Long-Term IoT-Based Maternal Monitoring: System Design and Evaluation
Abstract
1. Introduction
- We present a feasible long-term IoT-based maternal monitoring system used during pregnancy and postpartum. We investigate both system level and user level requirements (e.g., energy efficiency and feasibility) to enhance user experience.
- We implemented a proof-of-concept monitoring system for a real human subject study.
- We analyzed and evaluated the challenges in implementing such monitoring systems, including feasibility, reliability, energy efficiency and integration of the presented system with the current healthcare system.
- We integrated AI-based methods previously proposed by the authors into the presented system in a holistic way for analyzing the data and providing monitoring services.
2. Related Work
3. Long-Term IoT-Based Maternal Monitoring Services
3.1. Physical Activity Monitoring
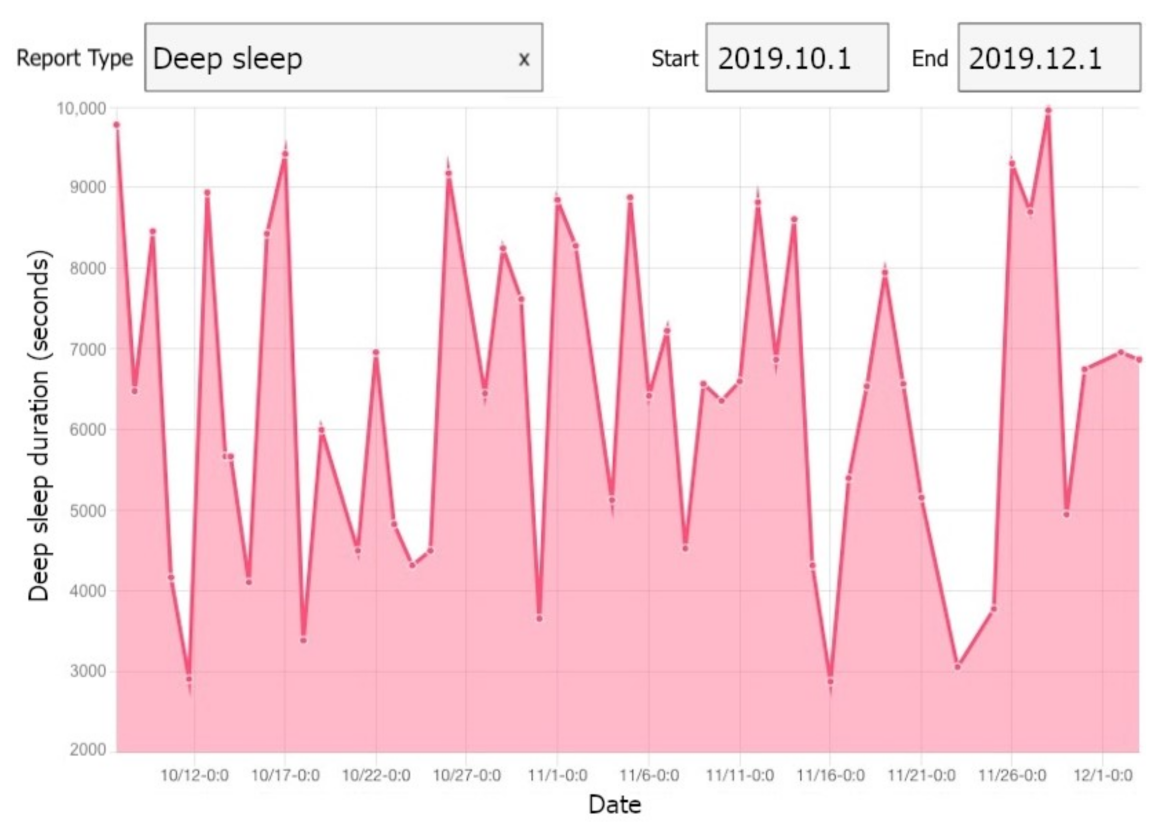
3.2. Sleep Monitoring
3.3. Stress Monitoring
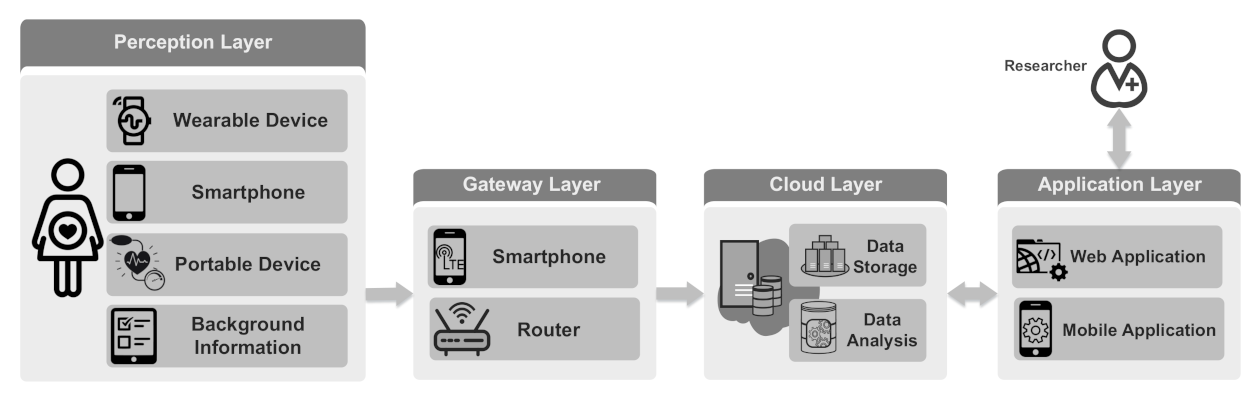
4. Maternal Health and Well-Being Monitoring System
4.1. Perception Layer
4.1.1. Wearable Devices
4.1.2. Smartphone
4.1.3. Portable Devices for Periodic Monitoring
4.1.4. Background and Demographic Information
4.2. Gateway Layer
4.3. Cloud Layer
4.4. Application Layer
5. Implementation
5.1. Perception Layer
5.1.1. Wearable Devices
5.1.2. Smartphone
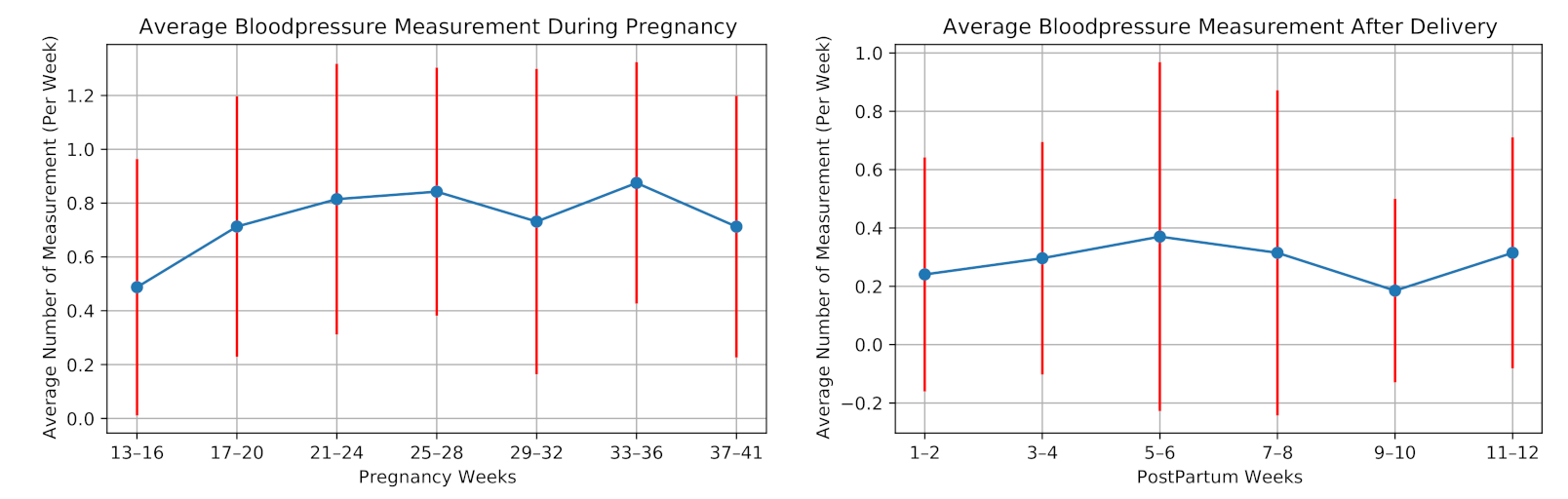
5.1.3. Portable Devices for Periodic Monitoring
5.1.4. Background and Demographic Information
5.2. Gateway Layer
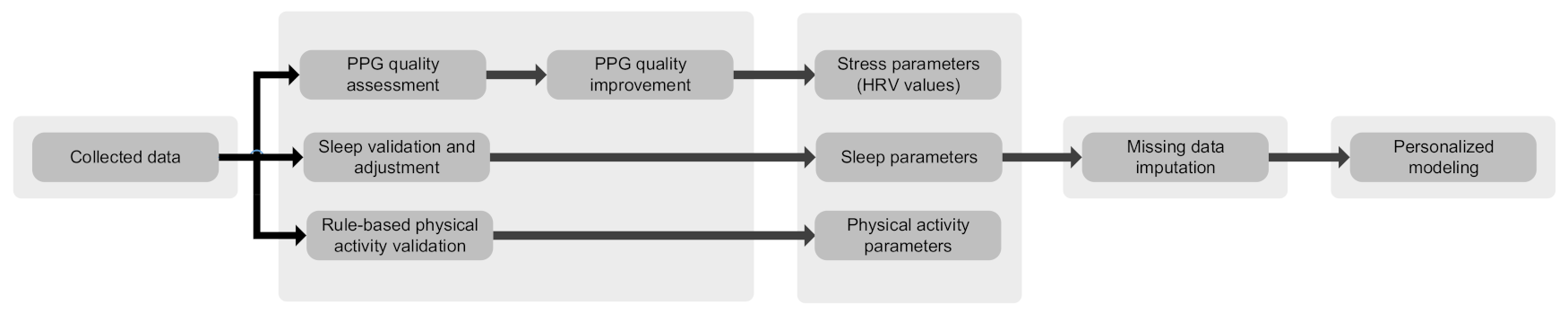
5.3. Cloud Layer
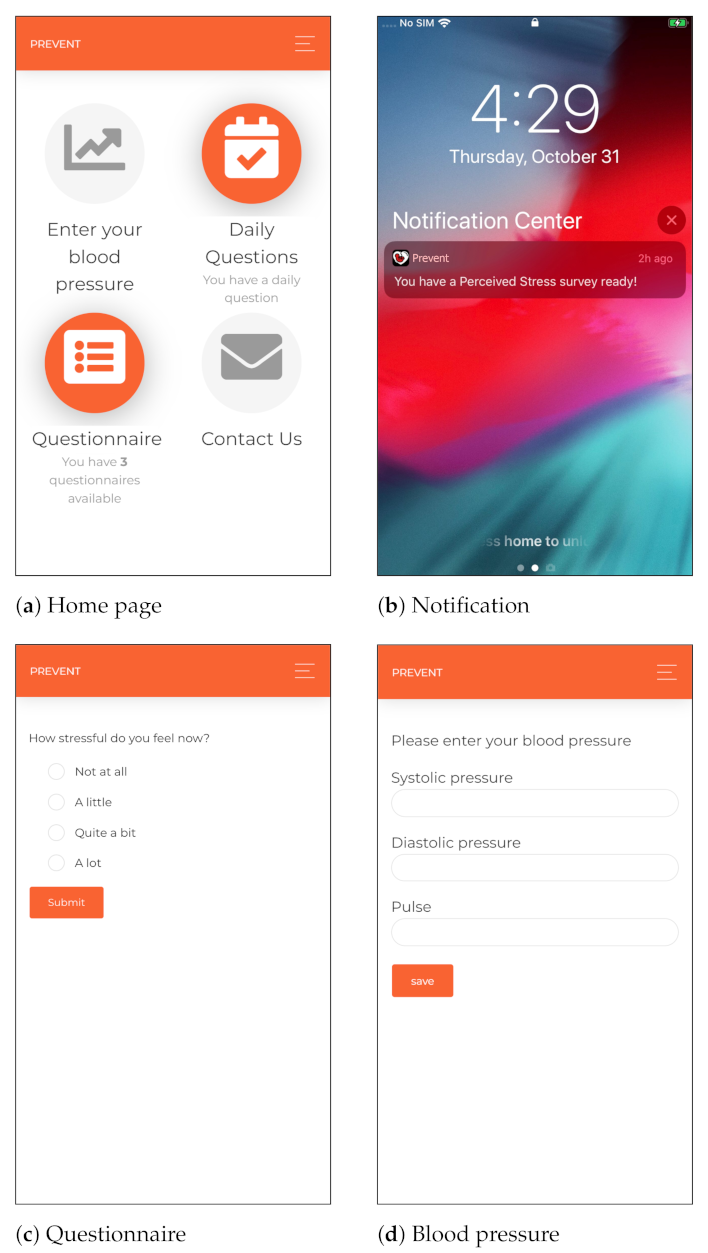
5.4. Application Layer
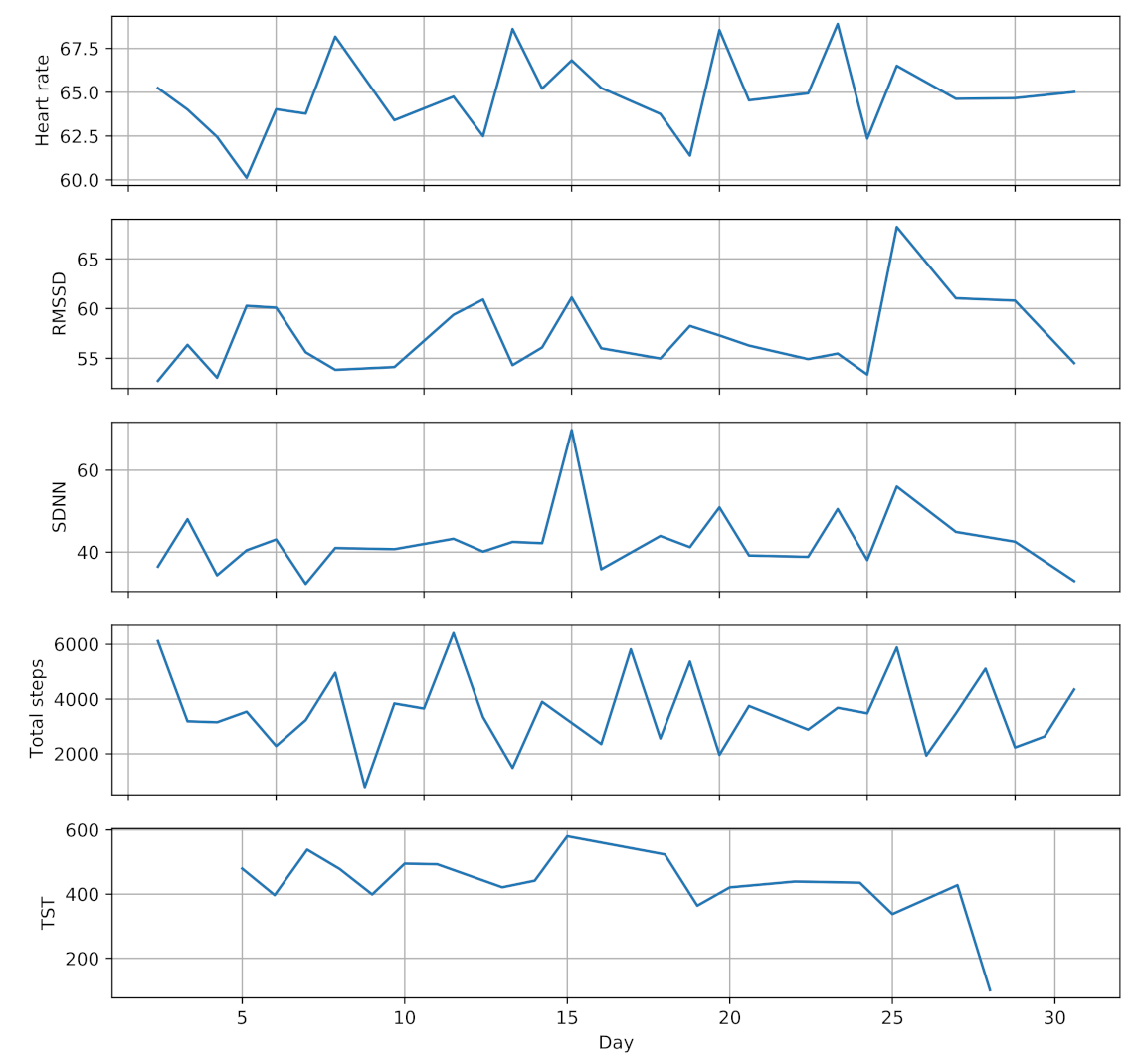
6. Evaluation and Discussion
6.1. Feasibility
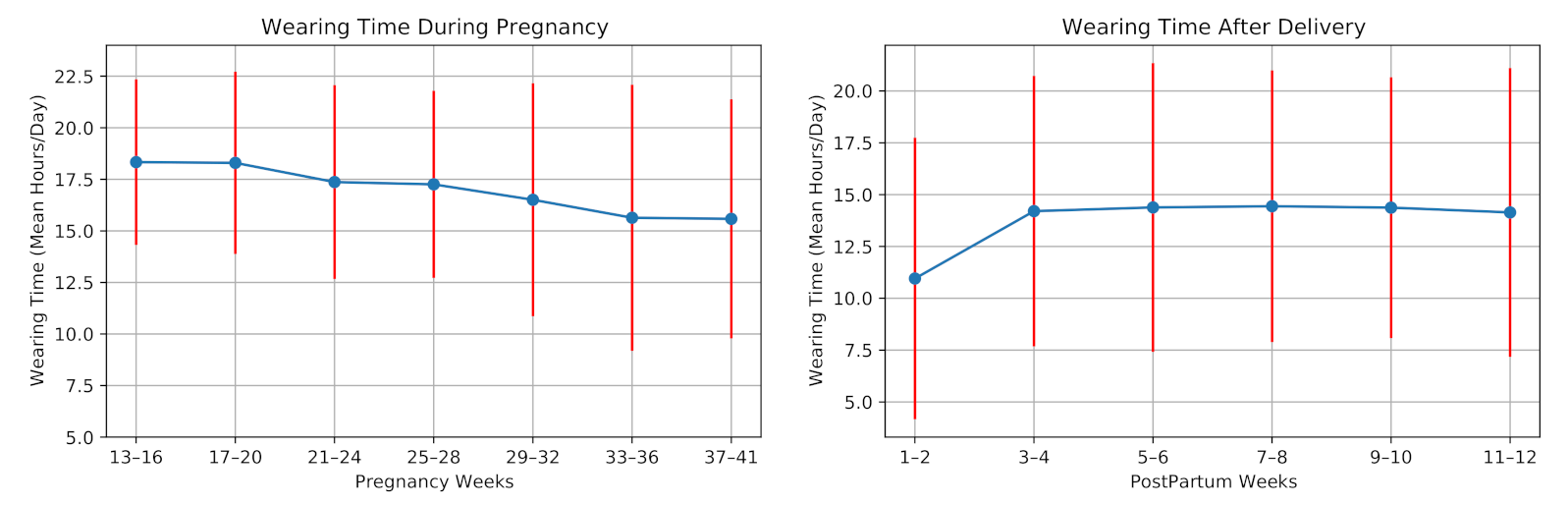
