Locomotor Strategy to Perform 6-Minute Walk Test in People with Multiple Sclerosis: A Prospective Observational Study
Abstract
1. Introduction
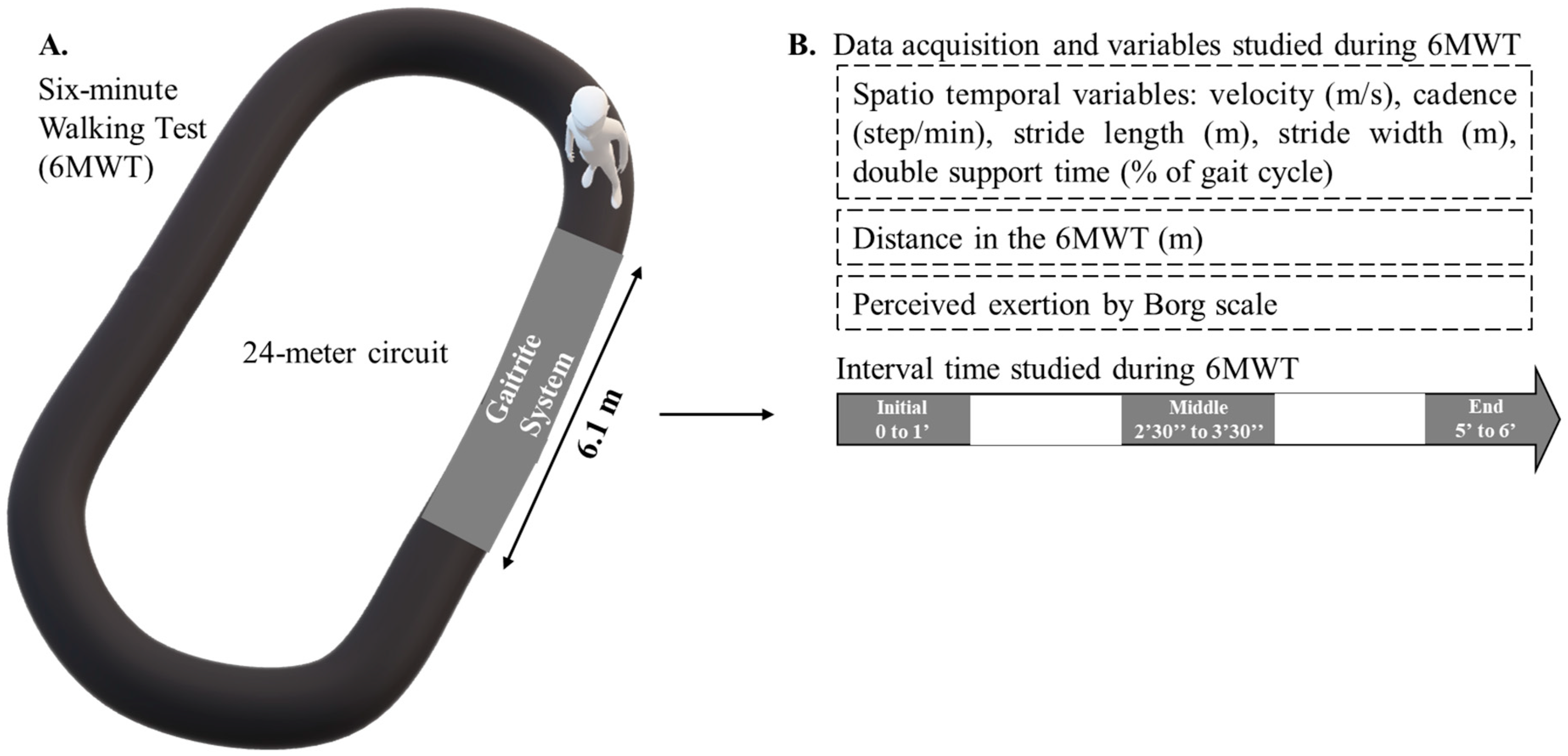
2. Methods
2.1. Study Design
2.2. Participants
- (i)
- an MS diagnosis according to the modified McDonald criteria [29];
- (ii)
- (iii)
- the capacity to walk for at least 6 min (according to the data from the medical examination, i.e., EDSS).
- (i)
- worsening MS symptoms during the previous 60 days;
- (ii)
- immunotherapy change in the previous 60 days;
- (iii)
- the presence of other neurological disorders.
