Left and Right Cortical Activity Arising from Preferred Walking Speed in Older Adults
Abstract
1. Introduction
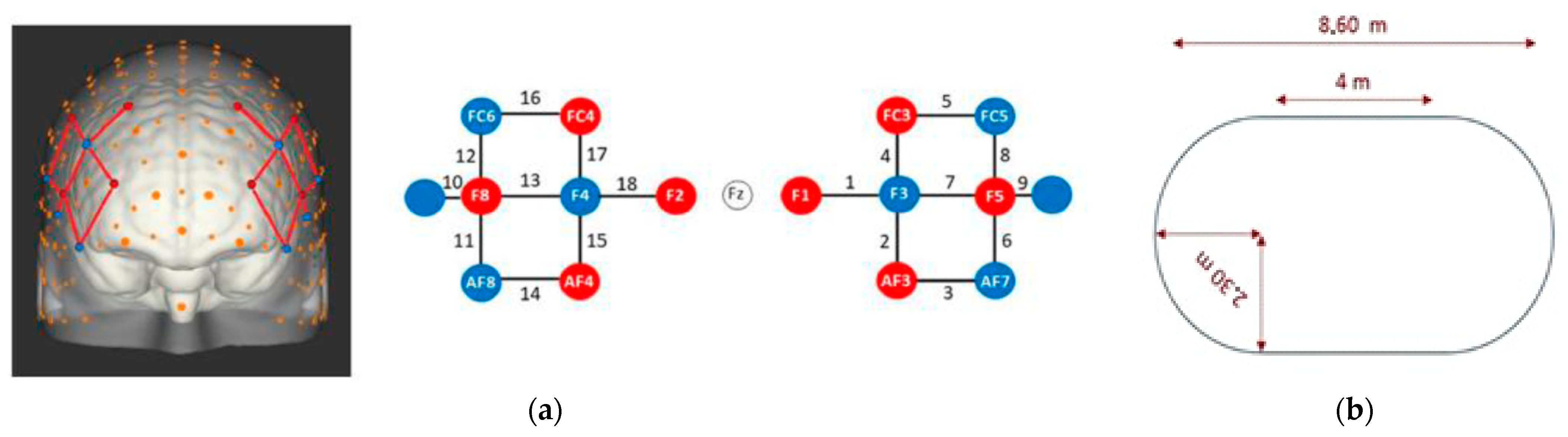
2. Materials and Methods
2.1. Initial Variables and Pre-Processing
2.2. Additional Variables
2.3. Complete List of Variables
2.4. Definition of Two Groups in the Population by K-Means Clustering
2.5. Statistical Methods
3. Results
3.1. Comparisons between Slow and Fast Clusters
3.2. Comparisons between Left and Right Cortical Hemispheres
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Utley, A.; Astill, S. BIOS Instant Notes in Motor Control, Learning and Development; Routledge: London, UK, 2018. [Google Scholar]
- Gage, J.R. An Overview of Normal Walking. Instr. Course Lect. 1990, 39, 291–303. [Google Scholar]
- Krebs, D.E.; Robbins, C.E.; Lavine, L.; Mann, R.W. Hip Biomechanics during Gait. J. Orthop. Sports Phys. Ther. 1998, 28, 51–59. [Google Scholar] [CrossRef]
- Zajac, F.E. Understanding Muscle Coordination of the Human Leg with Dynamical Simulations. J. Biomech. 2002, 35, 1011–1018. [Google Scholar] [CrossRef] [PubMed]
- Callisaya, M.L.; Blizzard, L.; Schmidt, M.D.; Martin, K.L.; McGinley, J.L.; Sanders, L.M.; Srikanth, V.K. Gait, Gait Variability and the Risk of Multiple Incident Falls in Older People: A Population-Based Study. Age Ageing 2011, 40, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Kwon, M.-S.; Kwon, Y.-R.; Park, Y.-S.; Kim, J.-W. Comparison of Gait Patterns in Elderly Fallers and Non-Fallers. Technol. Health Care 2018, 26, 427–436. [Google Scholar] [CrossRef]
- Purves, D.; Augustine, G.-J.; Fitzpatrick, D.; Hall, W.-C. Neurosciences, 3rd ed.; De Boeck: Paris, France, 2005. [Google Scholar]
- Yogev-Seligmann, G.; Hausdorff, J.M.; Giladi, N. The Role of Executive Function and Attention in Gait. Mov. Disord. 2008, 23, 329–342. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, N.; Mori, T.; Suzukamo, Y.; Tanaka, N.; Izumi, S.-I. Parallel Processing of Cognitive and Physical Demands in Left and Right Prefrontal Cortices during Smartphone Use While Walking. BMC Neurosci. 2016, 17, 9. [Google Scholar] [CrossRef]
- Hoang, I.; Ranchet, M.; Derollepot, R.; Moreau, F.; Paire-Ficout, L. Measuring the Cognitive Workload during Dual-Task Walking in Young Adults: A Combination of Neurophysiological and Subjective Measures. Front. Hum. Neurosci. 2020, 14, 592532. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Andrews, A.W.; Thomas, M.W. Walking Speed: Reference Values and Correlates for Older Adults. J. Orthop. Sports Phys. Ther. 1996, 24, 86–90. [Google Scholar] [CrossRef]
- Feltner, M.E.; MacRae, P.G.; McNitt-Gray, J.L. Quantitative Gait Assessment as a Predictor of Prospective and Retrospective Falls in Community-Dwelling Older Women. Arch. Phys. Med. Rehabil. 1994, 75, 447–453. [Google Scholar] [CrossRef]
- Judge, J.O.; Davis, R.B.; Ounpuu, S. Step Length Reductions in Advanced Age: The Role of Ankle and Hip Kinetics. J. Gerontol. A Biol. Sci. Med. Sci. 1996, 51, M303–M312. [Google Scholar] [CrossRef] [PubMed]
- König, N.; Taylor, W.R.; Armbrecht, G.; Dietzel, R.; Singh, N.B. Identification of Functional Parameters for the Classification of Older Female Fallers and Prediction of “first-Time” Fallers. J. R. Soc. Interface 2014, 11, 20140353. [Google Scholar] [CrossRef] [PubMed]
