Review on Medical Implantable Antenna Technology and Imminent Research Challenges
Abstract
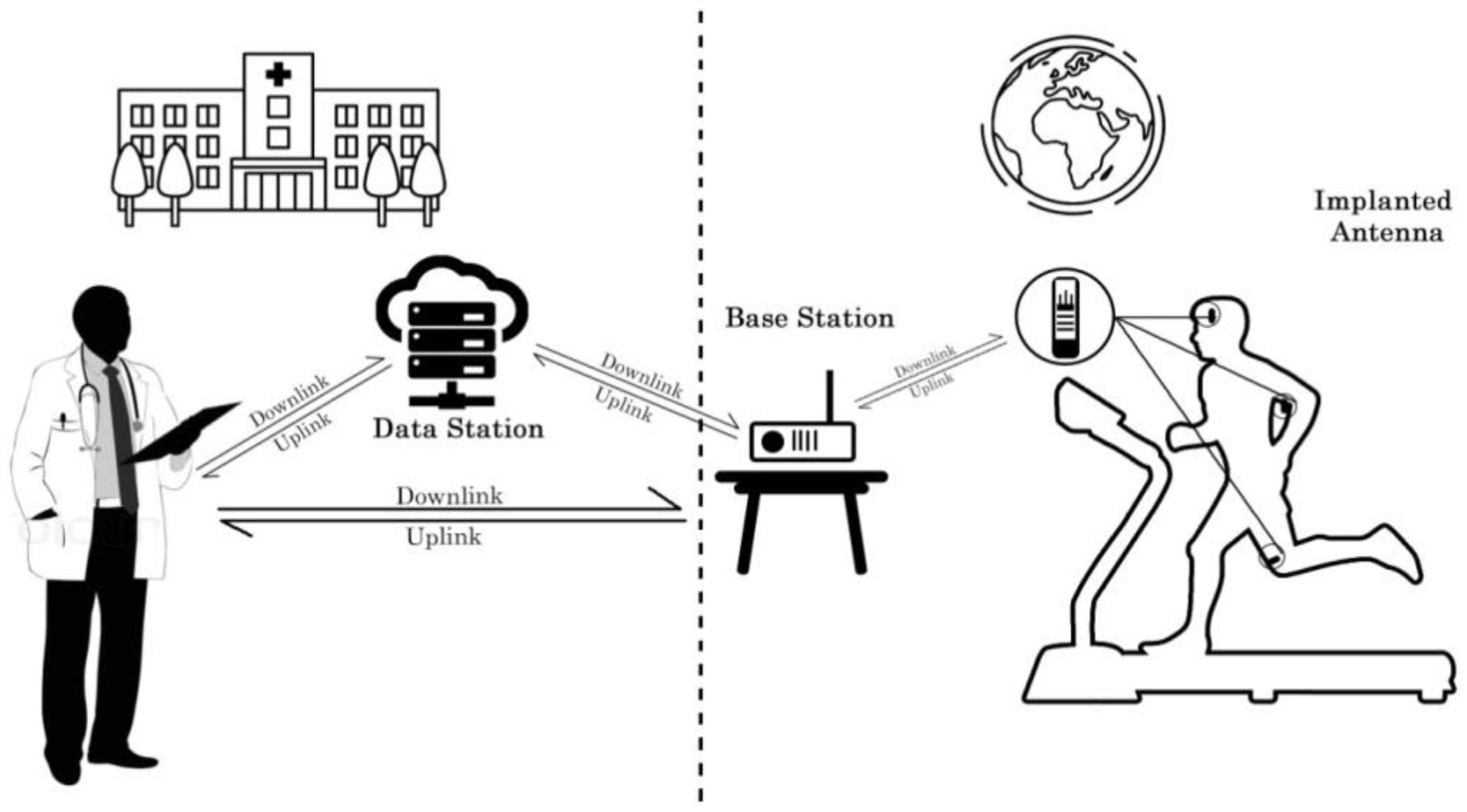
1. Introduction
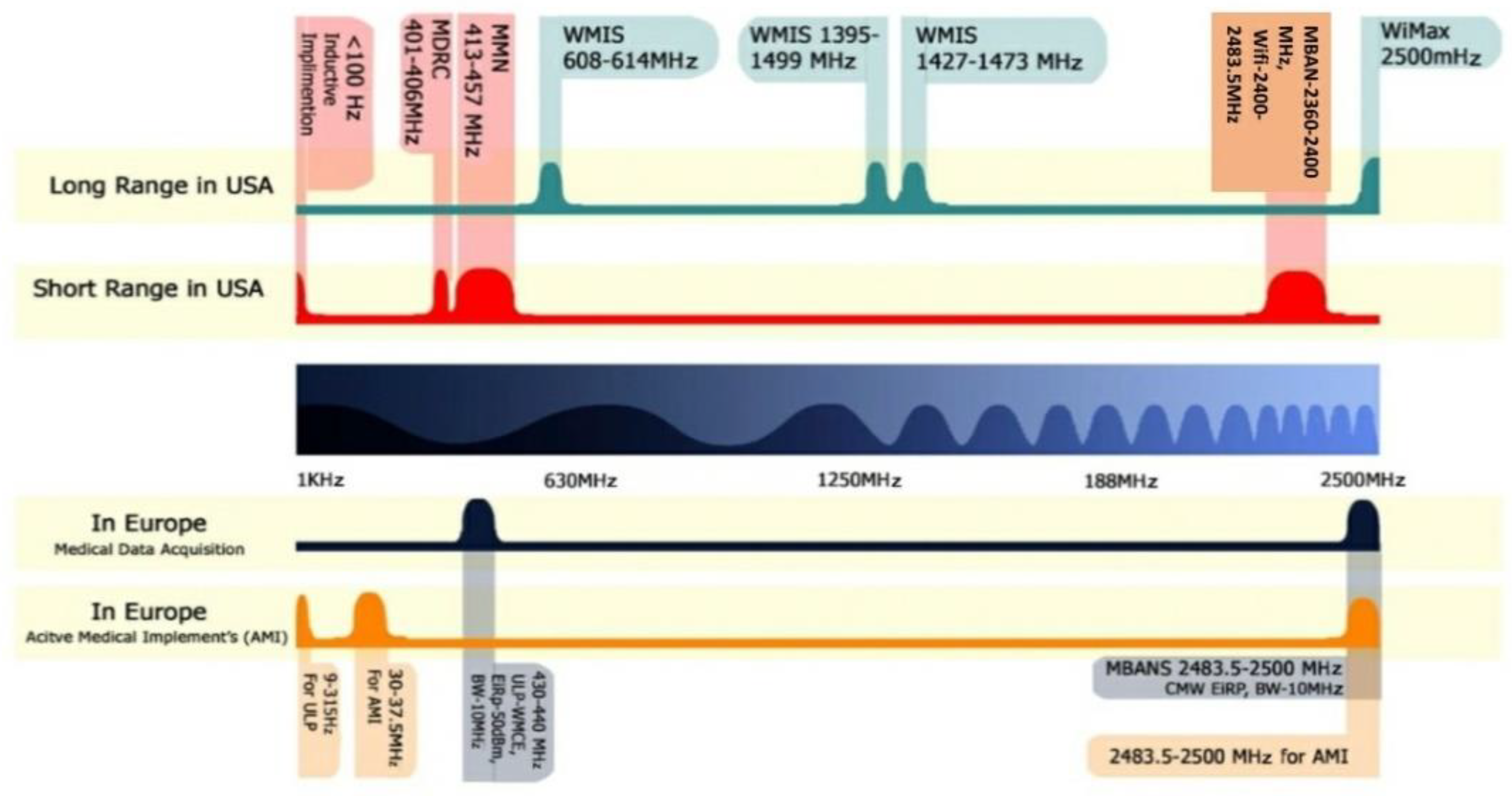
2. Radiofrequency Spectrum Allocation
2.1. Radio Frequency Spectrum Allocations in the United States
2.1.1. Short Range Wireless Medical Devices
- ▪
- ▪
- Medical Device Radio Communication Service (MDRC)—The frequency range 401–402 and 405–406 MHz are allocated for wearable medical applications. The channel bandwidth limit is 100 kHz for the bands of 401–402 and 405–406 MHz. On the other hand, 300 kHz is permitted for the band of 402–405 MHz [17,18].
- ▪
- Ultra-wide Band (UWB)—UWB is an emerging wireless band for medical applications in the band of 3.1–10.6 GHz. Wireless medical devices that are operating in UWB provide higher data transfer rate of 1 Gbps for a short range of communication (<1 m).
- ▪
- Medical Micropower Networks (MMNs)—FCC assigned a 24 MHz frequency spectrum in 413–457 MHz frequency band for implant medical device applications. The frequency spectrum is divided into four segments: 413–419, 426–432, 438–444, and 451–457 MHz [18].
- ▪
- Medical Body Area Networks (MBANs)—According to the General Electronic Health care (GEHC) proposal, FCC allocated a frequency spectrum in the band of 2360–2400 MHz to monitor human body conditions using medical body area networks [18].
- ▪
- Wi-Fi, Bluetooth, and Zigbee—FCC declared the frequency spectrum for Wi-Fi, Bluetooth, and ZigBee in the frequency bands of 902–928, 2400–2483.5, and 5725–5850 MHz, respectively. These frequency spectrums can be used for short-range digital modulation communication applicable for implant medical [18].
2.1.2. Long Range Wireless Medical Devices
- ▪
- Wireless Medical Telemetry Services (WMTS)—FCC allocated at 13 MHz spectrum for WMTS in the frequency bands of 608–614, 1395–1400, and 1427–1429 MHz. WMTS devices are used for monitoring the patient’s health condition via a bi-directional wireless link [18].
- ▪
- World Interoperability for Microwave Access (WiMAX)—The frequency spectrum allocated for WiMAX in the frequency band of 2.5 GHz, according to the IEEE 802.16. WiMAX can transmit approximately 70 Mbps, which is very efficient in data transfer, it is used to transfer information from an ambulance to the hospital [18].