3. Evaluations
3.1. Clinical Evaluation
3.2. Walking Evaluation
3.3. Statistical Analysis
4. Results
5. Discussion
Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Reese, H.H. What Do We Know of Multiple Sclerosis? J. Lancet 1946, 66, 359–362. [Google Scholar] [PubMed]
- Compston, A.; Coles, A. Multiple Sclerosis. Lancet 2008, 372, 1502–1517. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, M. The Impact of Slower Walking Speed on Activities of Daily Living in Patients with Multiple Sclerosis: The Impact of Slower Walking Speed on Activities of Daily Living in Patients with Multiple Sclerosis. Int. J. Clin. Pract. 2012, 66, 1088–1094. [Google Scholar] [CrossRef] [PubMed]
- Pike, J.; Jones, E.; Rajagopalan, K.; Piercy, J.; Anderson, P. Social and Economic Burden of Walking and Mobility Problems in Multiple Sclerosis. BMC Neurol. 2012, 12, 94. [Google Scholar] [CrossRef]
- Heesen, C.; Böhm, J.; Reich, C.; Kasper, J.; Goebel, M.; Gold, S.M. Patient Perception of Bodily Functions in Multiple Sclerosis: Gait and Visual Function Are the Most Valuable. Mult. Scler. 2008, 14, 988–991. [Google Scholar] [CrossRef]
- Larocca, N.G. Impact of Walking Impairment in Multiple Sclerosis: Perspectives of Patients and Care Partners. Patient 2011, 4, 189–201. [Google Scholar] [CrossRef]
- Kurtzke, J.F. Rating Neurologic Impairment in Multiple Sclerosis: An Expanded Disability Status Scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef]
- Skjerbæk, A.G.; Boesen, F.; Petersen, T.; Rasmussen, P.V.; Stenager, E.; Nørgaard, M.; Feys, P.; Kjeldgaard-Jørgensen, M.L.; Hvid, L.G.; Dalgas, U. Can We Trust Self-Reported Walking Distance When Determining EDSS Scores in Patients with Multiple Sclerosis? The Danish MS Hospitals Rehabilitation Study. Mult. Scler. 2018, 25, 1653–1660. [Google Scholar] [CrossRef]
- Berger, W.; Payne, M.W.C.; Morrow, S.A. Self-Reported Maximum Walking Distance in Persons with MS May Affect the EDSS. J. Neurol. Sci. 2017, 379, 77–80. [Google Scholar] [CrossRef]
- Motl, R.W.; Cohen, J.A.; Benedict, R.; Phillips, G.; LaRocca, N.; Hudson, L.D.; Rudick, R. Multiple Sclerosis Outcome Assessments Consortium Validity of the Timed 25-Foot Walk as an Ambulatory Performance Outcome Measure for Multiple Sclerosis. Mult. Scler. 2017, 23, 704–710. [Google Scholar] [CrossRef]