6.1.1. Wearable Device Usage
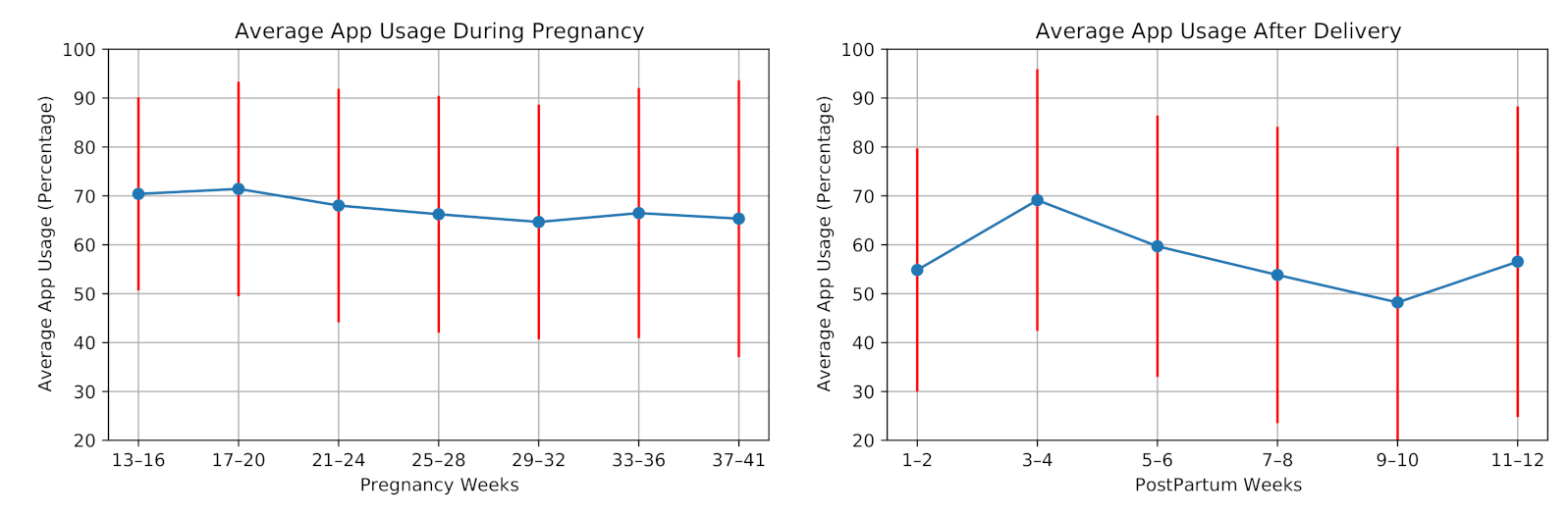
6.1.2. Cross-Platform Mobile Application Usage
6.2. Robustness and Reliability of Measurement
6.2.1. Duration of PPG Signal Recording
- Twenty-four-hour recordings (referred as long-term HRV analysis) are used to derive HRV parameters.
- Five-minute recordings (referred as short-term HRV analysis) are utilized to obtain HRV parameters.
- Less-than-five-minute recordings (referred as ultra-short-term HRV analysis) are exploited to extract some of the HRV parameters.
6.2.2. Sampling Frequency of the PPG Signal
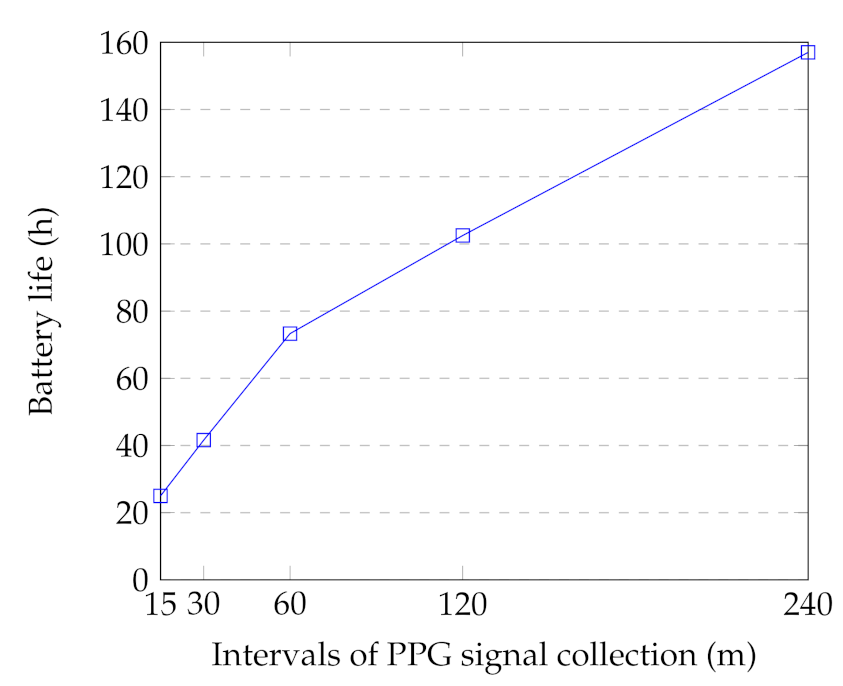
6.3. Energy Consumption
6.4. Practical Challenges
6.5. Integration to The Current Healthcare System
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sharma, S.; Sidhu, H.; Kaur, S. Analytical study of intrauterine fetal death cases and associated maternal conditions. Int. J. Appl. Basic Med. Res. 2016, 6, 11. [Google Scholar] [CrossRef]
- Gilmore, L.A.; Klempel-Donchenko, M.; Redman, L.M. Pregnancy as a window to future health: Excessive gestational weight gain and obesity. In Seminars in Perinatology; Elsevier: Amsterdam, The Netherlands, 2015; Volume 39, pp. 296–303. [Google Scholar]
- Puhkala, J.; Raitanen, J.; Kolu, P.; Tuominen, P.; Husu, P.; Luoto, R. Metabolic syndrome in Finnish women 7 years after a gestational diabetes prevention trial. BMJ Open 2017, 7, e014565. [Google Scholar] [CrossRef] [PubMed]
- WHO. Maternal Mortality; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Klemetti, R.; Hakulinen-Viitanen, T. Handbook for Finnish Maternity Health Clinics. Recommendations for Practices [In Finnish] Äitiysneuvolaopas. Suosituksia äitiysneuvolatoimintaan; National Institute for Health and Welfare: Helsinki, Finland, 2013.
