Abstract
We recently reported enhanced parasympathetic activation at rest throughout pregnancy associated with regular yoga practice. The present study presents a secondary analysis of data collected within a prospective cohort study of 33 pregnant women practicing yoga once weekly throughout pregnancy and 36 controls not involved in formal pregnancy exercise programs. The objective was to assess the impact of prenatal yoga on the autonomic nervous system stress response. Healthy pregnant women with singleton pregnancies were recruited in the first trimester. There was no significant difference in the maternal body mass index (BMI) between the yoga group and the controls (24.06 ± 3.55 vs. 23.74 ± 3.43 kg/m2, p = 0.693). Women practicing yoga were older (28.6 ± 3.9 vs. 31.3 ± 3.5 years, p = 0.005) and more often nulliparous (26 (79%) vs. 18 (50%), p = 0.001). We studied heart rate variability (HRV) parameters in the time domain (SDNN, standard deviation of regular R-R intervals, and RMSSD, square root of mean squared differences of successive R-R intervals) and frequency domain (ln(LF/HF), natural logarithm of low-frequency to high-frequency power), as well as synchronization indices of heart rate, blood pressure and respiration during and immediately following acute psychological stress of a standardized mental challenge test. Measurements were performed once per trimester before and after yoga or a 30 min moderate-intensity walk. Statistical comparison was performed using three-way analyses of variance (p < 0.05 significant). Time domain HRV parameters during and following mental challenge in the yoga group were significantly higher compared to the controls regardless of the trimester (F = 7.22, p = 0.009 for SDNN and F = 9.57, p = 0.003 for RMSSD, respectively). We observed no significant differences in the yoga group vs. the controls in terms of ln(LF/HF) and synchronization indices. Regular prenatal yoga practice was associated with a significantly reduced sympathetic response to mental challenge and quicker recovery after acute psychological stress. These effects persisted throughout pregnancy with regular practice.
1. Introduction
Yoga is a body–mind practice that encompasses a system of body postures (asanas), combined with breathing (pranayama) and concentration (dharana) exercises as well as meditation (dhyana) techniques [1]. It has gained popularity in Western countries over the last century [1]. Research has identified yoga as one of the most commonly used methods for a complementary health approach (besides meditation and seeing a chiropractor) [2]. The percentage of adults in the United States who used yoga for this purpose in the last 12 months increased from 9.5% in 2012 to 14.3% in 2017 [3]. About 70% of practitioners are women, with the majority in their reproductive age [4]. As a result, yoga is increasingly popular among pregnant women [4,5]. In the US, 7% of women reported practicing yoga during pregnancy [4].
Yoga is often listed among the safest and most beneficial forms of physical activity during pregnancy [6]. Studies showed associations between prenatal yoga and decreased incidence of fetal growth restriction, preterm delivery, prolonged and dysfunctional labor as well as perinatal mental disorders such as antenatal anxiety, depression and stress [7,8,9,10,11,12,13]. This could be, at least in part, attributed to the beneficial effects of yoga on autonomous nerve activity. The maternal cardiovascular system undergoes profound changes during pregnancy and the autonomic nervous system plays a central role in cardiovascular adaptation to pregnancy-related hemodynamic changes [14,15,16,17,18]. Our group has recently reported enhanced parasympathetic activation at rest throughout pregnancy associated with regular yoga practice [19].
Yoga has also been reported to improve stress reactivity in healthy non-pregnant adults [20]. This could further enhance yoga’s beneficial effects on the maternal cardiovascular system. The impact of yoga on acute stress response in pregnancy has, however, not been studied yet. This manuscript presents a secondary analysis of data collected within a prospective cohort study of pregnant women practicing yoga regularly from the first trimester [19]. Data on alterations of heart rate variability (HRV) and cardio-respiratory phase synchronization during and immediately following acute stress response to mental challenge are original and have not been published previously. The objective of the present study was to explore the effect of yoga compared to moderate walking on HRV parameters and cardio-respiratory synchronization indices during and following acute stress using non-invasive beat-to-beat monitoring for hemodynamic and autonomic functions of the human body.