2.2. Radio Frequency Spectrum Allocations in Europe
2.2.1. Active Medical Implants and Associated Peripherals
2.2.2. Medical Data Acquisition Band
- ▪
- Ultra-Low Power Wireless Medical Capsule Endoscopy (ULP-WMCE)—430–440 MHz frequency band is allocated for the wearable ULP-WMCE applications. The effective channel bandwidth is 10 MHz with Equivalent Isotropically Radiated Power (EIRP) −50 dBm.
- ▪
- Medical Body Area Network System (MBANS)—The frequency spectrum of 2483.5–2500 MHz allocated for MBANS is utilized for patient monitoring devices in indoor communications. The effective isotropic radiated power set for MBANS devices is 1 mW for a channel bandwidth of 3 MHz. In Figure 2, spectrum allocation for wireless medical applications in the United States and Europe is shown.
3. Factors that Affect the Design of an Implantable Antenna
3.1. Impact of Tissues Diversification
3.1.1. Radio Wave Propagation in the Lossy Medium
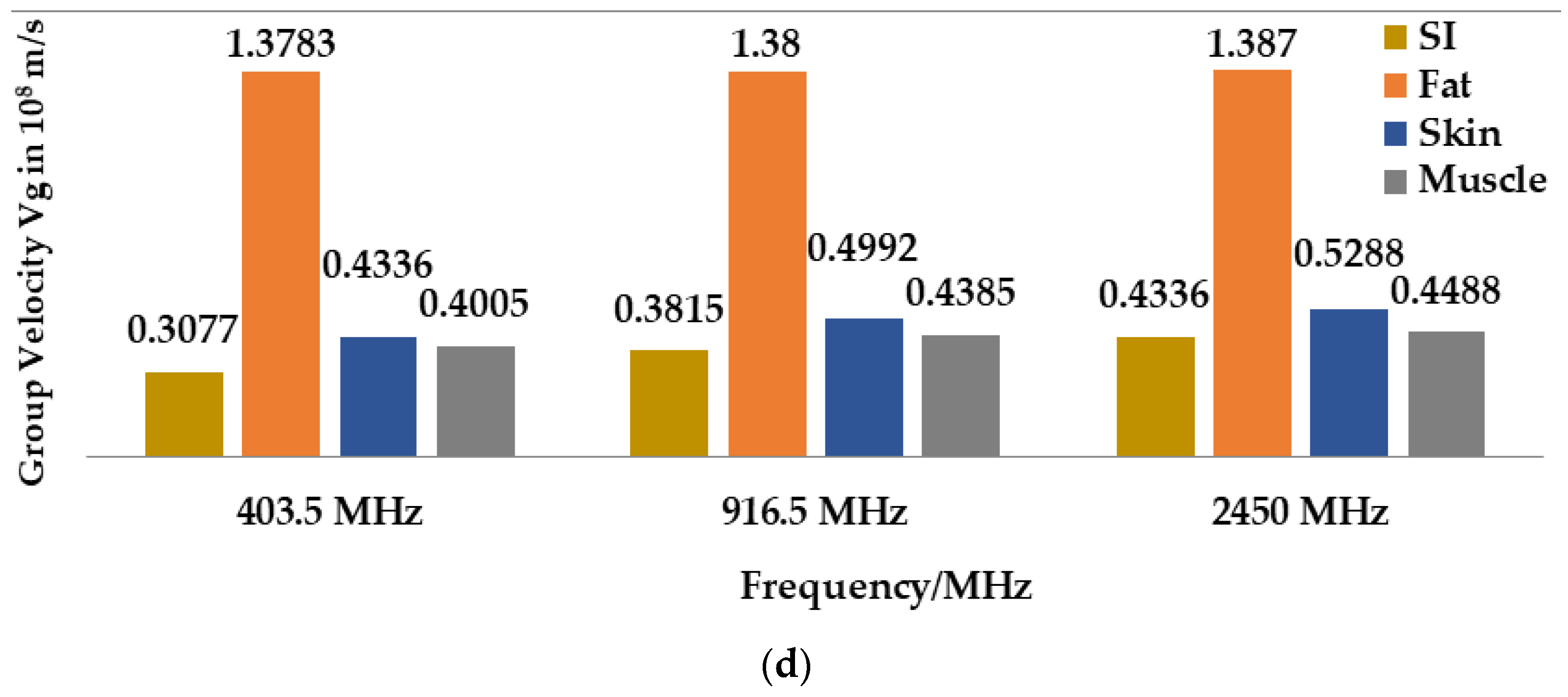
3.1.2. Propagation Speed inside the Human Body
3.2. Impact on Effective Wavelength
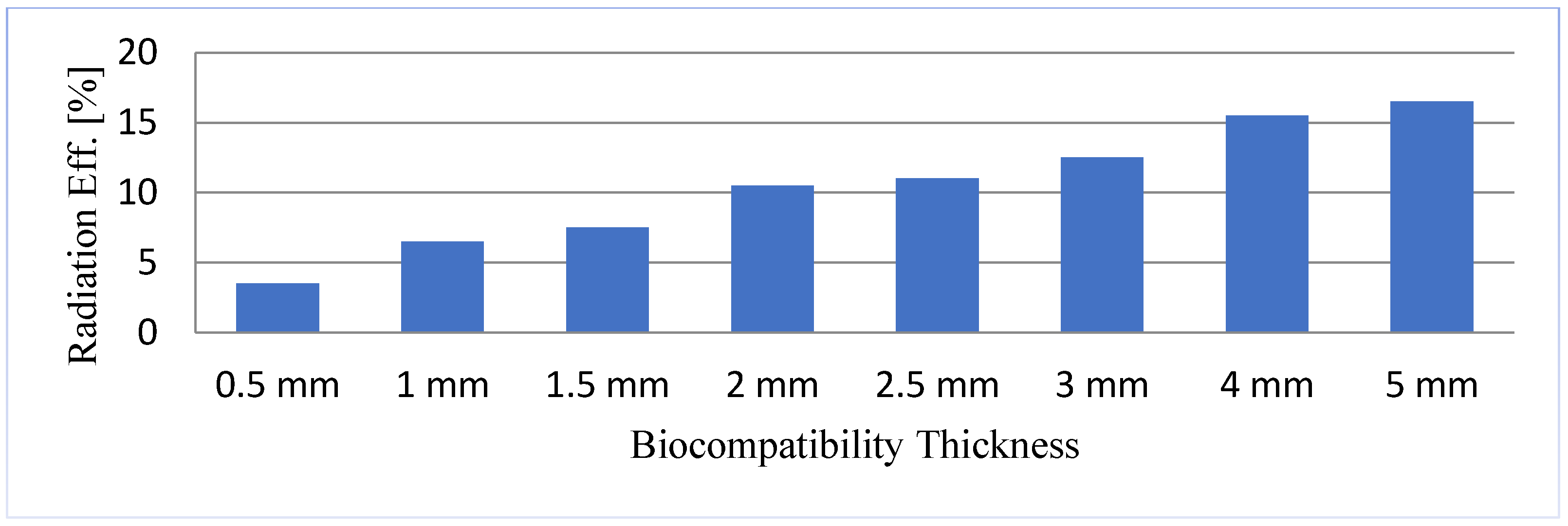
3.3. Biocompatible Encapsulation of the Implantable Antenna
3.4. Impact on Radiated Power and Efficiency
3.5. Requirement of Specific Absorption Rate (SAR)
3.6. Consideration in Powering System
4. Summary of the Existing Implant Antenna Technology
4.1. Different Antenna Design Techniques
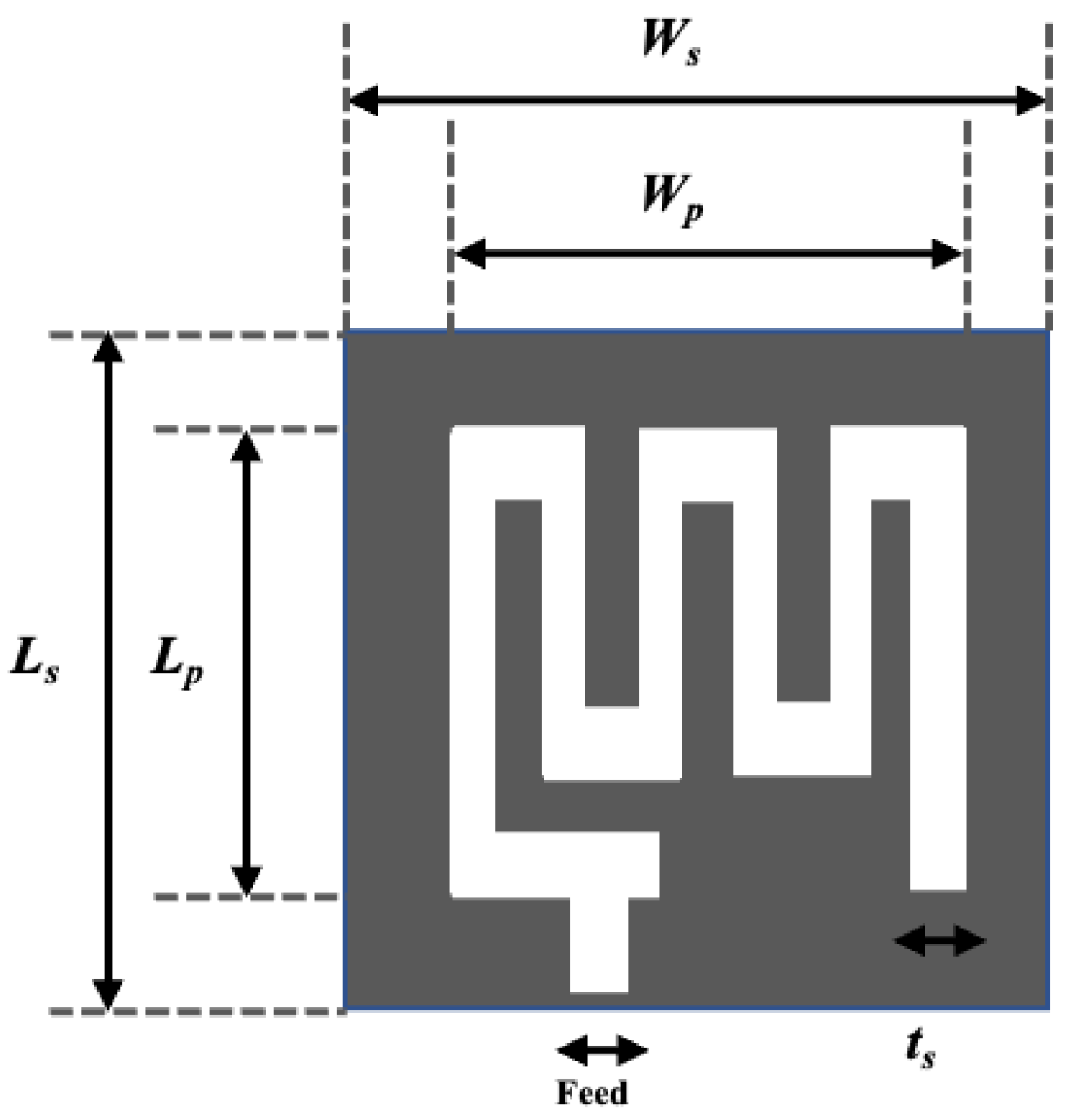
4.1.1. Miniaturization of Antenna Dimension
4.1.2. Spiral Shape Radiating Patch
4.1.3. Insertion of Shorting Pin-In Wireless Technology
4.1.4. Gain and Efficiency Enlargement Technique
- Insulating Layers: A theoretical calculation has been made in [65], where a multilayered insulation model considering fat and dry skin was taken as standard. Notably, the insulation with zirconia and 4 mm thickness around the implant antenna gave the lowest attenuation of 34.5 dB than the other insulation materials (e.g., alumina, polyamide, peek, polypropylene). This theoretical calculation agreed with the experimental results reported in [11]. Besides, several materials-based insulation models were investigated in [66,67,68,69,70,71] and the results showed that insulation for biocompatibility reduces the attenuation, while increasing gain and radiation efficiency.
