Surface EMG Statistical and Performance Analysis of Targeted-Muscle-Reinnervated (TMR) Transhumeral Prosthesis Users in Home and Laboratory Settings
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Statistical Properties Calculation
- Root Mean Square (RMS)
- 2.
- Mean Frequency (MeanF) [23]
- 3.
- Median Frequency (MedF) [23]
- 4.
- Variance
2.3. Signal Processing and Feature Extraction
2.4. Calibration Quality Quantification
2.4.1. Separability Indices
- Davies-Bouldin index (DBI) [26]
- Simplified Silhouette value (SS) [27]
- Fisher’s linear discriminate analysis index (FLDI) [28]
- Separability index (SI) [29]
2.4.2. Repeatability Index and Correlation Coefficients
- Repeatability index (RI) [29]
- Two-Sample Kolmogorov–Smirnov Test statistics (K-S) [31]
- Spearman correlations (rho) [32]
2.5. Data Analysis
3. Results
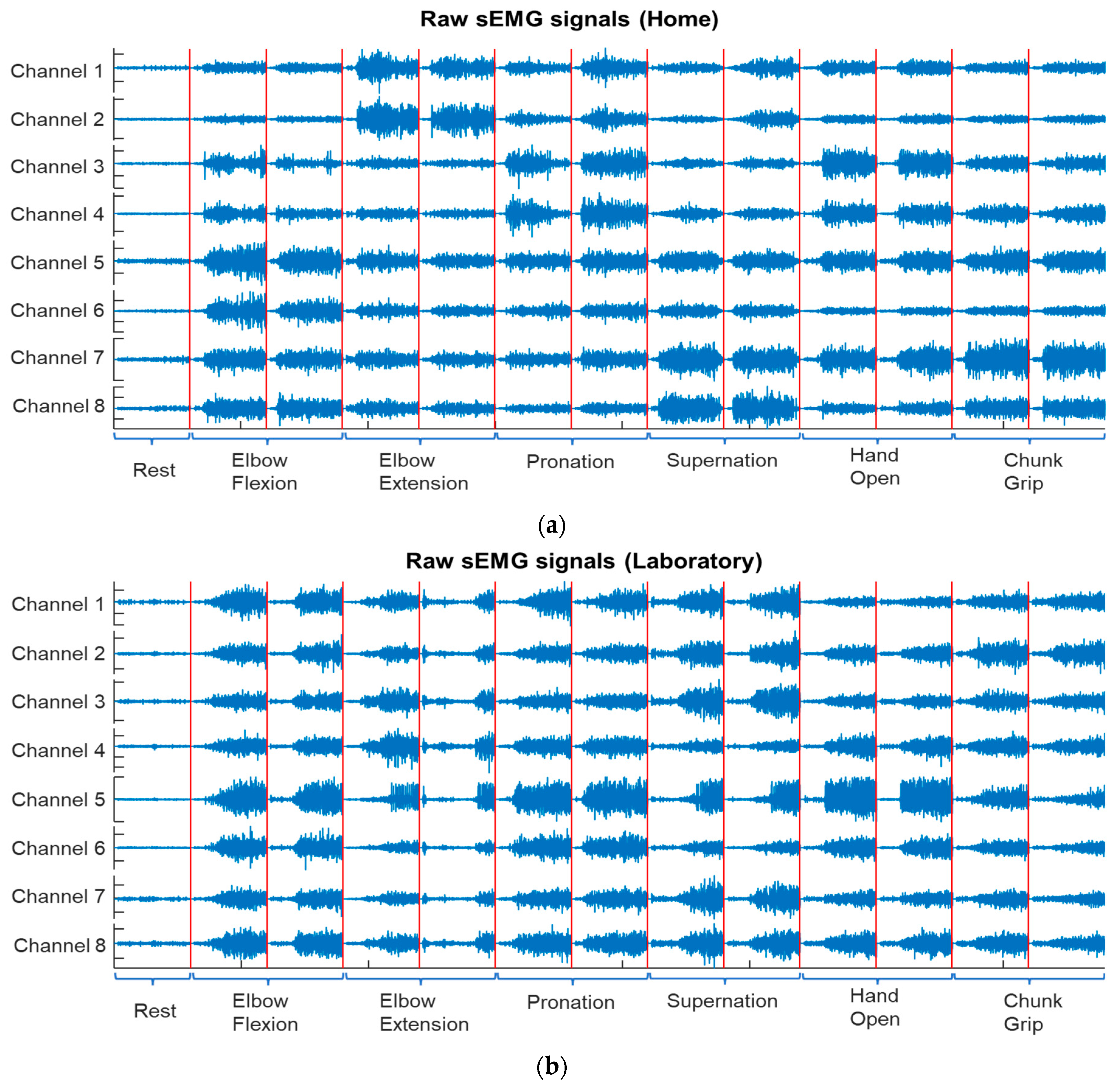
3.1. Raw sEMG Signals
3.2. Statistical Properties and Classification
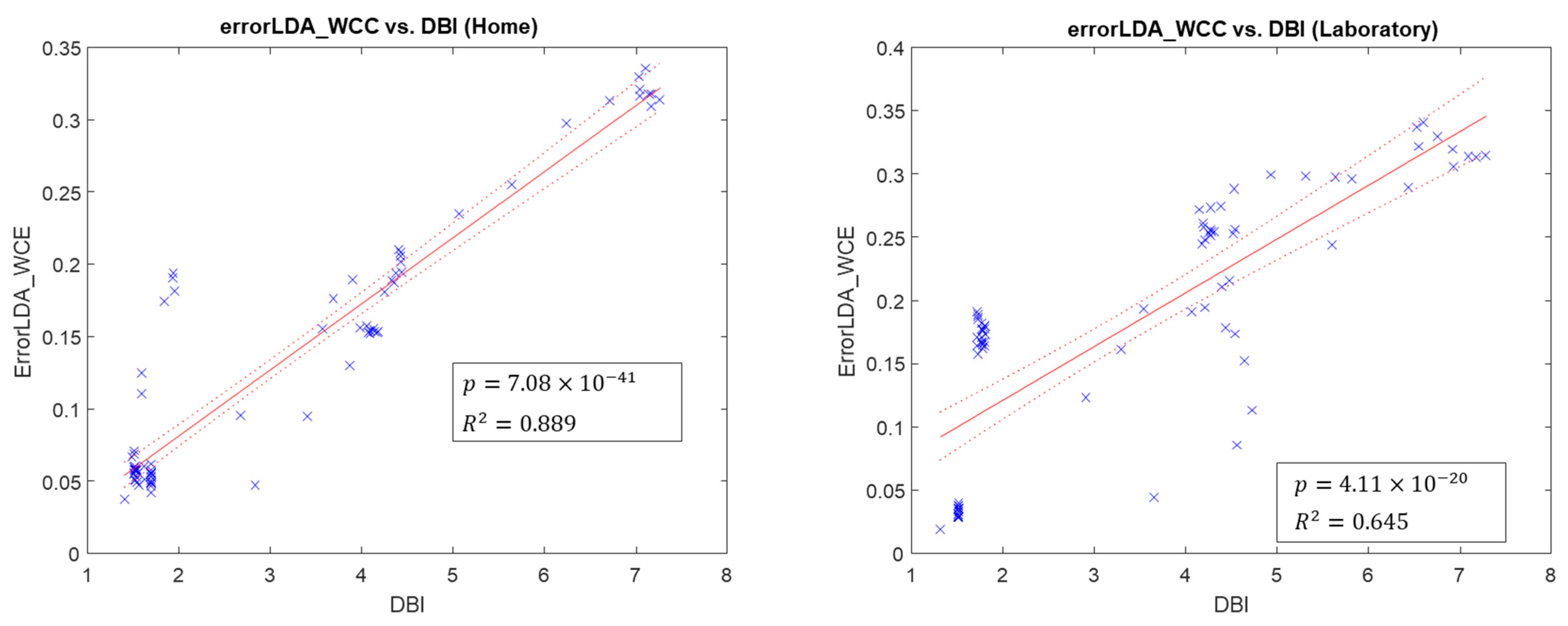
3.3. Metrics for Calibration Quality Quantification
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Specialised Commissioning Team; NHS England. Hand and Upper Limb Reconstruction Using Vascularised Composite Allotransplantation (HAUL-VCA); NHS England: Leeds, UK, 2015.