2. Materials and Methods
We included 69 healthy pregnant women in a prospective cohort study from August 2020 to April 2022. Women with preexisting cardiovascular disease (including hypertension and arrhythmias), taking medications that would affect heart rate or blood pressure, psychiatric disorders, epilepsy, kidney disease, liver disease, rheumatoid autoimmune disorders, diabetes mellitus, alcohol and/or illicit drug abuse, known fetal anomaly, or multiple pregnancies were excluded from the study. Previous yoga experience was not considered an exclusion criterion. Thirty-three women practiced pregnancy-adapted yoga according to the system Yoga in daily life regularly (at least once weekly) throughout all three trimesters of pregnancy [21]. Yoga classes were held at Soncna vila yoga studio in Maribor, Slovenia and were led by a certified experienced prenatal yoga instructor. Classes lasted for 90 min and consisted of initial relaxation (10–15 min), followed by yoga postures and stretching exercises and a final 20–30 min of breathing and meditation techniques. The adaptation of yoga practices for specific gestational age was based on in-depth consultations with gynecologists and experienced physical therapists. Thirty-six women (controls) did not attend any formal physical exercise program. All participants provided written informed consent to study participation. The study was approved by the Institutional Review Board of the University Medical Center Maribor [22] and the Slovenian National Medical Ethics Committee (project number 0120-575/2018/5, approved on 22 February 2019). The detailed participant enrollment procedure and study flow have been published previously [19] (Clinicaltrials.gov registration: NCT04476368).
The study protocol is presented in Figure 1. All measurements were performed in the afternoon, before and after yoga practice (or a 30 min moderate-intensity walk in the control group) once per trimester of pregnancy. Measurements in the yoga group were performed before and after yoga practice. Measurements in the control group were performed before and after 30 min of moderate-intensity walking.
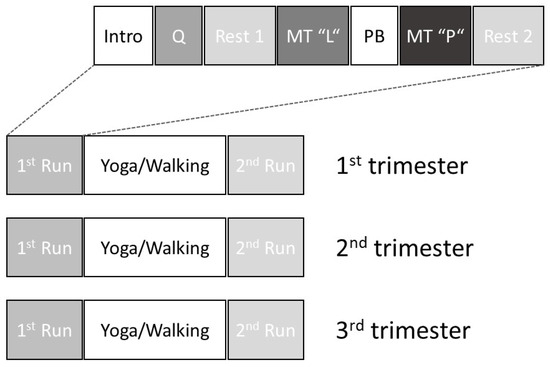
Figure 1.
Schematic representation of the study protocol. Intro: introduction to the study and demonstration of the interventions; Q: questionnaires; Rest 1: baseline; MT “L”: memory task “learning”; PB: paced breathing at 10 min−1; MT “P”: memory task “practicing”; Rest 2: post-intervention recovery.
Mental challenge comprised of a standardized memory task. First, the participants had to memorize 12 character strings of 4 letters. This “learning” memory task was followed by 2 min of paced breathing at 10 min−1 and then by the memory task itself, during which the participants had to choose the right (memorized) character string out of 5 options. This mental challenge was followed by a rest/recovery phase (Figure 1).
Continuous monitoring of blood pressure (sampling rate (sr) = 100 Hz, blood pressure range = 50–250 mmHg, ±5 mmHg) and heart rate (R-R intervals derived from 3-lead electrocardiography (ECG), sr = 1 kHz, fcut-off = 0.08–150 Hz) was carried out throughout the whole measurement protocol with the Task Force® Monitor (CNSystems, Medizintechnik AG, Graz, Austria) [23]. Continuous blood pressure was measured using the participants’ finger and a refined version of the vascular unloading technique, which was corrected to absolute values with oscillometric blood pressure measurement by the Task Force® Monitor [23]. Thoracic impedance electrodes were placed at the neck and thoracic regions (specifically in the midclavicular line at the xiphoid process level). Respiration was derived from thoracic impedance (sr = 500 Hz for thoracic impedance; for synchronization analysis, we used a resampled signal of 4 Hz). Raw data were exported to MATLAB® (The Math Works, Inc., Natick, MA, USA) data format for further analysis. A semi-automatic artifact-handling software, described in detail in our previous publications, was used for artifact handling of the continuous recordings [19,24].