- Menant, J.C.; Schoene, D.; Sarofim, M.; Lord, S.R. Single and Dual Task Tests of Gait Speed Are Equivalent in the Prediction of Falls in Older People: A Systematic Review and Meta-Analysis. Ageing Res. Rev. 2014, 16, 83–104. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Schapira, M.; Soriano, E.R.; Varela, M.; Kaplan, R.; Camera, L.A.; Mayorga, L.M. Gait Velocity as a Single Predictor of Adverse Events in Healthy Seniors Aged 75 Years and Older. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 1304–1309. [Google Scholar] [CrossRef] [PubMed]
- Mortaza, N.; Abu Osman, N.A.; Mehdikhani, N. Are the Spatio-Temporal Parameters of Gait Capable of Distinguishing a Faller from a Non-Faller Elderly? Eur. J. Phys. Rehabil. Med. 2014, 50, 677–691. [Google Scholar]
- Verghese, J.; Holtzer, R.; Lipton, R.B.; Wang, C. Quantitative Gait Markers and Incident Fall Risk in Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 896–901. [Google Scholar] [CrossRef]
- Verghese, J.; Wang, C.; Ayers, E.; Izzetoglu, M.; Holtzer, R. Brain Activation in High-Functioning Older Adults and Falls: Prospective Cohort Study. Neurology 2017, 88, 191–197. [Google Scholar] [CrossRef]
- Ranchet, M.; Hoang, I.; Cheminon, M.; Derollepot, R.; Devos, H.; Perrey, S.; Luauté, J.; Danaila, T.; Paire-Ficout, L. Changes in Prefrontal Cortical Activity during Walking and Cognitive Functions Among Patients with Parkinson’s Disease. Front. Neurol. 2020, 11, 601686. [Google Scholar] [CrossRef]
- Perrey, S. Possibilities for Examining the Neural Control of Gait in Humans with FNIRS. Front. Physiol. 2014, 5, 204. [Google Scholar] [CrossRef]
- Shaw, E.P.; Rietschel, J.C.; Hendershot, B.D.; Pruziner, A.L.; Miller, M.W.; Hatfield, B.D.; Gentili, R.J. Measurement of Attentional Reserve and Mental Effort for Cognitive Workload Assessment under Various Task Demands during Dual-Task Walking. Biol. Psychol. 2018, 134, 39–51. [Google Scholar] [CrossRef]
- Rubin, E.H.; Storandt, M.; Miller, J.P.; Kinscherf, D.A.; Grant, E.A.; Morris, J.C.; Berg, L.A. Prospective Study of Cognitive Function and Onset of Dementia in Cognitively Healthy Elders. Arch. Neurol. 1998, 55, 395–401. [Google Scholar] [CrossRef] [PubMed]
- De Groot, L.C.P.M.G.; Verheijden, M.W.; De Henauw, S.; Schroll, M.; Van Staveren, W.A.; SENECA Investigators. Lifestyle, Nutritional Status, Health, and Mortality in Elderly People across Europe: A Review of the Longitudinal Results of the SENECA Study. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, 1277–1284. [Google Scholar] [CrossRef] [PubMed]
- Buckner, R.L. Memory and Executive Function in Aging and AD: Multiple Factors That Cause Decline and Reserve Factors That Compensate. Neuron 2004, 44, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Belsky, D.W.; Caspi, A.; Houts, R.; Cohen, H.J.; Corcoran, D.L.; Danese, A.; Harrington, H.; Israel, S.; Levine, M.E.; Schaefer, J.D.; et al. Quantification of Biological Aging in Young Adults. Proc. Natl. Acad. Sci. USA 2015, 112, E4104–E4110. [Google Scholar] [CrossRef]
- Ahadi, S.; Zhou, W.; Schüssler-Fiorenza Rose, S.M.; Sailani, M.R.; Contrepois, K.; Avina, M.; Ashland, M.; Brunet, A.; Snyder, M. Personal Aging Markers and Ageotypes Revealed by Deep Longitudinal Profiling. Nat. Med. 2020, 26, 83–90. [Google Scholar] [CrossRef]