- Grym, K.; Niela-Vilén, H.; Ekholm, E.; Hamari, L.; Azimi, I.; Rahmani, A.; Liljeberg, P.; Löyttyniemi, E.; Axelin, A. Feasibility of smart wristbands for continuous monitoring during pregnancy and one month after birth. BMC Pregnancy Childbirth 2019, 19, 34. [Google Scholar] [CrossRef]
- Phillips, S.M.; Cadmus-Bertram, L.; Rosenberg, D.; Buman, M.P.; Lynch, B.M. Wearable technology and physical activity in chronic disease: Opportunities and challenges. Am. J. Prev. Med. 2018, 54, 144. [Google Scholar] [CrossRef]
- Steinhubl, S.R.; Muse, E.D.; Topol, E.J. The emerging field of mobile health. Sci. Transl. Med. 2015, 7, 283rv3. [Google Scholar] [CrossRef]
- Hassanalieragh, M.; Page, A.; Soyata, T.; Sharma, G.; Aktas, M.; Mateos, G.; Kantarci, B.; Andreescu, S. Health monitoring and management using Internet-of-Things (IoT) sensing with cloud-based processing: Opportunities and challenges. In Proceedings of the 2015 IEEE International Conference on Services Computing, New York, NY, USA, 27 June–2 July 2015; pp. 285–292. [Google Scholar]
- Gubbi, J.; Buyya, R.; Marusic, S.; Palaniswami, M. Internet of Things (IoT): A vision, architectural elements, and future directions. Future Gener. Comput. Syst. 2013, 29, 1645–1660. [Google Scholar] [CrossRef]
- Atzori, L.; Iera, A.; Morabito, G. The internet of things: A survey. Comput. Netw. 2010, 54, 2787–2805. [Google Scholar] [CrossRef]
- Lanssens, D.; Vandenberk, T.; Smeets, C.J.; De Cannière, H.; Vonck, S.; Claessens, J.; Heyrman, Y.; Vandijck, D.; Storms, V.; Thijs, I.M.; et al. Prenatal remote monitoring of women with gestational hypertensive diseases: Cost analysis. J. Med. Internet Res. 2018, 20, e102. [Google Scholar] [CrossRef]
- Kumar, S.; Gupta, Y.; Mago, V. Health-monitoring of pregnant women: Design requirements, and proposed reference architecture. In Proceedings of the 2019 16th IEEE Annual Consumer Communications & Networking Conference (CCNC), Las Vegas, NV, USA, 11–14 January 2019; pp. 1–6. [Google Scholar]
- Allahem, H.; Sampalli, S. Framework to monitor pregnant women with a high risk of premature labour using sensor networks. In Proceedings of the 2017 IFIP/IEEE Symposium on Integrated Network and Service Management (IM), Lisbon, Portugal, 8–12 May 2017; pp. 1178–1181. [Google Scholar]
- Tsai, S.Y.; Lee, P.L.; Lin, J.W.; Lee, C.N. Cross-sectional and longitudinal associations between sleep and health-related quality of life in pregnant women: A prospective observational study. Int. J. Nurs. Stud. 2016, 56, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Misri, S.; Kendrick, K.; Oberlander, T.F.; Norris, S.; Tomfohr, L.; Zhang, H.; Grunau, R.E. Antenatal depression and anxiety affect postpartum parenting stress: A longitudinal, prospective study. Can. J. Psychiatry 2010, 55, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Setse, R.; Grogan, R.; Pham, L.; Cooper, L.A.; Strobino, D.; Powe, N.R.; Nicholson, W. Longitudinal study of depressive symptoms and health-related quality of life during pregnancy and after delivery: The Health Status in Pregnancy (HIP) study. Matern. Child Health J. 2009, 13, 577–587. [Google Scholar] [CrossRef] [PubMed]
- Landry, G.J.; Best, J.R.; Liu-Ambrose, T. Measuring sleep quality in older adults: A comparison using subjective and objective methods. Front. Aging Neurosci. 2015, 7, 166. [Google Scholar] [CrossRef] [PubMed]
- Kalafat, E.; Leslie, K.; Bhide, A.; Thilaganathan, B.; Khalil, A. Pregnancy outcomes following home blood pressure monitoring in gestational hypertension. Pregnancy Hypertens. 2019, 18, 14–20. [Google Scholar] [CrossRef]
- Marko, K.I.; Krapf, J.M.; Meltzer, A.C.; Oh, J.; Ganju, N.; Martinez, A.G.; Sheth, S.G.; Gaba, N.D. Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: A prospective observational trial. JMIR Res. Protoc. 2016, 5, e200. [Google Scholar] [CrossRef] [PubMed]
- Azimi, I.; Oti, O.; Labbaf, S.; Niela-Vilén, H.; Axelin, A.; Dutt, N.; Liljeberg, P.; Rahmani, A.M. Personalized Maternal Sleep Quality Assessment: An Objective IoT-based Longitudinal Study. IEEE Access 2019, 7, 93433–93447. [Google Scholar] [CrossRef]
- Saarikko, J.; Niela-Vilen, H.; Ekholm, E.; Hamari, L.; Azimi, I.; Liljeberg, P.; Rahmani, A.M.; Löyttyniemi, E.; Axelin, A. Continuous 7-month Internet of Things -based monitoring of Health Parameters of Pregnant and Postpartum Women: A Feasibility Study. JMIR Form. Res. 2020, 4, e12417. [Google Scholar] [CrossRef]
- Moreira, M.W.; Rodrigues, J.J.; Oliveira, A.M.; Saleem, K. Smart mobile system for pregnancy care using body sensors. In Proceedings of the 2016 International Conference on Selected Topics in Mobile & Wireless Networking (MoWNeT), Cairo, Egypt, 11–13 April 2016; pp. 1–4. [Google Scholar]
- Meyer, J.; Beck, E.; Wasmann, M.; Boll, S. Making sense in the long run: Long-term health monitoring in real lives. In Proceedings of the 2017 IEEE International Conference on Healthcare Informatics (ICHI), Park City, UT, USA, 23–26 August 2017; pp. 285–294. [Google Scholar]