2.1. Heart Rate Variabity Parameters
The time domain HRV parameters analyzed during and following mental challenge (memory task and post-intervention recovery in Figure 1) were SDNN (standard deviation of the regular R-R intervals) and RMSSD (square root of the mean squared differences of successive R-R intervals). While the RMSSD is influenced more by vagal tone, the SDNN represents the activity of both sympathetic and parasympathetic branches.
The frequency domain HRV parameter analyzed was the ln(LF/HF) (natural logarithm of low-frequency (LF) to high-frequency (HF) power ratio) [25]. The prerequisites for the calculation of the HRV variables, such as the “quasi-stationarity” of the intervals and the appropriate estimation of the variables in the frequency range, were checked in advance using basic mathematical equations (e.g., Parseval’s theorem) [24].
2.2. Phase Synchronization Indices
The concept of analytic signals based on the Hilbert transform can be used to define the phase of an arbitrary signal such as the heart rate. This approach was implemented to calculate the phase synchronization indices, e.g., heart rate and systolic blood. The algorithm of our software toolbox, implemented in Matlab® (R2022a), operates in the following way:
- The function HILBERT compute the so-called discrete-time analytic signal X with X = Xr + I × Xi in a narrow frequency band such that Xi is the Hilbert transform of the real vector Xr. To obtain a clear physical interpretation that is given only for narrow band signals, we use the band-pass filtered time series.
- In the next step, the function ANGLE is used to calculate the phase of the resulting signal X at every time point with the function.
- Subsequently, the difference between two given phase vectors for the interpolated bivariate data series, e.g., between heart rate and systolic blood pressure, can be calculated.
- The distribution of phase difference Ψ(ti) is quantified by the synchronization index γ defined as
γ = {cos Ψ(ti)}2 + {sin Ψ(ti)}2 [0 ≤ γ ≤ 1],
If the synchronization index γ = 1, then both time series are completely synchronized in a statistical sense, while in the case of γ = 0, both time series are completely desynchronized, i.e., the values of Ψ(ti) are equally distributed in the range of [−π, π]. Thus, phase synchronization provides a quantitative indicator of the coordinated behavior of pairs of systems. The methodology to calculate cardio-respiratory indices and the rationale behind these calculations have been described previously by our research group [17].
Continuous blood pressure was obtained using the participants’ finger as mentioned above. Therefore, an additional aspect must be taken into account: the continuous blood pressure signal needs to be “calibrated” via the blood pressure cuff on the upper arm at regular intervals. Nevertheless, for offline recalculations like our software, recalculation criteria can be defined to correctly estimate the dynamic behavior between two “calibration points”. We use pulse transition time as additional plausibility criteria in our updated software to ensure an optimal estimation of the time series of systolic (and diastolic) blood pressure.
Synchronization indices between systolic blood pressure and RR interval (inter-beat interval between successive heartbeats) (γSBP* × RR), between respiratory frequency and RR interval (γRF × RR), as well as between respiratory frequency and systolic blood pressure (γRF × SBP) were analyzed for the purpose of the study.
2.3. Statistical Analysis
Statistical comparison of background clinical characteristics in yoga vs. control groups was performed using the univariate analysis of variance (F-test) for continuous variables and Chi-square test for categorical variables. For continuous variables, data were expressed as means with standard deviations. Categorical data were summarized as frequencies and percentages. To determine whether the intervention (yoga vs. control) significantly influenced a given parameter measured, the differences in HRV parameters and phase synchronization indices were statistically compared using 2 × 3 × 2 three-way analyses of variance. The delta values (e.g., SDNN after intervention [yoga or walk] minus heart rate before intervention) of time intervals (memory task and recovery) and trimester of pregnancy (first, second and third trimester) were the within-subject factors in these analyses, and intervention (yoga vs. control) was the between-subject factor, thus accounting for the physiological change in this parameter throughout pregnancy and following any physical activity. A p ≤ 0.05 was considered statistically significant and the effect size of yoga intervention was estimated using the partial Eta-squared (ηp2). IBM SPSS Statistics for Windows Version 25.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis.