- Moore, J.L.; Potter, K.; Blankshain, K.; Kaplan, S.L.; O’Dwyer, L.C.; Sullivan, J.E. A Core Set of Outcome Measures for Adults With Neurologic Conditions Undergoing Rehabilitation: A Clinical Practice Guideline. J. Neurol. Phys. Ther. 2018, 42, 174–220. [Google Scholar] [CrossRef] [PubMed]
- Goldman, M.D.; Marrie, R.A.; Cohen, J.A. Evaluation of the Six-Minute Walk in Multiple Sclerosis Subjects and Healthy Controls. Mult. Scler. J. 2008, 14, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Bethoux, F. Gait Disorders in Multiple Sclerosis. CONTINUUM Lifelong Learn. Neurol. 2013, 19, 1007–1022. [Google Scholar] [CrossRef] [PubMed]
- Givon, U.; Zeilig, G.; Achiron, A. Gait Analysis in Multiple Sclerosis: Characterization of Temporal–Spatial Parameters Using GAITRite Functional Ambulation System. Gait Posture 2009, 29, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Sosnoff, J.J.; Weikert, M.; Dlugonski, D.; Smith, D.C.; Motl, R.W. Quantifying Gait Impairment in Multiple Sclerosis Using GAITRite Technology. Gait Posture 2011, 34, 145–147. [Google Scholar] [CrossRef]
- Decavel, P.; Moulin, T.; Sagawa, Y. Gait Tests in Multiple Sclerosis: Reliability and Cut-off Values. Gait Posture 2019, 67, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Lizrova Preiningerova, J.; Novotna, K.; Rusz, J.; Sucha, L.; Ruzicka, E.; Havrdova, E. Spatial and Temporal Characteristics of Gait as Outcome Measures in Multiple Sclerosis (EDSS 0 to 6.5). J. Neuroeng. Rehabil. 2015, 12, 14. [Google Scholar] [CrossRef]
- Hochsprung, A.; Heredia-Camacho, B.; Castillo, M.; Izquierdo, G.; Escudero-Uribe, S. Clinical validity of the quantitative gait variables in patients with multiple sclerosis. A comparison of the Timed 25-foot Walk Test and the GAITRite® Electronic Walkway system. Rev. Neurol. 2014, 59, 8–12. [Google Scholar]
- Bethoux, F.; Bennett, S. Evaluating Walking in Patients with Multiple Sclerosis: Which Assessment Tools Are Useful in Clinical Practice? Int. J. MS Care 2011, 13, 4–14. [Google Scholar] [CrossRef]
- Dalgas, U.; Kjølhede, T.; Gijbels, D.; Romberg, A.; Santoyo, C.; Noordhout, B.; Knuts, K.; Feys, P. Aerobic Intensity and Pacing Pattern during the Six-Minute Walk Test in Patients with Multiple Sclerosis. J. Rehabil. Med. 2014, 46, 59–66. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS Statement. Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Butland, R.J.; Pang, J.; Gross, E.R.; Woodcock, A.A.; Geddes, D.M. Two-, Six-, and 12-Minute Walking Tests in Respiratory Disease. Br. Med. J. (Clin. Res. Ed.) 1982, 284, 1607–1608. [Google Scholar] [CrossRef] [PubMed]
