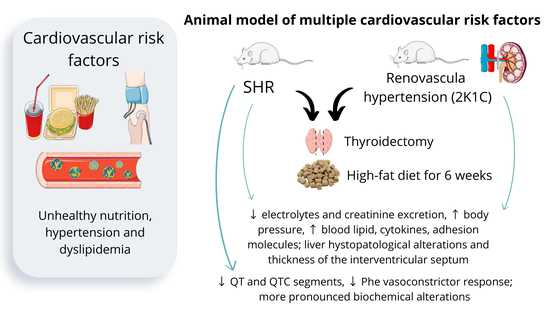
A New Approach for the Development of Multiple Cardiovascular Risk Factors in Two Rat Models of Hypertension
Abstract
:1. Introduction
2. Results
2.1. Behavioral Pattern and Body Weight Gain
2.2. Renal Function
2.3. Electrocardiography
2.4. Blood Pressure and Heart Rate
2.5. Mesenteric Vascular Bed Reactivity
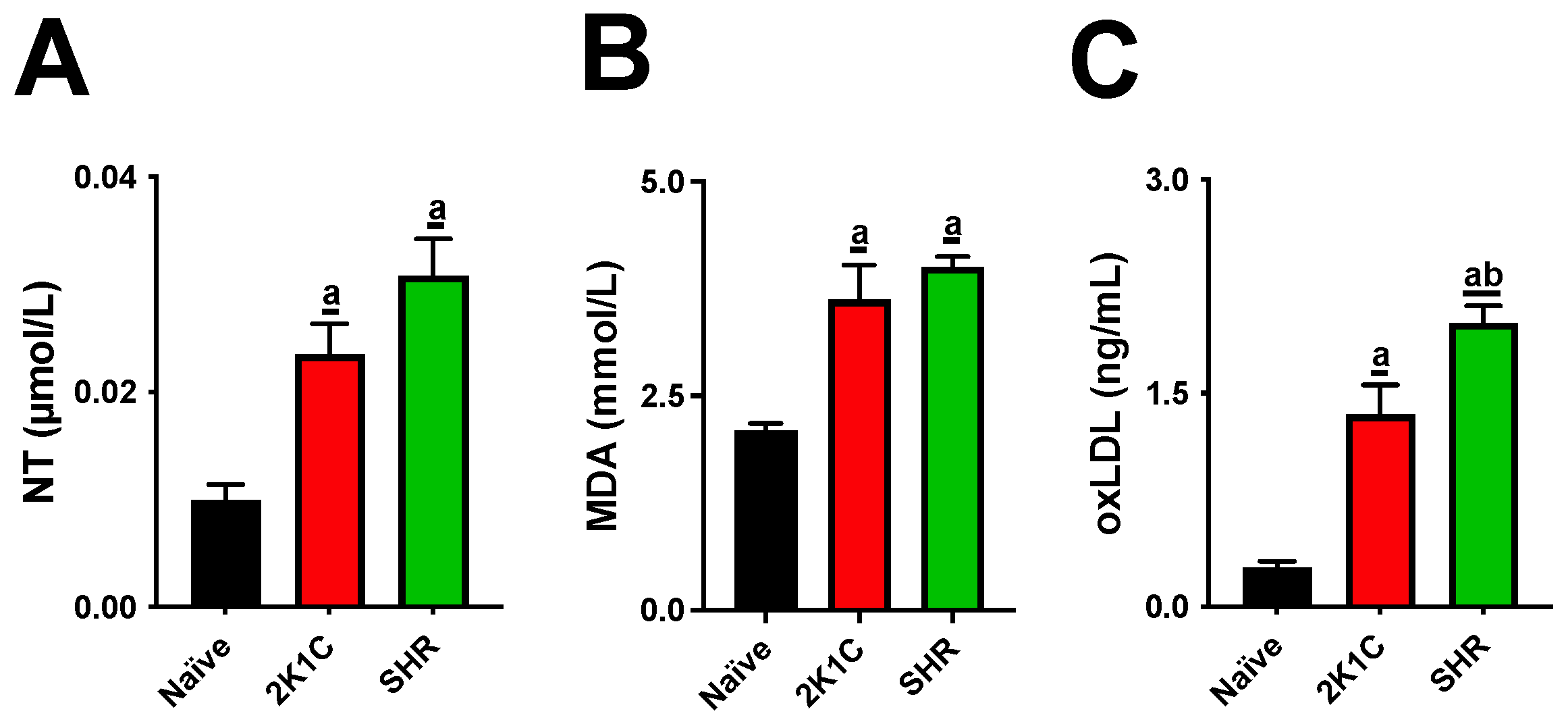
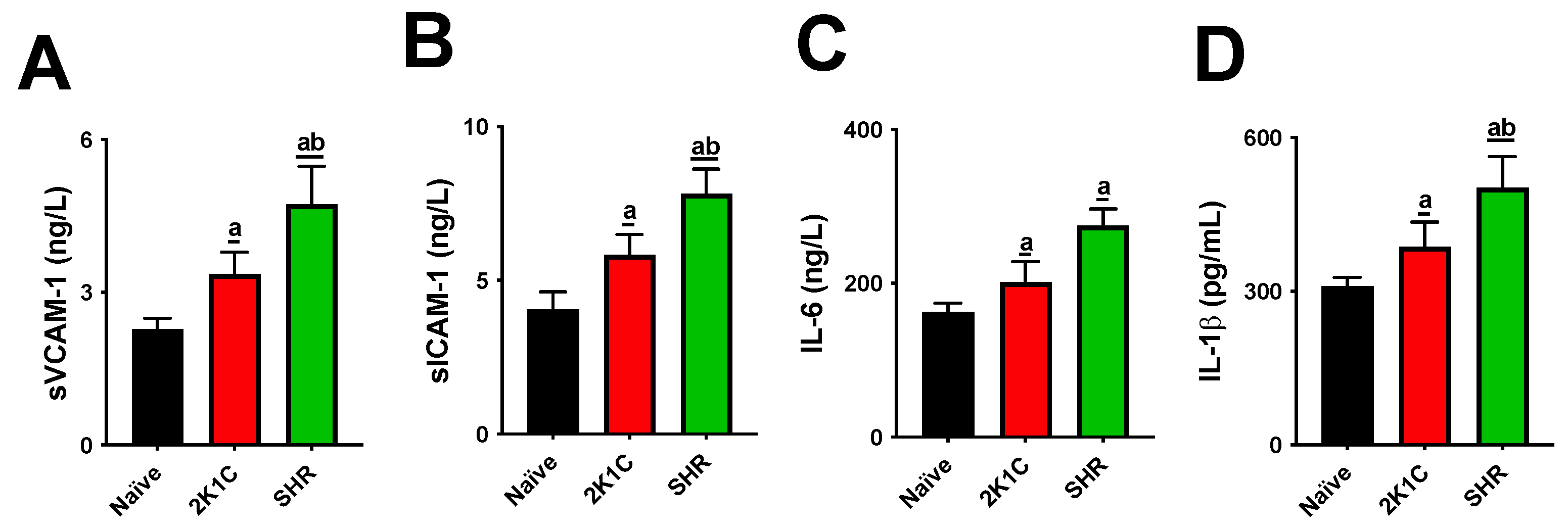
2.6. Blood Analyses
2.7. Relative Organ Weight
2.8. Histopathology and Morphometry
3. Discussion
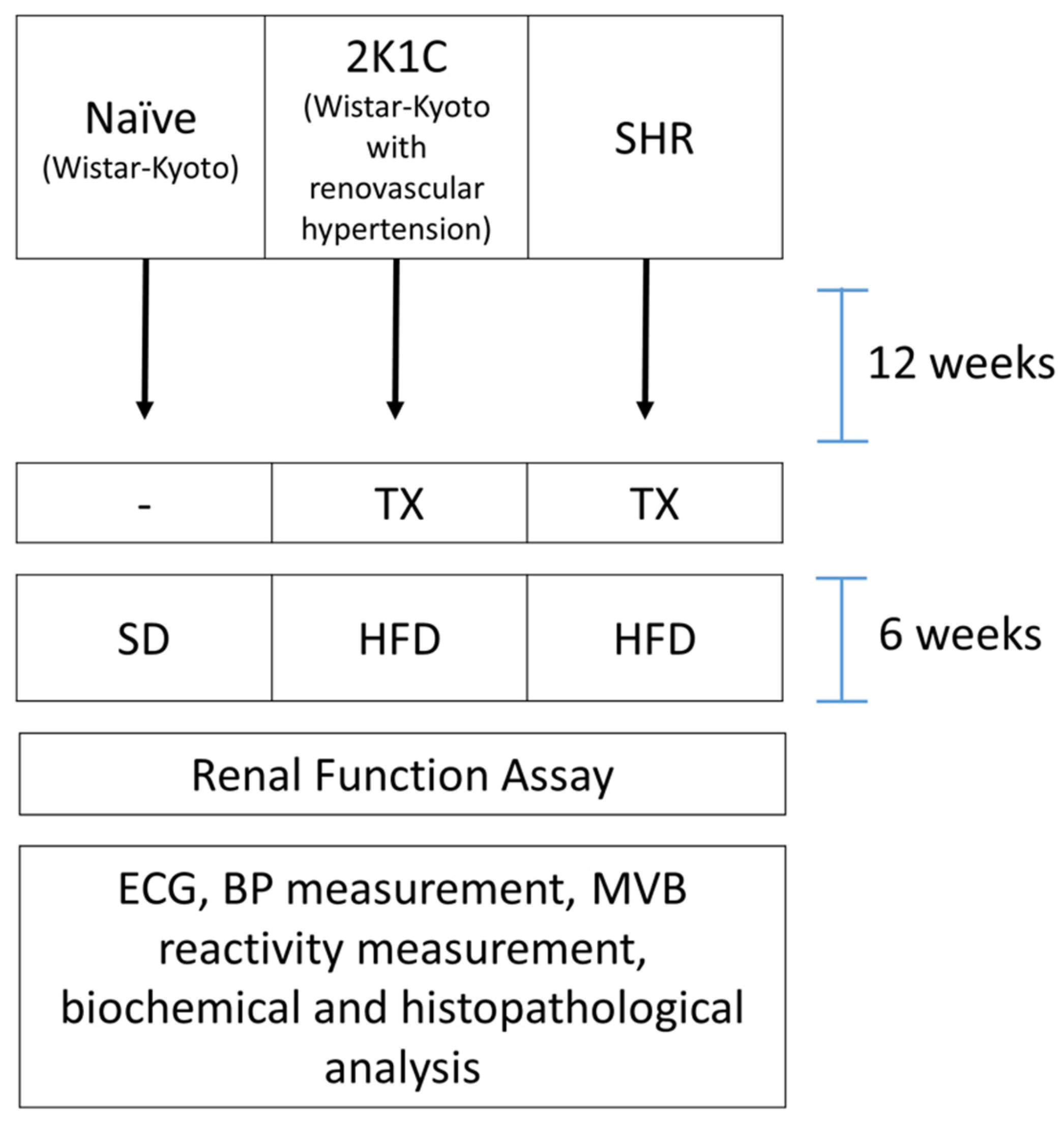
4. Materials and Methods
4.1. Drugs
4.2. Animals and Experimental Design
4.3. Experimental Procedures
4.3.1. Induction of Renovascular Hypertension
4.3.2. Thyroidectomy
4.3.3. High-Fat Diet
4.3.4. Renal Function Assay
4.3.5. Electrocardiography
4.3.6. Blood Pressure and Heart Rate Measurement
4.3.7. Mesenteric Vascular Reactivity
4.3.8. Blood Analyses
4.3.9. Relative Organ Weight
4.3.10. Histopathology and Morphometry
4.4. Statistical Analyses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef] [Green Version]
- Kaptoge, S.; Pennells, L.; De Bacquer, D.; Cooney, M.T.; Kavousi, M.; Stevens, G.; Riley, L.M.; Savin, S.; Khan, T.; Altay, S.; et al. World Health Organization cardiovascular disease risk charts: Revised models to estimate risk in 21 global regions. Lancet Glob. Health 2019, 7, e1332–e1345. [Google Scholar] [CrossRef] [Green Version]
- Bays, H.E.; Taub, P.R.; Epstein, E.; Michos, E.D.; Ferraro, R.A.; Bailey, A.L.; Kelli, H.M.; Ferdinand, K.C.; Echols, M.R.; Weintraub, H.; et al. Ten things to know about ten cardiovascular disease risk factors. Am. J. Prev. Cardiol. 2021, 5, 100149. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Oparil, S.; Acelajado, M.C.; Bakris, G.L.; Berlowitz, D.R.; Cífková, R.; Dominiczak, A.; Grassi, G.; Jordan, J.; Poulter, N.R.; Rodgers, A.; et al. Hypertension. Nat. Rev. Dis. Prim. 2018, 4, 18014. [Google Scholar] [CrossRef] [Green Version]
