensive Alopecia Areata: A New Therapeutic Option? Int. J. Trichol. 2018, 10, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, C.O.; Tolentino, S.; Gratieri, T.; Cunha-filho, M.S.S.; Lopes, R.F.V.; Gelfuso, G.M. Topical treatment for scarring and non-scarring alopecia: An overview of the current evidence. Clin. Cosmet. Investig. Dermatol. 2021, 14, 485–499. [Google Scholar] [CrossRef] [PubMed]
- Randolph, M.; Tosti, A. Oral minoxidil treatment for hair loss: A review of efficacy and safety. J. Am. Acad. Dermatol. 2021, 84, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Bleecker, E.R.; Menzies-Gow, A.N.; Price, D.B.; Bourdin, A.; Sweet, S.; Martin, A.L.; Alacqua, M.; Tran, T.N. Systematic Literature Review of Systemic Corticosteroid Use for Asthma Management. Am. J. Respir. Crit. Care Med. 2020, 201, 276–293. [Google Scholar] [CrossRef] [PubMed]
- Baryakova, T.H.; Pogostin, B.H.; Langer, R. Overcoming barriers to patient adherence: The case for developing innovative drug delivery systems. Nat. Rev. Drug Discov. 2023, 22, 87–409. [Google Scholar] [CrossRef]
- Matos, B.N.; Reis, T.A.; Gratieri, T.; Gelfuso, G.M. Chitosan nanoparticles for targeting and sustaining minoxidil sulphate delivery to hair follicles. Int. J. Biol. Macromol. 2015, 75, 225–229. [Google Scholar] [CrossRef]
- Patzelt, A.; Richter, H.; Knorr, F.; Schäfer, U.; Lehr, C.M.; Dähne, L.; Sterry, W.; Lademann, J. Selective follicular targeting by modification of the particle sizes. J. Control Release 2011, 150, 45–48. [Google Scholar] [CrossRef]
- Ushirobira, C.Y.; Afiune, L.A.F.; Pereira, M.N.; Cunha-Filho, M.; Gelfuso, G.M.; Gratieri, T. Dutasteride nanocapsules for hair follicle targeting: Effect of chitosan-coating and physical stimulus. Int. J. Biol. Macromol. 2020, 151, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-Nunes, R.; Cunha-Filho, M.; Gratieri, T.; Gelfuso, G.M. Follicular-targeted delivery of spironolactone provided by polymeric nanoparticles. Colloids Surf. B 2021, 208, 112101. [Google Scholar] [CrossRef] [PubMed]
- Pereira, M.N.; Tolentino, S.; Pires, F.Q.; Anjos, J.L.; Alonso, A.; Gratieri, T.; Cunha-Filho, M.S.S.; Gelfuso, G.M. Nanostructured lipid carriers for hair follicle-targeted delivery of clindamycin and rifampicin to hidradenitis suppurativa treatment. Colloids Surf. B 2021, 197, 111448. [Google Scholar] [CrossRef] [PubMed]
- Tolentino, S.; Pereira, M.N.; Cunha-Filho, M.; Gratieri, T.; Gelfuso, G.M. Targeted clindamycin delivery to pilosebaceous units by chitosan or hyaluronic acid nanoparticles for improved topical treatment of acne vulgaris. Carbohydr. Polym. 2021, 253, 117295. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, P.M.; Alencar-Silva, T.; Pires, F.Q.; Cunha-Filho, M.; Gratieri, T.; Carvalho, J.L.; Gelfuso, G.M. Nanostructured lipid carriers loaded with an association of minoxidil and latanoprost for targeted topical therapy of alopecia. Eur. J. Pharm. Biopharm. 2022, 172, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, T.; Kubota, T.; Choi, T.; Takahashi, M.; Ayano, E.; Kanazawa, H.; Higaki, M. Polymeric nanoparticles encapsulating betamethasone phosphate with different release profiles and stealthiness. Int. J. Pharm. 2009, 375, 148–154. [Google Scholar] [CrossRef]
- Shim, J.; Seok Kang, H.; Park, W.S.; Han, S.H.; Kim, J.; Chang, I.S. Transdermal delivery of mixnoxidil with block copolymer nanoparticles. JCR 2004, 97, 477–484. [Google Scholar] [CrossRef]
- Santos, A.C.; Pereira-Silva, M.; Guerra, C.; Costa, D.; Peixoto, D.; Pereira, I.; Pita, I.; Ribeiro, A.J.; Veiga, F. Topical Minoxidil-Loaded Nanotechnology Strategies for Alopecia. Cosmetics 2020, 7, 21. [Google Scholar] [CrossRef]
- Silva, C.O.; Rijo, P.; Molpeceres, J.; Figueiredo, I.V.; Ascensão, L.; Fernandes, A.S.; Roberto, A.; Reis, C.P. Polymeric nanoparticles modified with fatty acids encapsulating betamethasone for anti-inflammatory treatment. Int. J. Pharm. 2015, 493, 271–284. [Google Scholar] [CrossRef]
- Ghasemiyeh, P.; Mohammadi-Samani, S. Solid lipid nanoparticles and nanostructured lipid carriers as novel drug delivery systems: Applications, advantages and disadvantages. Res. Pharm. Sci. 2018, 13, 288–303. [Google Scholar] [CrossRef] [PubMed]
- Ajiboye, A.L.; Trivedi, V.; Mitchell, J.C. Preparation of polycaprolactone nanoparticles via supercritical carbon dioxide extraction of emulsions. Drug Deliv. Transl. Res. 2018, 8, 1790–1796. [Google Scholar] [CrossRef]
- Zanetti, M.; Mazon, L.R.; de Meneses, A.C.; Silva, L.L.; de Araújo, P.H.H.; Fiori, M.A.; de Oliveira, D. Encapsulation of geranyl cinnamate in polycaprolactone nanoparticles. Mater. Sci. Eng. C 2018, 97, 198–207. [Google Scholar] [CrossRef] [PubMed]
