The Use of Infrared Thermography to Develop and Assess a Wearable Sock and Monitor Foot Temperature in Diabetic Subjects
Abstract
1. Introduction
1.1. Diabetic Foot
1.2. The Role Temperature, Pressure Points and Activity on Diabetic Foot
1.3. The Utility of Wearables in Detecting Temperature and Aims of the Study
2. Types of Sensors to Monitor Temperatures
- Contact sensors, which must physically touch the object, using conductivity to measure changes.
- Noncontact sensors, which use convection and radiation to warn of a change in temperature.
3. Data Analysis
3.1. Data Collection
- General data about the individual, such as gender, age, weight, height, blood type, and the use of high heels; data specific for diabetes patients: type of diabetes, treatment, control of their diabetes; individuals suffering neuropathy disability; results of the modified Edinburgh questionnaire to diagnose arterial claudication; ankle-brachial index (ABI) and measurement of glycosylated hemoglobin.
- Habits: Way of life (sedentary lifestyle or practicing a sport); type of feeding (healthy diet or not); alcohol consumption; smoker or nonsmoker; any regular medication; and dominant foot.
- Comfort: Recent activity with current shoes; intensity of the most recent activity (no activity, walking, running, etc. during the last 30 min); comfort level with the current footwear (during the last 30 min) by means of a 1 to 5 Likert scale, being 1 “very comfortable” and 5 “very uncomfortable”; and the type of footwear that they usually use.
- Blood pressure and central temperature: data of systolic blood pressure (high), diastolic blood pressure (low), and central temperature (thermometer).
- Climate data (season data) including date, and number of photos from the foot (sole and dorsal from both feet).
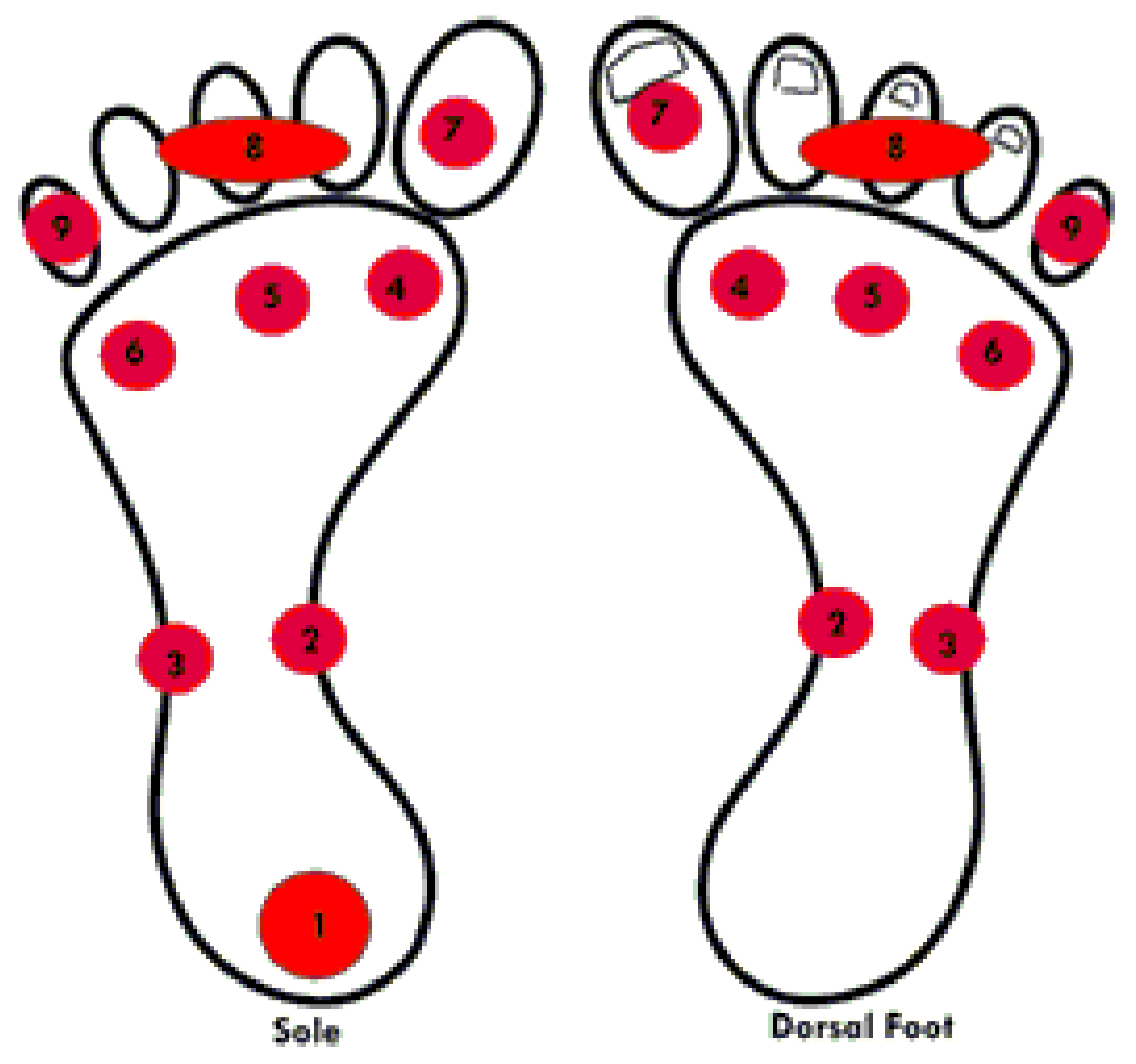
- Temperature measurements (prewalk right foot data) were performed with a thermal camera FLIR E60bx, with an infrared resolution of pixels, a sensitivity of C and a precision of %. Thermal picture were taken 1 m far from a foot covered in black cardboard. A total of 17 data average temperatures (9 plantar and 8 dorsal) of each participant were collected and stored using the The Flir Tools software (Similar to Figure 1). This number of ROIs has been used previously in thermographyc assessments [38,39,40] (see Figure 2). Room humidity (%) and temperature (C) were also measured with a Flir MR 77 device.