3. Results
All 69 women included in the study were of Caucasian ethnicity. There was no significant difference in the maternal body mass index (BMI) between the yoga group and controls (24.06 ± 3.55 vs. 23.74 ± 3.43 kg/m2, p = 0.693). Women practicing yoga were older (28.6 ± 3.9 vs. 31.3 ± 3.5 years, p = 0.005) and more often nulliparous (26 (79%) vs. 18 (50%), p = 0.001) [19].
Table 1 presents the changes in HRV parameters after minus before yoga practice (yoga group) and after minus before 30 min walk (control group) in all three trimesters of pregnancy.

Table 1.
Heart rate variability parameters after minus before yoga practice (yoga group) and after minus before 30 min walk (control group) throughout pregnancy.
Between-subject analysis showed a significantly lower heart rate during and immediately following a mental challenge in the yoga group compared to controls in all three trimesters (F = 31.26, p < 0.001, ηp2 = 0.32). We also observed significantly higher time domain HRV parameters during and following mental challenge in the yoga group vs. controls regardless of pregnancy trimester (F = 7.22, p = 0.009, ηp2 = 0.10 for SDNN and F = 9.57, p = 0.003, ηp2 = 0.13 for RMSSD, respectively). In terms of frequency domain HRV parameters, ln(LF/HF) did not significantly decrease during or following mental challenge in the yoga vs. control groups (F = 0.84, p = 0.363).
Within-subject analysis showed a significant interaction for time intervals (memory task and recovery phase) × group and three-time interaction for trimester × time intervals × group for RMSSD (F = 4.12, p = 0.046, ηp2 = 0.06 and F = 4.27, p = 0.016, ηp2 = 0.06, respectively), whereas no significant interactions were observed for HR, SDNN, or ln(LF/HF) (all p’s > 0.12 and >0.054, respectively) (Figure 2).
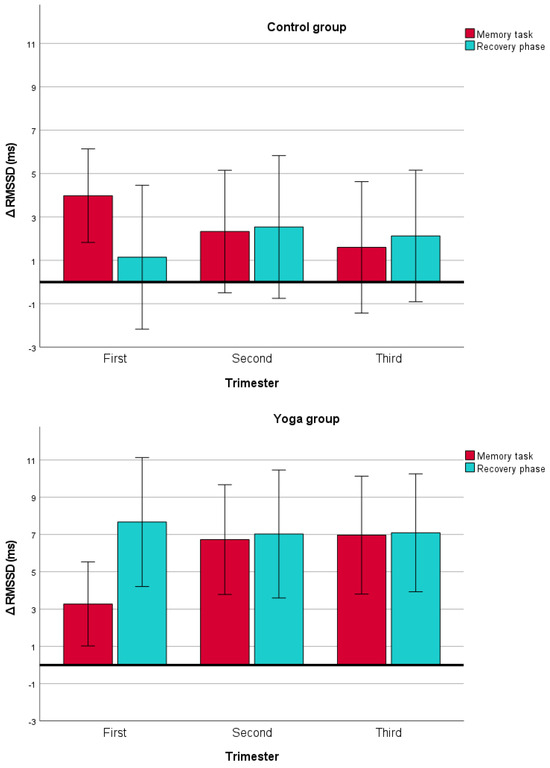
Figure 2.
Δ RMSSD (root mean square of successive RR interval differences) with 95% confidence intervals during and immediately following a mental challenge after minus before yoga (bottom figure) vs. walking (upper figure) throughout all three trimesters of pregnancy. Note a significantly higher RMSSD values following yoga, suggesting a more pronounced decrease in the sympathetic to parasympathetic autonomic balance in the yoga group compared to controls (F = 9.57, p = 0.003).
Table 2 presents blood pressure variables, respiratory frequency and phase synchronization indices after minus before yoga practice (yoga group) and after minus before 30 min walk (control group) in all three trimesters of pregnancy.