- Hurtubise, J.; McLellan, K.; Durr, K.; Onasanya, O.; Nwabuko, D.; Ndisang, J.F. The Different Facets of Dyslipidemia and Hypertension in Atherosclerosis. Curr. Atheroscler. Rep. 2016, 18, 82. [Google Scholar] [CrossRef]
- Sue, L.Y.; Leung, A.M. Levothyroxine for the Treatment of Subclinical Hypothyroidism and Cardiovascular Disease. Front. Endocrinol. 2020, 11, 591588. [Google Scholar] [CrossRef]
- Veseli, B.E.; Perrotta, P.; De Meyer, G.R.; Roth, L.; Van der Donckt, C.; Martinet, W.; De Meyer, G.R. Animal models of atherosclerosis. Eur. J. Pharmacol. 2017, 816, 3–13. [Google Scholar] [CrossRef]
- Zaragoza, C.; Gomez-Guerrero, C.; Martin-Ventura, J.L.; Blanco-Colio, L.M.; Lavin, B.; Mallavia, B.; Tarin, C.; Mas, S.; Ortiz, A.; Egido, J. Animal Models of Cardiovascular Diseases. J. Biomed. Biotechnol. 2011, 2011, 497841. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2021 Update: A Report From the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef]
- Zago, P.M.J.J.; da Silva, G.R.; Amaral, E.C.; Barboza, L.N.; Braga, F.D.A.; Lorençone, B.R.; Marques, A.A.M.; Moreno, K.G.T.; Leite, P.R.T.; Veiga, A.D.A.; et al. Multiple Risk Factors for Heart Disease: A Challenge to the Ethnopharmacological Use of Croton urucurana Baill. Evid.-Based Complement. Altern. Med. 2021, 2021, 6580458. [Google Scholar] [CrossRef] [PubMed]
- Goldblatt, H.; Lynch, J.; Hanzal, R.F.; Summerville, W.W. Studies on Experimental Hypertension. J. Exp. Med. 1934, 59, 347–379. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.G.; Lee, S.-H.; Kim, S.-Y.; Lee, A.; Moon, J.-Y.; Jeong, K.-H.; Lee, T.W.; Lim, S.J.; Sohn, I.S.; Ihm, C.-G. Sequential activation of the intrarenal renin-angiotensin system in the progression of hypertensive nephropathy in Goldblatt rats. Am. J. Physiol. Physiol. 2016, 311, F195–F206. [Google Scholar] [CrossRef] [Green Version]