- Temperature measurements (prewalk left foot data).
- Temperature measurements (postwalk right foot data). After the 100 m walking, the temperature was recorded in the same way as in point 6.
- Temperature measurements (postwalk left foot data).
- Foot Posture. Scores of Foot Posture Index (FPI) for left and right foot were assessed following standard procedure [41], subjects in their relaxed stance position, both limb support, arms relaxed and looking straight ahead; foot posture classification was found to be neutral when the score was between 0 to 5, supinated from to and pronated from 6 to 12 [42]; presence of plantar hyperkeratosis at any zone of the foot was also recorded.
- Final comments and remarks.
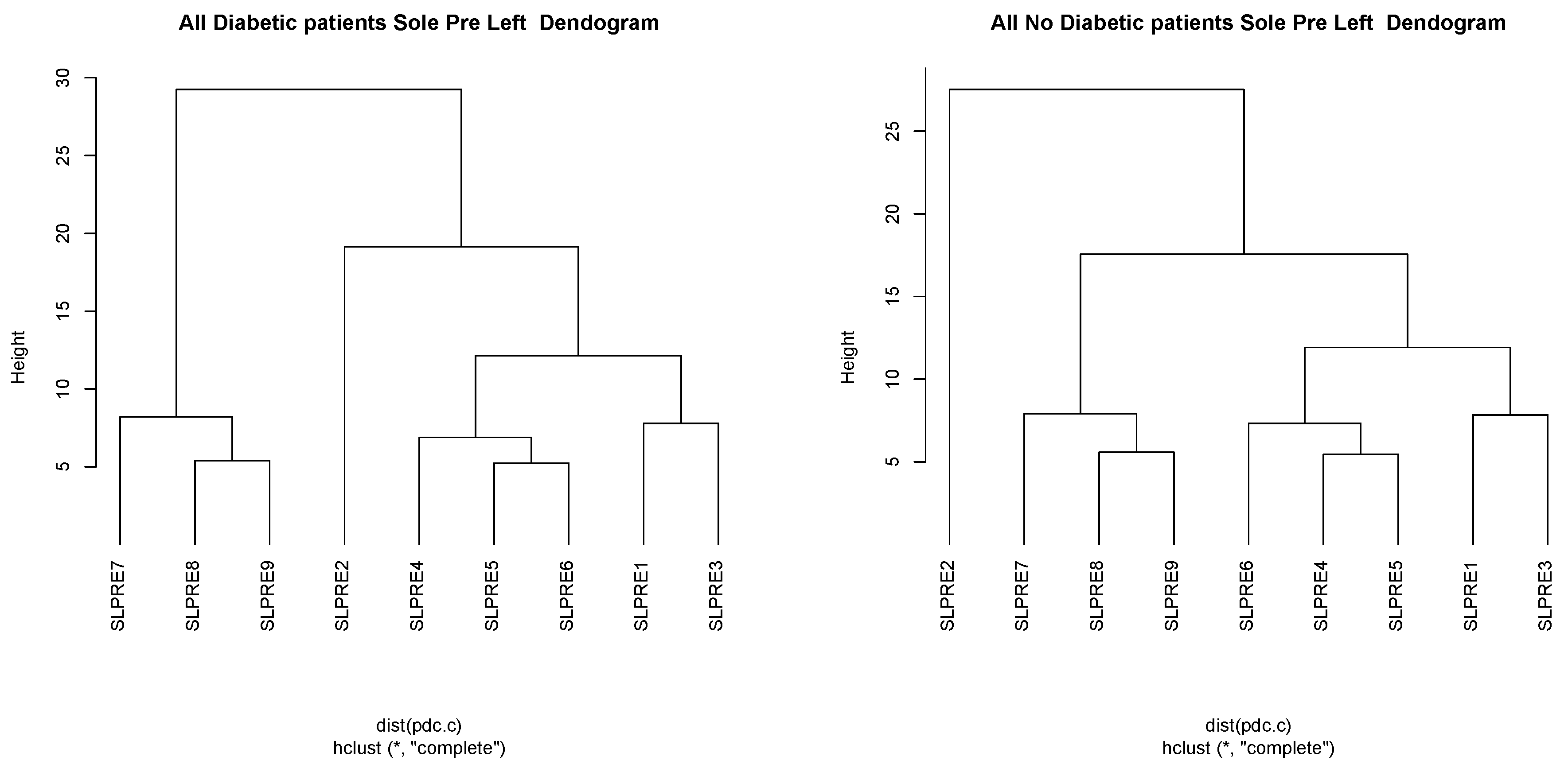
3.2. Statistical Data Analysis
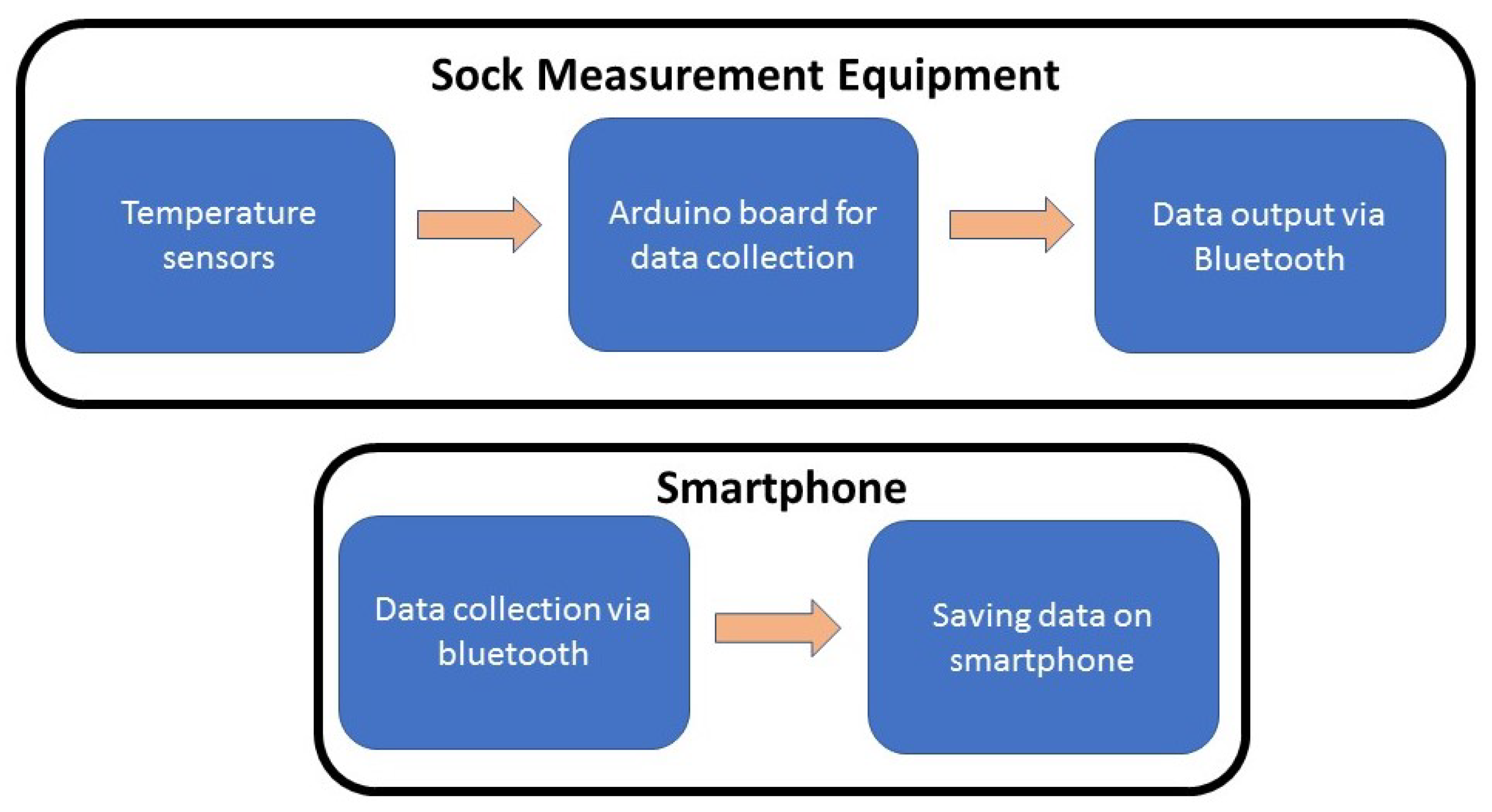
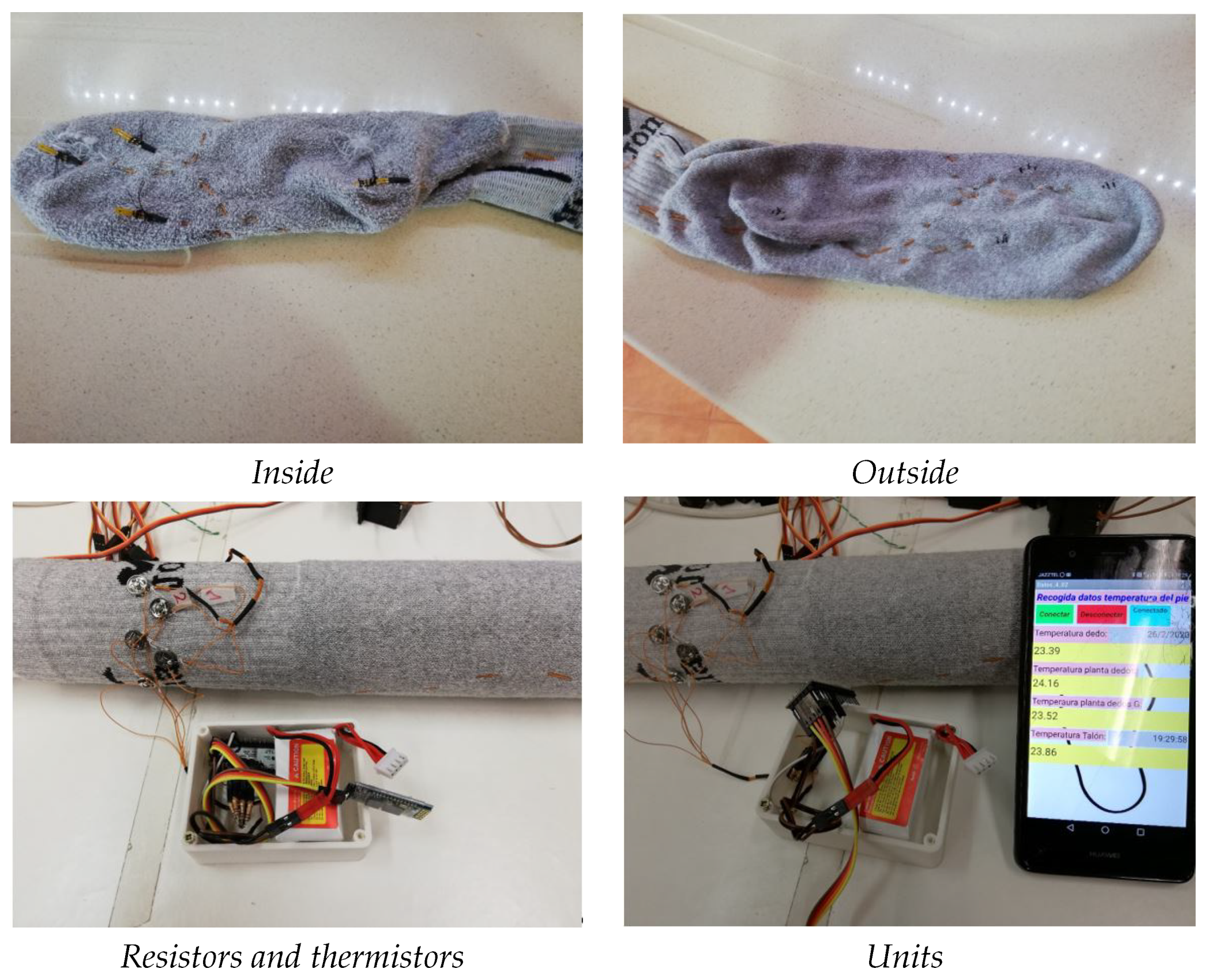
4. A Prototype of a Smart Sock
4.1. Introduction
4.2. NTC TTF 103 Thermistor
4.3. Arduino
4.4. Smartphone Application
5. Conclusions and Future Work
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dounis, E.; Makrilakis, K.; Tentolouris, N.; Tsapogas, P. Atlas of the Diabetic Foot; John Wiley & Sons: Hoboken, NJ, USA, 2010. [Google Scholar]
- Singh, N.; Armstrong, D.G.; Lipsky, B.A. Preventing foot ulcers in patients with diabetes. JAMA 2005, 293, 217–228. [Google Scholar] [CrossRef]
- Litzelman, D.K.; Marriott, D.J.; Vinicor, F. Independent physiological predictors of foot lesions in patients with NIDDM. Diabetes Care 1997, 20, 1273–1278. [Google Scholar] [CrossRef]
- National Diabetes Data Group (U.S.); National Institute of Diabetes and Digestive and Kidney Diseases (U.S.); National Institutes of Health (U.S.). Diabetes in America; NIH Publication: Washington, DC, USA, 1995.