Table 2.
Blood pressure variables, respiratory frequency and phase synchronization indices after minus before yoga practice (yoga group) and after minus before 30 min walk (control group) throughout pregnancy.
Between-subject analysis showed no difference in systolic blood pressure (SBP) (F = 0.30, p = 0.587), mean arterial pressure (MAP) (F = 0.80, p = 0.376), diastolic blood pressure (DPB) (F = 0.81, p = 0.371), respiratory frequency (RF) (F = 2.21, p = 0.142), γRF × RR (F = 0.01, p = 0.944), or γRF × SBP (F = 0.27, p = 0.606) during or immediately following a mental challenge in the yoga group compared to controls in all three trimesters. There was a statistically significant difference towards a lower change in the synchronization index between the SBP and RR interval γSBP × RR in the yoga group compared to the controls (F = 4.59, p = 0.037, ηp2 = 0.06).
Within-subject analysis showed no significant interaction for time intervals × group or three-time interaction for trimester × time intervals × group (all p values > 0.089 and > 0.061, respectively).
4. Discussion
Women in the yoga group had significantly increased time domain HRV parameters (i.e., SDNN and RMSSD) during the memory task and during the recovery phase compared to the controls.
The study adds important novel information to our previous report on significantly increased SDNN and RMSSD as well as decreased ln(LF/HF) at rest in women practicing prenatal yoga compared to pregnant controls not enrolled in formal pregnancy exercise programs [19]. The present analysis of non-invasive data acquired during the mental challenge and recovery phases of our measurement protocol shows that regular yoga practice during pregnancy results in improved stress reactivity with blunted sympathetic surges associated with acute stressful events as well as faster recovery from stress. These results are in accordance with several studies on the effects of yoga on the autonomic nervous system published to date by other groups. Practicing yoga has been shown to increase parasympathetic activity outside pregnancy in both novices and experienced practitioners [26,27,28,29,30,31]. Single yoga sessions have also been shown to improve stress reactivity in healthy non-pregnant adults [20]. In pregnancy, acute decreases in sympathetic activity not provoked by stress tests following single yoga classes have been reported by Satyapriya et al. [14]. As demonstrated in previous research, prenatal yoga practice was mostly associated with HRV changes while there was no significant impact of yoga on cardio-respiratory synchronization indices [14,19].
The neurovascular responses to psychological stress of a memory task are well known and include activation of the sympathetic system, increases in heart rate, cardiac output, blood pressure, vasoconstriction in the splanchnic and renal regions, and vasodilatation in skeletal muscles [18]. It has to be noted that response to memory tasks can be influenced by several factors, like the response option or the stimulus interval [32]. Nevertheless, in a recent review, Immanuel et al. concluded that HRV is a reliable measure of psychological stress response when standard stress induction and assessment protocols combined with validated HRV parameters in different domains are used [33]. They also stated that RMSSD was the most frequently reported HRV metric [33]. Several advantages of time domain HRV parameters have also recently been reported by our group [24]. In the present study, responses to memory-task-associated stress were assessed using a short and simple protocol with almost no influence of the response (a mouse click only) and stimulus interval (mouse clicks at irregular time intervals) on HRV parameters.
No study to date has focused on the effects of yoga on a pregnant woman’s ability to cope with acute psychological stress. Lackner et al. described a decrease in parasympathetic activity during mental challenge in healthy non-pregnant women [17]. In the present study, a decrease in time domain HRV parameters indicating shifts towards sympathetic dominance during mental challenge was markedly reduced after physical activity, including both yoga and moderate-intensity walking. However, this reduction was significantly more profound after practicing yoga compared to walking. Moreover, our results indicate a faster recovery, i.e., higher SDNN and RMSSD in the recovery phase after mental challenge in pregnant women practicing yoga regardless of the trimester. This may be explained by the fact that yoga typically encompasses more than just aerobic physical activity. Besides physical postures (asanas), yoga includes breathing (pranayama), concentration (dharana) and meditation (dhyana) exercises, which could increase parasympathetic activation and enhance stress-coping abilities.