- Beausoleil, S.; Miramand, L.; Turcot, K. Evolution of Gait Parameters in Individuals with a Lower-Limb Amputation during a Six-Minute Walk Test. Gait Posture 2019, 72, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Hadouiri, N.; Feuvrier, D.; Pauchot, J.; Decavel, P.; Sagawa, Y. Donor Site Morbidity after Vascularized Fibula Free Flap: Gait Analysis during Prolonged Walk Conditions. Int. J. Oral Maxillofac. Surg. 2018, 47, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Hadouiri, N.; Monnet, E.; Gouelle, A.; Decavel, P.; Sagawa, Y. Evaluation of Prolonged Walking in Persons with Multiple Sclerosis: Reliability of the Spatio-Temporal Walking Variables during the 6-Minute Walk Test. Sensors 2021, 21, 3075. [Google Scholar] [CrossRef] [PubMed]
- Plotnik, M.; Wagner, J.M.; Adusumilli, G.; Gottlieb, A.; Naismith, R.T. Gait Asymmetry, and Bilateral Coordination of Gait during a Six-Minute Walk Test in Persons with Multiple Sclerosis. Sci. Rep. 2020, 10, 12382. [Google Scholar] [CrossRef]
- Angelini, L.; Hodgkinson, W.; Smith, C.; Dodd, J.M.; Sharrack, B.; Mazzà, C.; Paling, D. Wearable Sensors Can Reliably Quantify Gait Alterations Associated with Disability in People with Progressive Multiple Sclerosis in a Clinical Setting. J. Neurol. 2020, 267, 2897–2909. [Google Scholar] [CrossRef]
- Chen, S.; Sierra, S.; Shin, Y.; Goldman, M.D. Gait Speed Trajectory During the Six-Minute Walk Test in Multiple Sclerosis: A Measure of Walking Endurance. Front. Neurol. 2021, 12, 1097. [Google Scholar] [CrossRef]
- Thompson, A.J.; Banwell, B.L.; Barkhof, F.; Carroll, W.M.; Coetzee, T.; Comi, G.; Correale, J.; Fazekas, F.; Filippi, M.; Freedman, M.S.; et al. Diagnosis of Multiple Sclerosis: 2017 Revisions of the McDonald Criteria. Lancet Neurol. 2018, 17, 162–173. [Google Scholar] [CrossRef]
- König, N.; Singh, N.B.; von Beckerath, J.; Janke, L.; Taylor, W.R. Is Gait Variability Reliable? An Assessment of Spatio-Temporal Parameters of Gait Variability during Continuous Overground Walking. Gait Posture 2014, 39, 615–617. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical Bases of Perceived Exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Walter, S.D.; Eliasziw, M.; Donner, A. Sample Size and Optimal Designs for Reliability Studies. Stat. Med. 1998, 17, 101–110. [Google Scholar] [CrossRef]