- Karrer, S. Diabetisches Fußsyndrom. Der Hautarzt 2011, 62, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Lahiri, B.; Bagavathiappan, S.; Jayakumar, T.; Philip, J. Medical applications of infrared thermography: A review. Infrared Phys. Technol. 2012, 55, 221–235. [Google Scholar] [CrossRef]
- Akimov, E.; Son’kin, V. Skin temperature and lactate threshold during muscle work in athletes. Hum. Physiol. 2011, 37, 621. [Google Scholar] [CrossRef]
- Purvis, A.; Tunstall, H. Effects of sock type on foot skin temperature and thermal demand during exercise. Ergonomics 2004, 47, 1657–1668. [Google Scholar] [CrossRef] [PubMed]
- McLellan, K.; Petrofsky, J.S.; Bains, G.; Zimmerman, G.; Prowse, M.; Lee, S. The effects of skin moisture and subcutaneous fat thickness on the ability of the skin to dissipate heat in young and old subjects, with and without diabetes, at three environmental room temperatures. Med. Eng. Phys. 2009, 31, 165–172. [Google Scholar] [CrossRef]
- Macdonald, A.; Petrova, N.L.; Ainarkar, S.; Allen, J.; Plassmann, P.; Whittam, A.; Bevans, J.T.; Ring, F.; Kluwe, B.; Simpson, R.M.; et al. Thermal symmetry of healthy feet: A precursor to a thermal study of diabetic feet prior to skin breakdown. Physiol. Meas. 2017, 38, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Astasio-Picado, A.; Martínez, E.E.; Nova, A.M.; Rodríguez, R.S.; Gómez–Martín, B. Thermal map of the diabetic foot using infrared thermography. Infrared Phys. Technol. 2018, 93, 59–62. [Google Scholar] [CrossRef]
- Rodríguez-Sáenz, S.D.; Franco-Pérez, S.S.; Espinoza-Valdez, A.; Salido-Ruiz, R.A.; Curiel-López, F.B. Instrumented Footwear for Diabetic Foot Monitoring: Foot Sole Temperature Measurement. In Proceedings of the Latin American Conference on Biomedical Engineering, Cancún, Mexico, 2–5 October 2019; Springer: Cham, Switzerland, 2019; pp. 501–507. [Google Scholar]
- Chatchawan, U.; Narkto, P.; Damri, T.; Yamauchi, J. An exploration of the relationship between foot skin temperature and blood flow in type 2 diabetes mellitus patients: A cross-sectional study. J. Phys. Ther. Sci. 2018, 30, 1359–1363. [Google Scholar] [CrossRef]
- Bagavathiappan, S.; Philip, J.; Jayakumar, T.; Raj, B.; Rao, P.N.S.; Varalakshmi, M.; Mohan, V. Correlation between Plantar Foot Temperature and Diabetic Neuropathy: A Case Study by Using an Infrared Thermal Imaging Technique. J. Diabetes Sci. Technol. 2010, 4, 1386–1392. [Google Scholar] [CrossRef] [PubMed]
- Petrova, N.L.; Whittam, A.; MacDonald, A.; Ainarkar, S.; Donaldson, A.N.; Bevans, J.; Allen, J.; Plassmann, P.; Kluwe, B.; Ring, F.; et al. Reliability of a novel thermal imaging system for temperature assessment of healthy feet. J. Foot Ankle Res. 2018, 11, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Gatt, A.; Falzon, O.; Cassar, K.; Ellul, C.; Camilleri, K.P.; Gauci, J.; Mizzi, S.; Mizzi, A.; Sturgeon, C.; Camilleri, L.; et al. Establishing Differences in Thermographic Patterns between the Various Complications in Diabetic Foot Disease. Int. J. Endocrinol. 2018, 2018, 9808295. [Google Scholar] [CrossRef] [PubMed]
- Gatt, A.; Falzon, O.; Cassar, K.; Camilleri, K.P.; Gauci, J.; Ellul, C.; Mizzi, S.; Mizzi, A.; Papanas, N.; Sturgeon, C.; et al. The Application of Medical Thermography to Discriminate Neuroischemic Toe Ulceration in the Diabetic Foot. Int. J. Low. Extrem. Wounds 2018, 17, 102–105. [Google Scholar] [CrossRef] [PubMed]
- Skafjeld, A.; Iversen, M.; Holme, I.; Ribu, L.; Hvaal, K.; Kilhovd, B. A pilot study testing the feasibility of skin temperature monitoring to reduce recurrent foot ulcers in patients with diabetes—A randomized controlled trial. BMC Endocr. Disord. 2015, 15, 55. [Google Scholar] [CrossRef] [PubMed]
- Pit’hová, P.; Patkova, H.; Galandakova, I.; Dolezalova, L.; Kvapil, M. Differences in ulcer location in diabetic foot syndrome. Vnitr. Lek. 2007, 53, 1278–1285. [Google Scholar]
- Mansor, H.; Shukor, M.H.A.; Meskam, S.S.; Rusli, N.Q.A.M.; Zamery, N.S. Body temperature measurement for remote health monitoring system. In Proceedings of the 2013 IEEE International Conference on Smart Instrumentation, Measurement and Applications (ICSIMA), Kuala Lumpur, Malaysia, 25–27 November 2013; IEEE: Piscataway, NJ, USA, 2013; pp. 1–5. [Google Scholar]
- Majumder, S.; Mondal, T.; Deen, M.J. Wearable sensors for remote health monitoring. Sensors 2017, 17, 130. [Google Scholar] [CrossRef]
- Electronics Tutorials (s.f.). Temperature Sensors. Available online: https://www.electronics-tutorials.ws/io/io_3.html (accessed on 13 January 2021).