Several limitations of the study should be considered. This was an observational study so we could not account for all potential confounders, such as differences in maternal age and parity. It is possible that younger and nulliparous women may have had a different reactivity in response to stress. In addition, potential sociodemographic and economic differences were not considered. Furthermore, pre-pregnancy experience with yoga and other relaxation techniques were not assessed. Future research in the field, ideally in the form of well-designed and adequately powered randomized trials will be needed to evaluate the impact of previous yoga experience and its impact on stress modulation in pregnancy. Currently, no definitive conclusions on the causal relationship between yoga and the observed results can be drawn. We were also not able to assess the actual amount of physical activity in either the yoga or control groups. Participants in the yoga group attended one guided yoga session weekly throughout pregnancy, but we do not have the data on whether and/or how often they practiced at home. As a result, it is not possible to assess a possible “dose-dependent” yoga effect with more profound effects of prenatal yoga on the autonomous nervous system with a higher frequency and duration of yoga sessions. We do also not know if the participants in either group engaged in other forms of exercise during pregnancy. Future research in this field could potentially utilize digital wearable technologies to more accurately assess physical activity of the study participants. It should also be mentioned that a single yoga teacher led all the classes throughout the study, which makes generalizing the results difficult. Further studies involving different yoga teachers and different populations of pregnant women will be needed to confirm or refute our results. Nevertheless, this study adds important information on the potential modulatory effects of different forms of physical activity on stress response during pregnancy. These could influence further research in the field with potential important clinical implications.
5. Conclusions
Time domain HRV parameters (SDNN and RMSSD) were increased in pregnant women who practiced yoga during acute stress provoked by a standardized memory task, as well as during recovery time intervals following mental challenge. With regular practice, the effects of yoga on the autonomic nervous system response to acute stress persisted throughout all three trimesters of pregnancy. Our results suggest potentially improved stress reactivity with blunted sympathetic surges in response to acute stressful events as well as quicker recovery after psychological stress associated with regular yoga practice during pregnancy.
Author Contributions
Conceptualization and supervision, I.Ž., M.L., D.D., H.K.L. and M.G.M.; writing—review and editing, I.Ž., D.D., M.G.M., I.V.D. and A.M.; writing—original draft preparation, M.L., D.D. and H.K.L.; software, H.K.L., A.M. and M.L.; methodology, I.Ž. and I.V.D.; validation, M.G.M.; formal analysis, H.K.L. and A.M.; investigation, I.Ž.; resources and project administration, M.L. and D.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially funded by University Clinical Center Maribor, grant number IRP-2019/01-12 and Slovenian Research and Innovation Agency, grant number P3-0036.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Slovenian National Medical Ethics Committee, project number 0120-575/2018/5, approved on 22 February 2019.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.
Conflicts of Interest
I.V.D. is the owner of the yoga studio “Soncna vila” and was the yoga instructor leading all the yoga classes in the study. She was not involved in the measurements or data analysis. The other authors declare no potential conflicts of interest.
References
- Sengupta, P. Health Impacts of Yoga and Pranayama: A State-of-the-Art Review. Int. J. Prev. Med. 2012, 3, 444–458. [Google Scholar] [PubMed]
- Clarke, T.C.; Black, L.I.; Stussman, B.J.; Barnes, P.M.; Nahin, R.L. Trends in the Use of Complementary Health Approaches among Adults: United States, 2002–2012; National Health Statistics Reports, no 79; National Center for Health Statistics: Hyattsville, MD, USA, 2015. [Google Scholar]
- Clarke, T.C.; Barnes, P.M.; Black, L.I.; Stussman, B.J.; Nahin, R.L. Use of Yoga, Meditation, and Chiropractors among U.S. Adults Aged 18 and over; NCHS Data Brief No. 325; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Washington, DC, USA, 2018. Available online: https://www.cdc.gov/nchs/data/databriefs/db325-h.pdf (accessed on 7 October 2023).