- Hanna, P.A.; Ghorab, M.M.; Gad, S. Development of Betamethasone Dipropionate-Loaded Nanostructured Lipid Carriers for Topical and Transdermal Delivery. Antiinflamm. Antiallergy Agents Med. Chem. 2019, 18, 26–44. [Google Scholar] [CrossRef] [PubMed]
- Mora-Huertas, C.E.; Fessi, H.; Elaissari, A. Influence of process and formulation parameters on the formation of submicron particles by solvent displacement and emulsification-diffusion methods: Critical comparison. Adv. Colloid Interface Sci. 2011, 163, 90–122. [Google Scholar] [CrossRef]
- Sakai, K.; Umemoto, N.; Matsuda, W.; Takamatsu, Y.; Matsumoto, M.; Sakai, H.; Abe, M. Oleic acid-based gemini surfactants with carboxylic acid headgroups. J. Oleo Sci. 2011, 60, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.C.; Yeh, M.K.; Cheng, S.N.; Chiang, C.H. The characteristics of betamethasone-loaded chitosan microparticles by spray-drying method. J. Microencapsul. 2003, 20, 459–472. [Google Scholar] [CrossRef]
- Kayes, J.B. Pharmaceutical suspensions: Micro electrophoretic properties. J. Pharm. Pharmacol. 1977, 29, 163–168. [Google Scholar] [CrossRef]
- Galindo-Pérez, M.J.; Quintanar-Guerrero, D.; Cornejo-Villegas, M.A.; Zambrano-Zaragoza, M.L. Optimization of the emulsification-diffusion method using ultrasound to prepare nanocapsules of different food-core oils. LWT Food Sci. Technol. 2018, 87, 333–341. [Google Scholar] [CrossRef]
- Hansch, C.; Leo, A.; Hoekman, D. Exploring QSAR: Hydrophobic, Electronic, Steric Constants; ACS: Washington, DC, USA, 1995. [Google Scholar]
- Li, W.; Zhang, X.; Liu, R.; Xu, S.; Xu, S.; Lan, Y.; Fu, Y.; Zhang, Y.; Feng, Y.; Cao, W. Thermal decomposition, flame propagation, and combustion reactions behaviours of stearic acid by experiments and molecular dynamic simulation. Chem. Eng. J. 2023, 461, 141906. [Google Scholar] [CrossRef]
- Speranza, V.; Sorrentino, A.; De Santis, F.; Pantani, R. Characterization of the polycaprolactone melt crystallization: Complementary optical microscopy, DSC, and AFM studies. Sci. World J. 2014, 214, 720157. [Google Scholar] [CrossRef]
- Tenorio-Alfonso, A.; Vázquez Ramos, E.; Martínez, I.; Ambrosi, M.; Raudino, M. Assessment of the structures contribution (crystalline and mesophases) and mechanical properties of polycaprolactone/pluronic blends. J. Mech. Behav. Biomed. Mater. 2023, 139, 105668. [Google Scholar] [CrossRef] [PubMed]
- Campos, E.V.R.; De Oliveira, J.L.; Da Silva, C.M.G.; Pascoli, M.; Pasquoto, T.; Lima, R. Polymeric and Solid Lipid Nanoparticles for Sustained Release of Carbendazim and Tebuconazole in Agricultural Applications. Sci. Rep. 2015, 5, 13809. [Google Scholar] [CrossRef] [PubMed]
- Gomes, M.J.; Martins, S.; Ferreira, D.; Segundo, M.A.; Reis, S. Lipid nanoparticles for topical and transdermal application for alopecia treatment: Development, physicochemical characterization, and in vitro release and penetration studies. Int. J. Nanomed. 2014, 9, 1231–1242. [Google Scholar] [CrossRef]
- Motawea, A.; Borg, T.; Abd El-Gawad, A.E.G.H. Topical phenytoin nanostructured lipid carriers: Design and development. Drug Dev. Ind. Pharm. Taylor Fr. 2018, 44, 144–157. [Google Scholar] [CrossRef]
- Oliveira, A.C.S.; Oliveira, P.M.; Cunha-Filho, M.; Gratieri, T.; Gelfuso, G.M. Latanoprost Loaded in Polymeric Nanocapsules for Effective Topical Treatment of Alopecia. AAPS PharmSciTech. 2020, 21, 305. [Google Scholar] [CrossRef]
- Kong, X.; Zhao, Y.; Quan, P.; Fang, L. Development of a topical ointment of betamethasone dipropionate loaded nanostructured lipid carrier. Asian J. Pharm. 2016, 11, 248–254. [Google Scholar] [CrossRef]
- Lohan, S.B.; Saeidpour, S.; Solik, A.; Schanzer, S.; Richter, H.; Dong, P.; Darvin, M.E.; Bodmeier, R.; Patzelt, A.; Zoubari, G.; et al. Investigation of the cutaneous penetration behavior of dexamethasone loaded to nano-sized lipid particles by EPR spectroscopy, and confocal Raman and laser scanning microscopy. Eur. J. Pharm. Biopharm. 2017, 116, 102–110. [Google Scholar] [CrossRef]
- Yu, Y.Q.; Yang, X.; Wu, X.F.; Fa, Y.B. Enhancing Permeation of Drug Molecules Across the Skin via Delivery in Nanocarriers: Novel Strategies for Effective Transdermal Applications. Front. Bioeng. Biotechnol. 2021, 29, 646554. [Google Scholar] [CrossRef]
- ICH. Harmonised Tripartite Guideline. Validation of Analytical Procedures: Text and Methodology Q2 (R1); 2023; pp. 1–13. Available online: https://www.ema.europa.eu/en/documents/scientific-guideline/ich-q-2-r1-validation-analytical-procedures-text-methodology-step-5_en.pdf (accessed on 19 July 2023).