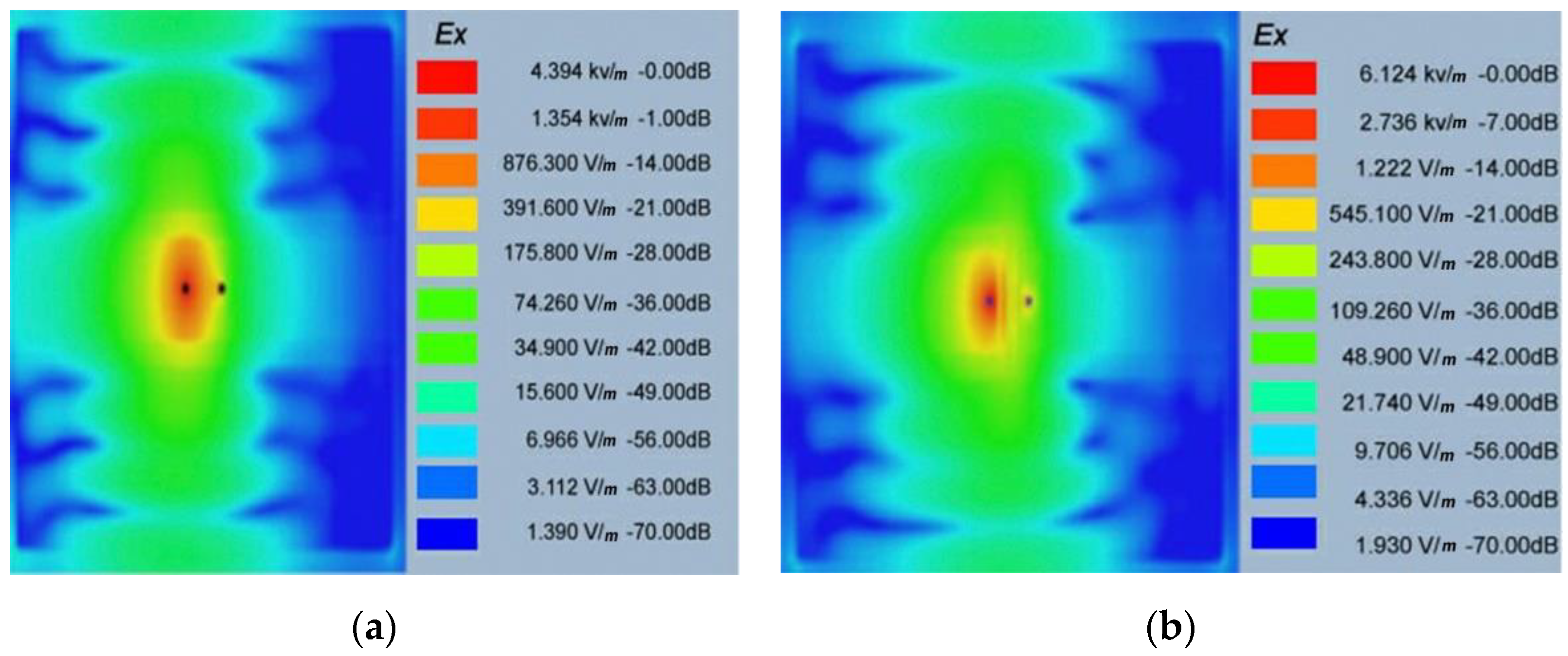
- Complimentary Split Ring Resonators (CSRRs) Antenna Model: The CSRR antenna model is an effective solution to enhance radiation efficiency and gain. This CSRR model compensates inductivity and electric field coupling with the near field due to the antenna’s negative permittivity [72,73]. The SAR is also reduced, which improves the radiation efficiency and gain. The CSRR implant antenna model for multiband (MICS, ISM, and 2.4 GHz) applications was designed and simulated in [74]. The simulation results showed that the electric field was at 403 MHz It can be noted that electric field absorption is reduced for the CSRR model compared to the non-CSRR model. Hence, radiation efficiency and gain are increased for all operational frequencies.
4.1.5. Bandwidth Enhancement Technique
4.1.6. Tuning Permanency Technique
4.2. Implant Antennas for Different Bio-Telemetry Applications
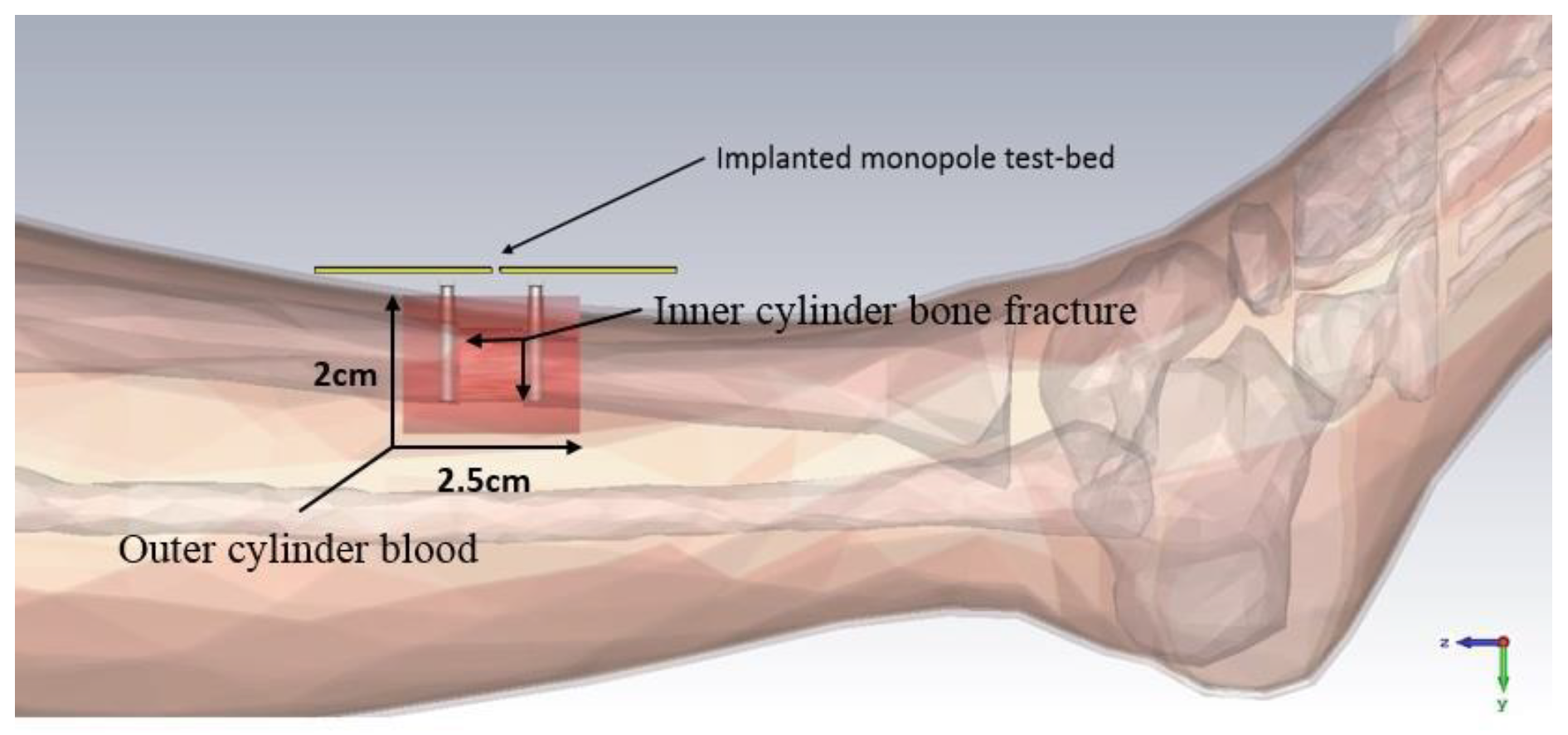
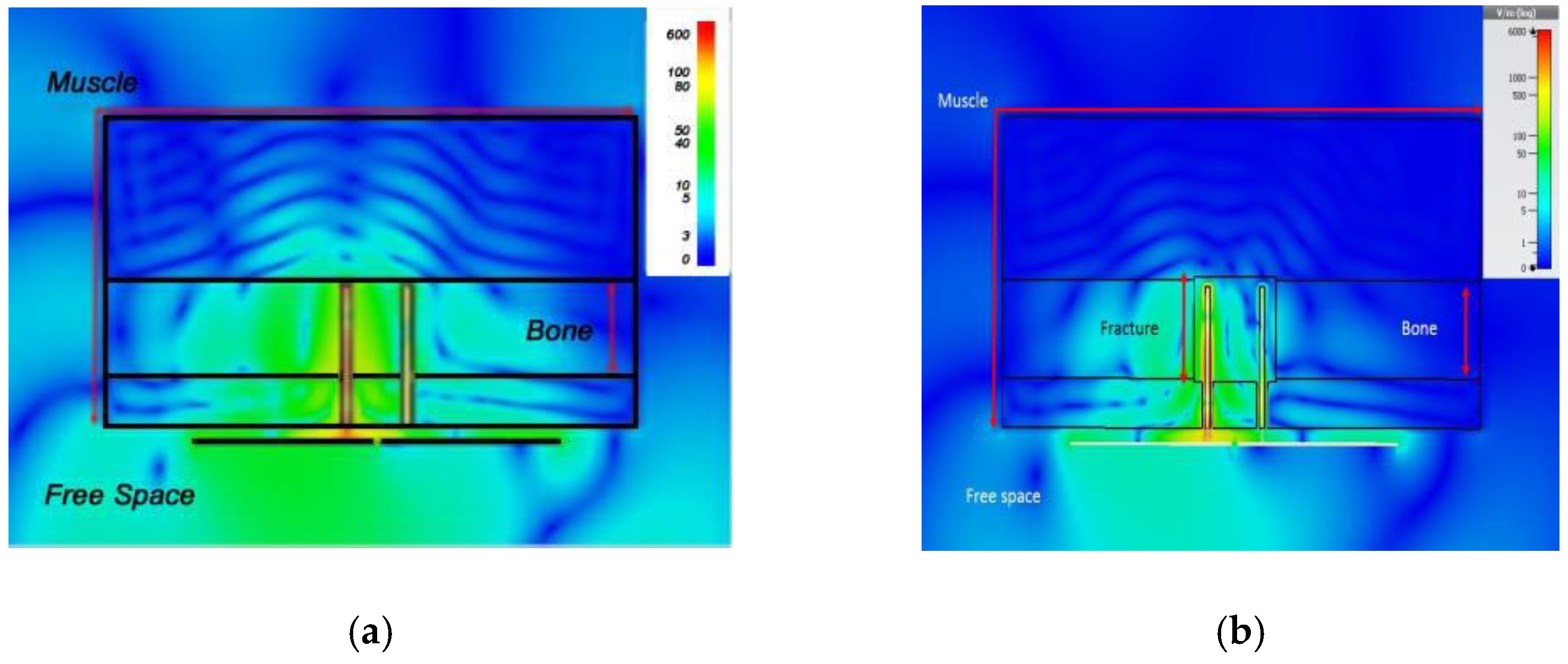
4.2.1. Implant Antenna for Monitoring of the Healing of Bone Fracture
4.2.2. Implant Antenna for Glucose Level Monitoring in Blood
4.2.3. Implant Antenna for Diagnosing Brain Diseases
4.2.4. Implant Antenna for Blood Pressure Measurement
5. Fabrication and Implantation Process of the Implant Antenna
5.1. Implant Antenna Fabrication Process
5.1.1. Antenna Fabrication
5.1.2. Verification of Implant Antenna in Biological Environment
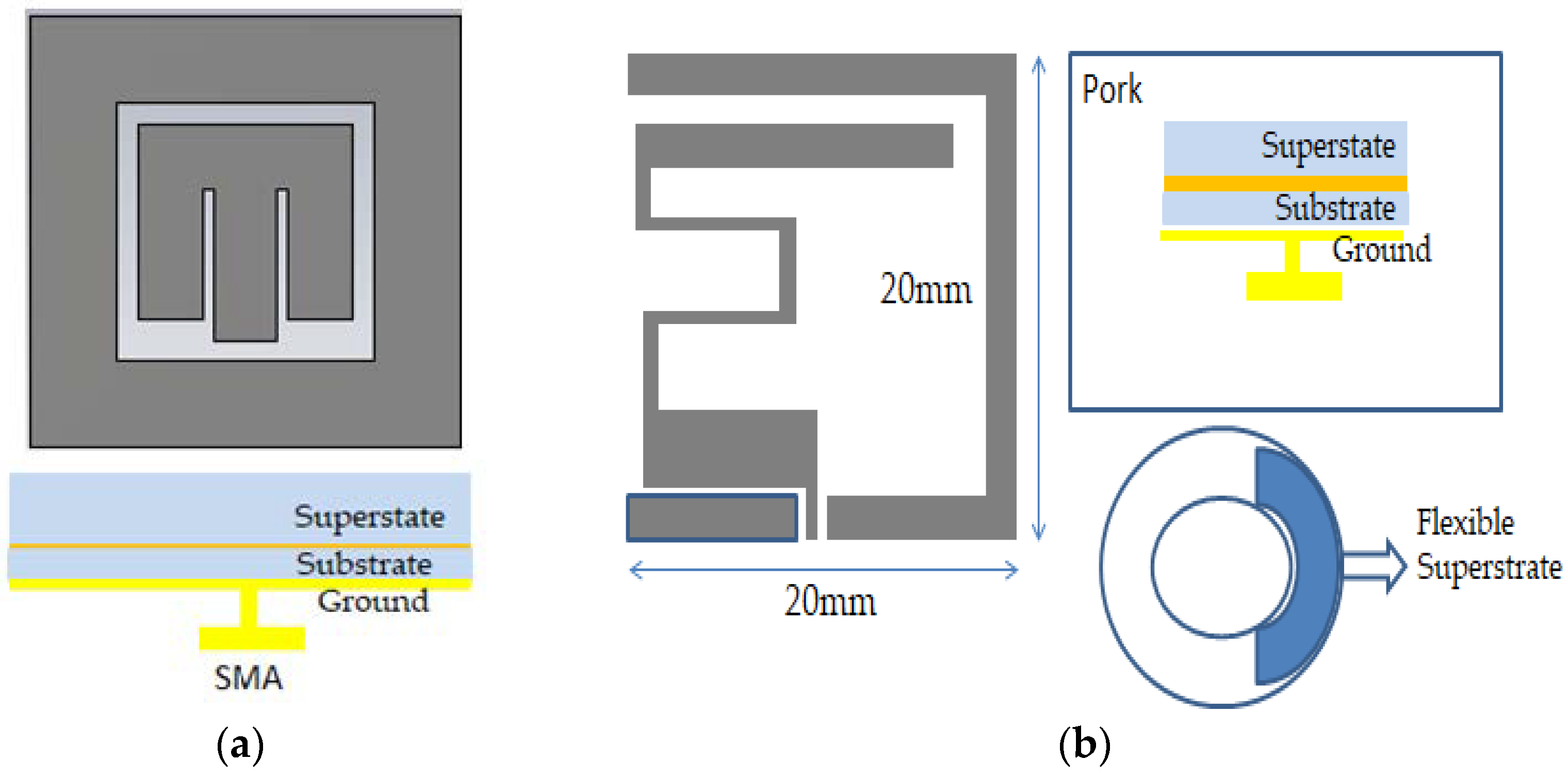
- In vitro Antenna Testing: The fabricated implant antenna is verified in the in vitro antenna testing process using an artificial biological environment [32,54]. Investigation of artificial emulation of the biological tissue environment in the MICS band has been performed in several recent works [64,87,88]. Gels are preferred rather than regular liquid for creating artificial tissue layers, where gels make the layers more solid. Deionized distilled water is used to make