- Vitorio, R.; Stuart, S.; Rochester, L.; Alcock, L.; Pantall, A. FNIRS Response during Walking—Artefact or Cortical Activity? A Systematic Review. Neurosci. Biobehav. Rev. 2017, 83, 160–172. [Google Scholar] [CrossRef]
- Pelicioni, P.H.S.; Lord, S.R.; Sturnieks, D.L.; Halmy, B.; Menant, J.C. Cognitive and Motor Cortical Activity during Cognitively Demanding Stepping Tasks in Older People at Low and High Risk of Falling. Front. Med. 2021, 8, 554231. [Google Scholar] [CrossRef]
- De Belli, V.; Orcioli-Silva, D.; Beretta, V.S.; Vitório, R.; Zampier, V.C.; Nóbrega-Sousa, P.; Conceição, N.R.D.A.; Gobbi, L.T.B. Prefrontal Cortical Activity during Preferred and Fast Walking in Young and Older Adults: An FNIRS Study. Neuroscience 2021, 473, 81–89. [Google Scholar] [CrossRef]
- Harada, T.; Miyai, I.; Suzuki, M.; Kubota, K. Gait Capacity Affects Cortical Activation Patterns Related to Speed Control in the Elderly. Exp. Brain Res. 2009, 193, 445–454. [Google Scholar] [CrossRef]
- Metzger, F.G.; Ehlis, A.-C.; Haeussinger, F.B.; Schneeweiss, P.; Hudak, J.; Fallgatter, A.J.; Schneider, S. Functional Brain Imaging of Walking While Talking—An FNIRS Study. Neuroscience 2017, 343, 85–93. [Google Scholar] [CrossRef]
- Suzuki, M.; Miyai, I.; Ono, T.; Oda, I.; Konishi, I.; Kochiyama, T.; Kubota, K. Prefrontal and Premotor Cortices Are Involved in Adapting Walking and Running Speed on the Treadmill: An Optical Imaging Study. NeuroImage 2004, 23, 1020–1026. [Google Scholar] [CrossRef] [PubMed]
- Meester, D.; Al-Yahya, E.; Dawes, H.; Martin-Fagg, P.; Piñon, C. Associations between Prefrontal Cortex Activation and H-Reflex Modulation during Dual Task Gait. Front. Hum. Neurosci. 2014, 8, 78. [Google Scholar] [CrossRef] [PubMed]
- Udina, C.; Avtzi, S.; Durduran, T.; Holtzer, R.; Rosso, A.L.; Castellano-Tejedor, C.; Perez, L.-M.; Soto-Bagaria, L.; Inzitari, M. Functional Near-Infrared Spectroscopy to Study Cerebral Hemodynamics in Older Adults during Cognitive and Motor Tasks: A Review. Front. Aging Neurosci. 2019, 11, 367. [Google Scholar] [CrossRef] [PubMed]
- Herold, F.; Wiegel, P.; Scholkmann, F.; Thiers, A.; Hamacher, D.; Schega, L. Functional Near-Infrared Spectroscopy in Movement Science: A Systematic Review on Cortical Activity in Postural and Walking Tasks. Neurophotonics 2017, 4, 041403. [Google Scholar] [CrossRef]
- Scholkmann, F.; Kleiser, S.; Metz, A.J.; Zimmermann, R.; Mata Pavia, J.; Wolf, U.; Wolf, M. A Review on Continuous Wave Functional Near-Infrared Spectroscopy and Imaging Instrumentation and Methodology. Neuroimage 2014, 85 Pt 1, 6–27. [Google Scholar] [CrossRef]
- Menant, J.C.; Maidan, I.; Alcock, L.; Al-Yahya, E.; Cerasa, A.; Clark, D.J.; de Bruin, E.D.; Fraser, S.; Gramigna, V.; Hamacher, D.; et al. A Consensus Guide to Using Functional Near-Infrared Spectroscopy in Posture and Gait Research. Gait Posture 2020, 82, 254–265. [Google Scholar] [CrossRef]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and Initial Validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Lord, S.R.; Sambrook, P.N.; Gilbert, C.; Kelly, P.J.; Nguyen, T.; Webster, I.W.; Eisman, J.A. Postural Stability, Falls and Fractures in the Elderly: Results from the Dubbo Osteoporosis Epidemiology Study. Med. J. Aust. 1994, 160, 684–685, 688–691. [Google Scholar] [CrossRef]