- Geethanjali, P. Myoelectric control of prosthetic hands: State-of-the-art review. Med. Devices 2016, 9, 247–255. [Google Scholar] [CrossRef]
- Farina, D.; Jiang, N.; Rehbaum, H.; Holobar, A.; Graimann, B.; Dietl, H.; Aszmann, O.C. The extraction of neural information from the surface EMG for the control of upper-limb prostheses: Emerging avenues and challenges. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 22, 797–809. [Google Scholar] [CrossRef]
- Salminger, S.; Stino, H.; Pichler, L.H.; Gstoettner, C.; Sturma, A.; Mayer, J.A.; Szivak, M.; Aszmann, O.C. Current rates of prosthetic usage in upper-limb amputees-have innovations had an impact on device acceptance? Disabil. Rehabil. 2020, 44, 3708–3713. [Google Scholar] [CrossRef]
- Waris, A.; Niazi, I.K.; Jamil, M.; Gilani, O.; Englehart, K.; Jensen, W.; Shafique, M.; Kamavuako, E.N. The effect of time on EMG classification of hand motions in able-bodied and transradial amputees. J. Electromyogr. Kinesiol. 2018, 40, 72–80. [Google Scholar] [CrossRef]
- Sheng, X.; Lv, B.; Guo, W.; Zhu, X. Common spatial-spectral analysis of EMG signals for multiday and multiuser myoelectric interface. Biomed. Signal Process. Control 2019, 53, 101572. [Google Scholar] [CrossRef]
- Jaber, H.A.; Rashid, M.T.; Fortuna, L. Using the Robust High Density-surface Electromyography Features for Real-Time Hand Gestures Classification. IOP Conf. Ser. Mater. Sci. Eng. 2020, 745, 012020. [Google Scholar] [CrossRef]
- Waris, A.; Niazi, I.K.; Jamil, M.; Englehart, K.; Jensen, W.; Kamavuako, E.N. Multiday Evaluation of Techniques for EMG-Based Classification of Hand Motions. IEEE J. Biomed. Health Inform. 2019, 23, 1526–1534. [Google Scholar] [CrossRef]
- Díaz-Amador, R.; Mendoza-Reyes, M.A. Towards the reduction of the effects of muscle fatigue on myoelectric control of upper limb prostheses. Dyna 2019, 86, 110–116. [Google Scholar] [CrossRef]
- Sae-lim, W.; Phukpattaranont, P.; Thongpull, K. Effect of Electrode Skin Impedance on Electromyography Signal Quality. In Proceedings of the 2018 15th International Conference on Electrical Engineering/Electronics, Computer, Telecommunications and Information Technology (ECTI-CON), Chiang Rai, Thailand, 18–21 July 2018; pp. 748–751. [Google Scholar]
- He, J.; Sheng, X.; Zhu, X.; Jiang, N. Position Identification for Robust Myoelectric Control Against Electrode Shift. IEEE Trans Neural Syst. Rehabil. Eng. 2020, 28, 3121–3128. [Google Scholar] [CrossRef]
- Hahne, J.M.; Markovic, M.; Farina, D. User adaptation in Myoelectric Man-Machine Interfaces. Sci. Rep. 2017, 7, 4437. [Google Scholar] [CrossRef]
- Atzori, M.; Muller, H. Control Capabilities of Myoelectric Robotic Prostheses by Hand Amputees: A Scientific Research and Market Overview. Front. Syst. Neurosci. 2015, 9, 162. [Google Scholar] [CrossRef]