- Hamari, L.; Kullberg, T.; Ruohonen, J.; Heinonen, O.J.; Díaz-Rodríguez, N.; Lilius, J.; Pakarinen, A.; Myllymäki, A.; Leppänen, V.; Salanterä, S. Physical activity among children: Objective measurements using Fitbit One® and ActiGraph. BMC Res. Notes 2017, 10, 1–6. [Google Scholar] [CrossRef]
- Anzanpour, A.; Amiri, D.; Azimi, I.; Levorato, M.; Dutt, N.; Liljeberg, P.; Rahmani, A.M. Edge-Assisted Control for Healthcare Internet of Things: A Case Study on PPG-Based Early Warning Score. ACM Trans. Internet Things 2020, 2, 1–21. [Google Scholar] [CrossRef]
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable sensors for remote health monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef]
- Memon, M.; Wagner, S.R.; Pedersen, C.F.; Beevi, F.H.A.; Hansen, F.O. Ambient assisted living healthcare frameworks, platforms, standards, and quality attributes. Sensors 2014, 14, 4312–4341. [Google Scholar] [CrossRef]
- Azimi, I.; Anzanpour, A.; Rahmani, A.M.; Pahikkala, T.; Levorato, M.; Liljeberg, P.; Dutt, N. HiCH: Hierarchical fog-assisted computing architecture for healthcare IoT. ACM Trans. Embed. Comput. Syst. (TECS) 2017, 16, 1–20. [Google Scholar] [CrossRef]
- Naeini, E.K.; Azimi, I.; Rahmani, A.M.; Liljeberg, P.; Dutt, N. A real-time PPG quality assessment approach for healthcare Internet-of-Things. Procedia Comput. Sci. 2019, 151, 551–558. [Google Scholar] [CrossRef]
- Azimi, I.; Pahikkala, T.; Rahmani, A.M.; Niela-Vilén, H.; Axelin, A.; Liljeberg, P. Missing data resilient decision-making for healthcare IoT through personalization: A case study on maternal health. Future Gener. Comput. Syst. 2019, 96, 297–308. [Google Scholar] [CrossRef]
- Hedman, C.; Pohjasvaara, T.; Tolonen, U.; Suhonen-Malm, A.; Myllylä, V. Effects of pregnancy on mothers’ sleep. Sleep Med. 2002, 3, 37–42. [Google Scholar] [CrossRef]
- Lopez, B.D.B.; Aguirre, J.A.A.; Coronado, D.A.R.; Gonzalez, P.A. Wearable technology model to control and monitor hypertension during pregnancy. In Proceedings of the 2018 13th Iberian Conference on Information Systems and Technologies (CISTI), Caceres, Spain, 13–16 June 2018; pp. 1–6. [Google Scholar]
- Polsky, S.; Garcetti, R. CGM, pregnancy, and remote monitoring. Diabetes Technol. Ther. 2017, 19, S49–S59. [Google Scholar] [CrossRef] [PubMed]
- Krapf, J.M.; Gaba, N.D.; Ganju, N.; Marko, K.I.; Martinez, A.G. Remote Capture and Monitoring of Clinical Data During Pregnancy. Obstet. Gynecol. 2015, 125, 26S. [Google Scholar] [CrossRef]
- Rubens, C.E.; Sadovsky, Y.; Muglia, L.; Gravett, M.G.; Lackritz, E.; Gravett, C. Prevention of preterm birth: Harnessing science to address the global epidemic. Sci. Transl. Med. 2014, 6, 262sr5. [Google Scholar] [CrossRef]
- Sentilhes, L.; Sénat, M.V.; Ancel, P.Y.; Azria, E.; Benoist, G.; Blanc, J.; Brabant, G.; Bretelle, F.; Brun, S.; Doret, M.; et al. Prevention of spontaneous preterm birth: Guidelines for clinical practice from the French College of Gynaecologists and Obstetricians (CNGOF). Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 210, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Fazal, N.; Webb, A.; Bangoura, J.; El Nasharty, M. Telehealth: Improving maternity services by modern technology. BMJ Open Qual. 2020, 9, e000895. [Google Scholar] [CrossRef] [PubMed]
- Niela-Vilen, H.; Rahmani, A.; Liljeberg, P.; Axelin, A. Being ‘A Google Mom’ or securely monitored at home: Perceptions of remote monitoring in maternity care. J. Adv. Nurs. 2020, 76, 243–252. [Google Scholar] [CrossRef]
- Evenson, K.R.; Barakat, R.; Brown, W.J.; Dargent-Molina, P.; Haruna, M.; Mikkelsen, E.M.; Mottola, M.F.; Owe, K.M.; Rousham, E.K.; Yeo, S. Guidelines for physical activity during pregnancy: Comparisons from around the world. Am. J. Lifestyle Med. 2014, 8, 102–121. [Google Scholar] [CrossRef]
- Barakat, R.; Pelaez, M.; Lopez, C.; Montejo, R.; Coteron, J. Exercise during pregnancy reduces the rate of cesarean and instrumental deliveries: Results of a randomized controlled trial. J. Matern.-Fetal Neonatal Med. 2012, 25, 2372–2376. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, S.L.; Surita, F.G.; Godoy, A.C.; Kasawara, K.T.; Morais, S.S. Physical activity patterns and factors related to exercise during pregnancy: A cross sectional study. PLoS ONE 2015, 10, e0128953. [Google Scholar]
- Coll, C.d.V.N.; Domingues, M.R.; Hallal, P.C.; da Silva, I.C.M.; Bassani, D.G.; Matijasevich, A.; Barros, A.; Santos, I.S.; Bertoldi, A.D. Changes in leisure-time physical activity among Brazilian pregnant women: Comparison between two birth cohort studies (2004–2015). BMC Public Health 2017, 17, 119. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Mao, J.; Ye, Z.; Zeng, X.; Zhao, H.; Liu, Y.; Li, J. Determinants of sleep quality among pregnant women in China: A cross-sectional survey. J. Matern.-Fetal Neonatal Med. 2018, 31, 2980–2985. [Google Scholar] [CrossRef]