- Lord, S.R.; Menz, H.B.; Tiedemann, A. A Physiological Profile Approach to Falls Risk Assessment and Prevention. Phys. Ther. 2003, 83, 237–252. [Google Scholar] [CrossRef]
- Phan, T.C.; Pranata, A.; Farragher, J.; Bryant, A.; Nguyen, H.T.; Chai, R. Machine Learning Derived Lifting Techniques and Pain Self-Efficacy in People with Chronic Low Back Pain. Sensors 2022, 22, 6694. [Google Scholar] [CrossRef]
- Stuart, S.; Vitorio, R.; Morris, R.; Martini, D.N.; Fino, P.C.; Mancini, M. Cortical activity during walking and balance tasks in older adults and in people with Parkinson’s disease: A structured review. Maturitas 2018, 113, 53–72. [Google Scholar] [CrossRef] [PubMed]
- Hoang, I.; Paire-Ficout, L.; Derollepot, R.; Perrey, S.; Devos, H.; Ranchet, M. Increased Prefrontal Activity during Usual Walking in Aging. Int. J. Psychophysiol. 2022, 174, 9–16. [Google Scholar] [CrossRef]
- Fukuchi, C.A.; Fukuchi, R.K.; Duarte, M. Effects of Walking Speed on Gait Biomechanics in Healthy Participants: A Systematic Review and Meta-Analysis. Syst. Rev. 2019, 8, 153. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.-T.; Yoshida, Y.; Hortobágyi, T.; Suzuki, S. Interaction between Thorax, Lumbar, and Pelvis Movements in the Transverse Plane during Gait at Three Velocities. J. Appl. Biomech. 2013, 29, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Ma, Y.; Hou, B.Y.; Lam, W.-K. Influence of Gait Speeds on Contact Forces of Lower Limbs. J. Healthc. Eng. 2017, 2017, 6375976. [Google Scholar] [CrossRef] [PubMed]
- Winiarski, S.; Pietraszewska, J.; Pietraszewski, B. Three-Dimensional Human Gait Pattern: Reference Data for Young, Active Women Walking with Low, Preferred, and High Speeds. Biomed. Res. Int. 2019, 2019, 9232430. [Google Scholar] [CrossRef] [PubMed]
- James, E.G.; Conatser, P.; Karabulut, M.; Leveille, S.G.; Hausdorff, J.M.; Travison, T.; Bean, J.F. Walking Speed Affects Gait Coordination and Variability Among Older Adults with and without Mobility Limitations. Arch. Phys. Med. Rehabil. 2020, 101, 1377–1382. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Kramer, P.A. Walking Speed Alters Barefoot Gait Coordination and Variability. J. Mot. Behav. 2022, 54, 410–421. [Google Scholar] [CrossRef]
- Hausdorff, J.M. Gait Variability: Methods, Modeling and Meaning. J. Neuroeng. Rehabil. 2005, 2, 19. [Google Scholar] [CrossRef]
- Prieto, T.E.; Myklebust, J.B.; Hoffmann, R.G.; Lovett, E.G.; Myklebust, B.M. Measures of Postural Steadiness: Differences between Healthy Young and Elderly Adults. IEEE Trans. Biomed. Eng. 1996, 43, 956–966. [Google Scholar] [CrossRef]
- Khanmohammadi, R.; Talebian, S.; Hadian, M.R.; Olyaei, G.; Bagheri, H. Preparatory Postural Adjustments during Gait Initiation in Healthy Younger and Older Adults: Neurophysiological and Biomechanical Aspects. Brain Res. 2015, 1629, 240–249. [Google Scholar] [CrossRef] [PubMed]
- Michalska, J.; Kamieniarz, A.; Sobota, G.; Stania, M.; Juras, G.; Słomka, K.J. Age-Related Changes in Postural Control in Older Women: Transitional Tasks in Step Initiation. BMC Geriatr. 2021, 21, 17. [Google Scholar] [CrossRef] [PubMed]
- Bauer, C.; Gröger, I.; Glabasnia, A.; Bergler, C.; Gassmann, K.G. First Results of Evaluation of a Falls Clinic. Int. J. Gerontol. 2010, 4, 130–136. [Google Scholar] [CrossRef]