- Babbar, S.; Shyken, J. Yoga in Pregnancy. Clin. Obs. Gynecol. 2016, 59, 600–612. [Google Scholar] [CrossRef]
- Evenson, K.R.; Wen, F. National trends in self-reported physical activity and sedentary behaviors among pregnant women: NHANES 1999–2006. Prev Med. 2010, 50, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Syed, H.; Slayman, T.; DuChene Thoma, K. ACOG Committee Opinion No. 804: Physical Activity and Exercise during Pregnancy and the Postpartum Period. Obs. Gynecol. 2021, 137, 375–376. [Google Scholar] [CrossRef] [PubMed]
- Rong, L.; Dai, L.J.; Ouyang, Y.Q. The effectiveness of prenatal yoga on delivery outcomes: A meta-analysis. Complement. Ther. Clin. Pract. 2020, 39, 101157. [Google Scholar] [CrossRef]
- Zhang, L.; Wang, S. The Efficacy of Prenatal Yoga on Labor Pain: A Systematic Review and Meta-analysis. Altern. Ther. Health Med. 2023, 29, 121–125. [Google Scholar]
- Villar-Alises, O.; Martinez-Miranda, P.; Martinez-Calderon, J. Prenatal Yoga-Based Interventions May Improve Mental Health during Pregnancy: An Overview of Systematic Reviews with Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 1556. [Google Scholar] [CrossRef]
- Corrigan, L.; Moran, P.; McGrath, N.; Eustace-Cook, J.; Daly, D. The characteristics and effectiveness of pregnancy yoga interventions: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2022, 22, 250. [Google Scholar] [CrossRef]
- Kwon, R.; Kasper, K.; London, S.; Haas, D.M. A systematic review: The effects of yoga on pregnancy. Eur. J. Obs. Gynecol. Reprod. Biol. 2020, 250, 171–177. [Google Scholar] [CrossRef]
- Pascoe, M.C.; Bauer, I.E. A systematic review of randomised control trials on the effects of yoga on stress measures and mood. J. Psychiatr. Res. 2015, 68, 270–282. [Google Scholar] [CrossRef]
- Lučovnik, M.; Pravst, T.; Vesenjak Dinevski, I.; Žebeljan, I.; Dinevski, D. Yoga during pregnancy: A systematic review. Zdr. Vestn. 2021, 90, 150–158. [Google Scholar] [CrossRef]
- Satyapriya, M.; Nagendra, H.R.; Nagarathna, R.; Padmalatha, V. Effect of integrated yoga on stress and heart rate variability in pregnant women. Int. J. Gynaecol. Obs. 2009, 104, 218–222. [Google Scholar] [CrossRef]
- Ekholm, E.M.; Erkkola, R.U. Autonomic cardiovascular control in pregnancy. Eur. J. Obs. Gynecol. Reprod. Biol. 1996, 64, 29–36. [Google Scholar] [CrossRef]
- Fu, Q.; Levine, B.D. Autonomic circulatory control during pregnancy in humans. Semin. Reprod. Med. 2009, 27, 330–337. [Google Scholar] [CrossRef]
- Lackner, H.K.; Papousek, I.; Batzel, J.J.; Roessler, A.; Scharfetter, H.; Hinghofer-Szalkay, H. Phase synchronization of hemodynamic variables and respiration during mental challenge. Int. J. Psychophysiol. 2011, 79, 401–409. [Google Scholar] [CrossRef]
- Sharifi-Heris, Z.; Rahmani, A.M.; Axelin, A.; Rasouli, M.; Bender, M. Heart Rate Variability and Pregnancy Complications: Systematic Review. Interact. J. Med. Res. 2023, 12, e44430. [Google Scholar] [CrossRef]
- Žebeljan, I.; Lučovnik, M.; Dinevski, D.; Lackner, H.K.; Moertl, M.G.; Vesenjak Dinevski, I.; Mujezinovic, F. Effect of Prenatal Yoga on Heart Rate Variability and Cardio-Respiratory Synchronization: A Prospective Cohort Study. J. Clin. Med. 2022, 11, 5777. [Google Scholar] [CrossRef]
- Benvenutti, M.J.; Alves, E.D.S.; Michael, S.; Ding, D.; Stamatakis, E.; Edwards, K.M. A single session of hatha yoga improves stress reactivity and recovery after an acute psychological stress task-A counterbalanced, randomized-crossover trial in healthy individuals. Complement. Ther. Med. 2017, 35, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Maheshwarananda, P.S. The System Yoga in Daily Life; Harmony for Body, Mind and Soul; Ibera Verlag/European University Press: Vienna, Austria, 2000; Available online: https://www.yogaindailylife.org/system/en/ (accessed on 11 April 2023).