- Weir, J.P. Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM. J. Strength Cond. Res. 2005, 19, 231–240. [Google Scholar] [CrossRef]
- Cederberg, K.L.J.; Sikes, E.M.; Bartolucci, A.A.; Motl, R.W. Walking Endurance in Multiple Sclerosis: Meta-Analysis of Six-Minute Walk Test Performance. Gait Posture 2019, 73, 147–153. [Google Scholar] [CrossRef]
- Chetta, A.; Zanini, A.; Pisi, G.; Aiello, M.; Tzani, P.; Neri, M.; Olivieri, D. Reference Values for the 6-Min Walk Test in Healthy Subjects 20–50 Years Old. Respir. Med. 2006, 100, 1573–1578. [Google Scholar] [CrossRef] [PubMed]
- Egerton, T.; Paterson, K.; Helbostad, J.L. The Association Between Gait Characteristics and Ambulatory Physical Activity in Older People: A Cross-Sectional and Longitudinal Observational Study Using Generation 100 Data. J. Aging Phys. Act. 2017, 25, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Comber, L.; Galvin, R.; Coote, S. Gait Deficits in People with Multiple Sclerosis: A Systematic Review and Meta-Analysis. Gait Posture 2017, 51, 25–35. [Google Scholar] [CrossRef]
- Moumdjian, L.; Gervasoni, E.; Van Halewyck, F.; Eijnde, B.O.; Wens, I.; Van Geel, F.; Van Wijmeersch, B.; Feys, P.; Van Asch, P. Walking Endurance and Perceived Symptom Severity after a Single Maximal Exercise Test in Persons with Mild Disability Because of Multiple Sclerosis. Int. J. Rehabil. Res. 2018, 41, 316–322. [Google Scholar] [CrossRef]
- Scalzitti, D.A.; Harwood, K.J.; Maring, J.R.; Leach, S.J.; Ruckert, E.A.; Costello, E. Validation of the 2-Minute Walk Test with the 6-Minute Walk Test and Other Functional Measures in Persons with Multiple Sclerosis. Int. J. MS Care 2018, 20, 158–163. [Google Scholar] [CrossRef]
- Backus, D. Increasing Physical Activity and Participation in People With Multiple Sclerosis: A Review. Arch. Phys. Med. Rehabil. 2016, 97, S210–S217. [Google Scholar] [CrossRef]
- Chung, L.H.; Angelo, J.; van Emmerik, R.E.A.; Kent, J.A. Energy Cost of Walking, Symptomatic Fatigue and Perceived Exertion in Persons with Multiple Sclerosis. Gait Posture 2016, 48, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Hak, L.; Houdijk, H.; Beek, P.J.; Dieën, J.H. van Steps to Take to Enhance Gait Stability: The Effect of Stride Frequency, Stride Length, and Walking Speed on Local Dynamic Stability and Margins of Stability. PLoS ONE 2013, 8, e82842. [Google Scholar] [CrossRef]
