Inter-Girdle Coordination as a Predictive Measure of Low Back Pain
Abstract
Highlights
- Inter-girdle coordination is a relevant determinant of LBP potential risk.
- Inter-girdle coordination allows trunk stability during gait.
- Range of motion in the transverse plane is relevant in functional prevention of LBP.
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Data Processing
2.4. Statistical Analysis
3. Results
3.1. Individual Parameters
3.2. Gait Parameters and Normalized Joint Angles
3.3. Inter-Girdle Coordination
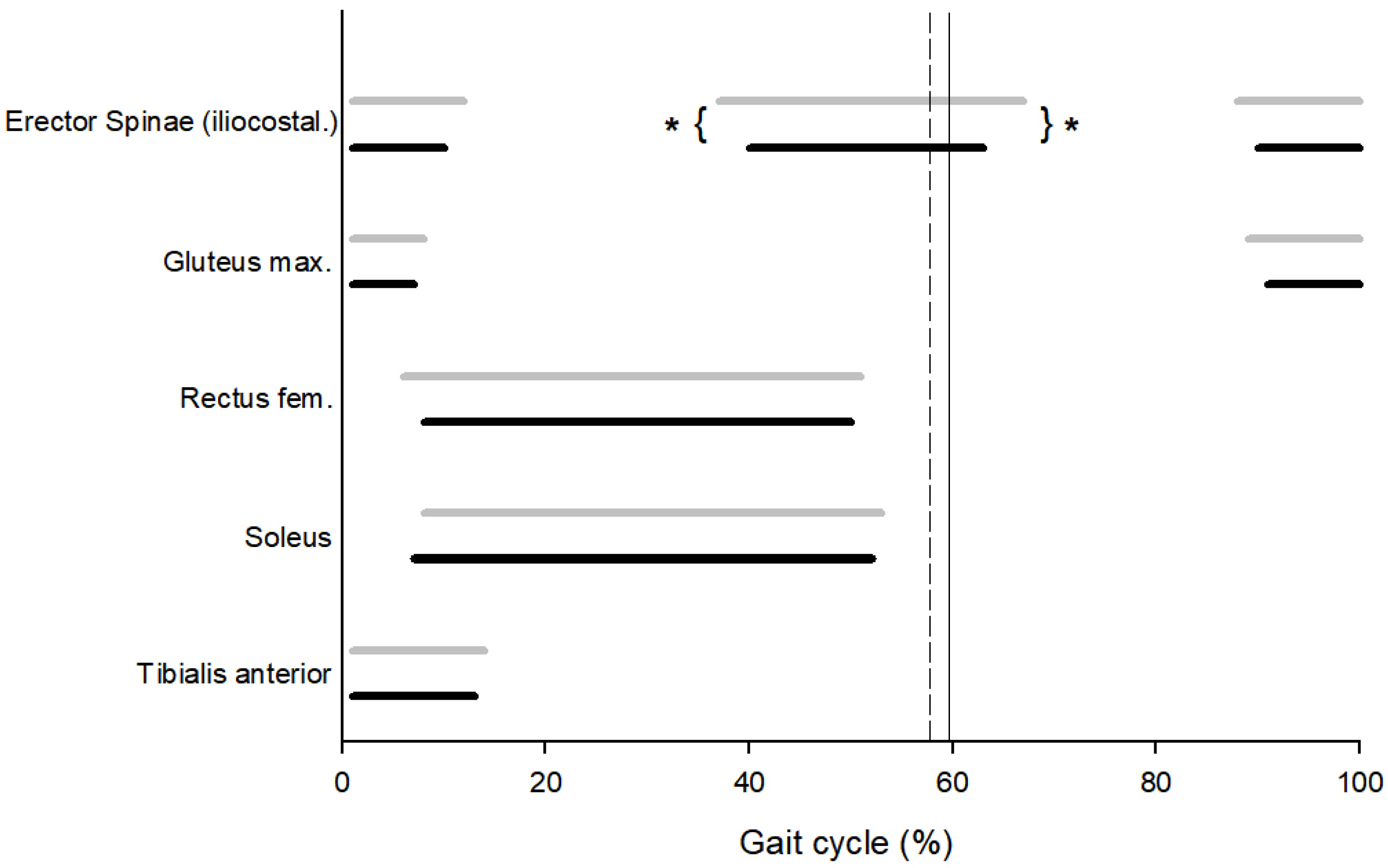
3.4. Muscular Pattern
3.5. k.Means Clustering Analysis
4. Discussion
4.1. Main Findings
4.2. Comparison with the Literature
4.3. Clinical Implications
4.4. Study Limitations and Future Directions
4.5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef]
- Brennan, G.P.; Fritz, J.M.; Hunter, S.J.; Thackeray, A.; Delitto, A.; Erhard, R.E. Identifying Subgroups of Patients with Acute/Subacute “Nonspecific” Low Back Pain: Results of a Randomized Clinical Trial. Spine 2006, 31, 623–631. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What LBP is and why we need to pay attention. Lancet Neurol. 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Steffens, D.; Maher, C.G.; Pereira, L.S.; Stevens, M.L.; Oliveira, V.C.; Chapple, M.; Teixeira-Salmela, L.F.; Hancock, M.J. Prevention of low back pain: A systematic review and meta-analysis. JAMA Intern. Med. 2016, 176, 199–208. [Google Scholar] [CrossRef]
- Shiri, R.; Coggon, D.; Falah-Hassani, K. Exercise for the Prevention of Low Back Pain: Systematic Review and Meta-Analysis of Controlled Trials. Am. J. Epidemiol. 2018, 187, 1093–1101. [Google Scholar] [CrossRef]
- Lemmers, G.P.G.; Melis, R.J.F.; Hak, R.; de Snoo, E.K.; Pagen, S.; Westert, G.P.; Staal, J.B.; van der Wees, P.J. The association of physical activity and sedentary behaviour with low back pain disability trajectories: A prospective cohort study. Musculoskelet. Sci. Pract. 2024, 72, 102954. [Google Scholar] [CrossRef] [PubMed]
- Hubley-Kozey, C.L.; Vezina, M.J. Muscle activation during exercises to improve trunk stability in men with low back pain. Arch. Phys. Med. Rehabil. 2002, 83, 1100–1108. [Google Scholar] [CrossRef] [PubMed]
- Sung, P.S.; Lee, D. Postural control and trunk stability on sway parameters in adults with and without chronic low back pain. Eur. Spine J. 2024, 33, 1455–1464. [Google Scholar] [CrossRef]
- Stuge, B. Evidence of stabilizing exercises for low back- and pelvic girdle pain—A critical review. Braz. J. Phys. Ther. 2018, 23, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Falah-Hassani, K. Does leisure time physical activity protect against low back pain? Systematic review and meta-analysis of 36 prospective cohort studies. Br. J. Sports Med. 2017, 51, 1410–1418. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, H.; Mackey, M.; Stamatakis, E.; Zadro, J.R.; Shirley, D. The association between physical activity and low back pain: A systematic review and metaanalysis of observational studies. Sci. Rep. 2019, 9, 8244. [Google Scholar] [CrossRef]