the synthetic tissue layers. An artificial biological environment containing 41.48% distilled water, 56.18% glucose, and 2.33% salt with a relative permittivity and conductivity of 46.7 and 0.69 s/m, respectively [87,89]. The properties of artificial phantoms are investigated using an Agilent network analyzer. The implant antenna prototype immersed in the artificial tissue environment is shown in Figure 22a [90]. It can be noted that the implant antenna is immersed in liquid at a distance, d from the surface. The prototype antenna is connected with a vector network analyzer (VNA) via co-axial feeding cable. An implant monopole antenna inserted in the three-layer materials phantoms, where two layers are of bone and one layer of muscle. The phantom is made up of six minerals consisting of flour, oil, deionized water, food color, sugar, and detergent. The in-vitro performance of the implant antenna was compared with the simulated antenna.
- In vivo Antenna Testing: In-vitro study carried out in an artificial biological environment cannot ensure the stability of the implanted antenna system, due to the lack of dynamic representation of a real biological environment in the in vitro study [30]. Hence, antenna testing in a real biological environment is highly recommended after in vitro testing. Before implantation of the prototype antenna inside the body, this must experience the temperature testing process below 100 °C. Generally, the implant antenna itself produces heat up to 60 °C temperature because of the battery and internal system components. Besides, the implant antenna is insulated by biocompatible material for protecting the antenna system from coupling loss. Figure 23 shows the in vivo experimental set-up, where pork body is taken as the standard environment, while Figure 24 a,b illustrates the in-vivo testing of the bone fracture healing process and monitoring of blood pressure inside the left ventricle respectively.