- Roche, N.; Chorin, F.; Gerus, P.; Deshayes, M.; Guerin, O.; Zory, R. Effects of Age, Gender, Frailty and Falls on Spatiotemporal Gait Parameters: A Retrospective Cohort Study. Eur. J. Phys. Rehabil. Med. 2021, 57, 923–930. [Google Scholar] [CrossRef]
- Jung, H.-W.; Jang, I.-Y.; Lee, C.K.; Yu, S.S.; Hwang, J.K.; Jeon, C.; Lee, Y.S.; Lee, E. Usual Gait Speed Is Associated with Frailty Status, Institutionalization, and Mortality in Community-Dwelling Rural Older Adults: A Longitudinal Analysis of the Aging Study of Pyeongchang Rural Area. Clin. Interv. Aging 2018, 13, 1079–1089. [Google Scholar] [CrossRef] [PubMed]
- Yamasaki, M.; Sasaki, T.; Torii, M. Sex Difference in the Pattern of Lower Limb Movement during Treadmill Walking. Eur. J. Appl. Physiol. 1991, 62, 99–103. [Google Scholar] [CrossRef]
- Dingwell, J.B.; Marin, L.C. Kinematic Variability and Local Dynamic Stability of Upper Body Motions When Walking at Different Speeds. J. Biomech. 2006, 39, 444–452. [Google Scholar] [CrossRef]
- Kang, H.G.; Dingwell, J.B. Separating the Effects of Age and Walking Speed on Gait Variability. Gait Posture 2008, 27, 572–577. [Google Scholar] [CrossRef]
- Clark, D.J. Automaticity of Walking: Functional Significance, Mechanisms, Measurement and Rehabilitation Strategies. Front. Hum. Neurosci. 2015, 9, 246. [Google Scholar] [CrossRef]
- Kang, W.; Wang, J.; Malvaso, A. Inhibitory Control in Aging: The Compensation-Related Utilization of Neural Circuits Hypothesis. Front. Aging Neurosci. 2021, 13, 771885. [Google Scholar] [CrossRef] [PubMed]
- Mirelman, A.; Maidan, I.; Bernad-Elazari, H.; Shustack, S.; Giladi, N.; Hausdorff, J.M. Effects of Aging on Prefrontal Brain Activation during Challenging Walking Conditions. Brain Cognit. 2017, 115, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, P.C.; Musicha, C.; Rowlands, A.V.; Davies, M.; Khunti, K.; Razieh, C.; Timmins, I.; Zaccardi, F.; Codd, V.; Nelson, C.P.; et al. Investigation of a UK Biobank Cohort Reveals Causal Associations of Self-Reported Walking Pace with Telomere Length. Commun. Biol. 2022, 5, 381. [Google Scholar] [CrossRef] [PubMed]
- Cabeza, R. Hemispheric Asymmetry Reduction in Older Adults: The HAROLD Model. Psychol. Aging 2002, 17, 85–100. [Google Scholar] [CrossRef]
- Weerdesteyn, V.; Rijken, H.; Geurts, A.C.H.; Smits-Engelsman, B.C.M.; Mulder, T.; Duysens, J. A Five-Week Exercise Program Can Reduce Falls and Improve Obstacle Avoidance in the Elderly. Gerontology 2006, 52, 131–141. [Google Scholar] [CrossRef]
- Kim, H.-D.; Brunt, D. The Effect of a Dual-Task on Obstacle Crossing in Healthy Elderly and Young Adults. Arch. Phys. Med. Rehabil. 2007, 88, 1309–1313. [Google Scholar] [CrossRef] [PubMed]
- Belluscio, V.; Casti, G.; Ferrari, M.; Quaresima, V.; Sappia, M.S.; Horschig, J.M.; Vannozzi, G. Modifications in Prefrontal Cortex Oxygenation in Linear and Curvilinear Dual Task Walking: A Combined FNIRS and IMUs Study. Sensors 2021, 21, 6159. [Google Scholar] [CrossRef]
- Hamacher, D.; Herold, F.; Wiegel, P.; Hamacher, D.; Schega, L. Brain activity during walking: A systematic review. Neurosci. Biobehav. Rev. 2015, 57, 310–327. [Google Scholar] [CrossRef]
- Haier, R.J.; Siegel, B.V.; Nuechterlein, K.H.; Hazlett, E.; Wu, J.C.; Paek, J.; Browning, H.L.; Buchsbaum, M.S. Cortical Glucose Metabolic Rate Correlates of Abstract Reasoning and Attention Studied with Positron Emission Tomography. Intelligence 1988, 12, 199–217. [Google Scholar] [CrossRef]