- Lamoth, C.J.C.; Meijer, O.G.; Wuisman, P.I.J.M.; van Dieën, J.H.; Levin, M.F.; Beek, P.J. Pelvis-thorax coordination in the transverse plane during walking in persons with nonspecific low back pain. Spine 2002, 27, E92–E99. [Google Scholar] [CrossRef]
- Huang, Y.; Meijer, O.G.; Lin, J.; Bruijn, S.M.; Wu, W.; Lin, X.; Hu, H.; Huang, C.; Shi, L.; van Dieën, J.H. The effects of stride length and stride frequency on trunk coordination in human walking. Gait Posture 2010, 31, 444–449. [Google Scholar] [CrossRef] [PubMed]
- Dedieu, P.; Zanone, P.-G. Effects of gait pattern and arm swing on intergirdle coordination. Hum. Mov. Sci. 2012, 31, 660–671. [Google Scholar] [CrossRef]
- Shamsi, M.; Sarrafzadeh, J.; Jamshidi, A.; Arjmand, N.; Ghezelbash, F. Comparison of spinal stability following motor control and general exercises in nonspecific chronic low back pain patients. Clin. Biomech. 2017, 48, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Imai, A.; Kaneoka, K.; Okubo, Y.; Shiina, I.; Tatsumura, M.; Izumi, S.; Shiraki, H. Trunk muscle activity during lumbar stabilization exercises on both a stable and unstable surface. J. Orthop. Sports Phys. Ther. 2010, 40, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Vogt, L.; Pfeifer, K.; Banzer, W. Neuromuscular control of walking with chronic low-back pain. Man. Ther. 2003, 8, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.A.; Kulig, K. Trunk-pelvis coordination during turning: A cross sectional study of young adults with and without a history of low back pain. Clin. Biomech. 2016, 36, 58–64. [Google Scholar] [CrossRef]
- Roland, M.; Morris, R. A study of the natural history of back pain. Part 1: Development of a reliable and sensitive measure of disability in low back pain. Spine 1983, 8, 141–144. [Google Scholar] [CrossRef]
- Zerkak, D.; Métivier, J.-C.; Fouquet, B.; Beaudreuil, J. Validation of a French version of Roland–Morris questionnaire in chronic low back pain patients. Ann. Phys. Rehabil. Med. 2013, 56, 613–620. [Google Scholar] [CrossRef]
- Smeets, R.; Köke, A.; Lin, C.; Ferreira, M.; Demoulin, C. Measures of function in low back pain/disorders: Low Back Pain Rating Scale (LBPRS), Oswestry Disability Index (ODI), Progressive Isoinertial Lifting Evaluation (PILE), Quebec Back Pain Disability Scale (QBPDS), and Roland-Morris Disability Questionnaire (RDQ). Arthritis Care Res. 2011, 63, S158–S173. [Google Scholar]
- Parkerson, G.R., Jr.; Broadhead, W.; Tse, C.-K.J. The Duke Health Profile: A 17-item measure of health and dysfunction. Med. Care 1990, 28, 1056–1072. [Google Scholar] [CrossRef]
- Plotnik, M.; Bartsch, R.P.; Zeev, A.; Giladi, N.; Hausdorff, J.M. Effects of walking speed on asymmetry and bilateral coordination of gait. Gait Posture 2013, 38, 864–869. [Google Scholar] [CrossRef]