- Badri, W.; Miladi, K.; Robin, S.; Viennet, C.; Nazari, Q.A.; Agusti, G.; Fessi, H.; Elaissari, A. Polycaprolactone Based Nanoparticles Loaded with Indomethacin for Anti-Inflammatory Therapy: From Preparation to Ex Vivo Study. Pharm. Res. 2017, 34, 1773–1783. [Google Scholar] [CrossRef]
- Bitter, H.; Lackner, S. Fast and easy quantification of semi-crystalline microplastics in exemplary environmental matrices by differential scanning calorimetry (DSC). J. Chem. Eng. 2021, 423, 129941. [Google Scholar] [CrossRef]
- Tsioptsias, C. On the latent limit of detection of thermogravimetric analysis. Measurement 2022, 204, 112136. [Google Scholar] [CrossRef]

| Nanoparticles | Hydrodynamic Diameter (nm) | PdI | Zeta Potential (mV) |
|---|---|---|---|
| Blank-PNPs | 270.7 ± 16.8 | 0.04 ± 0.04 | −20.7 ± 0.5 |
| PNPs | 413.9 ± 9.6 | 0.18 ± 0.01 | −32.1 ± 2.9 |
| Blank-NLCs | 272.0 ± 3.2 | 0.23 ± 0.04 | −21.3 ± 0.4 |
| NLCs | 566.7 ± 30.1 | 0.23 ± 0.20 | −37.9 ± 0.1 |
| Drug | Time (h) | Formulations | ||
|---|---|---|---|---|
| Control | PNPs | NLCs | ||
| Minoxidil | 12 | 0.18 | 0.32 | 0.44 |
| 24 | 0.28 | 0.51 | 0.52 | |
| Betamethasone | 12 | 0.19 | 0.32 | 0.37 |
| 24 | 0.43 | 0.49 | 0.74 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matos, B.N.; Lima, A.L.; Cardoso, C.O.; Cunha-Filho, M.; Gratieri, T.; Gelfuso, G.M. Follicle-Targeted Delivery of Betamethasone and Minoxidil Co-Entrapped in Polymeric and Lipid Nanoparticles for Topical Alopecia Areata Treatment. Pharmaceuticals 2023, 16, 1322. https://doi.org/10.3390/ph16091322
Matos BN, Lima AL, Cardoso CO, Cunha-Filho M, Gratieri T, Gelfuso GM. Follicle-Targeted Delivery of Betamethasone and Minoxidil Co-Entrapped in Polymeric and Lipid Nanoparticles for Topical Alopecia Areata Treatment. Pharmaceuticals. 2023; 16(9):1322. https://doi.org/10.3390/ph16091322
Chicago/Turabian StyleMatos, Breno N., Ana Luiza Lima, Camila O. Cardoso, Marcilio Cunha-Filho, Tais Gratieri, and Guilherme M. Gelfuso. 2023. "Follicle-Targeted Delivery of Betamethasone and Minoxidil Co-Entrapped in Polymeric and Lipid Nanoparticles for Topical Alopecia Areata Treatment" Pharmaceuticals 16, no. 9: 1322. https://doi.org/10.3390/ph16091322
APA StyleMatos, B. N., Lima, A. L., Cardoso, C. O., Cunha-Filho, M., Gratieri, T., & Gelfuso, G. M. (2023). Follicle-Targeted Delivery of Betamethasone and Minoxidil Co-Entrapped in Polymeric and Lipid Nanoparticles for Topical Alopecia Areata Treatment. Pharmaceuticals, 16(9), 1322. https://doi.org/10.3390/ph16091322