- Ludyga, S.; Gronwald, T.; Hottenrott, K. Effects of High vs. Low Cadence Training on Cyclists’ Brain Cortical Activity during Exercise. J. Sci. Med. Sport 2016, 19, 342–347. [Google Scholar] [CrossRef]
- Ludyga, S.; Hottenrott, K.; Gronwald, T. Four Weeks of High Cadence Training Alter Brain Cortical Activity in Cyclists. J. Sports Sci. 2017, 35, 1377–1382. [Google Scholar] [CrossRef] [PubMed]


| Variable Description | HbO | HbR |
|---|---|---|
| the mean value during the first 20 s of the walking trial. | avg_HbO | avg_HbR |
| the minimum or maximum values during the first 20 s of the walking trial. | max_HbO | min_HbR |
| time of the minimum or maximum values during the first 20 s of the walking trial. | tmax_HbO | tmin_HbR |
| Abbreviation | Definition | Description |
|---|---|---|
| avg_HbT | mean(HbO+HbR) | Average of total haemoglobin during the 20 first seconds of the walking trial. |
| max_HbT | max(HbT) | Maximum value of HbT during the 20 first seconds of the walking trial. |
| tmax_HbT | Time at max(HbT) | The time at which max_HbT occurs |
| diff_Hb | diff_Hb = avg_HbO − avg_HbR | Difference between the average in oxy- and deoxy-haemoglobin as a measure of cortical activation |
| deltaH | deltaH = max_HbO − min_HbR | Maximum difference in oxy- and deoxy-haemoglobin |
| Abbreviation | Description of the Cortical Activation Parameters |
|---|---|
| avg_HbO_l | Mean change in oxyhaemoglobin, left hemisphere |
| avg_HbO_r | Mean change in oxyhaemoglobin, right hemisphere |
| avg_HbR_l | Mean change in deoxyhaemoglobin, left hemisphere |
| avg_HbR_r | Mean change in deoxyhaemoglobin, right hemisphere |
| avg_HbT_l | Mean change in total haemoglobin, left hemisphere |
| avg_HbT_r | Mean change in total haemoglobin, right hemisphere |
| max_HbO_l | Maximum change in oxyhaemoglobin, left hemisphere |
| max_HbO_r | Maximum change in oxyhaemoglobin, right hemisphere |
| max_HbR_l | Maximum change in deoxyhaemoglobin, left hemisphere |
| max_HbR_r | Maximum change in deoxyhaemoglobin, right hemisphere |
| max_HbT_l | Maximum change in total haemoglobin, left hemisphere |
| max_HbT_r | Maximum change in total haemoglobin, right hemisphere |
| diff_Hb_l | Mean difference in oxy and deoxy -haemoglobin as a measure of cortical activation, left hemisphere |
| diff_Hb_r | Mean difference in oxy and deoxy -haemoglobin as a measure of cortical activation, right hemisphere |
| deltaH_l | Maximum difference in oxy and deoxy -haemoglobin, left hemisphere |
| deltaH_r | Maximum difference in oxy and deoxy -haemoglobin, right hemisphere |
| tmax_HbO_l | Time elapsed at maximal change in oxyhaemoglobin, left hemisphere |
| tmax_HbO_r | Time elapsed at maximal change in oxyhaemoglobin, right hemisphere |
| tmax_HbR_l | Time elapsed at maximal change in deoxyhaemoglobin, left hemisphere |
| tmax_HbR_r | Time elapsed at maximal change in deoxyhaemoglobin, right hemisphere |
| tmax_HbT_l | Time elapsed at maximal change in total haemoglobin, left hemisphere |
| tmax_HbT_r | Time elapsed at maximal change in total haemoglobin, right hemisphere |
| Abbreviation | Description of the Gait Parameters |
|---|---|
| avg_gct | Mean gait cycle time, the time from one heel strike to the next heel strike of the ipsilateral foot (stride time) |