- Alawi, L.F.; Dhakal, S.; Emberesh, S.E.; Sawant, H.; Hosawi, A.; Thanekar, U.; Grobe, N.; Elased, K.M. Effects of Angiotensin II Type 1A Receptor on ACE2, Neprilysin and KIM-1 in Two Kidney One Clip (2K1C) Model of Renovascular Hypertension. Front. Pharmacol. 2021, 11, 602985. [Google Scholar] [CrossRef] [PubMed]
- Gutsol, A.A.; Blanco, P.; Hale, T.M.; Thibodeau, J.-F.; Holterman, C.E.; Nasrallah, R.; Correa, J.W.N.; Afanasiev, S.A.; Touyz, R.M.; Kennedy, C.R.J.; et al. Comparative analysis of hypertensive nephrosclerosis in animal models of hypertension and its relevance to human pathology. Glomerulopathy. PLoS ONE 2022, 17, e0264136. [Google Scholar] [CrossRef] [PubMed]
- Lerman, L.O.; Kurtz, T.W.; Touyz, R.M.; Ellison, D.H.; Chade, A.R.; Crowley, S.D.; Mattson, D.L.; Mullins, J.J.; Osborn, J.; Eirin, A.; et al. Animal Models of Hypertension: A Scientific Statement From the American Heart Association. Hypertension 2019, 73, e87–e120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braun, M.C.; Herring, S.M.; Gokul, N.; Monita, M.; Bell, R.; Zhu, Y.; Gonzalez-Garay, M.L.; Wenderfer, S.E.; Doris, P.A. Hypertensive Renal Injury Is Associated With Gene Variation Affecting Immune Signaling. Circ. Cardiovasc. Genet. 2014, 7, 903–910. [Google Scholar] [CrossRef] [Green Version]
- Wirz, H.; Geigy, J.R. Kidney, Water and Electrolyte Metabolism. Annu. Rev. Physiol. 1961, 23, 577–606. [Google Scholar] [CrossRef]
- Weber, C.; Noels, H. Atherosclerosis: Current pathogenesis and therapeutic options. Nat. Med. 2011, 17, 1410–1422. [Google Scholar] [CrossRef]
- Sakakura, K.; Nakano, M.; Otsuka, F.; Ladich, E.; Kolodgie, F.D.; Virmani, R. Pathophysiology of Atherosclerosis Plaque Progression. Hear. Lung Circ. 2013, 22, 399–411. [Google Scholar] [CrossRef] [Green Version]