5.2. Power Management
5.2.1. Independent Power Approaches
5.2.2. Transferrable Source
6. Limitations of the Current Implantable Antenna System and Imminent Research Challenges
- ▪
- Absorption of an electromagnetic wave happens due to coupling with lossy tissue in the near reactive and far-field. A significant amount of absorption results in low radiation efficiency and inefficient antenna operation. The radiating wave travels through the near field and far field to reach the outside receiver antenna, since the absorption in the far-field is unavoidable. However, the absorption of a radio wave can be avoided if the biocompatibility of the implant antenna is covered near the field. Therefore, implant antenna design with biocompatibility covering the near field will be a possible research challenge in the future.
- ▪
- Inhomogeneous biological tissues and organs form the human body. Besides, the dimension and characteristics of biological tissues vary from time to time and gender to gender. Therefore, the detuning effect is considered the primary research challenge in designing an implanted antenna for biotelemetry applications. The implantable antenna tuned in a resonance frequency may not be stable for other persons or locations. In research work [103], the detuning effect was performed on four anatomical bodies and thirty tissues. An almost 70 MHz frequency shift from the primary resonance frequency was observed. To date, implant antenna design and experiments are limited to only a single tissue environment, which will be a significant disadvantage for diverse tissue environments. Hence, the upcoming implant antenna must be investigated in different biological environments for efficient antenna operation.
- ▪
- Injection of a radio-frequency device inside the human body may have a long-term complex health problem due to radiative power absorption. Therefore, effective implant antenna design with limiting SAR value and appropriate selection of biocompatible materials will be the primary research concern.
- ▪
- Conventional antenna dimension miniaturization techniques tend to narrow operational bandwidth. The narrowband operation cannot avoid the detuning effect that happens inside the biological environment. Even though biocompatible encapsulation of the implant antenna is utilized to enhance radiation efficiency and gain, it expands the overall thickness of the implant medical device. Hence, the antenna design technique with adequate operational bandwidth, radiation efficiency, and gain is still a challenging issue in implantable medical device technology.
- ▪
- Generally, IMD inside the human body is powered by a battery system. Still, a limited life-time power system and the bulky dimension cause inadequacy in the implant antenna power system. Also, the replacement of the battery system via a surgical procedure makes implementation difficult. The nuclear battery system can be an effective solution to the limited battery life. The nuclear battery provides stable power of 50 μW over an extended range of duration [91]. The only challenge is providing a proper guideline to avoid the poisonousness of radioactive radiation.
- ▪
- A biofuel cell is a battery-less power system that converts biochemical energy into electricity. The primary limitation of a biofuel cell is micro-watt level power, which limits its usefulness in IMDs. Moreover, biofuel cells can harm the tissue cell, even though it is biocompatible in laboratory testing [95].
- ▪
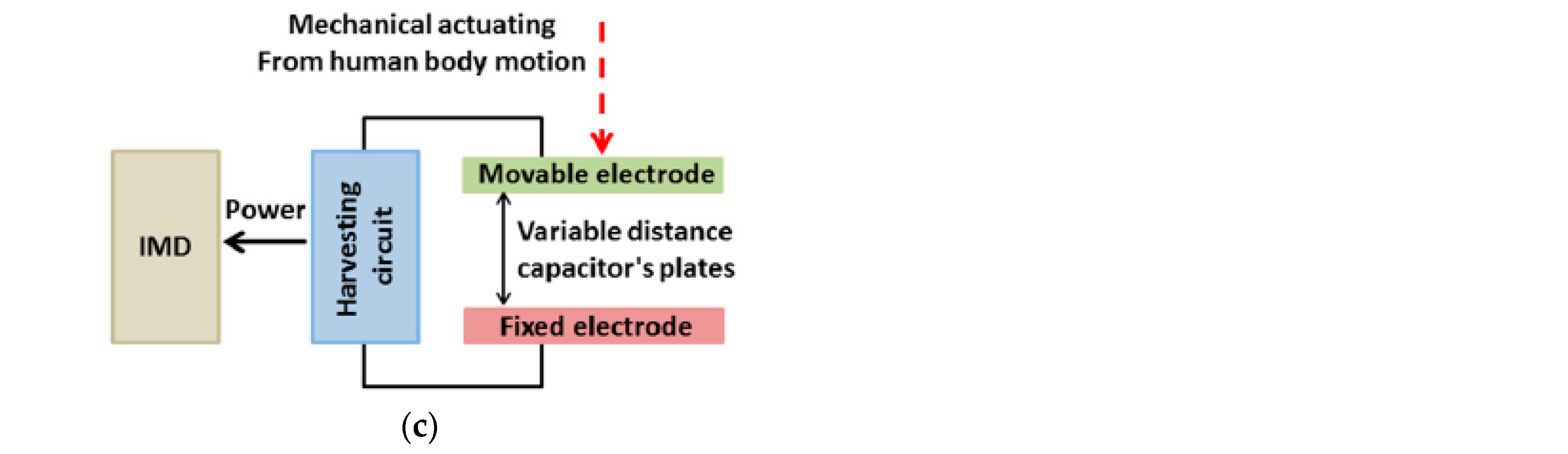
- There are also some other battery-less power system for implant antennas. For example thermoelectricity, piezoelectricity, and electrostatic generators. Although those provide microwatt-level power over a long time, biocompatibility and proper design are the major research challenges of those power source models.
- ▪
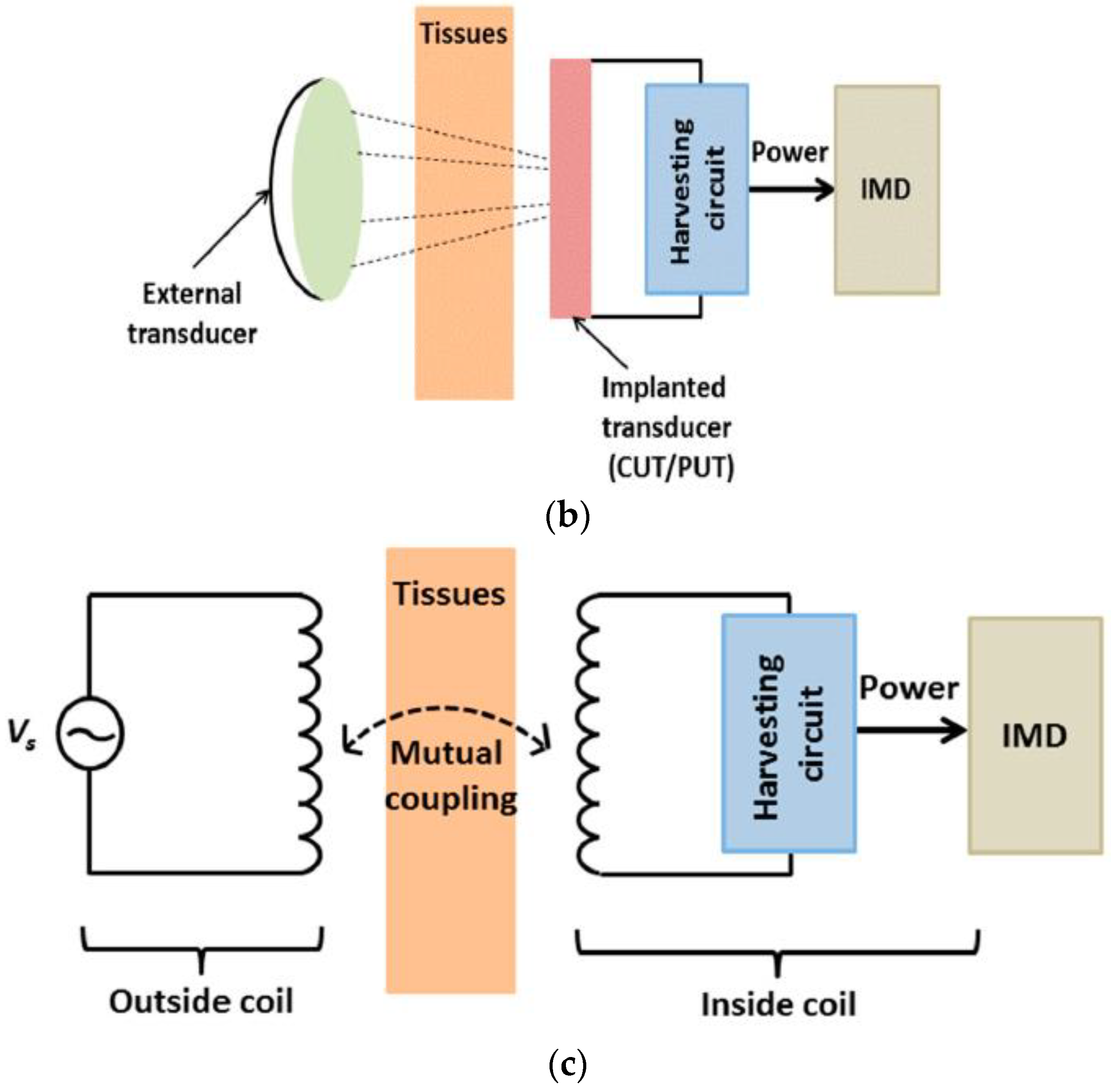
- Wireless power transfer is considered a promising solution in the implantable antenna power system [104]. Optical charging, ultrasonic transducers, and inductive coupling are the key examples of wireless power transfer in the implant antenna system to transfer milli-watt level power in the system. Nevertheless, during the power transfer with those systems, skin temperature rises, causing tissue damage and physical pain inside the body. Besides, there are limiting factors related to power transfer, which can reduce efficiency.
7. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chowdhury, M.E.; Khandakar, A.; Alzoubi, K.; Mansoor, S.; Tahir, A.M.; Reaz, M.B.I.; Al-Emadi, N. Real-time smart-digital stethoscope system for heart diseases monitoring. Sensors 2019, 19, 2781. [Google Scholar] [CrossRef]
- Chowdhury, M.E.; Alzoubi, K.; Khandakar, A.; Khallifa, R.; Abouhasera, R.; Koubaa, S.; Ahmed, R.; Hasan, A. Wearable real-time heart attack detection and warning system to reduce road accidents. Sensors 2019, 19, 2780. [Google Scholar] [CrossRef]
- Merli, F.; Bolomey, L.; Zurcher, J.-F.; Corradini, G.; Meurville, E.; Skrivervik, A.K. Design, realization and measurements of a miniature antenna for implantable wireless communication systems. IEEE Trans. Antennas Propag. 2011, 59, 3544–3555. [Google Scholar]
- Das, R.; Yoo, H. A multiband antenna associating wireless monitoring and nonleaky wireless power transfer system for biomedical implants. IEEE Trans. Microw. Theory Tech. 2017, 65, 2485–2495. [Google Scholar] [CrossRef]
- Skrivervik, A.K.; Merli, F. Design strategies for implantable antennas. In Proceedings of the 2011 Loughborough Antennas & Propagation Conference, Loughborough, UK, 14–15 November 2011; pp. 1–5. [Google Scholar]
- Scarpello, M.L.; Kurup, D.; Rogier, H.; Ginste, D.V.; Axisa, F.; Vanfleteren, J.; Joseph, W.; Martens, L.; Vermeeren, G. Design of an implantable slot dipole conformal flexible antenna for biomedical applications. IEEE Trans. Antennas Propag. 2011, 59, 3556–3564. [Google Scholar] [CrossRef]
- Liu, C.; Zhang, Y.; Liu, X. Circularly polarized implantable antenna for 915 MHz ISM-band far-field wireless power transmission. IEEE Antennas Wirel. Propag. Lett. 2018, 17, 373–376. [Google Scholar] [CrossRef]
- Loktongbam, P.; Pal, D.; Koley, C. Design of an implantable antenna for biotelemetry applications. Microsyst. Technol. 2019, 1–10. [Google Scholar] [CrossRef]
- Cil, E.; Dumanli, S. The Design of a Reconfigurable Slot Antenna Printed on Glass for Wearable Applications. IEEE Access 2020, 8, 95417–95423. [Google Scholar] [CrossRef]
- Merli, F. Implantable Antennas for Biomedical Applications. Ph.D. Thesis, Swiss Federal Institute of Technology (EPFL), Lausanne, Switzerland, September 2011. [Google Scholar]
- Kim, J.; Rahmat-Samii, Y. Implanted antennas inside a human body: Simulations, designs, and characterizations. IEEE Trans. Microw. Theory Tech. 2004, 52, 1934–1943. [Google Scholar] [CrossRef]
- Amar, A.B.; Kouki, A.B.; Cao, H. Power approaches for implantable medical devices. Sensors 2015, 15, 28889–28914. [Google Scholar] [CrossRef]
- Murakawa, K.; Kobayashi, M.; Nakamura, O.; Kawata, S. A wireless near-infrared energy system for medical implants. IEEE Eng. Med. Biol. Mag. 1999, 18, 70–72. [Google Scholar] [CrossRef] [PubMed]
- Parkhouse, L. Photovoltaic Powered Charging Apparatus for Implanted Rechargeable Batteries. U.S. Patent No. 7,003,353, 21 February 2006. [Google Scholar]
- Goto, K.; Nakagawa, T.; Nakamura, O.; Kawata, S. An implantable power supply with an optically rechargeable lithium battery. IEEE Trans. Biomed. Eng. 2001, 48, 830–833. [Google Scholar] [CrossRef]
- Banerji, S.; Goh, W.L.; Cheong, J.H.; Je, M. CMUT ultrasonic power link front-end for wireless power transfer deep in body. In Proceedings of the 2013 IEEE MTT-S International Microwave Workshop Series on RF and Wireless Technologies for Biomedical and Healthcare Applications (IMWS-BIO), Singapore, 9–11 December 2013; pp. 1–3. [Google Scholar]
- Conran, C.P. Antenna Designs for Wireless Medical Implants. Master’s Thesis, Technological University of Dublin, Ireland, September 2013. [Google Scholar]
- Fish & Richardson. Wireless Medical Technologies: Navigating Government Regulation in the New Medical Age; Fish & Richardson: Boston, MA, USA, 2017; pp. 1–36. [Google Scholar]
- European Communications Office. ERC Recommendation of 1997 on Relating to the Use of Short Range Devices (SRD), Latest Amended on 23 October 2020. Available online: https://docdb.cept.org/document/845 (accessed on 6 September 2019).
- Symeonidis, S.; Whittow, W.G.; Zecca, M.; Panagamuwa, C. Bone fracture monitoring using implanted antennas in the radius, tibia and phalange heterogeneous bone phantoms. Biomed. Phys. Eng. Express 2018, 4, 045006. [Google Scholar] [CrossRef]
- Murphy, O.H.; Bahmanyar, M.R.; Borghi, A.; McLeod, C.N.; Navaratnarajah, M.; Yacoub, M.H.; Toumazou, C. Continuous in vivo blood pressure measurements using a fully implantable wireless SAW sensor. Biomed. Microdevices 2013, 15, 737–749. [Google Scholar] [CrossRef]
- Dove, I. Analysis of Radio Propagation Inside the Human Body for in-Body Localization Purposes. Master’s Thesis, University of Twente, Enschede, The Netherlands, August 2014. [Google Scholar]
- Pozar, D.M. Microwave Engineering, 4th ed.; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2011. [Google Scholar]
- Andreuccetti, D.; Fossi, R.; Petrucci, C. An Internet Resource for the Calculation of the Dielectric Properties of Body Tissues in the Frequency Range 10 Hz–100 GHz. Available online: http://niremf.ifac.cnr.it/tissprop/ (accessed on 9 March 2021).
- Gabriel, S.; Lau, R.; Gabriel, C. The dielectric properties of biological tissues: II. Measurements in the frequency range 10 Hz to 20 GHz. Phys. Med. Biol. 1996, 41, 2251. [Google Scholar] [CrossRef]
- Furse, C.; Christensen, D.A.; Durney, C.H.; Nagel, J. Basic Introduction to Bioelectromagnetics, 3rd ed.; CRC Press: Boca Raton, FL, USA, 2018. [Google Scholar]
- Soontornpipit, P.; Furse, C.M.; Chung, Y.C. Design of implantable microstrip antenna for communication with medical implants. IEEE Trans. Microw. Theory Tech. 2004, 52, 1944–1951. [Google Scholar] [CrossRef]
- Piconi, C.; Maccauro, G. Zirconia as a ceramic biomaterial. Biomaterials 1999, 20, 1–25. [Google Scholar] [CrossRef]
- Abadia, J.; Merli, F.; Zürcher, J.; Mosig, J.R.; Skrivervik, A.K. 3D-spiral small antenna design and realization for biomedical telemetry in the MICS band. Radioengineering 2009, 18, 359–367. [Google Scholar]
- Karacolak, T.; Cooper, R.; Butler, J.; Fisher, S.; Topsakal, E. In vivo verification of implantable antennas using rats as model animals. IEEE Antennas Wirel. Propag. Lett. 2010, 9, 334–337. [Google Scholar] [CrossRef]
- Kneisz, L.; Schermann, M.; Unger, E.; Haller, M.; Krenn, M.; Mayr, W. The short-term effects of antenna insulation thickness on path losses in wireless telemetry implants at microwave frequencies. Eur. J. Transl. Myol. 2013, 23, 91–94. [Google Scholar] [CrossRef]
- Garcia Miquel, A. Antenna Design and Characterization for Biomedical Applications. Ph.D. Thesis, Department of Electronics and Biomedical Engineering, Universitat de Barcelona, Barcelona, Spain, June 2018. [Google Scholar]
- Balanis, C.A. Antenna Theory: Analysis and Design, 3rd ed.; John Wiley & Sons Inc: Hoboken, NJ, USA, 2015. [Google Scholar]
- Institute of Electrical and Electronics Engineers (IEEE). IEEE Standard for Safety Levels with Respect to Human Exposure to Electric, Magnetic, and Electromagnetic Fields, 0 Hz to 300 GHz; IEEE C95.1-2019/Cor 2-2020; Corrigenda 2; IEEE: Piscataway, NJ, USA, 2020. [Google Scholar]
- Institute of Electrical and Electronics Engineers (IEEE). IEEE Standard for Safety Levels with Respect to Human Exposure to Radio Frequency Electromagnetic Fields, 3 kHz to 300 GHz; IEEE C95.1-1991; IEEE: Piscataway, NJ, USA, 1992. [Google Scholar]
- Shadid, R.; Noghanian, S. A literature survey on wireless power transfer for biomedical devices. Int. J. Antennas Propag. 2018. [Google Scholar] [CrossRef]
- Sukhija, S.; Sarin, R.K. A U-shaped meandered slot antenna for biomedical applications. Prog. Electromagn. Res. 2017, 62, 65–77. [Google Scholar] [CrossRef]
- Samsuri, N.S.N.; Rahim, M.; Seman, F.; Inam, M. Compact Meander Line Telemetry Antenna for Implantable Pacemaker Applications. Indones. J. Electr. Eng. Comput. Sci. 2018, 10, 883–889. [Google Scholar]
- Alrawashdeh, R. A New Small Conformal Antenna for Capsule Endoscopy. In Proceedings of the 7th European Conference on Antennas and Propagation, EuCAP 2013, Gothenburg, Sweden, 8–12 April 2013; pp. 220–223. [Google Scholar]
- Faerber, J.; Desmulliez, M.P.Y. Conformal Meander Shaped Antenna for Biotelemetry in Endoscopic Capsules. In Proceedings of the Antennas & Propagation Conference (LAPC), Loughborough, UK, 2–3 November 2015. [Google Scholar] [CrossRef]