| gct_CV | Coefficient of variation for gait cycle time |
| avg_cad | Mean walking cadence |
| cad_CV | Coefficient of variation for walking cadence |
| avg_Slength | Mean stride length, the distance covered over a given stride |
| Slength_CV | Coefficient of variation for stride length, the distance covered over a given stride |
| avg_speed | Mean walking speed |
| speed_CV | Coefficient of variation for walking speed |
| 55–65 Years Old | 67–85 Years Old | Men | Women | Total | |
|---|---|---|---|---|---|
| slow cluster (0.95 m/s) | 14 | 8 | 7 | 15 | 22 |
| fast cluster (1.28 m/s) | 11 | 17 | 12 | 16 | 28 |
| Total | 25 | 25 | 19 | 31 | 50 |
| Variable | Slow Cluster (Mean ± SD) | Fast Cluster (Mean ± SD) | p-Value | Effect Size (Cohen’s d) [Lower CI, Upper CI] |
|---|---|---|---|---|
| Age (years) | 66.18 ± 5.87 | 67.46 ± 7.62 | 0.518 | −0.18 [−0.75, 0.37] |
| FES-I_score | 20.05 ± 3.75 | 19.21 ± 3.11 | 0.340 | 0.24 [−0.32, 0.8] |
| MoCA | 26.82 ± 2.08 | 27.14 ± 1.80 | 0.611 | −0.17 [−0.73, 0.39] |
| Gait parameters | ||||
| avg_gct (s) *** | 1.24 ± 0.14 | 1.07 ± 0.09 | <0.001 | 1.42 [0.82, 2.08] |
| avg_cad (steps/min) *** | 96.27 ± 12.11 | 112.81 ± 9.41 | <0.001 | −1.52 [−2.19, −0.91] |
| avg_Slength (m) *** | 1.16 ± 0.08 | 1.33 ± 0.11 | <0.001 | −1.76 [−2.45, −1.12] |
| avg_speed (m/s) *** | 0.95 ± 0.14 | 1.28 ± 0.10 | <0.001 | −2.68 [−3.50, −1.94] |
| gct_CV (%) | 4.42 ± 3.00 | 3.56 ± 1.53 | 0.054 | 0.37 [−0.19, 0.94] |
| cad_CV (%) * | 4.05 ± 1.65 | 3.49 ± 1.45 | 0.041 | 0.36 [−0.20, 0.93] |
| Slength_CV (%) | 6.65 ± 2.78 | 6.28 ± 1.46 | 0.792 | 0.17 [−0.39, 0.73] |
| speed_CV (%) | 8.08 ± 1.57 | 7.86 ± 1.81 | 0.406 | 0.13 [−0.43, 0.69] |
| Cortical activity parameters | ||||
| avg_HbO_l (µmol/L) ** | 0.056 ± 0.135 | −0.035 ± 0.190 | 0.005 | 0.54 [−0.02, 1.11] |
| avg_HbO_r (µmol/L) | 0.092 ± 0.153 | 0.084 ± 0.168 | 0.854 | 0.05 [−0.51, 0.61] |
| max_HbO_l (µmol/L) | 0.212 ± 0.141 | 0.170 ± 0.221 | 0.087 | 0.22 [−0.34, 0.78] |
| max_HbO_r (µmol/L) | 0.238 ± 0.154 | 0.279 ± 0.211 | 0.632 | −0.21 [−0.78, 0.34] |
| diff_Hb_l (µmol/L) ** | 0.068 ± 0.120 | −0.014 ± 0.238 | 0.003 | 0.42 [−0.14, 0.99] |
| diff_Hb_r (µmol/L) | 0.098 ± 0.160 | 0.079 ± 0.181 | 0.696 | 0.11 [−0.45, 0.67] |
| avg_HbR_l (µmol/L) | −0.012 ± 0.047 | −0.021 ± 0.071 | 0.777 | 0.15 [−0.41, 0.71] |
| avg_HbR_r (µmol/L) | −0.006 ± 0.036 | 0.005 ± 0.060 | 0.462 | −0.21 [−0.77, 0.35] |
| min_HbR_l (µmol/L) | −0.060 ± 0.050 | −0.074 ± 0.083 | 0.792 | 0.19 [−0.36, 0.76] |
| min_HbR_r (µmol/L) | −0.055 ± 0.037 | −0.060 ± 0.070 | 0.732 | 0.07 [−0.48, 0.63] |
| avg_HbT_l (µmol/L) * | 0.045 ± 0.163 | −0.056 ± 0.161 | 0.020 | 0.61 [0.05, 1.20] |
| avg_HbT_r (µmol/L) | 0.086 ± 0.154 | 0.088 ± 0.175 | 0.961 | −0.01 [−0.57, 0.54] |
| max_HbT_l (µmol/L) | 0.211 ± 0.155 | 0.152 ± 0.170 | 0.111 | 0.36 [−0.20, 0.93] |
| max_HbT_r (µmol/L) | 0.232 ± 0.153 | 0.280 ± 0.224 | 0.689 | −0.24 [−0.80, 0.32] |
| deltaH_l (µmol/L) | 0.272 ± 0.148 | 0.244 ± 0.283 | 0.071 | 0.12 [−0.44, 0.68] |
| deltaH_r (µmol/L) | 0.293 ± 0.162 | 0.338 ± 0.236 | 0.689 | −0.21 [−0.78, 0.34] |
| tmax_HbO_l (s) * | 9.47 ± 5.33 | 6.32 ± 3.70 | 0.018 | 0.69 [0.12, 1.28] |
| tmax_HbO_r (s) | 10.38 ± 3.44 | 8.37 ± 3.90 | 0.062 | 0.54 [−0.02, 1.11] |
| tmax_HbT_l (s) | 9.51 ± 5.86 | 6.66 ± 4.25 | 0.052 | 0.56 [0, 1.14] |