- Reddy, P.N.; Cooper, G.; Weightman, A.; Hodson-Tole, E.; Reeves, N. An in-shoe temperature measurement system for studying diabetic foot ulceration etiology: Preliminary results with healthy participants. Procedia CIRP 2016, 49, 153–156. [Google Scholar] [CrossRef]
- Recreational Physics (Spanish). Available online: https://www.fisicarecreativa.com/guias/sensorestemp.pdf (accessed on 13 January 2021).
- Martín-Vaquero, J.; Hernández Encinas, A.; Queiruga-Dios, A.; José Bullón, J.; Martínez-Nova, A.; Torreblanca González, J.; Bullón-Carbajo, C. Review on wearables to monitor foot temperature in diabetic patients. Sensors 2019, 19, 776. [Google Scholar] [CrossRef] [PubMed]
- Childs, P.R.; Greenwood, J.; Long, C. Review of temperature measurement. Rev. Sci. Instrum. 2000, 71, 2959–2978. [Google Scholar] [CrossRef]
- González, J.T.; Nova, A.M.; Encinas, A.; Martín-Vaquero, J.; Queiruga-Dios, A. Statistical Analysis to Control Foot Temperature for Diabetic People. In Proceedings of the World Conference on Information Systems and Technologies, Budva, Montenegro, 7–10 April 2020; Springer: Cham, Switzerland, 2020; pp. 295–306. [Google Scholar]
- Nath, J.K.; Sharma, S.; Sarma, K.C. A Comparative Study of Accuracy Improvement of Temperature Measurement with PT100 and PT1000 for Wider Range. Int. J. Electron. Eng. Res. 2017, 9, 735–743. [Google Scholar]
- Classification of Thermoresistances (Spanish). Available online: http://server-die.alc.upv.es/asignaturas/lsed/2003-04/0.Sens_Temp/Clasify/Termorresistencias.htm (accessed on 13 January 2021).
- NTC Thermistor. Available online: http://www.resistorguide.com/ntc-thermistor/ (accessed on 13 January 2021).
- PTC Thermistor. Available online: http://www.resistorguide.com/ptc-thermistor/ (accessed on 13 January 2021).
- Carr, J.J. Sensors and Circuits: Sensors, Transducers, and Supporting Circuits for Electronic Instrumentation, Measurement, and Control; PTR Prentice Hall: Englewood Cliffs, NJ, USA, 1993. [Google Scholar]
- Sudha, S.; Shruthi, P.; Sharanya, M. IOT Based Measurement of Body Temperature using MAX30205. Int. Res. J. Eng. Technol. 2018, 5, 3913–3915. [Google Scholar]
- MAX30205 Temperature Sensor. Available online: https://datasheets.maximintegrated.com/en/ds/MAX30205.pdf (accessed on 13 January 2021).
- Si7006-A20. Available online: https://www.silabs.com/documents/public/data-sheets/Si7006-A20.pdf (accessed on 13 January 2021).
- AD590 Temperature Transducer. Available online: http://www.analog.com/media/en/technical-documentation/data-sheets/AD590.pdf (accessed on 13 January 2021).