- Mindell, J.A.; Cook, R.A.; Nikolovski, J. Sleep patterns and sleep disturbances across pregnancy. Sleep Med. 2015, 16, 483–488. [Google Scholar] [CrossRef]
- Felder, J.N.; Baer, R.J.; Rand, L.; Jelliffe-Pawlowski, L.L.; Prather, A.A. Sleep disorder diagnosis during pregnancy and risk of preterm birth. Obstet. Gynecol. 2017, 130, 573–581. [Google Scholar] [CrossRef]
- Herring, S.J.; Nelson, D.B.; Pien, G.W.; Homko, C.; Goetzl, L.M.; Davey, A.; Foster, G.D. Objectively measured sleep duration and hyperglycemia in pregnancy. Sleep Med. 2014, 15, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Bei, B.; Coo, S.; Trinder, J. Sleep and mood during pregnancy and the postpartum period. Sleep Med. Clin. 2015, 10, 25–33. [Google Scholar] [CrossRef]
- Westerterp-Plantenga, M.S. Sleep, circadian rhythm and body weight: Parallel developments. Proc. Nutr. Soc. 2016, 75, 431–439. [Google Scholar] [CrossRef]
- Goletzke, J.; Kocalevent, R.D.; Hansen, G.; Rose, M.; Becher, H.; Hecher, K.; Arck, P.; Diemert, A. Prenatal stress perception and coping strategies: Insights from a longitudinal prospective pregnancy cohort. J. Psychosom. Res. 2017, 102, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Alderdice, F.; Lynn, F.; Lobel, M. A review and psychometric evaluation of pregnancy-specific stress measures. J. Psychosom. Obstet. Gynecol. 2012, 33, 62–77. [Google Scholar] [CrossRef]
- Korhonen, L.S.; Kortesluoma, S.; Lukkarinen, M.; Peltola, V.; Pesonen, H.; Pelto, J.; Tuulari, J.J.; Lukkarinen, H.; Vuorinen, T.; Karlsson, H.; et al. Prenatal maternal distress associates with a blunted cortisol response in rhinovirus-positive infants. Psychoneuroendocrinology 2019, 107, 187–190. [Google Scholar] [CrossRef]
- Hakanen, H.; Flykt, M.; Sinervä, E.; Nolvi, S.; Kataja, E.L.; Pelto, J.; Karlsson, H.; Karlsson, L.; Korja, R. How maternal pre-and postnatal symptoms of depression and anxiety affect early mother-infant interaction? J. Affect. Disord. 2019, 257, 83–90. [Google Scholar] [CrossRef]
- Rahmani, A.M.; Liljeberg, P.; Preden, J.S.; Jantsch, A. Fog Computing in the Internet of Things: Intelligence at the Edge; Springer: Berlin, Germany, 2017. [Google Scholar]
- Bonomi, F.; Milito, R.; Zhu, J.; Addepalli, S. Fog computing and its role in the internet of things. In Proceedings of the First Edition of the MCC Workshop on Mobile Cloud Computing, Helsinki, Finland, 17 August 2012; pp. 13–16. [Google Scholar]
- Allen, J. Photoplethysmography and its application in clinical physiological measurement. Physiol. Meas. 2007, 28, R1. [Google Scholar] [CrossRef] [PubMed]
- Faurholt-Jepsen, M.; Vinberg, M.; Frost, M.; Christensen, E.M.; Bardram, J.E.; Kessing, L.V. Smartphone data as an electronic biomarker of illness activity in bipolar disorder. Bipolar Disord. 2015, 17, 715–728. [Google Scholar] [CrossRef]
- El-Hajj, C.; Kyriacou, P.A. A review of machine learning techniques in photoplethysmography for the non-invasive cuff-less measurement of blood pressure. Biomed. Signal Process. Control 2020, 58, 101870. [Google Scholar] [CrossRef]
- Nawaz, A.; Øhlckers, P.; Sælid, S.; Jacobsen, M.; Nadeem Akram, M. Review: Non-invasive continuous blood glucose measurement techniques. J. Bioinform. Diabetes 2016, 1, 1–27. [Google Scholar] [CrossRef]
- Buchmayer, S.M.; Sparén, P.; Cnattingius, S. Previous pregnancy loss: Risks related to severity of preterm delivery. Am. J. Obstet. Gynecol. 2004, 191, 1225–1231. [Google Scholar] [CrossRef]
- Rahmani, A.M.; Thanigaivelan, N.K.; Gia, T.N.; Granados, J.; Negash, B.; Liljeberg, P.; Tenhunen, H. Smart e-health gateway: Bringing intelligence to internet-of-things based ubiquitous healthcare systems. In Proceedings of the 2015 12th Annual IEEE Consumer Communications and Networking Conference (CCNC), Las Vegas, NV, USA, 9–12 January 2015; pp. 826–834. [Google Scholar]
- Gear Sport. 2021. Available online: https://www.samsung.com/global/galaxy/gear-sport/specs/ (accessed on 12 January 2021).
- Tizen. 2021. Available online: https://www.tizen.org (accessed on 12 January 2021).
- Samsung Wearables. 2021. Available online: https://www.samsung.com/us/mobile/wearables/ (accessed on 12 January 2021).
- Angular. 2021. Available online: https://angular.io/ (accessed on 12 January 2021).
- Cordova. 2021. Available online: https://cordova.apache.org/ (accessed on 12 January 2021).
- Omron M3. 2021. Available online: https://www.omron-healthcare.fi/en/blood-pressure-monitors/m3_2.html#start=1 (accessed on 12 January 2021).
- Intelli Wrap Cuff. 2021. Available online: https://www.omron-healthcare.fi/en/blood-pressure-monitor-accessories/Intelli_Wrap_Cuff.html (accessed on 12 January 2021).
- Apache2 Web Server. 2021. Available online: https://ubuntu.com/server/docs/web-servers-apache (accessed on 12 January 2021).
- Flask. 2021. Available online: https://palletsprojects.com/p/flask/ (accessed on 12 January 2021).
- MongoDB. 2021. Available online: https://www.mongodb.com/ (accessed on 12 January 2021).