- Farzanegan, B.; Hosseinpoor, Z.; Baniasadi, S.; Seyyedi, S.R.; Rajabi, M. An Observational Study of QTc Prolongation in Critically Ill Patients: Identification of Incidence and Predictors. Indian J. Crit. Care Med. 2020, 24, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Coan, P.M.; Hummel, O.; Diaz, A.I.G.; Barrier, M.; Alfazema, N.; Norsworthy, P.; Pravenec, M.; Petretto, E.; Huebner, N.; Aitman, T.J. Genetic, physiological and comparative genomic studies of hypertension and insulin resistance in the spontaneously hypertensive rat. Dis. Model. Mech. 2017, 10, 297–306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romão, P.V.M.; Palozi, R.A.C.; Guarnier, L.P.; Silva, A.O.; Lorençone, B.R.; Nocchi, S.R.; Moura, C.C.D.F.S.; Lourenço, E.L.B.; Silva, D.B.; Junior, A.G. Cardioprotective effects of Plinia cauliflora (Mart.) Kausel in a rabbit model of doxorubicin-induced heart failure. J. Ethnopharmacol. 2019, 242, 112042. [Google Scholar] [CrossRef]
- Kasper, P.; Martin, A.; Lang, S.; Kütting, F.; Goeser, T.; Demir, M.; Steffen, H.-M. NAFLD and cardiovascular diseases: A clinical review. Clin. Res. Cardiol. 2020, 110, 921–937. [Google Scholar] [CrossRef] [PubMed]
- Tong, R.-C.; Qi, M.; Yang, Q.-M.; Li, P.-F.; Wang, D.-D.; Lan, J.-P.; Wang, Z.-T.; Yang, L. Extract of Plantago asiatica L. Seeds Ameliorates Hypertension in Spontaneously Hypertensive Rats by Inhibition of Angiotensin Converting Enzyme. Front. Pharmacol. 2019, 10, 403. [Google Scholar] [CrossRef]
- Guarnier, L.P.; Romão, P.V.M.; Palozi, R.A.C.; Silva, A.O.; Lorençone, B.R.; Marques, A.A.M.; dos Santos, A.C.; Souza, R.I.C.; Souza, K.D.; Lourenço, E.L.B.; et al. Development of a Predictive Model to Induce Atherogenesis and Hepato-Renal Impairment in Female Rats. Biomolecules 2019, 9, 664. [Google Scholar] [CrossRef] [Green Version]
- Ikawa, T.; Watanabe, Y.; Okuzaki, D.; Goto, N.; Okamura, N.; Yamanishi, K.; Higashino, T.; Yamanishi, H.; Okamura, H.; Higashino, H. A new approach to identifying hypertension-associated genes in the mesenteric artery of spontaneously hypertensive rats and stroke-prone spontaneously hypertensive rats. J. Hypertens. 2019, 37, 1644–1656. [Google Scholar] [CrossRef]
