How Much Protoporphyrin IX Must Be Activated to Obtain Full Efficacy of Methyl Aminolevulinate Photodynamic Therapy? Implication for Treatment Modifications
Abstract
1. Introduction
2. Results
2.1. PpIX Formation
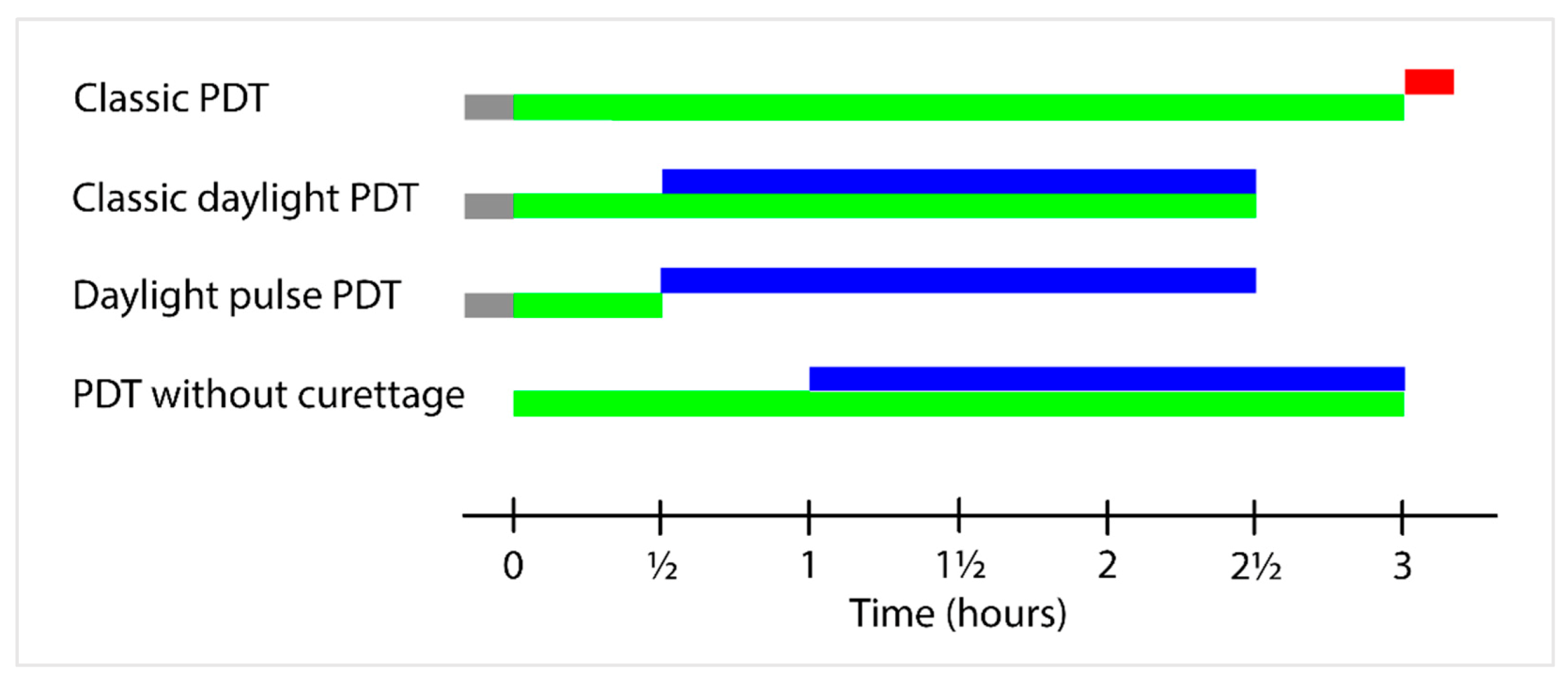
- (I)
- The amount of PpIX after 3 h in the +Cur3hourMAL group (see Methods) was normalized to 100 PpIX units, being the highest amount of PpIX measured in the study. One hundred PpIX units are the amount of PpIX available for photoactivation 3 h after MAL application before illumination with red light in classic PDT.
- (II)
- After 2.5 h, 85 PpIX units were formed in the +Cur3hourMAL group, representing the amount of PpIX available for photoactivation during classic daylight PDT.
- (III)
- After 2.5 h, 57 PpIX units were formed in the +Cur30MinMAL group, representing the amount of PpIX available for photoactivation during daylight pulse PDT.
- (IV)
- When no curettage is performed, 3 h after MAL application, 52 PpIX units were formed in the -Cur3hourMAL group, representing the amount of PpIX available for photoactivation during PDT without curettage.