- Kim, H.G.; Cheon, E.J.; Bai, D.S.; Lee, Y.H.; Koo, B.H. Stress and heart rate variability: A meta-analysis and review of the literature. Psychiatry Investig. 2018, 15, 235. [Google Scholar] [CrossRef]
- Castaldo, R.; Melillo, P.; Bracale, U.; Caserta, M.; Triassi, M.; Pecchia, L. Acute mental stress assessment via short term HRV analysis in healthy adults: A systematic review with meta-analysis. Biomed. Signal Process. Control 2015, 18, 370–377. [Google Scholar] [CrossRef]
- Mehrabadi, M.A.; Azimi, I.; Sarhaddi, F.; Axelin, A.; Niela-Vilén, H.; Myllyntausta, S.; Stenholm, S.; Dutt, N.; Liljeberg, P.; Rahmani, A.M. Sleep Tracking of a Commercially Available Smart Ring and Smartwatch Against Medical-Grade Actigraphy in Everyday Settings: Instrument Validation Study. JMIR MHealth UHealth 2020, 8, e20465. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J. An overview of heart rate variability metrics and norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.; Bigger, J.T.; Camm, A.J.; Kleiger, R.E.; Malliani, A.; Moss, A.J.; Schwartz, P.J. Heart rate variability: Standards of measurement, physiological interpretation, and clinical use. Eur. Heart J. 1996, 17, 354–381. [Google Scholar] [CrossRef]
- Pecchia, L.; Castaldo, R.; Montesinos, L.; Melillo, P. Are ultra-short heart rate variability features good surrogates of short-term ones? State-of-the-art review and recommendations. Healthc. Technol. Lett. 2018, 5, 94–100. [Google Scholar] [CrossRef]
- Choi, A.; Shin, H. Photoplethysmography sampling frequency: Pilot assessment of how low can we go to analyze pulse rate variability with reliability? Physiol. Meas. 2017, 38, 586. [Google Scholar] [CrossRef] [PubMed]
- Amiri, D.; Anzanpour, A.; Azimi, I.; Levorato, M.; Rahmani, A.M.; Liljeberg, P.; Dutt, N. Edge-assisted sensor control in healthcare iot. In Proceedings of the 2018 IEEE Global Communications Conference (GLOBECOM), Abu Dhabi, United Arab Emirates, 9–13 December 2018; pp. 1–6. [Google Scholar]
- Gopalan, S.A.; Park, J.T. Energy-efficient MAC protocols for wireless body area networks: Survey. In Proceedings of the International Congress on Ultra Modern Telecommunications and Control Systems, Moscow, Russia, 18–20 October 2010; pp. 739–744. [Google Scholar]
- Aijaz, A.; Aghvami, A.H. Cognitive machine-to-machine communications for Internet-of-Things: A protocol stack perspective. IEEE Internet Things J. 2015, 2, 103–112. [Google Scholar] [CrossRef]
- Anzanpour, A.; Azimi, I.; Götzinger, M.; Rahmani, A.M.; TaheriNejad, N.; Liljeberg, P.; Jantsch, A.; Dutt, N. Self-awareness in remote health monitoring systems using wearable electronics. In Proceedings of the Conference on Design, Automation & Test in Europe, Lausanne, Switzerland, 27–31 March 2017; pp. 1056–1061. [Google Scholar]
- Sasai, K.; Izumi, S.; Watanabe, K.; Yano, Y.; Kawaguchi, H.; Yoshimoto, M. A Low-Power Photoplethysmography Sensor using Correlated Double Sampling and Reference Readout Circuit. In Proceedings of the 2019 IEEE SENSORS, Montreal, QC, Canada, 27–30 October 2019; pp. 1–4. [Google Scholar]
- Clawson, J.; Pater, J.A.; Miller, A.D.; Mynatt, E.D.; Mamykina, L. No longer wearing: Investigating the abandonment of personal health-tracking technologies on craigslist. In Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Osaka, Japan, 7 September 2015; pp. 647–658. [Google Scholar]
- Karapanos, E.; Gouveia, R.; Hassenzahl, M.; Forlizzi, J. Wellbeing in the making: Peoples’ experiences with wearable activity trackers. Psychol. Well-Being 2016, 6, 4. [Google Scholar] [CrossRef]
- Validic. 2021. Available online: https://validic.com/ (accessed on 20 March 2021).
- Fantinelli, S.; Marchetti, D.; Verrocchio, M.C.; Franzago, M.; Fulcheri, M.; Vitacolonna, E. Assessment of psychological dimensions in telemedicine care for gestational diabetes mellitus: A systematic review of qualitative and quantitative studies. Front. Psychol. 2019, 10, 153. [Google Scholar] [CrossRef]
- Lau, Y.; Htun, T.P.; Wong, S.N.; Tam, W.S.W.; Klainin-Yobas, P. Efficacy of internet-based self-monitoring interventions on maternal and neonatal outcomes in perinatal diabetic women: A systematic review and meta-analysis. J. Med. Internet Res. 2016, 18, e220. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening: Web Supplement 2: Summary of Findings and GRADE Tables; Technical Report; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- WHO. eHealth and Innovation in Women’S and Children’S Health: A Baseline Review: Based on the Findings of the 2013 Survey of CoIA Countries by the WHO Global Observatory for eHealth; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Bender, D.; Sartipi, K. HL7 FHIR: An Agile and RESTful approach to healthcare information exchange. In Proceedings of the 26th IEEE International Symposium on Computer-Based Medical Systems, Porto, Portugal, 20–22 June 2013; pp. 326–331. [Google Scholar]
| Variable | Units | Description |
|---|---|---|
| NN interval | ms | Normal inter-beat interval |
| RMSSD | ms | The square root of the mean of the sum of the squares of differences between adjacent NN intervals |
| AVNN | ms | Average of NN intervals |
| SDNN | ms | Standard deviation of all NN intervals |
| LF | ms | Power in low-frequency range (0.04–0.15 Hz) |
| HF | ms | Power in the high-frequency range (0.15–0.4 Hz) |
| LF/HF | - | LF/HF |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarhaddi, F.; Azimi, I.; Labbaf, S.; Niela-Vilén, H.; Dutt, N.; Axelin, A.; Liljeberg, P.; Rahmani, A.M. Long-Term IoT-Based Maternal Monitoring: System Design and Evaluation. Sensors 2021, 21, 2281. https://doi.org/10.3390/s21072281
Sarhaddi F, Azimi I, Labbaf S, Niela-Vilén H, Dutt N, Axelin A, Liljeberg P, Rahmani AM. Long-Term IoT-Based Maternal Monitoring: System Design and Evaluation. Sensors. 2021; 21(7):2281. https://doi.org/10.3390/s21072281
Chicago/Turabian StyleSarhaddi, Fatemeh, Iman Azimi, Sina Labbaf, Hannakaisa Niela-Vilén, Nikil Dutt, Anna Axelin, Pasi Liljeberg, and Amir M. Rahmani. 2021. "Long-Term IoT-Based Maternal Monitoring: System Design and Evaluation" Sensors 21, no. 7: 2281. https://doi.org/10.3390/s21072281
APA StyleSarhaddi, F., Azimi, I., Labbaf, S., Niela-Vilén, H., Dutt, N., Axelin, A., Liljeberg, P., & Rahmani, A. M. (2021). Long-Term IoT-Based Maternal Monitoring: System Design and Evaluation. Sensors, 21(7), 2281. https://doi.org/10.3390/s21072281