- Bossuyt, P.M.; Reitsma, J.B.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.P.; Irwig, L.M.; Moher, D.; Rennie, D.; de Vet, H.C.W.; et al. The STARD statement for reporting studies of diagnostic accuracy: Explanation and elaboration. Ann. Intern. Med. 2003, 138, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Queiruga-Dios, A.; Pérez, J.B.; Encinas, A.H.; Martín-Vaquero, J.; Nova, A.M.; González, J.T. Skin Temperature Monitoring to Avoid Foot Lesions in Diabetic Patients. In Proceedings of the International Conference on Practical Applications of Computational Biology & Bioinformatics, Porto, Portugal, 21–23 June 2017; Springer: Cham, Switzerland, 2017; pp. 110–117. [Google Scholar]
- Armstrong, D.G.; Lavery, L.A.; Harkless, L.B. Validation of a Diabetic Wound Classification System: The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care 1998, 21, 855–859. [Google Scholar] [CrossRef] [PubMed]
- Escamilla-Martínez, E.; Gómez-Martín, B.; Sánchez-Rodríguez, R.; Fernández-Seguín, L.M.; Pérez-Soriano, P.; Martínez-Nova, A. Running thermoregulation effects using bioceramics versus polyester fibres socks. J. Ind. Text. 2020. [Google Scholar] [CrossRef]
- Pascual-Huerta, J.; Arcas Lorente, C.; Trincado Villa, L.; García Carmona, F.; Fernández Morato, D. Relationship between foot posture index and plantar pressure distribution in patients with limb length inequality: A case series study. Rev. Esp. Podol. 2018, 29, 21–26. [Google Scholar]
- Sánchez-Rodríguez, R.; Valle-Estévez, S.; Fraile-García, P.; Martínez-Nova, A.; Gómez-Martín, B.; Escamilla-Martínez, E. Modification of Pronated Foot Posture after a Program of Therapeutic Exercises. Int. J. Environ. Res. Public Health 2020, 17, 8406. [Google Scholar] [CrossRef]
- Hughes-Riley, T.; Lugoda, P.; Dias, T.; Trabi, C.L.; Morris, R.H. A Study of thermistor performance within a textile structure. Sensors 2017, 17, 1804. [Google Scholar] [CrossRef] [PubMed]
- Hatamie, A.; Angizi, S.; Kumar, S.; Pandey, C.M.; Simchi, A.; Willander, M.; Malhotra, B.D. Textile based chemical and physical sensors for healthcare monitoring. J. Electrochem. Soc. 2020, 167, 037546. [Google Scholar] [CrossRef]
- Thermistor Calculator V1.1. Available online: https://www.thinksrs.com/downloads/programs/Therm%20Calc/NTCCalibrator/NTCcalculator.htm (accessed on 13 January 2021).







| CAT | CTE | AGE | BMI | DB | TNMX | TNMN | TC | TEXT | TPRE | HPRE |
|---|---|---|---|---|---|---|---|---|---|---|
| SRPRE1 | 8.78695 | 0.03 | −0.91140 | 0.04171 | −0.05392 | 0.56426 | 0.12670 | |||
| SRPRE2 | 17.94235 | 0.01558 | −1.47390 | 0.03612 | −0.03644 | 0.38426 | 0.07408 | |||
| SRPRE4 | −20.96860 | 0.02549 | 0.10193 | −1.36591 | −0.04557 | 0.82781 | 0.67369 | 0.13880 | ||
| SRPRE6 | −26.14073 | 0.13748 | −1.02450 | 0.04952 | −0.09264 | 0.79693 | 0.74866 | 0.18130 | ||
| SRPRE7 | −38.27672 | 0.03712 | 0.11602 | −1.28288 | −0.05528 | 1.14328 | 0.81583 | 0.15686 | ||
| SLPRE1 | −14.00475 | 0.03628 | −0.84698 | 0.04798 | −0.05280 | 0.61893 | 0.53951 | 0.11614 | ||
| SLPRE2 | 15.65169 | −0.74912 | 0.04795 | −0.04274 | 0.39359 | 0.09685 | ||||
| SLPRE4 | −31.30703 | 0.11339 | −1.42929 | 0.06371 | −0.08094 | 0.93555 | 0.72724 | 0.16288 | ||
| SLPRE6 | −32.83695 | 0.02528 | 0.09846 | −1.33277 | 0.05504 | −0.07547 | 0.92974 | 0.76525 | 0.15994 | |
| SLPRE7 | −39.72836 | 0.04965 | −1.20896 | 1.11495 | 0.84074 | 0.14443 | ||||
| SRPOST1 | −7.01999 | 0.04641 | −0.93266 | 0.48558 | 0.64667 | |||||
| SRPOST2 | −3.44379 | 0.10557 | −1.33277 | 0.06073 | −0.04858 | 0.56932 | 0.07686 | 0.27156 | ||