- Faerber, J.; Cummins, G.; Desmulliez, M.P.Y. Design of conformal wideband antennas for capsule endoscopy within a body tissue environment. In Proceedings of the 2016 46th European Microwave Conference (EuMC), London, UK, 4–6 October 2016; pp. 1223–1226. [Google Scholar] [CrossRef]
- Arefin, M.S.; Redoute, J.-M.; Yuce, M. Meandered conformai antenna for ISM-band ingestible capsule communication systems. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016. [Google Scholar]
- Kiourti1, A.; Psathas, K.; Costa, J.; Fernandes, C.; Nikita, K. Dual-Band Implantable Antennas for Medical Telemetry: A Fast Design Methodology and Validation for Intra-Cranial Pressure Monitoring. Prog. Electromagn. Res. 2013, 141, 161–183. [Google Scholar] [CrossRef]
- Tirkey, S.; Jha, N.; Pandeeswari, R.; Raghavan, S. Design of flexible meandered loop antennas loaded with CSRR and SRR for implantable applications. In Proceedings of the International Conference on Wireless Communications, Signal Processing and Networking, Chennai, India, 23–25 March 2016; pp. 1595–1598. [Google Scholar]
- Khan, M.; Moradi, E.; Sydänheimo, L.; Björninen, T.; Rahmat-Samii, Y.; Ukkonen, L. Miniature coplanar implantable antenna on thin and flexible platform for fully wireless intracranial pressure monitoring system. Int. J. Antennas Propag. 2017, 2017, 1–9. [Google Scholar] [CrossRef]
- Lee, J.; Seo, D.; Lee, H. Design of implantable rectangular spiral antenna for wireless biotelemetry in MICS band. Electron. Telecommun. Res. Inst. J. 2015, 37, 204–211. [Google Scholar] [CrossRef][Green Version]
- Liu, X.; Wu, Z.; Fan, Y.; Tentzeris, M.M. A miniaturized CSRR loaded wide-beamwidth circularly polarized implantable antenna for subcutaneous real-time glucose monitoring. IEEE Antennas Wirel. Propag. Lett. 2017, 16, 577–580. [Google Scholar] [CrossRef]
- Eldek, A.; Elhefnawi, F. Split Ring Resonator-Based Miniaturized Antennas. In Proceedings of the 28th National Radio Science Conference, Cairo, Egypt, 26–28 April 2011; pp. 1–7. [Google Scholar]
- Yamac, Y.; Basaran, S. A compact dual band implantable antenna based on split-ring resonators with meander line slots. In Proceedings of the 22nd International Conference on Applied Electromagnetics and Communications, Dubrovnik, Croatia, 19–22 September 2016; pp. 1–3. [Google Scholar]
- Gurdogan, O.; Eren, A.; Basaran, S. Multilayered implantable antenna design for biotelemetry communication. Turk. J. Electromech. Energy 2018, 3, 27–30. [Google Scholar]
- Lee, C.; Yo, T.; Luo, C.; Tu, C.; Juang, Y. Compact broadband stacked implantable antenna for biotelemetry with medical devices. Electron. Lett. 2007, 43, 660–662. [Google Scholar] [CrossRef]
- Lee, J.; Seo, D. Compact and tissue-insensitive implantable antenna on magneto-dielectric substrate for wireless biotelemetry. J. Electromagn. Waves Appl. 2019, 33, 2449–2461. [Google Scholar] [CrossRef]
- Miquel, A.; Curto, S.; Vidal, N.; Lopez-Villegas, J.; Ramos, J.; Prakash, P. Multilayered broadband antenna for compact embedded implantable medical devices: Design and characterization. Progr. Electromagn. Res. 2017, 159, 1–13. [Google Scholar] [CrossRef]
- Kiourti, A.; Nikita, K.S. Implantable Antennas: A Tutorial on Design, Fabrication, and In Vitro\/In Vivo Testing. IEEE Microw. Mag. 2014, 15, 77–91. [Google Scholar]
- Jain, L.; Singh, R.; Rawat, S.; Ray, K. Stacked arrangement of meandered patches for biomedical applications. Int. J. Syst. Assur. Eng. Manag. 2018, 9, 139–146. [Google Scholar] [CrossRef]
- Yeboah-Akowuah, B.; Kallos, E.; Palikaras, G.; Chen, Y.; Kosmas, P. A novel compact planar inverted-F antenna for biomedical applications in the MICS band. In Proceedings of the The 8th European Conference on Antennas and Propagation (EuCAP 2014), Hague, The Netherlands, 6–11 April 2014; pp. 822–824. [Google Scholar]
- Serhal, D.; Nasser, N.; Rammal, M.; Vaudon, P. Impact of Phone and Hand Position on SAR Distribution Using Liquid-Based PIFA Antenna. In Proceedings of the International conference on the Sciences of Electronics, Technologies of Information and Telecommunications, Hammamet, Tunisia, 20–22 December 2018; pp. 312–320. [Google Scholar]
- Harish, A.; Hidayat, M.R.; Nur, L.O.; Nugroho, B.S.; Munir, A. Spiral-shaped printed planar inverted-F antenna for body wearable application. In Proceedings of the 2017 11th International Conference on Telecommunication Systems Services and Applications (TSSA), Lombok, Indonesia, 26–27 October 2017; pp. 1–4. [Google Scholar]
- Sultana, S.; Miran, M.M.; Uddin, S.M.A.; Naby, M.M.; Haque, M. Performance analysis of a Mmodified implantable PIFA operates at MICS band for human head phantom model. In Proceedings of the 2017 3rd International Conference on Electrical Information and Communication Technology (EICT), Khulna, Bagladesh, 7–9 December 2017; pp. 1–5. [Google Scholar]
- Sultana, S.; Hasan, R.R.; Mondal, T.K.; Tusher, R.T.H.; Zabin, S. Performance analysis of body implantable PIFA at different substrate material. In Proceedings of the 2017 4th International Conference on Advances in Electrical Engineering (ICAEE), Dhaka, Bangladesh, 28–30 September 2017; pp. 68–73. [Google Scholar]
- Bouazizi, A.; Zaibi, G.; Samet, M.; Kachouri, A. A Miniaturized Invasive Antenna Study for a Better performance in Medical Application. In Proceedings of the 2018 32nd International Conference on Advanced Information Networking and Applications Workshops (WAINA), Grenbole, France, 8–12 June 2018; pp. 98–103. [Google Scholar]
- Sajjad, H.; Sethi, W.T.; Khan, S.; Jan, L. Compact dual-band implantable antenna for E-health monitoring. In Proceedings of the 2017 International Symposium on Wireless Systems and Networks (ISWSN), Lahore, Pakistan, 19–22 November 2017; pp. 1–4. [Google Scholar]
- Houzen, T.; Takahashi, M.; Saito, K.; Ito, K. Implanted planar inverted F-antenna for cardiac pacemaker system. In Proceedings of the 2008 International Workshop on Antenna Technology: Small Antennas and Novel Metamaterials, Santa Monica, CA, USA, 2–4 March 2008; pp. 346–349. [Google Scholar]
- Kiourti, A.; Christopoulou, M.; Koulouridis, S.; Nikita, K.S. Design of a novel miniaturized implantable PIFA for biomedical telemetry. In Proceedings of the International Conference on Wireless Mobile Communication and Healthcare, Ayia Napa, Cyprus, 18–20 October 2010; pp. 127–134. [Google Scholar]
- Merli, F.; Fuchs, B.; Mosig, J.R.; Skrivervik, A.K. The effect of insulating layers on the performance of implanted antennas. IEEE Trans. Antennas Propag. 2010, 59, 21–31. [Google Scholar]
- El-Saboni, Y.; Zelenchuk, D.; Conway, D.; Scanlon, W. Assessing the intrinsic radiation efficiency of tissue implanted UHF antennas. IEEE Trans. Antennas Propag. 2019, 68, 1–10. [Google Scholar] [CrossRef]
- Zhao, Y.; Rennaker, R.L.; Hutchens, C.; Ibrahim, T.S. Implanted miniaturized antenna for brain computer interface applications: Analysis and design. PLoS ONE 2014, 9, e103945. [Google Scholar] [CrossRef] [PubMed][Green Version]
- El-Saboni, Y.; Conway, G.A.; Scanlon, W.G. The importance of antenna near-field losses in intra-body UHF communication applications. In Proceedings of the 2017 IEEE International Symposium on Antennas and Propagation & USNC/URSI National Radio Science Meeting, San Diego, CA, USA, 9–14 July 2017; pp. 399–400. [Google Scholar]
- Bahrami, H.; Gosselin, B.; Rusch, L.A. Design of a miniaturized UWB antenna optimized for implantable neural recording systems. In Proceedings of the 10th IEEE International NEWCAS Conference, Montreal, QC, Canada, 17–20 June 2012; pp. 309–312. [Google Scholar]
- Yazdandoost, K.Y. A 2.4 GHz antenna for medical implanted communications. In Proceedings of the 2009 Asia Pacific Microwave Conference, Singapore, 7–10 December 2009; pp. 1775–1778. [Google Scholar]
- Bahrami, H.; Gosselin, B.; Rusch, L.A. Realistic modeling of the biological channel for the design of implantable wireless UWB communication systems. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; pp. 6015–6018. [Google Scholar]
- Cheng, X.; Senior, D.E.; Kim, C.; Yoon, Y.-K. A compact omnidirectional self-packaged patch antenna with complementary split-ring resonator loading for wireless endoscope applications. IEEE Antennas Wirel. Propag. Lett. 2011, 10, 1532–1535. [Google Scholar] [CrossRef]
- Baena, J.D.; Bonache, J.; Martín, F.; Sillero, R.M.; Falcone, F.; Lopetegi, T.; Laso, M.A.; Garcia-Garcia, J.; Gil, I.; Portillo, M.F. Equivalent-circuit models for split-ring resonators and complementary split-ring resonators coupled to planar transmission lines. IEEE Trans. Microw. Theory Tech. 2005, 53, 1451–1461. [Google Scholar] [CrossRef]