- Dedieu, P.; Chamoun, R.; Lacaud, G.; Moulinat, T.; Queron, M.; Zanone, P.G. Does a not-so-recent ankle sprain influence interjoint coordination during walking? Clin. Biomech. 2017, 50 (Suppl. C), 114–121. [Google Scholar] [CrossRef] [PubMed]
- Perry, J.; Burnfield, J. Gait Analysis: Normal and Pathological Function, 2nd ed.; SLACK Incorporated: West Deptford, NJ, USA, 2010. [Google Scholar]
- Hermens, H.J.; Freriks, B.; Disselhorst-Klug, C.; Rau, G. Development of recommendations for SEMG sensors and sensor placement procedures. J. Electromyogr. Kinesiol. 2000, 10, 361–374. [Google Scholar] [CrossRef]
- Winter, D.A.; Yack, H.J. EMG profiles during normal human walking: Stride-to-stride and inter-subject variability. Electroencephalogr. Clin. Neurophysiol. 1987, 67, 402–411. [Google Scholar] [CrossRef]
- Kurz, M.J.; Stergiou, N. Effect of normalization and phase angle calculations on continuous relative phase. J. Biomech. 2002, 35, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Pikovsky, A.; Rosenblum, M.; Kurths, J. Synchronization: A Universal Concept in Nonlinear Sciences; The Cambridge Nonlinear Science Series; Cambridge University Press: Cambridge, UK, 2001. [Google Scholar]
- Winter, D.A. Biomechanics and Motor Control of Human Movement, 4th ed.; John Wiley & Sons: Hoboken, NJ, USA, 2009. [Google Scholar]
- Yang, J.F.; Winter, D.A. Electromyographic amplitude normalization methods: Improving their sensitivity as diagnostic tools in gait analysis. Arch. Phys. Med. Rehabil. 1984, 65, 517–521. [Google Scholar] [PubMed]
- Burden, A.M.; Trew, M.; Baltzopoulos, V. Normalisation of gait EMGs: A re-examination. J. Electromyogr. Kinesiol. 2003, 13, 519–532. [Google Scholar] [CrossRef]
- Chang, W.-N.; Lipton, J.S.; Tsirikos, A.I.; Miller, F. Kinesiological surface electromyography in normal children: Range of normal activity and pattern analysis. J. Electromyogr. Kinesiol. 2007, 17, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: London, UK, 2010. [Google Scholar]
- Cohen, J. A Power Primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Bruijn, S.M.; Meijer, O.G.; van Dieën, J.H.; Kingma, I.; Lamoth, C.J. Coordination of leg swing, thorax rotations, and pelvis rotations during gait: The organisation of total body angular momentum. Gait Posture 2008, 27, 455–462. [Google Scholar] [CrossRef]
- Winter, D.A.; Prince, F.; Frank, J.S.; Powell, C.; Zabjek, K.F. Unified theory regarding A/P and M/L balance in quiet stance. J. Neurophysiol. 1996, 75, 2334–2343. [Google Scholar] [CrossRef]
- Della Volpe, R.; Popa, T.; Ginanneschi, F.; Spidalieri, R.; Mazzocchio, R.; Rossi, A. Changes in coordination of postural control during dynamic stance in chronic low back pain patients. Gait Posture 2006, 24, 349–355. [Google Scholar] [CrossRef]