| SRPOST4 | −15.45718 | 0.02753 | −1.63835 | 0.04549 | −0.05258 | 0.67605 | 0.73318 | |||
| SRPOST6 | −20.78108 | 0.11620 | −1.07018 | 0.05828 | −0.08463 | 0.65984 | 0.79016 | 0.08394 | ||
| SRPOST7 | −24.79945 | 0.03964 | −1.35335 | 0.88517 | 0.78046 | |||||
| SLPOST1 | −12.99850 | 0.03859 | −1.03925 | 0.05417 | −0.04706 | 0.58444 | 0.63557 | |||
| SLPOST2 | 15.67648 | 0.02831 | −1.21562 | 0.03380 | 0.39475 | |||||
| SLPOST4 | −15.34189 | 0.02699 | −1.32829 | 0.04989 | −0.05053 | 0.62868 | 0.74446 | |||
| SLPOST6 | −20.94168 | 0.02664 | −1.15666 | 0.05514 | −0.04966 | 0.73794 | 0.76450 | |||
| SLPOST7 | −29.61293 | 0.04579 | −1.07319 | 0.96990 | 0.81785 |
| DSPRE | Mean | sd | se(mean) | IQR | cv | Skewness | Kurtosis | 0% | 25% | 50% | 75% | 100% |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DSPRE1 | 0.0938 | 0.8234 | 0.1176 | 0.7 | 8.7716 | −1.7464 | 7.6044 | −3.6 | −0.2 | 0.1 | 0.5 | 1.7 |
| DSPRE2 | 0.4326 | 0.5550 | 0.0792 | 0.6 | 1.2828 | 0.2910 | 0.9031 | −0.9 | 0.1 | 0.4 | 0.7 | 2.0 |
| DSPRE4 | 0.2081 | 1.2282 | 0.1754 | 0.9 | 5.9005 | −1.1939 | 3.8264 | −3.9 | −0.1 | 0.3 | 0.8 | 3.1 |
| DSPRE6 | 0.0551 | 0.9757 | 0.1393 | 1.1 | 17.7082 | −1.2871 | 5.0223 | −4.0 | −0.5 | 0.1 | 0.6 | 1.8 |
| DSPRE7 | 0.1163 | 1.1422 | 0.1631 | 1.1 | 9.8193 | 0.25053 | 0.3911 | −2.7 | −0.5 | 0.0 | 0.6 | 3.0 |
| Resistence/Thermistor | Res 1 | Temp 1 | Res 2 | Temp 2 | Res 3 | Temp 3 | Res 4 | Temp 4 |
|---|---|---|---|---|---|---|---|---|
| R1/NTC1 | 9.80 k | C | 24.88 k | C | 8.31 k | C | 5.02 k | C |
| R2/NTC2 | 9.83 k | C | 24.33 k | C | 8.38 k | C | 5.20 k | C |
| R3/NTC3 | 9.82 k | C | 24.19 k | C | 8.30 k | C | 5.15 k | C |
| R4/NTC4 | 9.85 k | C | 24.50 k | C | 8.34 k | C | 5.19 k | C |
| R5/NTC5 | 9.79 k | C | 25.12 k | C | 8.34 k | C | 5.26 k | C |
| R6/NTC6 | 9.84 k | C | 25.21 k | C | 8.47 k | C | 5.47 k | C |
| Thermistor | |||
|---|---|---|---|
| NTC1 | 1.409294790 | 1.684156947 | 5.069508025 |
| NTC2 | 1.149226326 | 2.051360360 | 4.064329590 |
| NTC3 | 1.076255140 | 2.180997134 | 3.519982960 |
| NTC4 | 0.762209845 | 2.695628622 | 1.483573950 |
| NTC5 | 1.300653498 | 1.843001087 | 4.536745780 |
| NTC6 | 0.579418628 | 2.997765865 | 0.2115108092 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torreblanca González, J.; Gómez-Martín, B.; Hernández Encinas, A.; Martín-Vaquero, J.; Queiruga-Dios, A.; Martínez-Nova, A. The Use of Infrared Thermography to Develop and Assess a Wearable Sock and Monitor Foot Temperature in Diabetic Subjects. Sensors 2021, 21, 1821. https://doi.org/10.3390/s21051821
Torreblanca González J, Gómez-Martín B, Hernández Encinas A, Martín-Vaquero J, Queiruga-Dios A, Martínez-Nova A. The Use of Infrared Thermography to Develop and Assess a Wearable Sock and Monitor Foot Temperature in Diabetic Subjects. Sensors. 2021; 21(5):1821. https://doi.org/10.3390/s21051821
Chicago/Turabian StyleTorreblanca González, José, Beatriz Gómez-Martín, Ascensión Hernández Encinas, Jesús Martín-Vaquero, Araceli Queiruga-Dios, and Alfonso Martínez-Nova. 2021. "The Use of Infrared Thermography to Develop and Assess a Wearable Sock and Monitor Foot Temperature in Diabetic Subjects" Sensors 21, no. 5: 1821. https://doi.org/10.3390/s21051821
APA StyleTorreblanca González, J., Gómez-Martín, B., Hernández Encinas, A., Martín-Vaquero, J., Queiruga-Dios, A., & Martínez-Nova, A. (2021). The Use of Infrared Thermography to Develop and Assess a Wearable Sock and Monitor Foot Temperature in Diabetic Subjects. Sensors, 21(5), 1821. https://doi.org/10.3390/s21051821