- Beauchet, O.; Allali, G.; Annweiler, C.; Bridenbaugh, S.; Assal, F.; Kressig, R.W.; Herrmann, F.R. Gait Variability among Healthy Adults: Low and High Stride-to-Stride Variability Are Both a Reflection of Gait Stability. Gerontology 2009, 55, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Socie, M.J.; Motl, R.W.; Sosnoff, J.J. Examination of Spatiotemporal Gait Parameters during the 6-Min Walk in Individuals with Multiple Sclerosis. Int. J. Rehabil. Res. 2014, 37, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Alexander, S.; Peryer, G.; Gray, E.; Barkhof, F.; Chataway, J. Wearable Technologies to Measure Clinical Outcomes in Multiple Sclerosis: A Scoping Review. Mult. Scler. 2021, 27, 1643–1656. [Google Scholar] [CrossRef]
- Lecat, M.; Decavel, P.; Magnin, E.; Lucas, B.; Gremeaux, V.; Sagawa, Y. Multiple Sclerosis and Clinical Gait Analysis before and after Fampridine: A Systematic Review. Eur. Neurol. 2017, 78, 272–286. [Google Scholar] [CrossRef]
- Deboeck, G.; Niset, G.; Vachiery, J.-L.; Moraine, J.-J.; Naeije, R. Physiological Response to the Six-Minute Walk Test in Pulmonary Arterial Hypertension. Eur. Respir. J. 2005, 26, 667–672. [Google Scholar] [CrossRef]
- Ibrahim, A.A.; Flachenecker, F.; Gaßner, H.; Rothhammer, V.; Klucken, J.; Eskofier, B.M.; Kluge, F. Short Inertial Sensor-Based Gait Tests Reflect Perceived State Fatigue in Multiple Sclerosis. Mult. Scler. Relat. Disord. 2022, 58, 103519. [Google Scholar] [CrossRef]
| PwMS (n = 45) | Healthy (n = 24) | p | |
|---|---|---|---|
| Gender (female/male; %) | 26/19; 58/42 | 14/10; 58/42 | 0.812 |
| Age (years) a | 51.4 (12.3) | 51.3 (10.7) | 0.22 |
| Body mass (kg) a | 75.5 (18.3) | 75.2 (13.7) | 0.54 |
| Body height (m) a | 1.7 (0.08) | 1.7 (0.08) | 0.78 |
| BMI (kg·m−2) a | 26.2 (5.5) | 26.1 (3.9) | 0.27 |
| Tobacco exposition (yes/no; %) | 11/34; 32/68 | 5/19; 21/79 | 0.64 |
| Alcohol exposition (yes/no; %) | 4/41; 10/90 | 0/24; 0/100 | 0.09 |
| EDSS (4–6.5) b | 4.5 [4;5] | NA | NA |
| Disease duration (years) a | 17.4 (8.9) | NA | NA |
| MS phenotype (n/%) | NA | NA | |
| Relapsing-remitting | 11/24 | NA | NA |
| Secondary progressive | 20/45 | NA | NA |
| Primary progressive | 14/31 | NA | NA |
| EDSS per MS phenotype b | |||
| Relapsing-remitting | 4 [4;4.125] | NA | NA |
| Secondary progressive | 4.5 [4;5] | NA | NA |
| Primary progressive | 5 [4;5.75] | NA | NA |
| Disease duration per MS phenotype b | |||
| Relapsing-remitting | 13 [9;16] | NA | NA |
| Secondary progressive | 19 [13.75;23] | NA | NA |