- Samuel, O.W.; Li, X.; Geng, Y.; Asogbon, M.G.; Fang, P.; Huang, Z.; Li, G. Resolving the adverse impact of mobility on myoelectric pattern recognition in upper-limb multifunctional prostheses. Comput. Biol. Med. 2017, 90, 76–87. [Google Scholar] [CrossRef]
- Islam, M.J.; Ahmad, S.; Haque, F.; Reaz, M.B.I.; Bhuiyan, M.A.S.; Islam, M.R. Force-Invariant Improved Feature Extraction Method for Upper-Limb Prostheses of Transradial Amputees. Diagnostics 2021, 11, 843. [Google Scholar] [CrossRef]
- Gigli, A.; Gijsberts, A.; Castellini, C. The Merits of Dynamic Data Acquisition for Realistic Myocontrol. Front. Bioeng. Biotechnol. 2020, 8, 361. [Google Scholar] [CrossRef]
- Bao, T.; Zaidi, S.A.R.; Xie, S.Q.; Yang, P.; Zhang, Z.Q. CNN Confidence Estimation for Rejection-Based Hand Gesture Classification in Myoelectric Control. IEEE Trans. Hum.-Mach. Syst. 2022, 52, 99–109. [Google Scholar] [CrossRef]
- Osborn, L.E.; Moran, C.W.; Dodd, L.D.; Sutton, E.E.; Norena Acosta, N.; Wormley, J.M.; Pyles, C.O.; Gordge, K.D.; Nordstrom, M.J.; Butkus, J.A.; et al. Monitoring at-home prosthesis control improvements through real-time data logging. J. Neural Eng. 2022, 19, 036021. [Google Scholar] [CrossRef]
- Simon, A.; Turner, K.; Miller, L.; Potter, B.; Beachler, M.; Dumanian, G.; Hargrove, L.; Kuiken, T. User performance with a transradial multi-articulating hand prosthesis during pattern recognition and direct control home use. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 1. [Google Scholar] [CrossRef]
- Resnik, L.; Acluche, F.; Borgia, M. The DEKA hand: A multifunction prosthetic terminal device—Patterns of grip usage at home. Prosthet. Orthot. Int. 2018, 42, 446–454. [Google Scholar] [CrossRef]
- Hargrove, L.J.; Miller, L.A.; Turner, K.; Kuiken, T.A. Myoelectric Pattern Recognition Outperforms Direct Control for Transhumeral Amputees with Targeted Muscle Reinnervation: A Randomized Clinical Trial. Sci. Rep. 2017, 7, 13840. [Google Scholar] [CrossRef]
- Tkach, D.C.; Young, A.J.; Smith, L.H.; Rouse, E.J.; Hargrove, L.J. Real-Time and Offline Performance of Pattern Recognition Myoelectric Control Using a Generic Electrode Grid With Targeted Muscle Reinnervation Patients. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 22, 727–734. [Google Scholar] [CrossRef]
- Phinyomark, A.; Thongpanja, S.; Hu, H.; Phukpattaranont, P.; Limsakul, C. The Usefulness of Mean and Median Frequencies in Electromyography Analysis; Intech: Singapore, 2012; pp. 195–220. [Google Scholar] [CrossRef]
- Hudgins, B.; Parker, P.; Scott, R.N. A new strategy for multifunction myoelectric control. IEEE Trans. Biomed. Eng. 1993, 40, 82–94. [Google Scholar] [CrossRef]
- Wang, B.; Kamavuako, E.N. Correlation between the stability of feature distribution and classification performance in sEMG signals. In Proceedings of the 2021 4th International Conference on Bio-Engineering for Smart Technologies (BioSMART), Salford Manchester, UK, 8–10 December 2021; pp. 1–4. [Google Scholar]