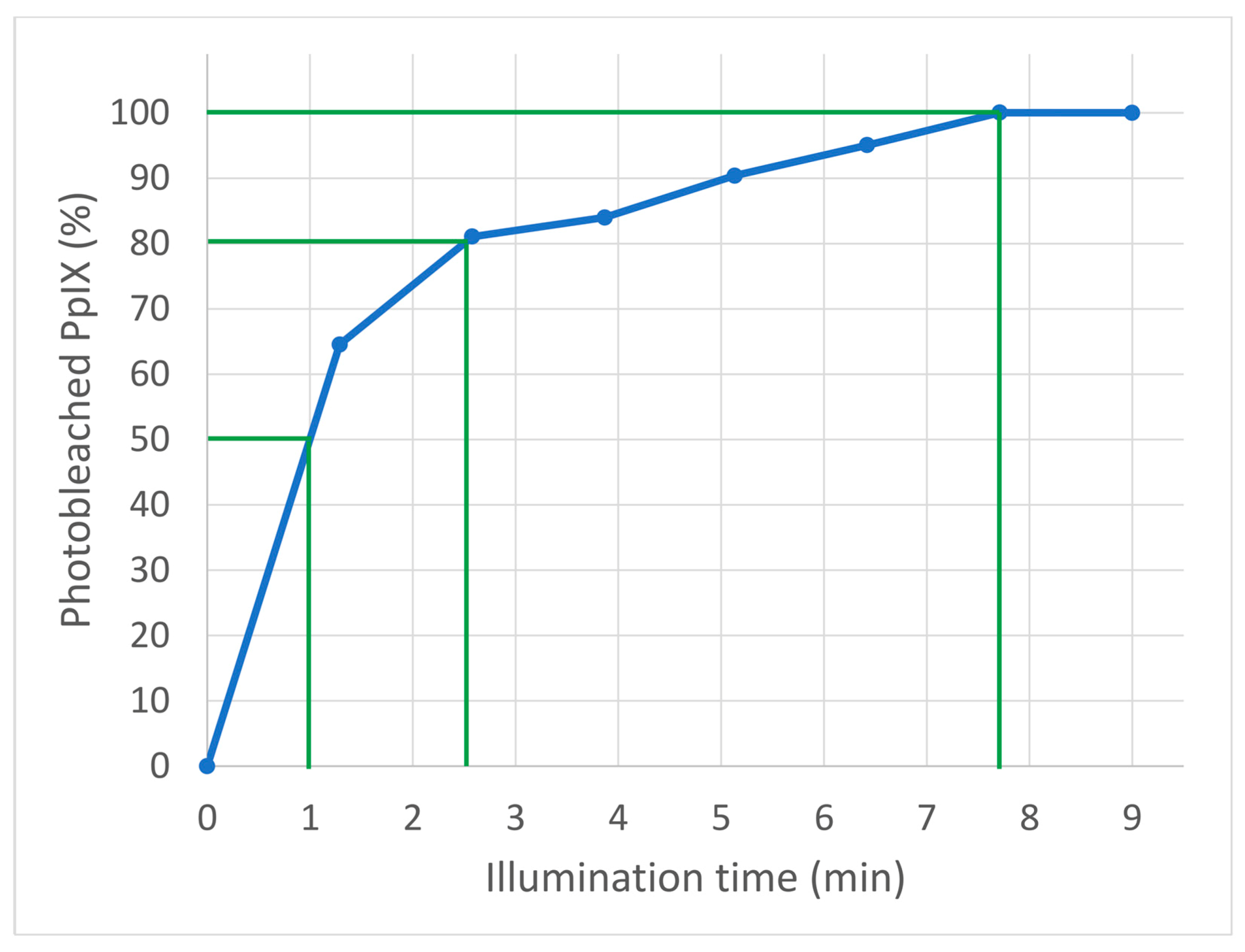
2.2. PpIX Photoactivation
3. Discussion
4. Materials and Methods
4.1. PpIX Measurements
4.2. PpIX Formation
4.3. PpIX Photoactivation
4.4. Statistics
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grapengiesser, S.; Gudmundsson, F.; Larkö, O.; Ericson, M.; Rosen, A.; Wennberg, A.M. Pain caused by photodynamic therapy of skin cancer. Clin. Exp. Dermatol. 2002, 27, 493–497. [Google Scholar] [CrossRef]
- Ang, J.M.; Riaz, I.B.; Kamal, M.U.; Paragh, G.; Zeitouni, N.C. Photodynamic therapy and pain: A systematic review. Photodiagnosis Photodyn. Ther. 2017, 19, 308–344. [Google Scholar] [CrossRef]
- Peng, Q.; Warloe, T.; Berg, K.; Moan, J.; Kongshaug, M.; Giercksky, K.E.; Nesland, J.M. 5-Aminolevulinic acid-based photodynamic therapy: Clinical research and future challenges. Cancer 1997, 79, 2282–2308. [Google Scholar] [CrossRef]
- Szeimiesa, R.M.; Karrera, S.; Radakovic-Fijanb, S.; Tanewb, A.; Calzavara-Pintonc, P.G.; Zanec, C.; Sidoroffd, A.; Hempele, M.; Ulrichf, J.; Proebstleg, T.; et al. Photodynamic therapy using topical methyl 5-aminolevulinate compared with cryotherapy for actinic keratosis: A prospective, randomized study. J. Am. Acad. Dermatol. 2002, 47, 258–262. [Google Scholar] [CrossRef]
- Lerche, C.M.; Heerfordt, I.M.; Heydenreich, J.; Wulf, H.C. Alternatives to Outdoor Daylight Illumination for Photodynamic Therapy—Use of Greenhouses and Artificial Light Sources. Int. J. Mol. Sci. 2016, 17, 309. [Google Scholar] [CrossRef] [PubMed]
- Wiegell, S.R.; Haedersdal, M.; Eriksen, P.; Wulf, H.C. Photodynamic therapy of actinic keratoses with 8% and 16% methyl aminolaevulinate and home-based daylight exposure: A double-blinded randomized clinical trial. Br. J. Dermatol. 2009, 160, 1308–1314. [Google Scholar] [CrossRef] [PubMed]
- Wiegell, S.R.; Petersen, B.; Wulf, H.C. Pulse photodynamic therapy reduces inflammation without compromising efficacy in the treatment of multiple mild actinic keratoses of the face and scalp: A randomized clinical trial. Br. J. Dermatol. 2016, 174, 979–984. [Google Scholar] [CrossRef] [PubMed]
- Wiegell, S.; Johansen, U.; Wulf, H. Pulse–Daylight–Photodynamic Therapy in Combination with Corticosteroid and Brimonidine Tartrate for Multiple Actinic Keratoses: A Randomized Clinical Trial. Acta Derm. Venereol. 2019, 99, 242–243. [Google Scholar] [CrossRef] [PubMed]
- Heerfordt, I.M.; Wulf, H.C. Daylight photodynamic therapy of actinic keratosis without curettage is as effective as with curettage: A randomized clinical trial. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 2058–2061. [Google Scholar] [CrossRef]