- Alrawashdeh, R.S.; Huang, Y.; Kod, M.; Sajak, A.A.B. A broadband flexible implantable loop antenna with complementary split ring resonators. IEEE Antennas Wirel. Propag. Lett. 2015, 14, 1506–1509. [Google Scholar] [CrossRef]
- Yang, Z.-J.; Xiao, S. A wideband implantable antenna for 2.4 GHz ISM band biomedical application. In Proceedings of the 2018 International Workshop on Antenna Technology (iWAT), Kuching, Malaysia, 24–26 July 2018; pp. 1–3. [Google Scholar]
- Tsai, C.-L.; Chen, K.-W.; Yang, C.-L. Implantable wideband low-specific-absorption-rate antenna on a thin flexible substrate. IEEE Antennas Wirel. Propag. Lett. 2015, 15, 1048–1052. [Google Scholar] [CrossRef]
- Nikolayev, D.; Zhadobov, M.; Karban, P.; Sauleau, R. Increasing the radiation efficiency and matching stability of in-body capsule antennas. In Proceedings of the 2016 10th European Conference on Antennas and Propagation (EuCAP), Abu Dhabi, United Arab Emirates, 14–16 November 2016; pp. 1–5. [Google Scholar]
- Ali, S.M.; Jeoti, V.; Saeidi, T.; Wen, W.P. Design of compact microstrip patch antenna for WBAN applications at ISM 2.4 GHz. Indones. J. Electr. Eng. Comput. Sci. 2019, 15, 1509–1516. [Google Scholar] [CrossRef]
- Basir, A.; Yoo, H. A stable impedance-matched ultrawideband antenna system mitigating detuning effects for multiple biotelemetric applications. IEEE Trans. Antennas Propag. 2019, 67, 3416–3421. [Google Scholar] [CrossRef]
- Bao, Z.; Guo, Y.-X.; Mittra, R. An ultrawideband conformal capsule antenna with stable impedance matching. IEEE Trans. Antennas Propag. 2017, 65, 5086–5094. [Google Scholar] [CrossRef]
- Symeonidis, S.; Whittow, W.G.; Panagamuwa, C.; Zecca, M. An implanted antenna system for the monitoring of the healing of bone fractures. In Proceedings of the 2015 Loughborough Antennas & Propagation Conference (LAPC), Loughborough, UK, 2–3 November 2015; pp. 1–4. [Google Scholar]
- Gabriel, C. Compilation of the Dielectric Properties of Body Tissues at RF and Microwave Frequencies; King’s Coll London (United Kingdom) Department of Physics: London, UK, 1996. [Google Scholar]
- Ming-Kuei, H. Fresnel region field distributions of circular aperture antennas. IRE Trans. Antennas Propag. 1960, 8, 344–346. [Google Scholar] [CrossRef]
- Afroz, S.; Thomas, S.W.; Mumcu, G.; Locke, C.W.; Saddow, S.E. A Biocompatible SiC RF Antenna for In-vivo Sensing Applications. MRS Online Proc. Libr. 2012, 1433, 119–124. [Google Scholar] [CrossRef]
- Hout, S.; Chung, J.-Y. Design and Characterization of a Miniaturized Implantable Antenna in a Seven-Layer Brain Phantom. IEEE Access 2019, 7, 162062–162069. [Google Scholar] [CrossRef]
- Kiourti, A.; Christopoulou, M.; Nikita, K.S. Performance of a novel miniature antenna implanted in the human head for wireless biotelemetry. In Proceedings of the 2011 IEEE International Symposium on Antennas and Propagation (APSURSI), Spokane, WA, USA, 3–8 July 2011; pp. 392–395. [Google Scholar]
- Karacolak, T.; Hood, A.Z.; Topsakal, E. Design of a dual-band implantable antenna and development of skin mimicking gels for continuous glucose monitoring. IEEE Trans. Microw. Theory Tech. 2008, 56, 1001–1008. [Google Scholar] [CrossRef]
- Ito, K.; Furuya, K.; Okano, Y.; Hamada, L. Development and characteristics of a biological tissue-equivalent phantom for microwaves. Electron. Commun. Jpn. (Part. I Commun.) 2001, 84, 67–77. [Google Scholar] [CrossRef]
- Kiourti, A.; Costa, J.R.; Fernandes, C.A.; Nikita, K.S. A broadband implantable and a dual-band on-body repeater antenna: Design and transmission performance. IEEE Trans. Antennas Propag. 2014, 62, 2899–2908. [Google Scholar] [CrossRef]
- Kiourti, A.; Costa, J.R.; Fernandes, C.A.; Santiago, A.G.; Nikita, K.S. Miniature implantable antennas for biomedical telemetry: From simulation to realization. IEEE Trans. Biomed. Eng. 2012, 59, 3140–3147. [Google Scholar] [CrossRef]
- Wei, X.; Liu, J. Power sources and electrical recharging strategies for implantable medical devices. Front. Energy Power Eng. China 2008, 2, 1–13. [Google Scholar] [CrossRef]
- Mano, N.; Mao, F.; Heller, A. Characteristics of a miniature compartment-less glucose−O2 biofuel cell and its operation in a living plant. J. Am. Chem. Soc. 2003, 125, 6588–6594. [Google Scholar] [CrossRef]
- Bullen, R.A.; Arnot, T.; Lakeman, J.; Walsh, F. Biofuel cells and their development. Biosens. Bioelectron. 2006, 21, 2015–2045. [Google Scholar] [CrossRef] [PubMed]
- Stark, I.; Stordeur, M. New micro thermoelectric devices based on bismuth telluride-type thin solid films. In Proceedings of the Eighteenth International Conference on Thermoelectrics. Proceedings, ICT’99 (Cat. No. 99TH8407), Baltimore, MD, USA, 29 August–2 September 1999; pp. 465–472. [Google Scholar]
- Settaluri, K.T.; Lo, H.; Ram, R.J. Thin thermoelectric generator system for body energy harvesting. J. Electron. Mater. 2012, 41, 984–988. [Google Scholar] [CrossRef]
- Niu, P.; Chapman, P.; Riemer, R.; Zhang, X. Evaluation of motions and actuation methods for biomechanical energy harvesting. In Proceedings of the 2004 IEEE 35th Annual Power Electronics Specialists Conference (IEEE Cat. No. 04CH37551), Aachen, Germany, 20–25 June 2004; pp. 2100–2106. [Google Scholar]
- Sohn, J.; Choi, S.B.; Lee, D. An investigation on piezoelectric energy harvesting for MEMS power sources. Proc. Inst. Mech. Eng. Part. C J. Mech. Eng. Sci. 2005, 219, 429–436. [Google Scholar] [CrossRef]
- Miyazaki, M.; Tanaka, H.; Ono, G.; Nagano, T.; Ohkubo, N.; Kawahara, T. Electric-energy generation through variable-capacitive resonator for power-free LSI. IEICE Trans. Electron. 2004, 87, 549–555. [Google Scholar]
- Tashiro, R.; Kabei, N.; Katayama, K.; Tsuboi, E.; Tsuchiya, K. Development of an electrostatic generator for a cardiac pacemaker that harnesses the ventricular wall motion. J. Artif. Organs 2002, 5, 0239–0245. [Google Scholar] [CrossRef]
- Christensen, D.B.; Roundy, S. Ultrasonically powered piezoelectric generators for bio-implantable sensors: Plate versus diaphragm. J. Intell. Mater. Syst. Struct. 2016, 27, 1092–1105. [Google Scholar] [CrossRef]
- Phillips, W.; Towe, B.; Larson, P. An ultrasonically-driven piezoelectric neural stimulator. In Proceedings of the 25th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (IEEE Cat. No. 03CH37439), Cancun, Mexico, 17–21 September 2003; pp. 1983–1986. [Google Scholar]
- Parramon, J.; Doguet, P.; Marin, D.; Verleyssen, M.; Munoz, R.; Leija, L.; Valderrama, E. ASIC-based batteryless implantable telemetry microsystem for recording purposes. In Proceedings of the 19th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. Magnificent Milestones and Emerging Opportunities in Medical Engineering (Cat. No. 97CH36136), Chicago, IL, USA, 30 October–2 November 1997; pp. 2225–2228. [Google Scholar]
- Vidal, N.; Curto, S.; Lopez-Villegas, J.M.; Sieiro, J.; Ramos, F.M. Detuning study of implantable antennas inside the human body. Prog. Electromagn. Res. 2012, 124, 265–283. [Google Scholar] [CrossRef]
- Qiblawey, Y.; Chowdhury, M.E.H.; Musharavati, F.; Zalnezhad, E.; Khandakar, A.; Islam, M.T. Instrumented Hip Implant: A Review. IEEE Sens. J. 2021, 21, 7179–7194. [Google Scholar] [CrossRef]
















Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soliman, M.M.; Chowdhury, M.E.H.; Khandakar, A.; Islam, M.T.; Qiblawey, Y.; Musharavati, F.; Zal Nezhad, E. Review on Medical Implantable Antenna Technology and Imminent Research Challenges. Sensors 2021, 21, 3163. https://doi.org/10.3390/s21093163
Soliman MM, Chowdhury MEH, Khandakar A, Islam MT, Qiblawey Y, Musharavati F, Zal Nezhad E. Review on Medical Implantable Antenna Technology and Imminent Research Challenges. Sensors. 2021; 21(9):3163. https://doi.org/10.3390/s21093163
Chicago/Turabian StyleSoliman, Md Mohiuddin, Muhammad E. H. Chowdhury, Amith Khandakar, Mohammad Tariqul Islam, Yazan Qiblawey, Farayi Musharavati, and Erfan Zal Nezhad. 2021. "Review on Medical Implantable Antenna Technology and Imminent Research Challenges" Sensors 21, no. 9: 3163. https://doi.org/10.3390/s21093163
APA StyleSoliman, M. M., Chowdhury, M. E. H., Khandakar, A., Islam, M. T., Qiblawey, Y., Musharavati, F., & Zal Nezhad, E. (2021). Review on Medical Implantable Antenna Technology and Imminent Research Challenges. Sensors, 21(9), 3163. https://doi.org/10.3390/s21093163