- Beaudreuil, J.; Zerkak, D.; Métivier, J.-C.; Fouquet, B. Care related pain and functional restoration for chronic low back pain: A prospective study. Ann. Phys. Rehabil. Med. 2013, 56, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Schelldorfer, S.; Ernst, M.J.; Rast, F.M.; Bauer, C.M.; Meichtry, A.; Kool, J. Low back pain and postural control, effects of task difficulty on centre of pressure and spinal kinematics. Gait Posture 2015, 41, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W.; Tucker, K. Moving differently in pain: A new theory to explain the adaptation to pain. Pain 2011, 152, S90–S98. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, N.; Feldman, A.G. Interjoint coordination in lower limbs during different movements in humans. Exp. Brain Res. 2003, 148, 139–149. [Google Scholar] [CrossRef] [PubMed]
- Dedieu, P.; Salesse, M.; Champain, G.; Zanone, P.G. Comparing lunge techniques depending on the weapon used: Differences between foil and epee fencers. J. Phys. Educ. Sport 2024, 24, 974–985. [Google Scholar]

| Control Group (n = 16) | Low Back Pain Group (n = 18) | p | |
|---|---|---|---|
| Age (years) | 29.41 (3.32) | 29.67 (2.92) | 0.41 |
| Height (m) | 1.65 (0.09) | 1.67 (0.08) | 0.23 |
| Mass (kg) | 62.25 (11.17) | 64.25 (7.98) | 0.28 |
| Body Mass Index | 22.73 (2.25) | 21.93 (1.98) | 0.39 |
| Duration from Low Back Pain Diagnostic (months) | 27.25 (9.76) | ||
| Disability (Roland–Morris Disability Questionnaire) | 0.88 (0.72) | 1.94 (1.02) | 0.001 |
| Duke Health Profile (General Health Score) | 82.63 (4.65) | 80.81 (5.98) | 0.17 |
| Duke Health Profile (Perceived Health Score) | 87.5 (22.36) | 78.13 (22.62) | 0.14 |
| Duke Health Profile (Pain Score) | 75 (31.62) | 68.75 (30.96) | 0.29 |
| Control Group (n = 16) | Low Back Pain Group (n = 18) | p | d | |
|---|---|---|---|---|
| Stance phase (%) | 58.06 (2.62) | 59.25 (2.49) | 0.20 | |
| Speed (m.s−1) | 0.96 (0.04) | 0.97 (0.04) | 0.46 | |
| Hip (°) | 0.26 (0.12) | 0.18 (0.16) | 0.09 | |
| Knee (°) | 0.41 (0.01) | 0.4 (0.01) | 0.11 | |
| Ankle (°) | 0.49 (0.17) | 0.58 (0.14) | 0.12 | |
| Inter-girdle CRP (°) * | −132.06 (9.86) | −109.88 (9.7) | 0.001 | 1.49 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pascaud, P.; Houel, N.; Dedieu, P. Inter-Girdle Coordination as a Predictive Measure of Low Back Pain. Sensors 2025, 25, 4928. https://doi.org/10.3390/s25164928
Pascaud P, Houel N, Dedieu P. Inter-Girdle Coordination as a Predictive Measure of Low Back Pain. Sensors. 2025; 25(16):4928. https://doi.org/10.3390/s25164928
Chicago/Turabian StylePascaud, Paul, Nicolas Houel, and Philippe Dedieu. 2025. "Inter-Girdle Coordination as a Predictive Measure of Low Back Pain" Sensors 25, no. 16: 4928. https://doi.org/10.3390/s25164928
APA StylePascaud, P., Houel, N., & Dedieu, P. (2025). Inter-Girdle Coordination as a Predictive Measure of Low Back Pain. Sensors, 25(16), 4928. https://doi.org/10.3390/s25164928