- Campbell, E.; Phinyomark, A.; Scheme, E. Current Trends and Confounding Factors in Myoelectric Control: Limb Position and Contraction Intensity. Sensors 2020, 20, 1613. [Google Scholar] [CrossRef]
- Wang, F.; Franco-Penya, H.-H.; Kelleher, J.; Pugh, J.; Ross, R. An Analysis of the Application of Simplified Silhouette to the Evaluation of k-means Clustering Validity; Springer: Berlin/Heidelberg, Germany, 2017. [Google Scholar] [CrossRef]
- Phinyomark, A.; Khushaba, R.; Ibáñez-Marcelo, E.; Patania, A.; Scheme, E.; Petri, G. Navigating Features: A Topologically Informed Chart of Electromyographic Features Space. J. R. Soc. Interface 2017, 14, 20170734. [Google Scholar] [CrossRef]
- Bunderson, N.E.; Kuiken, T.A. Quantification of Feature Space Changes With Experience During Electromyogram Pattern Recognition Control. IEEE Trans. Neural Syst. Rehabil. Eng. 2012, 20, 239–246. [Google Scholar] [CrossRef]
- He, J.; Zhang, D.; Jiang, N.; Sheng, X.; Farina, D.; Zhu, X. User adaptation in long-term, open-loop myoelectric training: Implications for EMG pattern recognition in prosthesis control. J. Neural Eng. 2015, 12, 046005. [Google Scholar] [CrossRef]
- Duda, R.O.; Hart, P.E.; Stork, D.G. Pattern Classification, 2nd ed.; Wiley-Interscience: Hoboken, NJ, USA, 2000. [Google Scholar]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation Coefficients: Appropriate Use and Interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef]
- Al-Timemy, A.H.; Khushaba, R.N.; Bugmann, G.; Escudero, J. Improving the Performance Against Force Variation of EMG Controlled Multifunctional Upper-Limb Prostheses for Transradial Amputees. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 650–661. [Google Scholar] [CrossRef]
- Van Cutsem, J.; Marcora, S.; De Pauw, K.; Bailey, S.; Meeusen, R.; Roelands, B. The Effects of Mental Fatigue on Physical Performance: A Systematic Review. Sport. Med. 2017, 47, 1569–1588. [Google Scholar] [CrossRef]
- Roman-Liu, D. The influence of confounding factors on the relationship between muscle contraction level and MF and MPF values of EMG signal: A review. Int. J. Occup. Saf. Ergon. 2016, 22, 77–91. [Google Scholar] [CrossRef]
- Waris, A.; Kamavuako, E.N. Effect of threshold values on the combination of EMG time domain features: Surface versus intramuscular EMG. Biomedical Signal Process. Control. 2018, 45, 267–273. [Google Scholar] [CrossRef]
- Brantly, N.; Feuser, A.; Cummins, F.; Hargrove, L.J.; Lock, B.A. Patter Recognition Myoelectric Control Calibration Quality Feedback Tool To Increase Function. In Proceedings of the MEC Symposion 2017, Fredericton, NB, Canada, 15–18 August 2017. [Google Scholar]



| Participant | Age | Time Since Amputation (Years) | Time Since TMR | Amputation Side | Etiology | Calibration Times | |