- Pahor, D. The Code of Ethical Conduct of the University of Maribor/Kodeks etičnega Ravnanja Univerze V Mariboru. Acta Med.-Biotechnol. 2022, 14, 7–9. [Google Scholar] [CrossRef]
- Fortin, J.; Habenbacher, W.; Heller, A.; Hacker, A.; Grüllenberger, R.; Innerhofer, J.; Passath, H.; Wagner, C.H.; Haitchi, G.; Flotzinger, D.; et al. Non-invasive beat-to-beat cardiac output monitoring by an improved method of transthoracic bioimpedance measurement. Comput. Biol. Med. 2006, 36, 1185–1203. [Google Scholar] [CrossRef] [PubMed]
- Lackner, H.K.; Eglmaier, M.T.W.; Hackl-Wimmer, S.; Paechter, M.; Rominger, C.; Eichen, L.; Rettenbacher, K.; Walter-Laager, C.; Papousek, I. How to Use Heart Rate Variability: Quantification of Vagal Activity in Toddlers and Adults in Long-Term ECG. Sensors 2020, 20, 5959. [Google Scholar] [CrossRef] [PubMed]
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Posadzki, P.; Kuzdzal, A.; Lee, M.S.; Ernst, E. Yoga for Heart Rate Variability: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Appl. Psychophysiol. Biofeedback 2015, 40, 239–249. [Google Scholar] [CrossRef]
- Chu, I.H.; Wu, W.L.; Lin, I.M.; Chang, Y.K.; Lin, Y.J.; Yang, P.C. Effects of Yoga on Heart Rate Variability and Depressive Symptoms in Women: A Randomized Controlled Trial. J. Altern. Complement. Med. 2017, 23, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Hewett, Z.L.; Pumpa, K.L.; Smith, C.A.; Fahey, P.P.; Cheema, B.S. Effect of a 16-week Bikram yoga program on heart rate variability and associated cardiovascular disease risk factors in stressed and sedentary adults: A randomized controlled trial. BMC Complement. Altern. Med. 2017, 17, 226. [Google Scholar] [CrossRef]
- Khattab, K.; Khattab, A.A.; Ortak, J.; Richardt, G.; Bonnemeier, H. Iyengar yoga increases cardiac parasympathetic nervous modulation among healthy yoga practitioners. Evid.-Based Complement. Altern. Med. 2007, 4, 511–517. [Google Scholar] [CrossRef]
- Sarang, P.; Telles, S. Effects of two yoga based relaxation techniques on heart rate variability (HRV). Int. J. Stress Manag. 2006, 13, 460. [Google Scholar] [CrossRef]
- Melville, G.W.; Chang, D.; Colagiuri, B.; Marshall, P.W.; Cheema, B.S. Fifteen minutes of chair-based yoga postures or guided meditation performed in the office can elicit a relaxation response. Evid.-Based Complement. Altern. Med. 2012, 2012, 501986. [Google Scholar] [CrossRef]
- Lackner, H.K.; Goswami, N.; Hinghofer-Szalkay, H.; Papousek, I.; Scharfetter, H.; Furlan, R.; Schwaberger, G. Effects of Stimuli on Cardiovascular Reactivity Occurring at Regular Intervals During Mental Stress. J. Psychophysiol. 2010, 24, 48–60. [Google Scholar] [CrossRef]
- Immanuel, S.; Teferra, M.N.; Baumert, M.; Bidargaddi, N. Heart Rate Variability for Evaluating Psychological Stress Changes in Healthy Adults: A Scoping Review. Neuropsychobiology 2023, 82, 187–202. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).