| Primary progressive | 15 [8.75;20] | NA | NA |
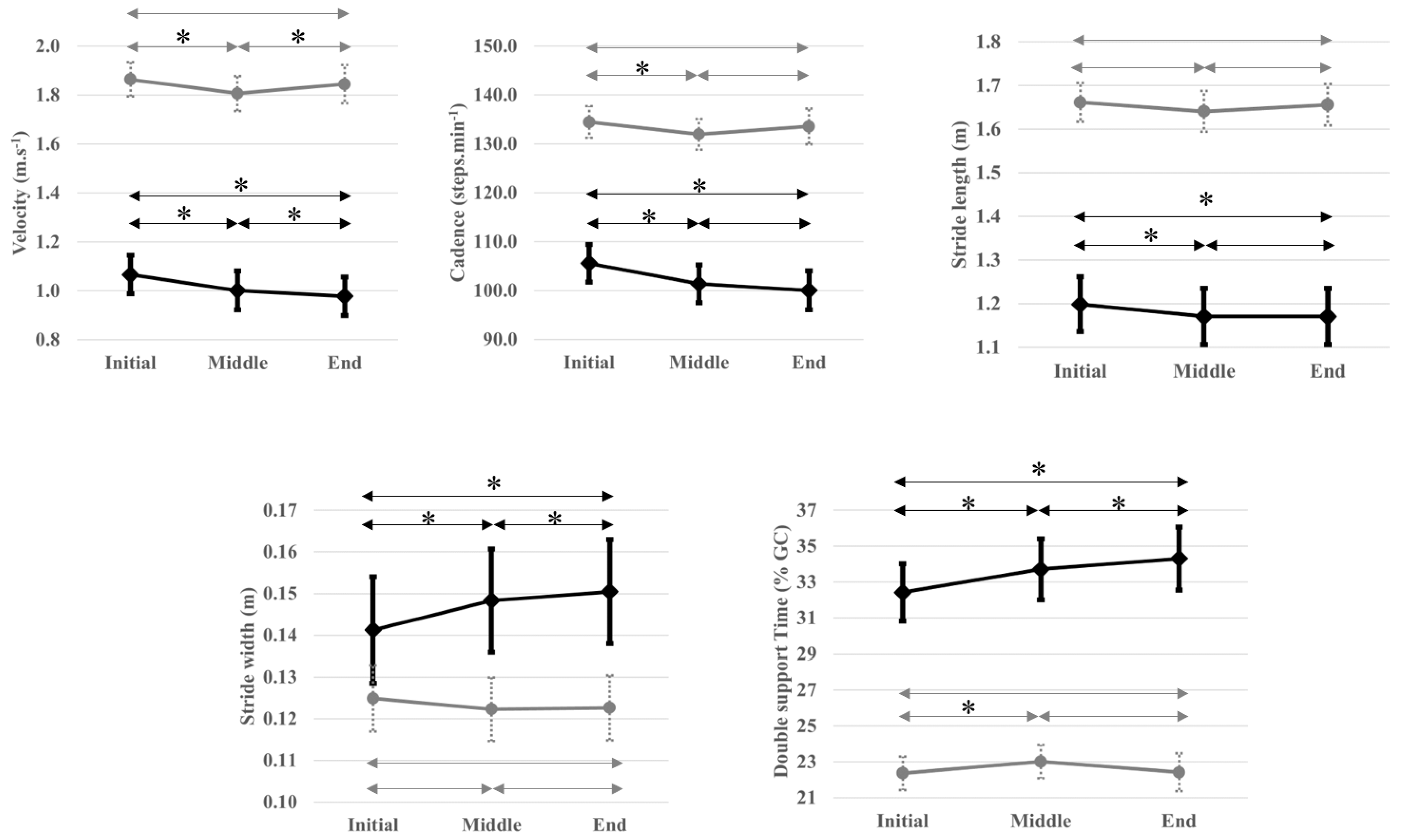
| PwMS (n = 45) | Healthy (n = 24) | |||||
|---|---|---|---|---|---|---|
| 6MWT Intervals | ||||||
| Variables | Initial | Middle | Final | Initial | Middle | Final |
| Velocity (m·s−1) a | 1.07 (0.27) | 1.00 (0.27) | 0.98 (0.27) | 1.88 (0.22) | 1.82 (0.22) | 1.86 (0.25) |
| Cadence (step·min−1) a | 105.57 (13.17) | 101.38 (13.23) | 100.03 (13.51) | 134.55 (8.90) | 132.16 (9.00) | 133.81 (10.82) |
| Stride length (m) a | 1.20 (0.21) | 1.17 (0.22) | 1.17 (0.22) | 1.67 (0.13) | 1.65 (0.14) | 1.66 (0.14) |
| Stride width (m) a | 0.14 (0.04) | 0.15 (0.04) | 0.15 (0.04) | 0.13 (0.02) | 0.12 (0.02) | 0.12 (0.02) |
| Double support time (% GC) a | 32.42 (5.49) | 33.71 (5.83) | 34.31 (5.99) | 22.68 (2.67) | 23.42 (2.74) | 22.70 (3.24) |
| Borg scale (6; 20) b | 10 [9; 11] | 12 [10; 13] | 13 [12; 15] | 9 [6; 10] | 9 [8; 10] | 9 [8; 10] |
| 6MWT distance (m) a | 358 (99) | 655 (75) | ||||
| PwMS (n = 45) | Healthy (n = 24) | |||
|---|---|---|---|---|
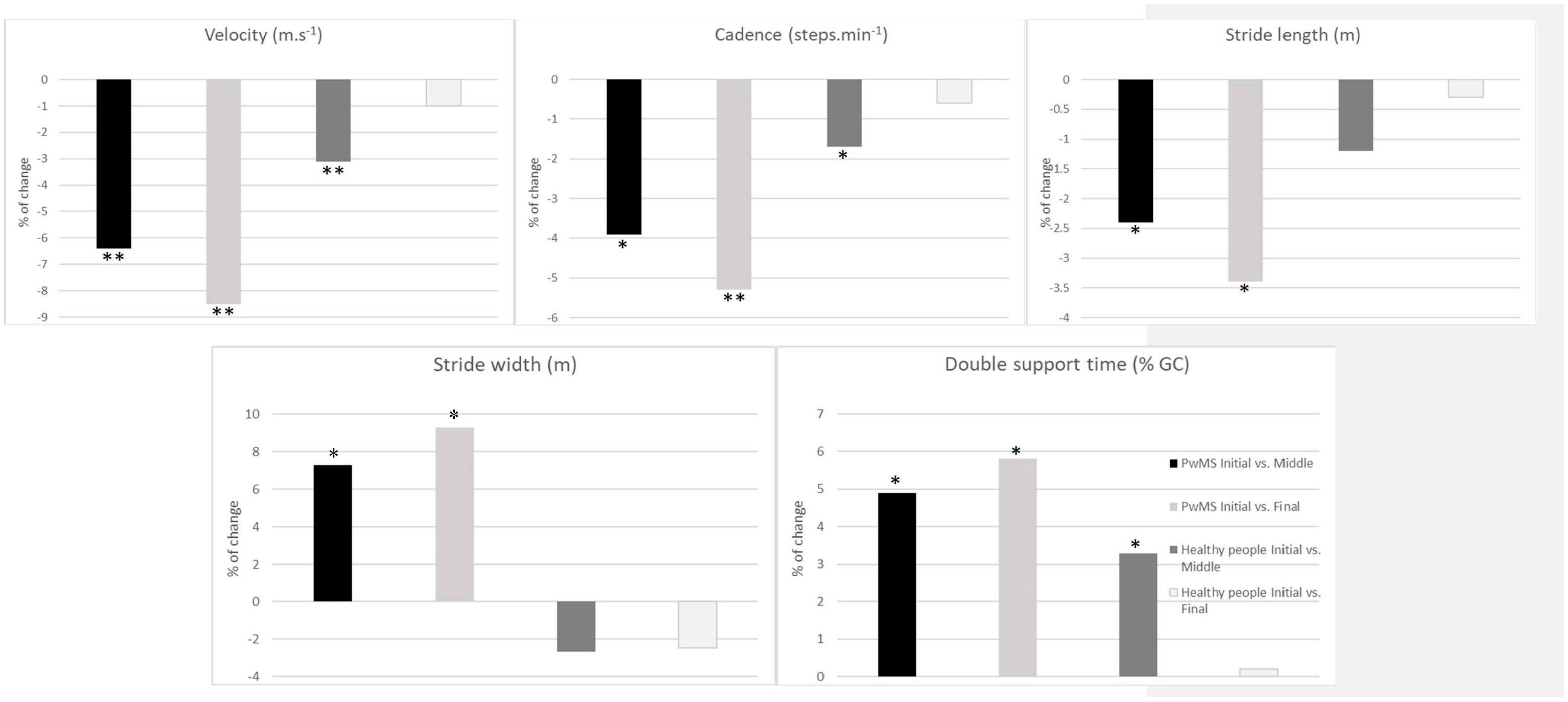
| ST Variables a | Middle/Initial | Final/Initial | Middle/Initial | Final/Initial |
| Velocity | −6.4 (5.5) ** | −8.5 (7.7) ** | −3.1 (3.3) ** † | −1.0 (5.0) ‡ |
| Cadence | −3.9 (3.4) * | −5.3 (4.6) ** | −1.7 (1.8) * ‡ | −0.6 (3.1) ‡ |
| Stride length | −2.4 (3.3) * | −3.4 (4.5) * | −1.2 (2.1) | −0.3 (3.6) ‡ |
| Stride width | 7.3 (14.5) * | 9.3 (18.8) * | −2.7 (6.8) | −2.5 (10) ‡ |
| Double support | 4.0 (3.9) * | 5.8 (4.9) * | 3.3 (3.6) * ‡ | 0.2 (6.8) † |
| SEM (%) | ||||
| Velocity | 9.3 | 7.1 | 6.6 | 7.1 |
| Cadence | 4.4 | 4.8 | 4.1 | 4.5 |
| Stride length | 2.5 | 2.6 | 2.9 | 3.5 |
| Stride width | 9.1 | 8.4 | 6.3 | 7.3 |
| Double support | 4.9 | 5.1 | 3.9 | 6.2 |
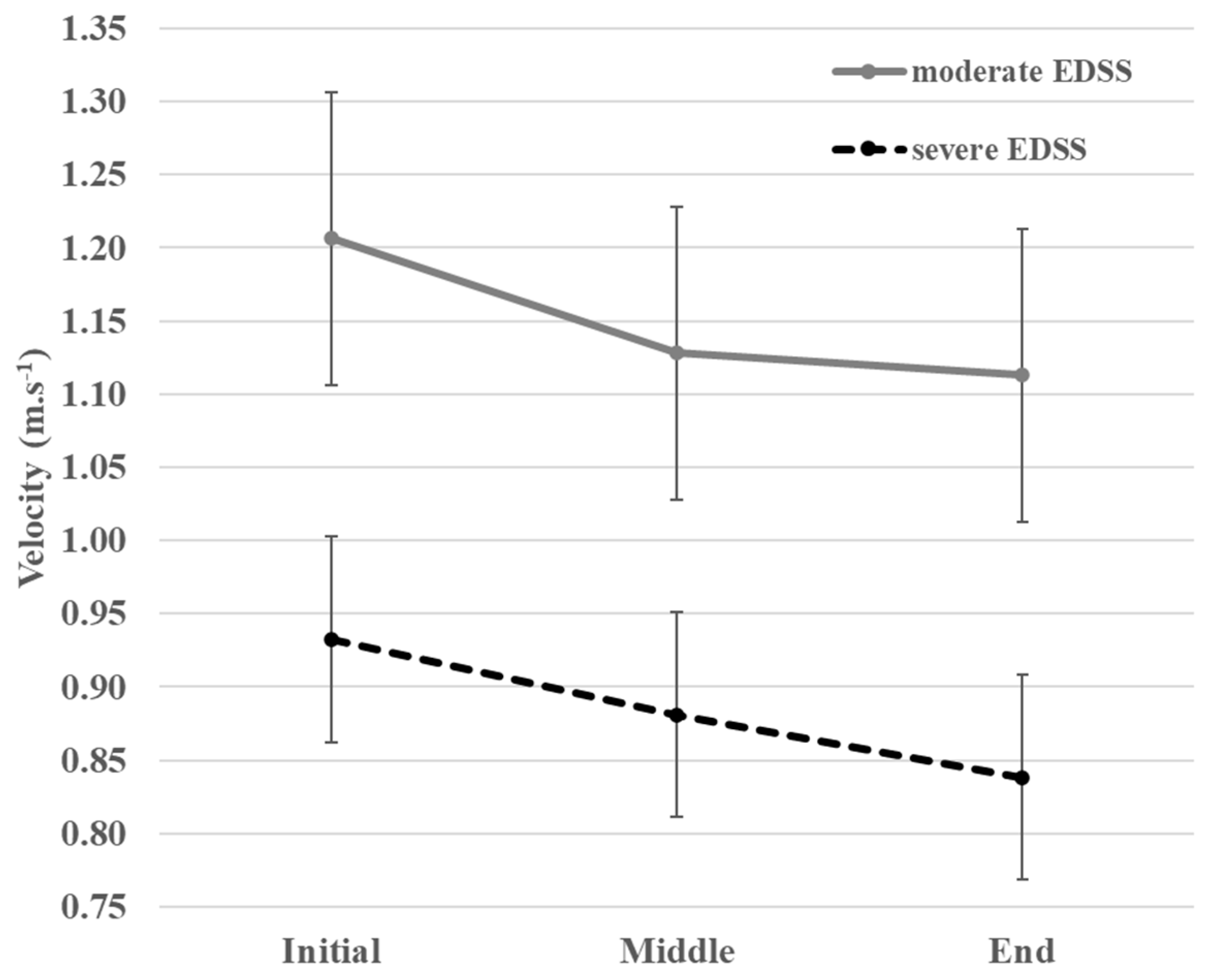
| Moderate EDSS [4] (n = 22) | Severe EDSS [4.5–6.5] (n = 23) | ||||||
|---|---|---|---|---|---|---|---|
| 6MWT Interval | |||||||
| ST Variables | Initial | Middle | End | ST Variables | Initial | Middle | End |
| Velocity (m·s−1) | 1.21 (0.24) | 1.13 (0.24) | 1.11 (0.24) | Velocity (m·s−1) | 0.93 (0.23) | 0.88 (0.23) | 0.84 (0.23) |
| Cadence (step·min−1) | 111.32 (10.52) | 107.93 (9.48) | 106.36 (9.88) | Cadence (step·min−1) | 100.06 (13.27) | 95.11 (13.42) | 91.97 (13.90) |
| Stride length (m) | 1.29 (0.20) | 1.27 (0.21) | 1.25 (0.21) | Stride length (m) | 1.11 (0.19) | 1.06 (0.19) | 1.02 (0.19) |