- Patel, M.; Mishra, V.; Pawar, V.; Ranvir, R.; Sundar, R.; Dabhi, R. Evaluation of acute physiological and molecular alterations in surgically developed hypothyroid Wistar rats. J. Pharmacol. Pharmacother. 2013, 4, 110–115. [Google Scholar] [CrossRef] [Green Version]
- Junior, A.G.; Gasparotto, F.M.; Lourenço, E.L.B.; Crestani, S.; Stefanello, M.E.A.; Salvador, M.J.; da Silva-Santos, J.E.; Marques, M.C.A.; Kassuya, C.A.L. Antihypertensive effects of isoquercitrin and extracts from Tropaeolum majus L.: Evidence for the inhibition of angiotensin converting enzyme. J. Ethnopharmacol. 2011, 134, 363–372. [Google Scholar] [CrossRef] [Green Version]
- McGregor, D.D. The effect of sympathetic nerve stimulation on vasoconstrictor responses in perfused mesenteric blood vessels of the rat. J. Physiol. 1965, 177, 21–30. [Google Scholar] [CrossRef]

| Parameter | Naive | 2K1C | SHR |
|---|---|---|---|
| Urinary volume (mL/100 g/24 h) | 30.83 ± 6.82 | 23.26 ± 4.67 | 26.63 ± 8.00 |
| pH | 8.01 ± 0.44 | 7.44 ± 0.25 a | 7.19 ± 0.20 a |
| Density | 1015 ± 7.81 | 1025 ± 4.00 a | 1023 ± 4.42 |
| Chloride (µmol/100 g/24 h) | 1033.12 ± 121.22 | 657.12 ± 85.21 a | 700.66 ± 34.32 a |
| Potassium (µmol/100 g/24 h) | 844.21 ± 85.11 | 534.23 ± 56.23 a | 602.11 ± 45.66 a |
| Sodium (µmol/100 g/24 h) | 1311.61 ± 178.11 | 855.21 ± 87.34 a | 867.14 ± 77.66 a |
| Urea (mg/100 g/24 h) | 105.51 ± 25.22 | 109.12 ± 22.31 | 111.22 ± 30.11 |
| Creatinine (mg/100 g/24 h) | 2.66 ± 0.36 | 1.33 ± 0.29 a | 1.55 ± 0.30 a |
| Parameter | Naive | 2K1C | SHR |
|---|---|---|---|
| P segment (ms) | 31.75 ± 6.20 | 32.38 ± 7.05 | 37.33 ± 6.30 |
| PR segment (ms) | 41.00 ± 5.75 | 38.75 ± 10.79 | 44.00 ± 8.54 |
| QRS segment (ms) | 45.50 ± 4.95 | 54.88 ± 9.09 | 54.33 ± 8.68 |
| QT segment (ms) | 98.75 ± 11.56 | 113.50 ± 12.68 | 145.40 ± 16.74 a |
| QTC segment (ms) | 165.40 ± 42.19 | 176.40 ± 24.80 | 245.40 ± 36.92 a |
| P wave (mV) | 0.04 ± 0.02 | 0.03 ± 0.01 | 0.05 ± 0.01 |
| Q wave (mV) | −0.01 ± 0.01 | −0.05 ± 0.09 | −0.02 ± 0.02 |