- Nissen, C.V.; Heerfordt, I.M.; Wiegell, S.R.; Mikkelsen, C.S.; Wulf, H.C. Increased protoporphyrin IX accumulation does not improve the effect of photodynamic therapy for actinic keratosis: A randomized controlled trial. Br. J. Dermatol. 2017, 176, 1241–1246. [Google Scholar] [CrossRef]
- Wiegell, S.R.; Heydenreich, J.; Fabricius, S.; Wulf, H.C. Continuous ultra-low-intensity artificial daylight is not as effective as red LED light in photodynamic therapy of multiple actinic keratoses. Photodermatol. Photoimmunol. Photomed. 2011, 27, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Guarino, M.; Fonda Pascual, P.; Lizuain Gomez, P.; Harto Castaño, A.; Jaén Olasolo, P. Split-face study comparing conventional MAL photodynamic therapy in multiple actinic keratosis with complete time vs. half-time red light LED conventional illumination. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 1529–1534. [Google Scholar] [CrossRef] [PubMed]
- Togsverd-Bo, K.; Haak, C.; Thaysen-Petersen, D.; Wulf, H.; Anderson, R.; Haedesdal, M. Intensified photodynamic therapy of actinic keratoses with fractional CO2 laser: A randomized clinical trial. Br. J. Dermatol. 2012, 166, 1262–1269. [Google Scholar] [CrossRef] [PubMed]
- Wiegell, S.R.; Fabricius, S.; Stender, I.M.; Berne, B.; Kroon, S.; Andersen, B.L.; Mørk, C.; Sandberg, C.; Jemec, G.B.E.; Mogensen, M.; et al. A randomized, multicentre study of directed daylight exposure times of 1½ vs. 2½ h in daylight-mediated photodynamic therapy with methyl aminolaevulinate in patients with multiple thin actinic keratoses of the face and scalp. Br. J. Dermatol. 2011, 164, 1083–1090. [Google Scholar] [CrossRef]
- Wiegell, S.R.; Haedersdal, M.; Philipsen, P.A.; Eriksen, P.; Enk, C.D.; Wulf, H.C. Continuous activation of PpIX by daylight is as effective as and less painful than conventional photodynamic therapy for actinic keratoses; a randomized, controlled, single-blinded study. Br. J. Dermatol. 2008, 158, 740–746. [Google Scholar] [CrossRef] [PubMed]
- Braathen, L.R.; Paredes, B.E.; Saksela, O.; Fritsch, C.; Gardlo, K.; Morken, T.; Frølich, K.W.; Warloe, T.; Solér, A.M.; Ros, A.M. Short incubation with methyl aminolevulinate for photodynamic therapy of actinic keratoses. J. Eur. Acad. Dermatol. Venereol. 2009, 23, 550–555. [Google Scholar] [CrossRef]
- von Dobbeler, C.; Schmitz, L.; Dicke, K.; Szeimies, R.M.; Dirschka, T. PDT with PPIX absorption peaks adjusted wavelengths: Safety and efficacy of a new irradiation procedure for actinic keratoses on the head. Photodiagnosis Photodyn. Ther. 2019, 27, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Nissen, C.V.; Philipsen, P.A.; Wulf, H.C. Protoporphyrin IX formation after topical application of methyl aminolaevulinate and BF-200 aminolaevulinic acid declines with age. Br. J. Dermatol. 2015, 173, 760–766. [Google Scholar] [CrossRef]