| Stride width (m) | 0.14 (0.04) | 0.15 (0.04) | 0.15 (0.04) | Stride width (m) | 0.14 (0.05) | 0.15 (0.04) | 0.15 (0.04) |
| Double support time (% GC) | 31 (4.18) | 32 (4.21) | 32 (4.62) | Double support time (% GC) | 34 (6.16) | 36 (6.55) | 37 (6.68) |
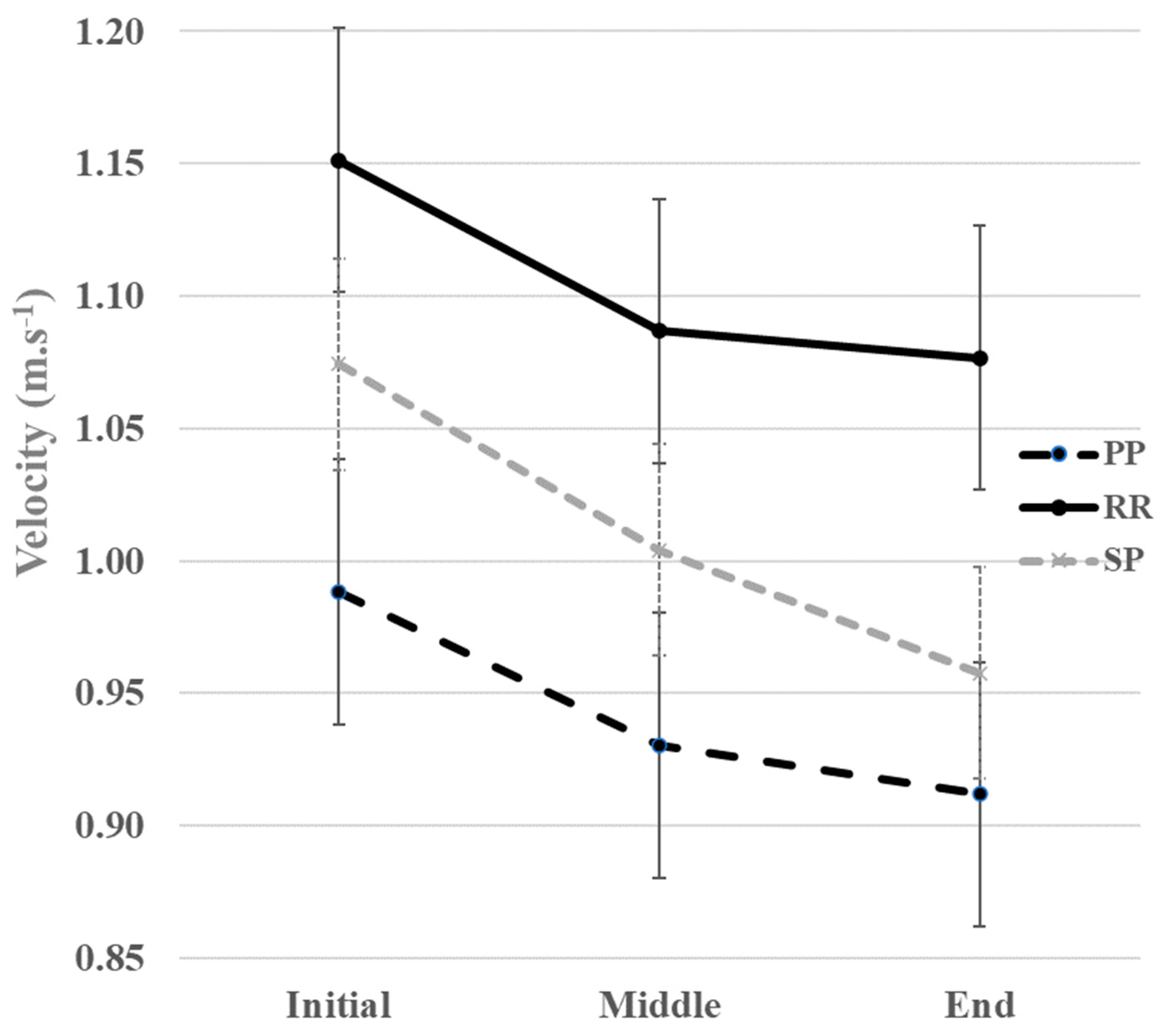
| PwMS with PP Phenotype (n = 14) | PwMS with RR Phenotype (n = 11) | PwMS with SP Phenotype (n = 20) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 6MWT Intervals | |||||||||
| ST Variables | Initial | Middle | End | Initial | Middle | End | Initial | Middle | End |
| Velocity (m·s−1) | 0.98 (0.31) | 0.93 (0.32) | 0.91 (0.31) | 1.15 (0.22) | 1.09 (0.25) | 1.08 (0.20) | 1.07 (0.26) | 1.00 (0.25) | 0.96 (0.27) |
| Cadence (step·min−1) | 101.98 (15.16) | 97.66 (15.49) | 96.61 (15.46) | 109.63 (7.00) | 105.78 (6.88) | 104.30 (7.02) | 105.83 (14.12) | 101.55 (13.96) | 98.06 (14.62) |
| Stride length (m) | 1.14 (0.27) | 1.12 (0.27) | 1.11 (0.28) | 1.25 (0.20) | 1.22 (0.23) | 1.21 (0.20) | 1.21 (0.17) | 1.17 (0.18) | 1.14 (0.19) |
| Stride width (m) | 0.14 (0.03) | 0.15 (0.04) | 0.15 (0.04) | 0.12 (0.03) | 0.13 (0.03) | 0.14 (0.03) | 0.14 (0.06) | 0.15 (0.05) | 0.15 (0.05) |
| Double support time (% GC) | 35 (7.31) | 36 (7.91) | 37 (7.85) | 32 (4.27) | 33 (4.40) | 34 (4.44) | 31 (4.07) | 32 (4.25) | 32 (4.72) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hadouiri, N.; Monnet, E.; Gouelle, A.; Sagawa, Y., Jr.; Decavel, P. Locomotor Strategy to Perform 6-Minute Walk Test in People with Multiple Sclerosis: A Prospective Observational Study. Sensors 2023, 23, 3407. https://doi.org/10.3390/s23073407
Hadouiri N, Monnet E, Gouelle A, Sagawa Y Jr., Decavel P. Locomotor Strategy to Perform 6-Minute Walk Test in People with Multiple Sclerosis: A Prospective Observational Study. Sensors. 2023; 23(7):3407. https://doi.org/10.3390/s23073407
Chicago/Turabian StyleHadouiri, Nawale, Elisabeth Monnet, Arnaud Gouelle, Yoshimasa Sagawa, Jr., and Pierre Decavel. 2023. "Locomotor Strategy to Perform 6-Minute Walk Test in People with Multiple Sclerosis: A Prospective Observational Study" Sensors 23, no. 7: 3407. https://doi.org/10.3390/s23073407
APA StyleHadouiri, N., Monnet, E., Gouelle, A., Sagawa, Y., Jr., & Decavel, P. (2023). Locomotor Strategy to Perform 6-Minute Walk Test in People with Multiple Sclerosis: A Prospective Observational Study. Sensors, 23(7), 3407. https://doi.org/10.3390/s23073407