| R wave (mV) | 0.28 ± 0.05 | 0.25 ± 0.09 | 0.31 ± 0.05 |
| S wave (mV) | −0.001 ± 0.001 | −0.001 ± 0.001 | −0.001 ± 0.001 |
| Parameter | Naive | 2K1C | SHR |
|---|---|---|---|
| SBP (mm Hg) | 98.60 ± 24.27 | 164.10 ± 24.76 a | 144.80 ± 10.10 a |
| DBP (mm Hg) | 63.79 ± 3.61 | 100.95 ± 14.50 a | 99.39 ± 7.86 a |
| MAP (mm Hg) | 80.22 ± 16.05 | 121.56 ± 12.39 a | 115.79 ± 8.22 a |
| HR (bpm) | 246.00 ± 11.56 | 178.60 ± 20.42 a | 153.00 ± 21.88 a |
| Parameter | Naive | 2K1C | SHR |
|---|---|---|---|
| Phe (nmol) | |||
| 3 | 17.90 ± 7.92 | 8.96 ± 5.47 | 3.52 ± 1.93 a |
| 10 | 39.23 ± 8.07 | 24.90 ± 11.11 | 17.08 ± 7.49 a |
| 30 | 76.90 ± 12.13 | 57.38 ± 21.90 | 36.83 ± 9.40 a |
| 100 | 102.74 ± 21.98 | 94.66 ± 28.64 | 78.05 ± 31.29 |
| ACh (nmol) | |||
| 0.3 | −5.06 ± 1.19 | −3.70 ± 1.20 | −5.06 ± 1.72 |
| 1 | −5.93 ± 1.90 | −5.59 ± 2.05 | −7.71 ± 2.98 |
| 3 | −6.35 ± 2.05 | −4.96 ± 2.76 | −4.21 ± 1.97 |
| 10 | −6.04 ± 2.66 | −6.34 ± 2.18 | −7.60 ± 1.54 |
| SNP (nmol) | |||
| 0.03 | −6.18 ± 2.52 | −7.12 ± 2.18 | −8.70 ± 3.56 |
| 0.1 | −9.74 ± 3.39 | −7.62 ± 2.50 | −8.07 ± 4.33 |
| 0.3 | −14.50 ± 4.82 | −17.85 ± 3.13 | −15.58 ± 3.81 |
| 1 | −22.72 ± 8.00 | −19.44 ± 6.78 | −19.76 ± 6.79 |
| Parameter | Naive | 2K1C | SHR |
|---|---|---|---|
| AST (U/L) | 193.40 ± 62.51 | 205.00 ± 61.02 | 183.40 ± 49.51 |
| ALT (U/L) | 56.00 ± 12.46 | 92.67 ± 10.99 a | 73.57 ± 11.12 |
| Triglycerides (mg/dL) | 18.75 ± 6.65 | 492.7 ± 143.20 a | 551.20 ± 160.00 a |
| Total cholesterol (mg/dL) | 89.40 ± 17.17 | 127.20 ± 14.96 a | 175.20 ± 17.03 ab |
| HDL-C (mg/dL) | 31.00 ± 10.32 | 28.67 ± 15.10 | 22.14 ± 8.97 |
| LDL-C (mg/dL) | 66.65 ± 10.64 | 102.33 ± 15.34 a | 215.40 ± 7.07 ab |
| VLDL-C (mg/dL) | 3.20 ± 1.69 | 98.53 ± 28.64 a | 123.00 ± 8.03 a |
| Urea (mg/dL) | 27.75 ± 3.59 | 44.33 ± 7.39 a | 38.60 ± 6.91 a |
| Creatinine (mg/dL) | 0.70 ± 0.21 | 0.90 ± 0.12 | 0.58 ± 0.13 b |
| Parameter | Naive | 2K1C | SHR |