- Ericson, M.B.; Sandberg, C.; Stenquist, B.; Gudmundson, F.; Karlsson, M.; Ros, A.M.; Rosén, A.; Larkö, O.; Wennberg, A.M.; Rosdahl, I. Photodynamic therapy of actinic keratosis at varying fluence rates: Assessment of photobleaching, pain and primary clinical outcome. Br. J. Dermatol. 2004, 151, 1204–1212. [Google Scholar] [CrossRef]
- Bjerring, P.; Christiansen, K.; Troilius, A.; Bekhor, P.; de Leeuw, J. Skin fluorescence controlled photodynamic photorejuvenation (wrinkle reduction). Lasers Surg. Med. 2009, 41, 327–336. [Google Scholar] [CrossRef]
- Haak, C.S.; Christiansen, K.; Erlendsson, A.M.; Taudorf, E.H.; Thaysen-Petersen, D.; Wulf, H.C.; Haedersdal, M. Ablative fractional laser enhances MAL-induced PpIX accumulation: Impact of laser channel density, incubation time and drug concentration. J. Photochem. Photobiol. B Biol. 2016, 159, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Togsverd-Bo, K.; Idorn, L.W.; Philipsen, P.A.; Wulf, H.C.; Hædersdal, M. Protoporphyrin IX formation and photobleaching in different layers of normal human skin: Methyl- and hexylaminolevulinate and different light sources. Exp. Dermatol. 2012, 21, 745–750. [Google Scholar] [CrossRef] [PubMed]
- Heerfordt, I.M.; Bieliauskiene, G.; Wulf, H.C. Protoporphyrin IX formation after application of methyl aminolevulinate on the face and scalp with and without prior curettage. Photodiagnosis Photodyn. Ther. 2018, 22, 155–157. [Google Scholar] [CrossRef] [PubMed]
- Wulf, H.C. Daylight PDT acts by continuous activation of PpIX. Photodiagnosis Photodyn. Ther. 2019, 27, A1–A2. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wulf, H.C.; Heerfordt, I.M.; Philipsen, P.A. How Much Protoporphyrin IX Must Be Activated to Obtain Full Efficacy of Methyl Aminolevulinate Photodynamic Therapy? Implication for Treatment Modifications. Pharmaceuticals 2021, 14, 333. https://doi.org/10.3390/ph14040333
Wulf HC, Heerfordt IM, Philipsen PA. How Much Protoporphyrin IX Must Be Activated to Obtain Full Efficacy of Methyl Aminolevulinate Photodynamic Therapy? Implication for Treatment Modifications. Pharmaceuticals. 2021; 14(4):333. https://doi.org/10.3390/ph14040333
Chicago/Turabian StyleWulf, Hans Christian, Ida M. Heerfordt, and Peter Alshede Philipsen. 2021. "How Much Protoporphyrin IX Must Be Activated to Obtain Full Efficacy of Methyl Aminolevulinate Photodynamic Therapy? Implication for Treatment Modifications" Pharmaceuticals 14, no. 4: 333. https://doi.org/10.3390/ph14040333
APA StyleWulf, H. C., Heerfordt, I. M., & Philipsen, P. A. (2021). How Much Protoporphyrin IX Must Be Activated to Obtain Full Efficacy of Methyl Aminolevulinate Photodynamic Therapy? Implication for Treatment Modifications. Pharmaceuticals, 14(4), 333. https://doi.org/10.3390/ph14040333