| tmax_HbT_r (s) | 10.02 ± 3.96 | 8.54 ± 4.10 | 0.113 | 0.36 [−0.20, 0.93] |
| Variable | LH (Mean ± SD) | RH (Mean ± SD) | LH–RH (Mean ± SD) | p-Value | Effect Size (Cohen’s d) [Lower CI Upper CI] |
|---|---|---|---|---|---|
| Slow cluster | |||||
| avg_HbO (µmol/L) | 0.056 ± 0.135 | 0.092 ± 0.153 | −0.036 ± 0.147 | 0.269 | −0.24 [−0.69, 0.19] |
| max_HbO (µmol/L) | 0.212 ± 0.141 | 0.238 ± 0.154 | −0.025 ± 0.136 | 0.391 | −0.17 [−0.57, 0.22] |
| diff_Hb (µmol/L) | 0.068 ± 0.120 | 0.098 ± 0.160 | −0.030 ± 0.137 | 0.315 | −0.21 [−0.63, 0.21] |
| avg_HbR (µmol/L) | −0.012 ± 0.047 | −0.006 ± 0.036 | −0.006 ± 0.060 | 0.671 | −0.13 [−0.75, 0.48] |
| min_HbR (µmol/L) | −0.060 ± 0.050 | −0.055 ± 0.037 | −0.004 ± 0.057 | 0.935 | −0.13 [−0.75, 0.48] |
| avg_HbT (µmol/L) | 0.045 ± 0.163 | 0.086 ± 0.154 | −0.041 ± 0.178 | 0.291 | −0.25 [−0.74, 0.22] |
| max_HbT (µmol/L) | 0.211 ± 0.155 | 0.232 ± 0.153 | −0.020 ± 0.163 | 0.563 | −0.13 [−0.59, 0.32] |
| deltaH (µmol/L) | 0.272 ± 0.148 | 0.293 ± 0.162 | −0.021 ± 0.124 | 0.438 | −0.13 [−0.48, 0.21] |
| tmax_HbO (s) | 9.47 ± 5.33 | 10.38 ± 3.44 | −0.92 ± 5.50 | 0.443 | −0.20 [−0.73, 0.32] |
| tmax_HbT (s) | 9.51 ± 5.86 | 10.02 ± 3.96 | −0.51 ± 5.91 | 0.689 | −0.10 [−0.61, 0.40] |
| Fast cluster | |||||
| avg_HbO (µmol/L) ** | −0.035 ± 0.190 | 0.084 ± 0.168 | −0.119 ± 0.148 | 0.001 | −0.65 [−1.01, −0.32] |
| max_HbO (µmol/L) ** | 0.170 ± 0.221 | 0.279 ± 0.211 | −0.108 ± 0.147 | 0.002 | −0.49 [−0.78, −0.22] |
| diff_Hb (µmol/L) ** | −0.014 ± 0.238 | 0.079 ± 0.181 | −0.093 ± 0.170 | 0.004 | −0.43 [−0.76, −0.12] |
| avg_HbR (µmol/L) | −0.021 ± 0.071 | 0.005 ± 0.060 | −0.026 ± 0.070 | 0.088 | −0.38 [−0.80, 0.02] |
| min_HbR (µmol/L) | −0.074 ± 0.083 | −0.060 ± 0.070 | −0.014 ± 0.079 | 0.202 | −0.18 [−0.57, 0.21] |
| avg_HbT (µmol/L) *** | −0.056 ± 0.161 | 0.088 ± 0.175 | −0.144 ± 0.157 | <0.001 | −0.84 [−1.26, −0.46] |
| max_HbT (µmol/L) ** | 0.152 ± 0.170 | 0.280 ± 0.224 | −0.128 ± 0.165 | 0.001 | −0.63 [−0.99, −0.30] |
| deltaH (µmol/L) ** | 0.244 ± 0.283 | 0.338 ± 0.236 | −0.094 ± 0.170 | 0.004 | −0.36 [−0.62, −0.10] |
| tmax_HbO (s) * | 6.32 ± 3.70 | 8.37 ± 3.90 | −2.04 ± 4.09 | 0.014 | −0.53 [−0.96, −0.12] |
| tmax_HbT (s) * | 6.66 ± 4.25 | 8.54 ± 4.10 | −1.87 ± 4.60 | 0.040 | −0.44 [−0.8, −0.02] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Greenfield, J.; Delcroix, V.; Ettaki, W.; Derollepot, R.; Paire-Ficout, L.; Ranchet, M. Left and Right Cortical Activity Arising from Preferred Walking Speed in Older Adults. Sensors 2023, 23, 3986. https://doi.org/10.3390/s23083986
Greenfield J, Delcroix V, Ettaki W, Derollepot R, Paire-Ficout L, Ranchet M. Left and Right Cortical Activity Arising from Preferred Walking Speed in Older Adults. Sensors. 2023; 23(8):3986. https://doi.org/10.3390/s23083986
Chicago/Turabian StyleGreenfield, Julia, Véronique Delcroix, Wafae Ettaki, Romain Derollepot, Laurence Paire-Ficout, and Maud Ranchet. 2023. "Left and Right Cortical Activity Arising from Preferred Walking Speed in Older Adults" Sensors 23, no. 8: 3986. https://doi.org/10.3390/s23083986
APA StyleGreenfield, J., Delcroix, V., Ettaki, W., Derollepot, R., Paire-Ficout, L., & Ranchet, M. (2023). Left and Right Cortical Activity Arising from Preferred Walking Speed in Older Adults. Sensors, 23(8), 3986. https://doi.org/10.3390/s23083986