|---|---|---|---|
| Heart (%) | 0.23 ± 0.01 | 0.31 ± 0.02 a | 0.32 ± 0.02 a |
| Right kidney (%) | 0.30 ± 0.01 | 0.31 ± 0.06 | 0.32 ± 0.02 |
| Liver (%) | 2.78 ± 0.34 | 3.39 ± 0.16 a | 4.08 ± 0.30 a |
| Right ventricle (mm) | 0.78 ± 0.15 | 0.94 ± 0.14 a | 0.73 ± 0.10 |
| Left ventricle (mm) | 1.65 ± 0.20 | 1.76 ± 0.34 | 1.52 ± 0.27 |
| IV septum (mm) | 1.67 ± 0.35 | 2.12 ± 0.18 a | 2.07 ± 0.53 a |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moreno, K.G.T.; Marques, A.A.M.; da Silva, G.P.; Lourençone, B.R.; Fortini, C.S.; Leite, P.R.T.; dos Santos, A.C.; Souza, R.I.C.; da Siva, L.I.; Gasparotto Junior, A. A New Approach for the Development of Multiple Cardiovascular Risk Factors in Two Rat Models of Hypertension. Pharmaceuticals 2022, 15, 853. https://doi.org/10.3390/ph15070853
Moreno KGT, Marques AAM, da Silva GP, Lourençone BR, Fortini CS, Leite PRT, dos Santos AC, Souza RIC, da Siva LI, Gasparotto Junior A. A New Approach for the Development of Multiple Cardiovascular Risk Factors in Two Rat Models of Hypertension. Pharmaceuticals. 2022; 15(7):853. https://doi.org/10.3390/ph15070853
Chicago/Turabian StyleMoreno, Karyne Garcia Tafarelo, Aline Aparecida Macedo Marques, Gabriela Pereira da Silva, Bethânia Rosa Lourençone, Clara Soligo Fortini, Patrícia Regina Terço Leite, Ariany Carvalho dos Santos, Roosevelt Isaías Carvalho Souza, Leila Isabel da Siva, and Arquimedes Gasparotto Junior. 2022. "A New Approach for the Development of Multiple Cardiovascular Risk Factors in Two Rat Models of Hypertension" Pharmaceuticals 15, no. 7: 853. https://doi.org/10.3390/ph15070853
APA StyleMoreno, K. G. T., Marques, A. A. M., da Silva, G. P., Lourençone, B. R., Fortini, C. S., Leite, P. R. T., dos Santos, A. C., Souza, R. I. C., da Siva, L. I., & Gasparotto Junior, A. (2022). A New Approach for the Development of Multiple Cardiovascular Risk Factors in Two Rat Models of Hypertension. Pharmaceuticals, 15(7), 853. https://doi.org/10.3390/ph15070853