|---|---|---|---|---|---|---|---|
| Home | Laboratory | ||||||
| TH01 | 35 | 4 | 3 | Right | Trauma (military) | 7 | 28 |
| TH02 | 54 | 6 | <1 | Left | Trauma (military) | 78 | 20 |
| TH03 | 58 | 5 | 1 | Left | Sarcoma | 57 | 17 |
| TH04 | 31 | 8 | 7 | Left | Trauma (military) | 22 | 25 |
| TH05 | 27 | 2 | 1 | Right | Trauma (crushing) | 18 | 100 |
| Statistical Property | Home | Laboratory | p Value |
|---|---|---|---|
| RMS | 0.33 ± 0.11 | ||
| Variance | 0.19 ± 0.12 | 0.22 ± 0.13 | |
| Mean F | 151.42 ± 10.81 | 145.16 ± 10.21 | |
| Med F | 138.70 ± 11.27 | 131.95 ± 11.15 |
| Participant | WCC Error (%) | BCC Error (%) | ||
|---|---|---|---|---|
| Home | Lab | Home | Lab | |
| TH01 | 5.61 ± 1.55 | 5.80 ± 3.60 | 28.40 ± 4.91 | 33.14 ± 12.47 |
| TH02 | 6.72 ± 1.62 | 8.30 ± 3.14 | 21.10 ± 10.96 | 31.25 ± 10.94 |
| TH03 | 7.77 ± 2.42 | 8.66 ± 3.33 | 40.85 ± 9.64 | 43.84 ± 13.79 |
| TH04 | 6.73 ± 3.55 | 10.62 ± 4.37 | 54.49 ± 10.23 | 60.09 ± 10.36 |
| TH05 | 4.84 ± 1.49 | 4.55 ± 2.78 | 58.22 ± 10.21 | 56.59 ± 13.19 |
| Overall mean error (%) | 6.33 ± 2.13 | 7.57 ± 3.44 | 40.61 ± 9.19 | 44.98 ± 12.15 |
| Metric | R-Squared Value | p-Value | Averaged Value across All Calibrations | |||
|---|---|---|---|---|---|---|
| Home | Lab | Home | Lab | |||
| Separability indices | DBI | 0.89 | 0.65 | 0.011 | 3.06 ± 1.87 | 3.34 ± 1.87 |
| SS | 0.81 | 0.84 | 0.063 | 0.31 ± 0.12 | 0.25 ± 0.14 | |
| FLDI | 0.86 | 0.72 | 0.156 | −7.17 ± 2.86 | −7.58 ± 2.68 | |
| SI | 0.54 | 0.85 | 0.012 | 6.96 ± 5.64 | 4.47 ± 2.99 | |
| Repeatability index and CC 1 | RI | 0.66 | 0.51 | 0.445 | 2.05 ± 1.48 | 2.16 ± 1.59 |
| K-S | 0.29 | 0.00 | 0.156 | 0.19 ± 0.03 | 0.21 ± 0.04 | |
| rho | 0.46 | 0.12 | 0.913 | 0.89 ± 0.03 | 0.88 ± 0.04 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, B.; Hargrove, L.; Bao, X.; Kamavuako, E.N. Surface EMG Statistical and Performance Analysis of Targeted-Muscle-Reinnervated (TMR) Transhumeral Prosthesis Users in Home and Laboratory Settings. Sensors 2022, 22, 9849. https://doi.org/10.3390/s22249849
Wang B, Hargrove L, Bao X, Kamavuako EN. Surface EMG Statistical and Performance Analysis of Targeted-Muscle-Reinnervated (TMR) Transhumeral Prosthesis Users in Home and Laboratory Settings. Sensors. 2022; 22(24):9849. https://doi.org/10.3390/s22249849
Chicago/Turabian StyleWang, Bingbin, Levi Hargrove, Xinqi Bao, and Ernest N. Kamavuako. 2022. "Surface EMG Statistical and Performance Analysis of Targeted-Muscle-Reinnervated (TMR) Transhumeral Prosthesis Users in Home and Laboratory Settings" Sensors 22, no. 24: 9849. https://doi.org/10.3390/s22249849
APA StyleWang, B., Hargrove, L., Bao, X., & Kamavuako, E. N. (2022). Surface EMG Statistical and Performance Analysis of Targeted-Muscle-Reinnervated (TMR) Transhumeral Prosthesis Users in Home and Laboratory Settings. Sensors, 22(24), 9849. https://doi.org/10.3390/s22249849








